What is skin turgor
Skin turgor is the skin’s elasticity. Skin turgor is the ability of skin to change shape and return to normal. Skin turgor is a sign of fluid loss (dehydration). Skin turgor measurement, whilst part of the initial assessment of children with suspected dehydration, is only moderately reliable and other clinical signs should be sought to confirm this diagnosis 1. Evaluation of the individual signs of dehydration revealed the presence of sunken eyes to be the most significantly correlated with degree of dehydration, followed by decreased skin turgor, week radial pulse, general appearance, dry mucous membranes, absent tears, increased heart rate, altered breathing, capillary refill time more than 2 seconds and decreased urine output 2. Sunken eyes, decreased skin turgor, weak radial pulse and general appearance are an optimal four variable model. Of these four findings, the presence of any two indicates a deficit of 5% or more, and three or more findings indicates a deficit of at least 10% 2.
Diarrhea or vomiting can cause fluid loss. Infants and young children with these conditions can rapidly lose lot of fluid, if they do not take enough water. Fever speeds up this process.
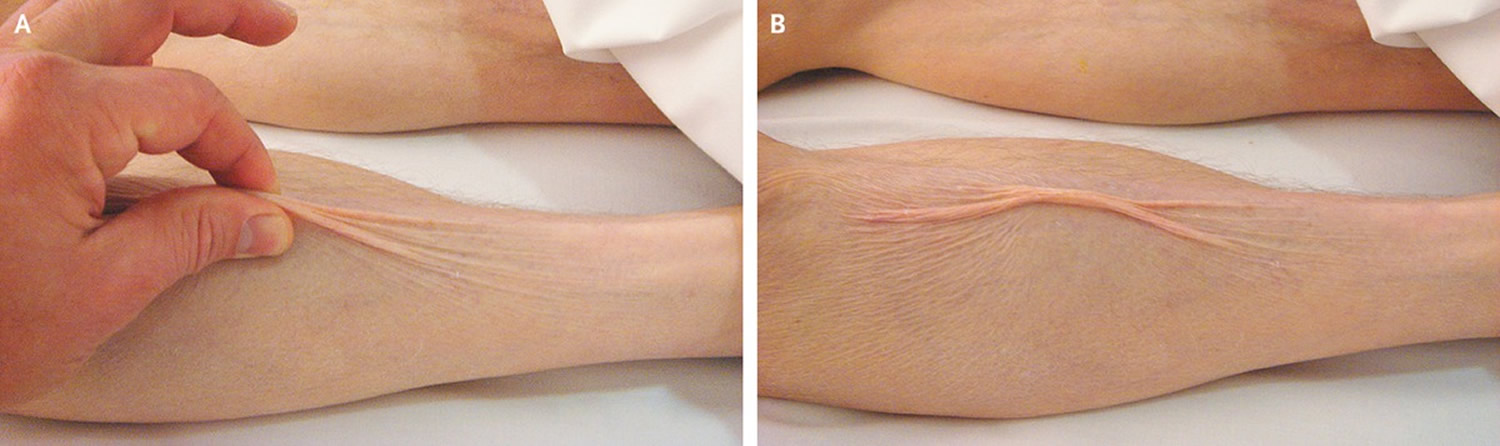
To check for skin turgor, the health care provider grasps the skin between two fingers so that it is tented up. Commonly on the lower arm or abdomen is checked. The skin is held for a few seconds then released.
Skin with normal turgor snaps rapidly back to its normal position. Skin with poor turgor takes time to return to its normal position.
Lack of skin turgor occurs with moderate to severe fluid loss. Mild dehydration is when fluid loss of 5% of the body weight. Moderate dehydration is 10% loss and severe dehydration is 15% or more loss of body weight.
Edema is a condition where fluid builds up in the tissues and causes swelling. This causes the skin to be extremely difficult to pinch up.
Your doctor can often diagnose dehydration on the basis of physical signs and symptoms. If you’re dehydrated, you’re also likely to have low blood pressure, especially when moving from a lying to a standing position, a faster than normal heart rate and reduced blood flow to your extremities.
To help confirm the diagnosis and pinpoint the degree of dehydration, you may have other tests, such as:
- Blood tests. Blood samples may be used to check for a number of factors, such as the levels of your electrolytes — especially sodium and potassium — and how well your kidneys are working.
- Urinalysis. Tests done on your urine can help show whether you’re dehydrated and to what degree. They also can check for signs of a bladder infection.
See your doctor if:
- Poor skin turgor occurs with vomiting, diarrhea, or fever.
- The skin is very slow to return to normal, or the skin “tents” up during a check. This can indicate severe dehydration that needs quick treatment.
- You have reduced skin turgor and are unable to increase your intake of fluids (for example, because of vomiting).
Skin turgor test
You can quickly check for dehydration at home. Pinch the skin over the back of the hand, on the abdomen, or over the front of the chest under the collarbone. This will show skin turgor.
A decrease in skin turgor is indicated when the skin (on the back of the hand for an adult or on the abdomen for a child) is pulled up for a few seconds and does not return to its original state. A decrease in skin turgor is a late sign of dehydration.
Mild dehydration will cause the skin to be slightly slow in its return to normal. To rehydrate, drink more fluids — particularly water.
Severe poor skin turgor indicates moderate or severe fluid loss. See your doctor right away.
Poor skin turgor causes
Common causes of poor skin turgor are:
- Decreased fluid intake
- Dehydration
- Diarrhea
- Diabetes
- Extreme weight loss
- Heat exhaustion (excessive sweating without enough fluid intake)
- Vomiting
Connective tissue disorders such as scleroderma and Ehlers-Danlos syndrome can affect the elasticity of the skin. These connective tissue disorders do not have to do with fluids.
Signs of dehydration in adults include:
- Being thirsty
- Urinating less often than usual
- Dark-colored urine
- >Dry skin
- Feeling tired
- Dizziness and fainting
Signs of dehydration in babies and young children include a dry mouth and tongue, crying without tears, no wet diapers for 3 hours or more, a high fever and being unusually sleepy or drowsy.
How is poor skin turgor treated?
The only effective treatment for dehydration is to replace lost fluids and lost electrolytes. The best approach to dehydration treatment depends on age, the severity of dehydration and its cause.
For infants and children who have become dehydrated from diarrhea, vomiting or fever, use an over-the-counter oral rehydration solution. These solutions contain water and salts in specific proportions to replenish both fluids and electrolytes.
Start with about a teaspoon (5 milliliters) every one to five minutes and increase as tolerated. It may be easier to use a syringe for very young children. Older children can be given diluted sports drinks. Use 1 part sports drink to 1 part water.
Most adults with mild to moderate dehydration from diarrhea, vomiting or fever can improve their condition by drinking more water or other liquids. Diarrhea may be worsened by full-strength fruit juice and soft drinks.
If you work or exercise outdoors during hot or humid weather, cool water is your best bet. Sports drinks containing electrolytes and a carbohydrate solution also may be helpful.
Children and adults who are severely dehydrated should be treated by emergency personnel arriving in an ambulance or in a hospital emergency room. Salts and fluids delivered through a vein (intravenously) are absorbed quickly and speed recovery.
References- Fayomi O, Maconochie I, Body R. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Is skin turgor reliable as a means of assessing hydration status in children?. Emerg Med J. 2007;24(2):124-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2658191/
- Hoxha T, Xhelili L, Azemi M, et al. Performance of clinical signs in the diagnosis of dehydration in children with acute gastroenteritis. Med Arch. 2015;69(1):10-2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4384849/