Normal sinus rhythm
In normal sinus rhythm, the heart rhythm originates from the sinus node or sinoatrial (SA) node (the dominant pacemaker of the heart). Normal sinus rhythm is often regular with constant P-P intervals 1. When the sinus rhythm has some irregularity to it, it is known as sinus arrhythmia. In general, the normal heart rate in adults ranges between 60 and 100 beats per minute. However, normal variations do exist depending on the individual’s age and gender. A sinus rhythm with a rate above the normal range is called sinus tachycardia, and one below the normal range is called sinus bradycardia.
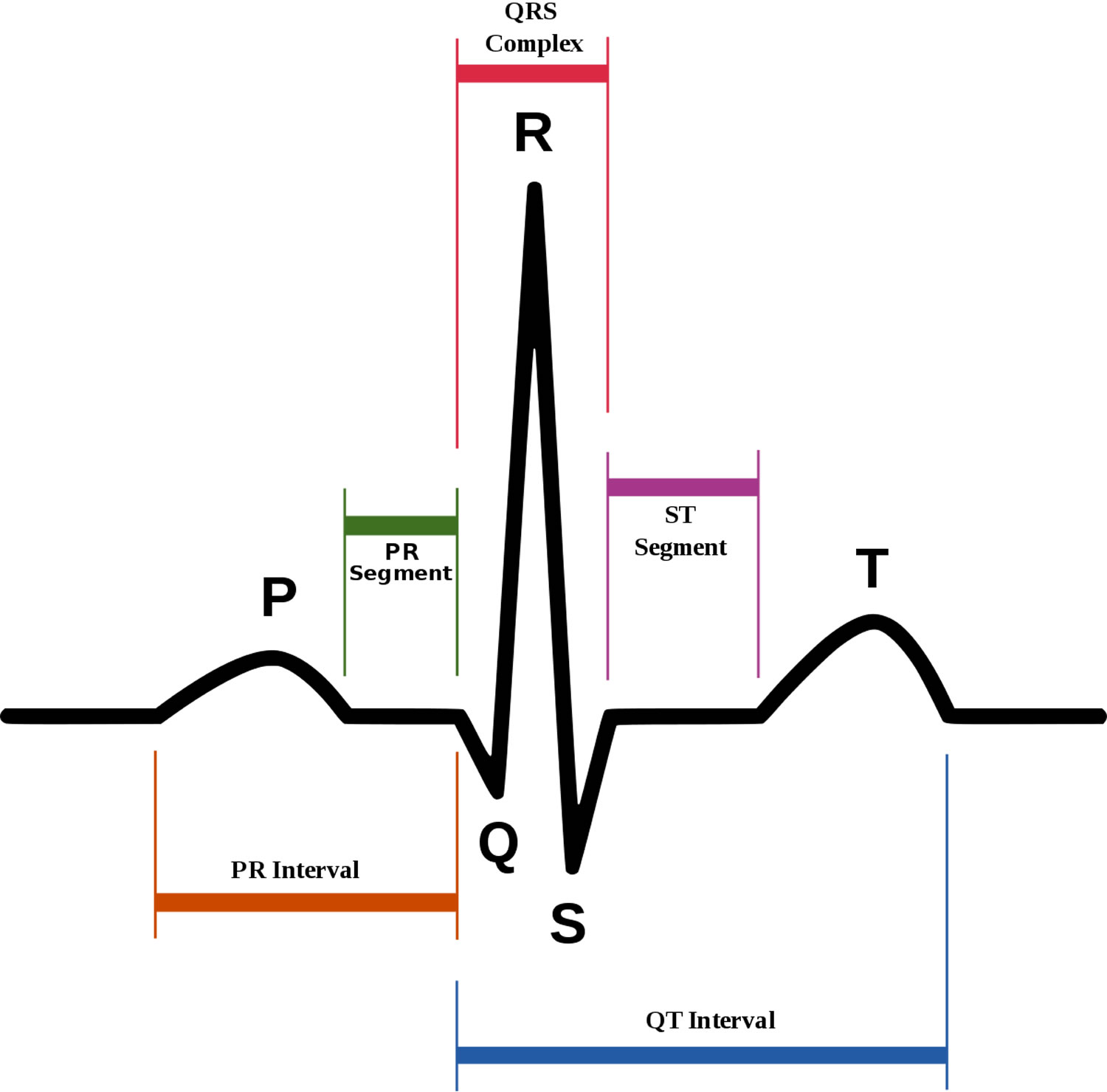
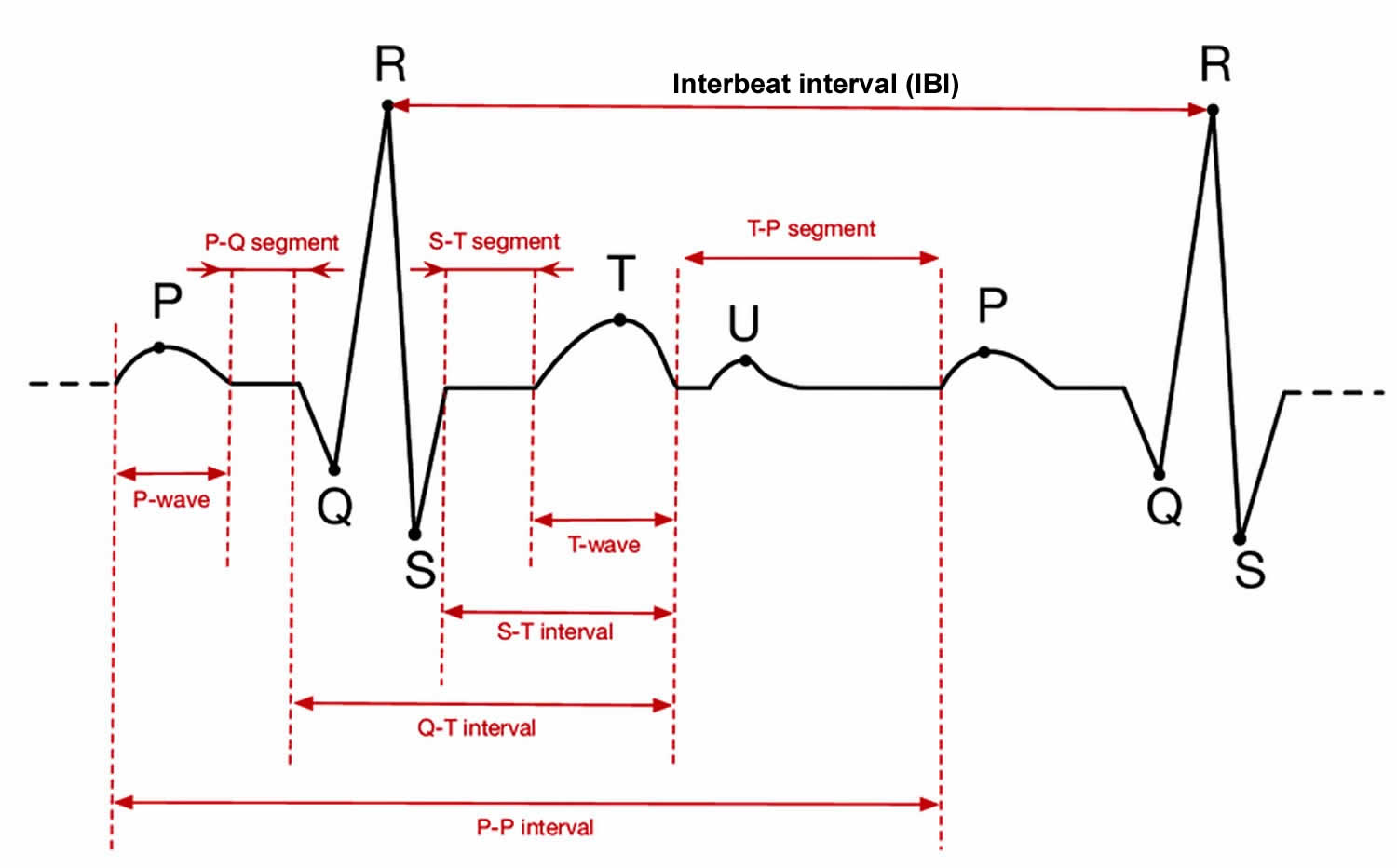
In normal sinus rhythm, the P wave is less than 120 milliseconds in duration and less than 0.15 mV to 0.25 mV in height in lead II. The permissible maximum varies based on the lead. If there is a biphasic P wave in lead V1, the terminal component should be less than 40 milliseconds in duration and 0.10 mV in depth. The P wave should also have a normal axis (0 degrees to more than 90 degrees) and constant morphology. The normal axis is indicated by P waves that are:
- Upright in leads I, II, and often aVF
- Inverted in lead aVR
- Upright, inverted, or biphasic in leads III and aVL
- Upright or biphasic in leads V1 and V2
- Upright in leads V3 through V6.
There are some cases of normal sinus rhythm in which the P wave duration and morphology may be abnormal. This usually reflects atrial disease and/or an atrial electrical conduction defect.
The normal PR interval ranges between 120 ms and 200 ms. It tends to be in the lower range of normal as the heart rate increases due to rate-related shortening of action potentials. Conversely, slower heart rates tend to increase the PR interval towards the upper range of normal. Nevertheless, the PR interval is independent of the presence or absence of sinus rhythm.
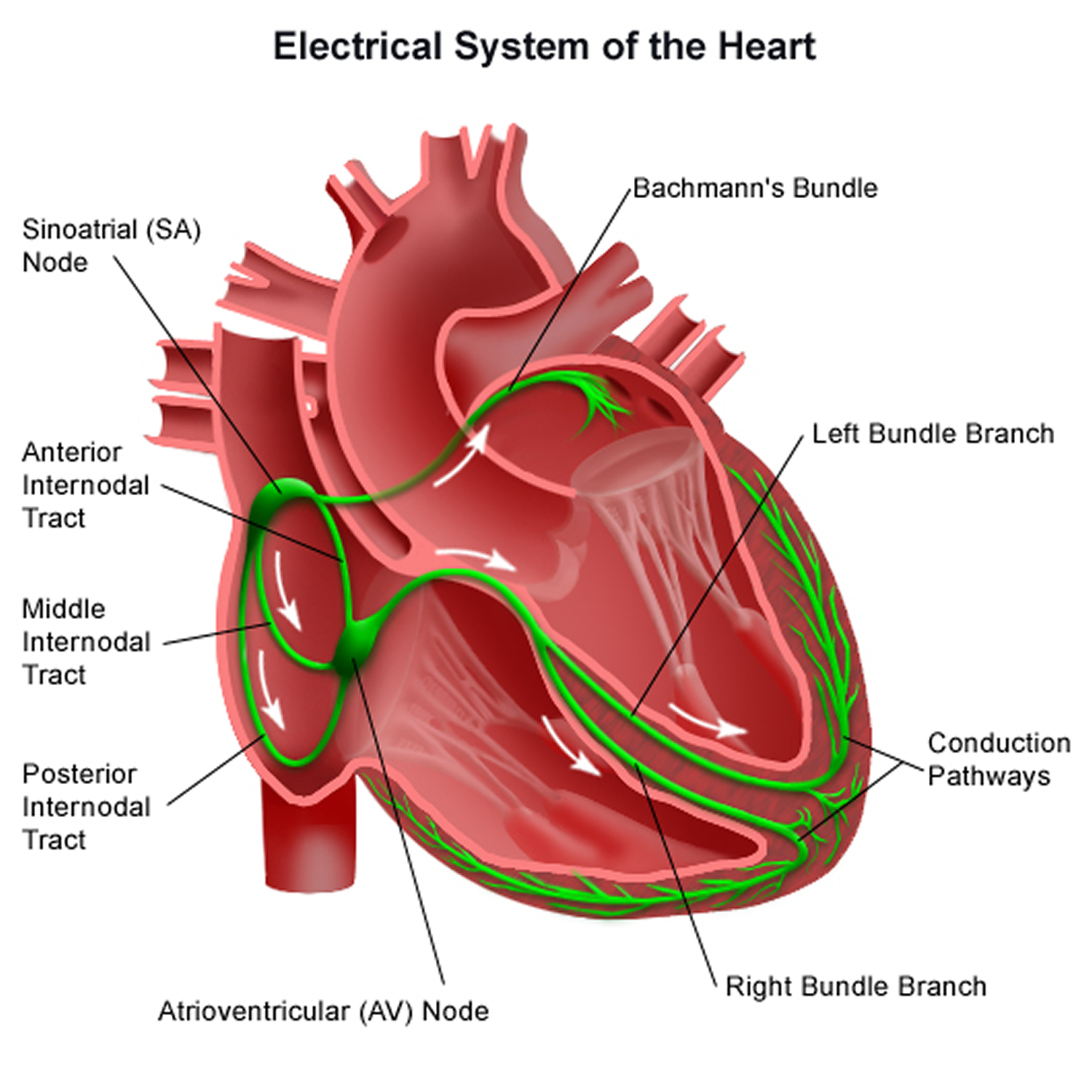
Your heart is made up of four chambers — two upper (atria) and two lower (ventricles). The rhythm of your heart is normally controlled by the sinus node (sinoatrial node [SA node]), an area of specialized cells in the right atrium (Figure 2). This natural pacemaker produces the electrical impulses that trigger each heartbeat. From the sinus node, electrical impulses travel across the atria to the ventricles, causing them to contract and pump blood to your lungs and body.
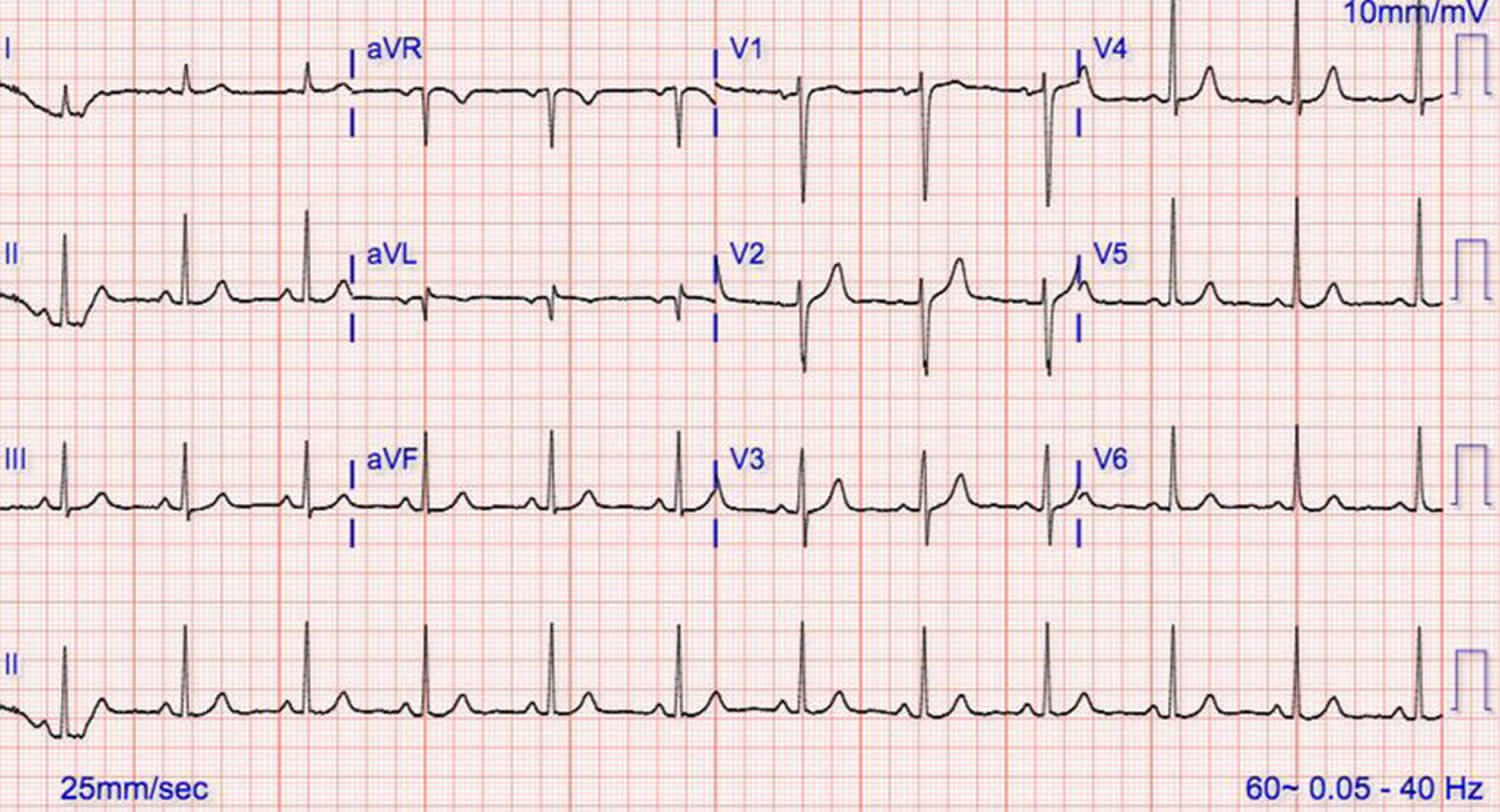
Figure 1. Normal sinus rhythm ECG
Figure 2. Heart’s electrical system
Abnormal sinus rhythm
Sick sinus rhythm
Sinus node dysfunction also known by its historical name sick sinus syndrome or sinus node disease, is a group of heart rhythm problems (arrhythmias) in which the heart’s natural pacemaker (sinoatrial node [SA node]) doesn’t work properly to produce an adequate heart rate that meets the physiologic needs of the individual 2. If you have sick sinus syndrome, your sinoatrial node [SA node] isn’t functioning properly, causing your heart rate to be too slow (bradycardia), too fast (tachycardia) or irregular. Sinus node dysfunction is often due to either abnormality in impulses produced by the pacemaker cells or abnormality in conduction across the perinodal cells. Sick sinus syndrome can be either acquired or inherited; the acquired form is more common. Patients may or may not be symptomatic. Per definition, sinus node dysfunction should include symptoms and ECG findings simultaneously such as sinus bradycardia, sinus pauses or arrest, sinus exit blocks, or chronotropic incompetence (inadequate heart rate response to activity). Or the failure of the return of sinoatrial node (SA) nodal activity after electrical cardioversion 3. Sinus node dysfunction can be associated with atrial tachycardia as part of the tachycardia-bradycardia syndrome.
Types of sick sinus syndrome and their causes include:
- Sinoatrial block. Electrical signals move too slowly through the sinus node, causing an abnormally slow heart rate.
- Sinus arrest. The sinus node activity pauses, causing skipped beats.
- Bradycardia-tachycardia syndrome. The heart rate alternates between abnormally fast and slow rhythms, usually with a long pause (asystole) between heartbeats.
There are several types and variations of sinus node dysfunction. Some of these include sinus pause, arrest, exit block, and arrhythmia as well as wandering atrial pacemaker 1. Because the mass of the sinus node is too small to create a significant electrical signal, it is not manifested directly on the ECG. Instead, sinoatrial nodal pacemaker activity must be inferred from the P waves of atrial depolarization. Hence, sinus node dysfunction is often noted with an inappropriate sinoatrial nodal response to the body’s metabolic demands and/or the absence of P waves.
Sick sinus rhythm causes
Sinus node dysfunction results from the abnormal automaticity, conduction, or both of the sinoatrial node and surrounding tissues. Both could result from abnormal mechanisms, including fibrosis, atherosclerosis, and inflammatory/infiltrative processes.
- Sinus Node Fibrosis: Replacement of the sinus node tissue by fibrous tissue is the most common cause of sinus node dysfunction, the replacement can also include other parts of the conduction system, including the atrioventricular (AV) node 4.
- Medication: Prescription medications can depress the sinus node function, potentially resulting in sinus node dysfunction include: beta blocker, non-dihydropyridine calcium channel blockers, digoxin, antiarrhythmic medications, and acetylcholinesterase inhibitors 5.
- Infiltrative disease: The SA node tissue can be affected during the disease process of some of the infiltrative diseases such as amyloidosis, sarcoidosis, scleroderma, hemochromatosis, and pericarditis leading to sinus node dysfunction.
- Ischemia: The sinus node is perfused by the sinoatrial nodal artery, which arises from the right coronary artery in 60 % of the time and from the left circumflex artery in 40 % of the time. Narrowing of this artery can lead to impairment of the sinus node function leading to sinus node dysfunction that can be potentially reversible. Almost all such cases are present in inferior myocardial infarction 6.
- Familial sinus node dysfunction in rare cases can be the result of cardiac sodium channel mutations of SCN5A and HCN4 genes 7.
- Miscellaneous: Other disorders that can rarely cause sinus node dysfunction to include hypothyroidism, hypothermia, and hypoxia.
What makes the sinus node misfire?
Diseases and conditions that cause scarring or damage to your heart’s electrical system can be the reason. Scar tissue from a previous heart surgery also can be the cause, particularly in children. Rarely, the cause can be genetic.
Sick sinus syndrome can be unmasked by medications, such as calcium channel blockers or beta blockers used to treat high blood pressure, or by other conditions causing the heartbeat to be slower or faster than normal. In most cases, the sinus node doesn’t work properly because of age-related wear and tear to the heart muscle.
Sick sinus rhythm symptoms
Most people with sick sinus syndrome initially have few or no symptoms. In some cases, symptoms come and go. When they occur, sick sinus syndrome signs and symptoms might include:
- Slower than normal pulse (bradycardia)
- Fatigue
- Dizziness or lightheadedness
- Fainting or near fainting
- Shortness of breath
- Chest pains
- Confusion
- A sensation of rapid, fluttering heartbeats (palpitations)
Sick sinus rhythm complications
When your heart’s natural pacemaker isn’t working properly, your heart can’t perform as efficiently as it should. This can lead to:
- Atrial fibrillation, a chaotic rhythm of the upper chambers of the heart
- Heart failure
- Stroke
- Cardiac arrest
Sick sinus rhythm diagnosis
Diagnosing for sick sinus syndrome might include:
- Electrocardiogram (ECG). During this test, sensors (electrodes) are attached to your chest and limbs to create a record of the electrical signals traveling through your heart. The test might show patterns that indicate sick sinus syndrome, including fast heart rate, slow heart rate or a long pause in the heartbeat (asystole) after a fast heart rate.
- Exercise stress testing: If the diagnosis could not be made based on history, and ECG then exercise stress testing is necessary. Things to look for is the failure of appropriate chronotropic response to exercise, defined as less than 80 percent of the predictable heart rate response to exercise. Also, it will exclude myocardial ischemia and help to program the devices for patients who ultimately receive a permanent pacemaker 8.
- Holter monitor. This portable device is carried in your pocket or in a pouch on a belt or shoulder strap. It automatically records your heart’s activity for 24 to 72 hours, which provides your health care provider with an extended look at your heart rhythms.
- Event recorder. This portable electrocardiogram device can also be carried in your pocket or worn on a belt or shoulder strap for home monitoring of your heart’s activity. You might be asked to use this device to use for up to a month.When you feel symptoms, you push a button, and a brief ECG recording is saved. This allows your health care provider to see your heart rhythm at the time of your symptoms, which can help pinpoint sick sinus syndrome.
- Implantable loop recorder. This small device is implanted just under the skin of your chest and is used for continuous, long-term monitoring of your heart’s electrical activity. An implantable loop recorder may be worn from months to years.This device is automatically triggered by an irregular heart rhythm (arrhythmia) or you can trigger it when you feel symptoms.
- Electrophysiologic testing: This test is rarely used to screen for sick sinus syndrome. However, in some cases, it can help check the function of your sinus node, as well as other electrical properties of your heart. During this test, thin, flexible tubes (catheters) tipped with electrodes are threaded through your blood vessels to various spots along the electrical pathways in your heart. Once in place, the electrodes can precisely map the spread of electrical impulses during each beat and may identify the source of heart rhythm problems.
Sick sinus rhythm treatment
Treatment for sick sinus syndrome focuses on eliminating or reducing unpleasant symptoms. If you aren’t bothered by symptoms, you may only need regular checkups to monitor your condition. For people who are bothered by symptoms, the treatment of choice is usually an implanted electronic pacemaker.
Pacing the heart
Most people with sick sinus syndrome eventually need a permanent artificial pacemaker to maintain a regular heartbeat. This small, battery-powered electronic device is implanted under the skin near your collarbone during a minor surgical procedure. The pacemaker is programmed to stimulate or “pace” your heart as needed to keep it beating normally.
The type of pacemaker you need depends on the type of irregular heart rhythm you have. Some rhythms can be treated with a single chamber pacemaker, which uses only one wire (lead) to pace one chamber of the heart — in this case, the atrium. However, most people with sick sinus syndrome benefit from dual chamber pacemakers, in which one lead paces the atrium and one lead paces the ventricle.
You’ll be able to resume normal or near-normal activities after you recover from pacemaker implantation surgery. The risk of complications, such as swelling or infection in the area where the pacemaker was implanted, is small.
Additional treatments for fast heart rate
If you have a rapid heart rate as part of your sick sinus syndrome, you may need additional treatments to control these rhythms:
- Medications: If you have a pacemaker and your heart rate is still too fast, your doctor may prescribe anti-arrhythmia medications to prevent fast rhythms. If you have atrial fibrillation or other abnormal heart rhythms that increase your risk of stroke, you may need a blood-thinning medicine, such as warfarin (Coumadin, Jantoven) or dabigatran (Pradaxa).
- AV node ablation: This procedure can also control fast heart rhythms in people with pacemakers. It involves applying radiofrequency energy through a long, thin tube (catheter) to destroy (ablate) the tissue around the atrioventricular (AV) node between the atria and the ventricles. This stops fast heart rhythms from reaching the ventricles and causing problems.
- Radiofrequency ablation of atrial fibrillation: This procedure is similar to AV node ablation. However, in this case, ablation targets the tissue that triggers atrial fibrillation. This actually eliminates atrial fibrillation itself, rather than just preventing it from reaching the ventricles.
Sick sinus rhythm prognosis
Sinus node dysfunction is a progressive noncurable but manageable disease. Complications of sinus node dysfunction without a pacemaker include hypotension and syncope. In a study that followed 52 patients with sinus node dysfunction presenting with sinus bradycardia associated with a sinoatrial block or sinoatrial arrest, it took an average of 13 years to progress to complete the sinoatrial arrest and an escape rhythm 9. It is unclear if sinus node dysfunction is associated with increased mortality as most patients with sinus node dysfunction have other cardiovascular comorbidities. In a study of 19000 from two cohorts followed for an average of 17 years, 213 persons developed sinus node dysfunction (0.6 events per 1000 person a year). While the development of sinus node dysfunction carried an association with increased mortality, it became attenuated when adjusted for incident cardiovascular disease. Sinus node dysfunction correlates with increased morbidity, but it is unclear if it affects mortality 10.
Sinus pause and arrest
Sinus pause or arrest results when there is a problem with initiating electrical discharge from the sinoatrial node (SA) node. As a result, the ECG will show a transient absence of sinus P waves. This can last for a few seconds or even several minutes. Because the sinus node stops firing and can start back up at any moment, there is often no relationship between previous P waves and those that follow (i.e., non-compensatory). Also, the sinus pause or arrest tends to permit enough time for escape beats or rhythms to follow. A sinus pause of a few seconds is not always pathologic and may, in fact, be seen in non-diseased hearts. However, if a sinus pause and arrest goes on for longer, patients can become symptomatic experiencing lightheadedness, dizziness, presyncope, syncope, and possibly death 11.
Sinoatrial nodal exit block
Sinoatrial (SA) nodal exit block occurs when the sinus node fires, although the impulse is unable to reach neighboring atrial tissue. It is believed to involve the perinodal (T) cells. Similar to sinus pause and arrest, the atria do not receive the proper signal to contract, and thus, the ECG shows an absence of P waves. There are three degrees of SA nodal exit block, first, second, and third degree. They follow the conventional atrioventricular (AV) nodal blocks. To conceptualize these, there are three components to keep in mind: 1) a relatively constant input from the SA node, 2) an area across which the block occurs, and 3) output (i.e., the P waves). The type of SA nodal exit block can be determined by evaluating the P waves.
- First degree sinoatrial nodal exit block. With first-degree SA nodal exit block, there is impulse exit slowing with normal 1:1 conduction. A body surface EKG is not able to recognize this.
- Second degree sinoatrial nodal exit block. Like second-degree AV nodal blocks, there are two types second-degree SA nodal exit blocks – type I (Wenckebach) and type II.
- With type I (Wenckebach), the P-P intervals progressively shorten in duration until there is a dropped P wave. The dropped P wave results in a pause that is less than two P-P intervals in duration.
- Type II also has a pause from a dropped P wave, it is a multiple of the SA nodal pacemaker input. Therefore, the P-P intervals should remain constant and compensatory in nature.
- Third degree sinoatrial nodal exit block. With third-degree SA nodal exit block, the SA node impulse is unable to reach the right atrium. Thus, the atrial will not depolarize, and there will be no P wave. For this reason, it cannot be distinguished from sinus arrest
Sinus arrhythmia
Sinus arrhythmia is a commonly encountered variation of normal sinus rhythm. Sinus arrhythmia represents small variations in the sinus cycle length. Sinus arrhythmia characteristically presents with an irregular rate in which the variation in the R-R interval is greater than 120 milliseconds in the presence of normal P waves 12. There can be small variations in the PR interval. Sinus arrhythmias are more commonly seen in young individuals and those exposed to morphine or digoxin. The two predominant types are a result of normal respiration and digoxin toxicity. During respiration, the intermittent vagus nerve activation occurs, which results in beat to beat variations in the resting heart rate. When present, sinus arrhythmia typically indicates good cardiovascular health. Therefore, unless the patient has been receiving digoxin, patients are often asymptomatic and do not require treatment.
Wandering atrial pacemaker
Wandering atrial pacemaker is not pathologic and is often seen in young, healthy individuals. It results from a change in the dominant pacemaker focus from the sinus node to ectopic atrial foci. There must be at least three dominant ectopic atrial foci to meet the diagnostic criteria for wandering atrial pacemaker. This can be seen on ECG by a variation in P wave morphology and the PR interval. Each variation in P wave morphology represents a different ectopic focus. The closer the ectopic focus is to the AV node, the shorter the PR interval will be. Because wandering atrial pacemaker is not considered pathologic and often asymptomatic, there is no indication for treatment.
References- Kashou AH, Basit H, Chhabra L. Physiology, Sinoatrial Node (SA Node) [Updated 2019 Jun 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459238
- Jabbour F, Kanmanthareddy A. Sinus Node Dysfunction. [Updated 2019 Jun 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544253
- Ferrer MI. The sick sinus syndrome in atrial disease. JAMA. 1968 Oct 14;206(3):645-6.
- Thery C, Gosselin B, Lekieffre J, Warembourg H. Pathology of sinoatrial node. Correlations with electrocardiographic findings in 111 patients. Am. Heart J. 1977 Jun;93(6):735-40.
- Vera Z, Awan NA, Mason DT. Assessment of oral quinidine effects on sinus node function in sick sinus syndrome patients. Am. Heart J. 1982 Jan;103(1):80-4.
- Hatle L, Bathen J, Rokseth R. Sinoatrial disease in acute myocardial infarction. Long-term prognosis. Br Heart J. 1976 Apr;38(4):410-4.
- Benson DW, Wang DW, Dyment M, Knilans TK, Fish FA, Strieper MJ, Rhodes TH, George AL. Congenital sick sinus syndrome caused by recessive mutations in the cardiac sodium channel gene (SCN5A). J. Clin. Invest. 2003 Oct;112(7):1019-28.
- Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR, Goldschlager NF, Hamilton RM, Joglar JA, Kim RJ, Lee R, Marine JE, McLeod CJ, Oken KR, Patton KK, Pellegrini CN, Selzman KA, Thompson A, Varosy PD. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2018 Nov 06
- Lien WP, Lee YS, Chang FZ, Lee SY, Chen CM, Tsai HC. The sick sinus syndrome: natural history of dysfunction of the sinoatrial node. Chest. 1977 Nov;72(5):628-34.
- Alonso A, Jensen PN, Lopez FL, Chen LY, Psaty BM, Folsom AR, Heckbert SR. Association of sick sinus syndrome with incident cardiovascular disease and mortality: the Atherosclerosis Risk in Communities study and Cardiovascular Health Study. PLoS ONE. 2014;9(10):e109662
- Hafeez Y, Grossman SA. Paroxysmal Supraventricular (PSVT) [Updated 2019 May 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507699
- Soos MP, McComb D. Sinus Arrhythmia. [Updated 2019 Jun 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537011