Sleep deprivation
Sleep deprivation is defined as not obtaining adequate total sleep or sleep deprivation is defined as “obtaining inadequate sleep to support adequate daytime alertness” 1. Sleep deprivation describes the cumulative effect of a person not having sufficient sleep 2. Insufficient sleep adversely effects your body, brain, mood and cognitive function 3. All aspects of your health can be impacted by sleep deprivation. When someone is in a chronic sleep-deprived state, they’ll notice excessive daytime sleepiness, fatigue, clumsiness, and weight gain or weight loss 2. In addition, being sleep-deprived affects both the brain and cognitive function 4. Long-term sleep deprivation has a detrimental effect on your attention, learning, working memory and is associated with exaggerated neural reactivity 4. According to the Centers for Disease Control and Prevention (CDC), 1 in every 25 adults report that they fall asleep at the wheel at least once a month which results in an estimated 6000 fatal crashes a year 5. If you have trouble sleeping, there are many natural tips you can try. If you are someone who doesn’t take sleep seriously, you may want to reconsider. Moreover, sleep deprivation is also associated with maladaptations of physiological and behavioral functions.
There are strong associations with serious medical conditions such as diabetes mellitus and insulin resistance, hypertension, obesity, obstructive sleep apnea, depression, and anxiety 6. These medical and psychiatric comorbidities put a person at risk for heart attack and stroke 6. Other adverse consequences of chronic sleep loss on public health include increased mortality and morbidity, poor performance on waking activities resulting in increased accidents and injuries, lower self-reported quality of life, decreased family well-being, and reduced use of health care. Sleep deprivation affects the ability of health workers who are involved in multitude of life saving tasks which need more attention and concentration 4. Extended work shifts of twelve hours or longer is common with nurses, whose insufficient sleep puts patients’ health and their health at risk 7. Sleep deprivation among nurses is the major cause for making an error in patient care and significant decrease in vigilance of the job 8.
It is clear that sleep loss has a profound effect on human health and well-being. Quantity and quality of sleep play an essential role in mental and physical health and merit consideration in any treatment plan. Interestingly, there’s a subset of cases whereby sleep deprivation can actually lead to an enhanced mood, alertness, and increased energy 2. Note that relatively few studies have compared the different effects between chronic partial-sleep restriction and acute total-sleep deprivation, and the total absence of sleep over long periods of time has not been studied in humans. That being said, long-term total sleep deprivation resulted in death in lab animals 2.
If you are struggling with sleep deprivation symptoms, talk to your physician or sleep doctor about treatment options.
How many hours of sleep do I need?
The amount of sleep you need each day will change over the course of your life, your sleep patterns change as you age. Despite variations in sleep quantity and quality, both related to age and between individuals, studies suggest that the optimal amount of sleep needed to perform adequately, avoid a sleep debt, and not have problem sleepiness during the day is about 7–8 hours for adults and at least 10 hours for school-aged children and adolescents. Similar amounts seem to be necessary to avoid an increased risk of developing obesity, diabetes, or cardiovascular diseases.
Quality of sleep and the timing of sleep are as important as quantity. People whose sleep is frequently interrupted or cut short may not get enough of both non-REM sleep and REM sleep. Both types of sleep appear to be crucial for learning and memory—and perhaps for the restorative benefits of healthy sleep, including the growth and repair of cells.
The table below shows general recommendations for different age groups. This table reflects recent American Academy of Sleep Medicine recommendations that the American Academy of Pediatrics has endorsed.
Table 1. Recommended Amount of Sleep
| Age | Recommended Amount of Sleep |
|---|---|
| Infants aged 4-12 months | 12-16 hours a day (including naps) |
| Children aged 1-2 years | 11-14 hours a day (including naps) |
| Children aged 3-5 years | 10-13 hours a day (including naps) |
| Children aged 6-12 years | 9-12 hours a day |
| Teens aged 13-18 years | 8-10 hours a day |
| Adults aged 18 years or older | 7–8 hours a day |
Babies initially sleep as much as 16 to 18 hours per day, which may boost growth and development (especially of the brain). School-age children and teens on average need about 9.5 hours of sleep per night. Most adults need 7-9 hours of sleep a night, but after age 60, nighttime sleep tends to be shorter, lighter, and interrupted by multiple awakenings. Elderly people are also more likely to take medications that interfere with sleep.
For example, some older people complain of difficulty falling asleep, early morning awakenings, frequent and long awakenings during the night, daytime sleepiness, and a lack of refreshing sleep. Many sleep problems, however, are not a natural part of sleep in the elderly. Their sleep complaints may be due, in part, to medical conditions, illnesses, or medications they are taking—all of which can disrupt sleep. In fact, one study found that the prevalence of sleep problems is very low in healthy older adults. Other causes of some of older adults’ sleep complaints are sleep apnea, restless legs syndrome, and other sleep disorders that become more common with age. Also, older people are more likely to have their sleep disrupted by the need to urinate during the night.
There is no evidence that indicates older people can get by with less sleep than younger people. There is some evidence showing that the biological clock shifts in older people, so they are more apt to go to sleep earlier at night and wake up earlier in the morning. Poor sleep in older people may result in excessive daytime sleepiness, attention and memory problems, depressed mood, and overuse of sleeping pills.
Across the lifespan, the sleep period tends to advance, namely relative to teenagers; older adults tend to go to bed earlier and wake earlier. The quality—but not necessarily the quantity—of deep, NREM sleep also changes, with a trend toward lighter sleep. The relative percentages of stages of sleep appear to stay mostly constant after infancy. From midlife through late life, people awaken more throughout the night. These sleep disruptions cause older people to lose more and more of stages 1 and 2 non-REM sleep as well as REM sleep.
In general, people are getting less sleep than they need due to longer work hours and the availability of round-the-clock entertainment and other activities 10.
If you routinely lose sleep or choose to sleep less than needed, the sleep loss adds up. The total sleep lost is called your sleep debt. For example, if you lose 2 hours of sleep each night, you’ll have a sleep debt of 14 hours after a week. Many people feel they can “catch up” on missed sleep during the weekend but, depending on how sleep-deprived they are, sleeping longer on the weekends may not be adequate 10.
Some people nap as a way to deal with sleepiness. Naps may provide a short-term boost in alertness and performance. However, napping doesn’t provide all of the other benefits of night-time sleep. Thus, you can’t really make up for lost sleep.
Some people sleep more on their days off than on work days. They also may go to bed later and get up later on days off.
Sleeping more on days off might be a sign that you aren’t getting enough sleep. Although extra sleep on days off might help you feel better, it can upset your body’s sleep–wake rhythm.
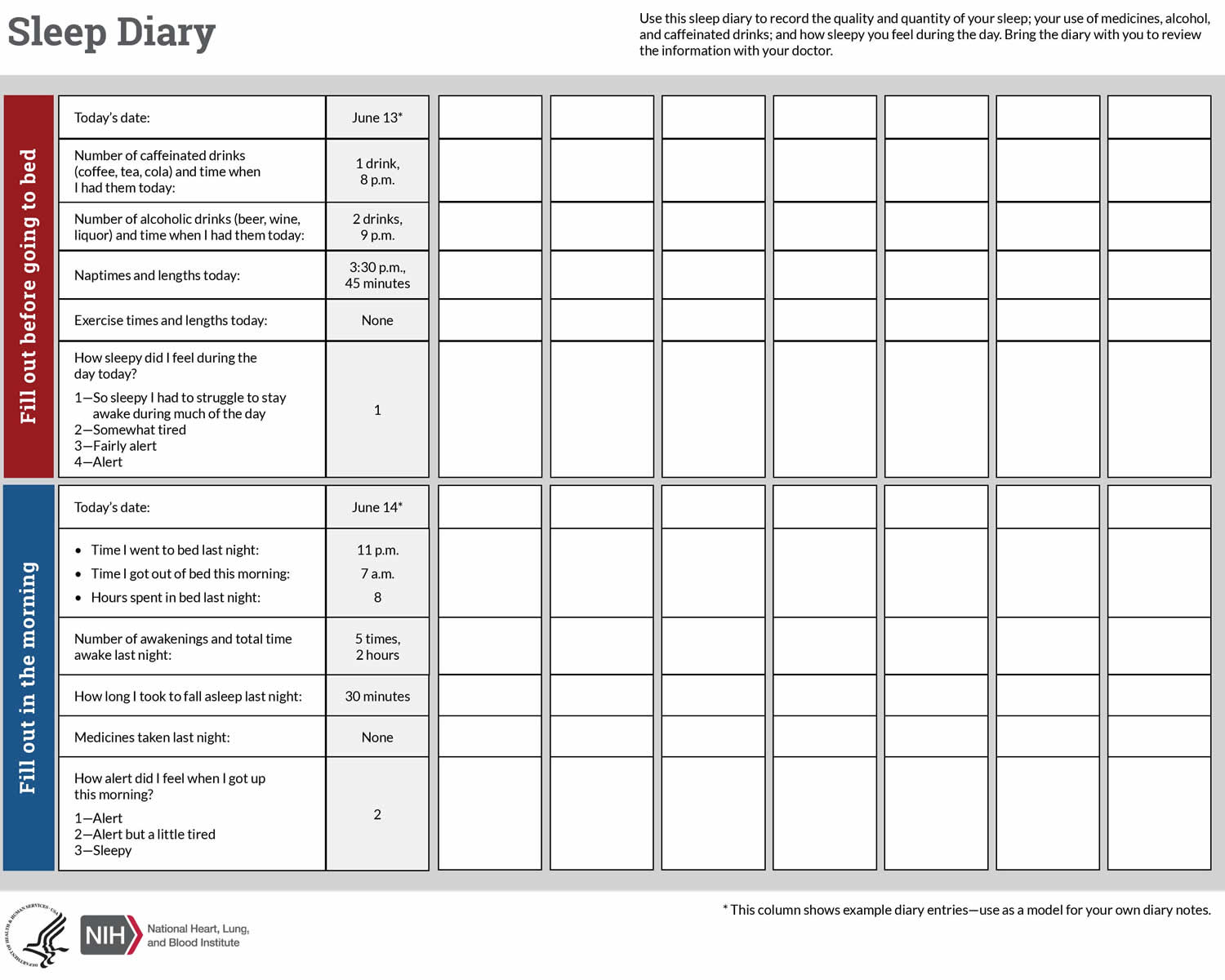
Bad sleep habits and long-term sleep loss will affect your health. If you’re worried about whether you’re getting enough sleep, try using a sleep diary for a couple of weeks.
Sleeping when your body is ready to sleep also is very important. Sleep deficiency can affect people even when they sleep the total number of hours recommended for their age group.
For example, people whose sleep is out of sync with their body clocks (such as shift workers) or routinely interrupted (such as caregivers or emergency responders) might need to pay special attention to their sleep needs.
If your job or daily routine limits your ability to get enough sleep or sleep at the right times, talk with your doctor. You also should talk with your doctor if you sleep more than 8 hours a night, but don’t feel well rested. You may have a sleep disorder or other health problem.
What influences the quality and length of sleep?
Since sleep and wakefulness are influenced by different neurotransmitter signals in the brain, foods and medicines that change the balance of these signals affect whether you feel alert or drowsy and how well you sleep. Caffeinated drinks such as coffee and drugs such as diet pills and decongestants stimulate some parts of the brain and can cause insomnia, or an inability to sleep. Many antidepressants suppress REM sleep. Heavy smokers often sleep very lightly and have reduced amounts of REM sleep. They also tend to wake up after 3 or 4 hours of sleep due to nicotine withdrawal. Many people who suffer from insomnia try to solve the problem with alcohol – the so-called night cap. While alcohol does help people fall into light sleep, it also robs them of REM and the deeper, more restorative stages of sleep. Instead, it keeps them in the lighter stages of sleep, from which they can be awakened easily.
People lose some of the ability to regulate their body temperature during REM, so abnormally hot or cold temperatures in the environment can disrupt this stage of sleep. If your REM sleep is disrupted one night, your body don’t follow the normal sleep cycle progression the next time you doze off. Instead, you often slip directly into REM sleep and go through extended periods of REM until you “catch up” on this stage of sleep.
People who are under anesthesia or in a coma are often said to be asleep. However, people in these conditions cannot be awakened and do not produce the complex, active brain wave patterns seen in normal sleep. Instead, their brain waves are very slow and weak, sometimes all but undetectable.
TIP: Having a comfortable bedroom and mattress are also important for facilitating good sleep. Have a quiet bedroom. Mattresses and beds should be comfortable for you and your bed partner. There are a lot of changes you can make to help you get better sleep.
Top 10 Sleep Myths
- Myth 1: Sleep is a time when your body and brain shut down for rest and relaxation.
No evidence shows that any major organ (including the brain) or regulatory system in the body shuts down during sleep. Some physiological processes actually become more active while you sleep. For example, secretion of certain hormones is boosted, and activity of the pathways in the brain linked to learning and memory increases.
- Myth 2: Getting just 1 hour less sleep per night than needed will not have any effect on your daytime functioning.
This lack of sleep may not make you noticeably sleepy during the day. But even slightly less sleep can affect your ability to think properly and respond quickly, and it can impair your cardiovascular health and energy balance as well as your body’s ability to fight infections, particularly if lack of sleep continues. If you consistently do not get enough sleep, a sleep debt builds up that you can never repay. This sleep debt affects your health and quality of life and makes you feel tired during the day.
- Myth 3: Your body adjusts quickly to different sleep schedules.
Your biological clock makes you most alert during the daytime and least alert at night. Thus, even if you work the night shift, you will naturally feel sleepy when nighttime comes. Most people can reset their biological clock, but only by appropriately timed cues—and even then, by 1–2 hours per day at best. Consequently, it can take more than a week to adjust to a substantial change in your sleep–wake cycle—for example, when traveling across several time zones or switching from working the day shift to the night shift.
- Myth 4: People need less sleep as they get older.
Older people don’t need less sleep, but they may get less sleep or find their sleep less refreshing. That’s because as people age, the quality of their sleep changes. Older people are also more likely to have insomnia or other medical conditions that disrupt their sleep.
- Myth 5: Extra sleep for one night can cure you of problems with excessive daytime fatigue.
Not only is the quantity of sleep important, but also the quality of sleep. Some people sleep 8 or 9 hours a night but don’t feel well rested when they wake up because the quality of their sleep is poor. A number of sleep disorders and other medical conditions affect the quality of sleep. Sleeping more won’t lessen the daytime sleepiness these disorders or conditions cause. However, many of these disorders or conditions can be treated effectively with changes in behavior or with medical therapies. Additionally, one night of increased sleep may not correct multiple nights of inadequate sleep.
- Myth 6: You can make up for lost sleep during the week by sleeping more on the weekends.
Although this sleeping pattern will help you feel more rested, it will not completely make up for the lack of sleep or correct your sleep debt. This pattern also will not necessarily make up for impaired performance during the week or the physical problems that can result from not sleeping enough. Furthermore, sleeping later on the weekends can affect your biological clock, making it much harder to go to sleep at the right time on Sunday nights and get up early on Monday mornings.
- Myth 7: Naps are a waste of time.
Although naps are no substitute for a good night’s sleep, they can be restorative and help counter some of the effects of not getting enough sleep at night. Naps can actually help you learn how to do certain tasks quicker. But avoid taking naps later than 3 p.m., particularly if you have trouble falling asleep at night, as late naps can make it harder for you to fall asleep when you go to bed. Also, limit your naps to no longer than 20 minutes, because longer naps will make it harder to wake up and get back in the swing of things. If you take more than one or two planned or unplanned naps during the day, you may have a sleep disorder that should be treated.
- Myth 8: Snoring is a normal part of sleep.
Snoring during sleep is common, particularly as a person gets older. Evidence is growing that snoring on a regular basis can make you sleepy during the day and increase your risk for diabetes and heart disease. In addition, some studies link frequent snoring to problem behavior and poorer school achievement in children. Loud, frequent snoring also can be a sign of sleep apnea, a serious sleep disorder that should be evaluated and treated.
- Myth 9: Children who don’t get enough sleep at night will show signs of sleepiness during the day.
Unlike adults, children who don’t get enough sleep at night typically become hyperactive, irritable, and inattentive during the day. They also have increased risk of injury and more behavior problems, and their growth rate may be impaired. Sleep debt appears to be quite common during childhood and may be misdiagnosed as attention-deficit hyperactivity disorder.
- Myth 10: The main cause of insomnia is worry.
Although worry or stress can cause a short bout of insomnia, a persistent inability to fall asleep or stay asleep at night can be caused by a number of other factors. Certain medications and sleep disorders can keep you up at night. Other common causes of insomnia are depression, anxiety disorders, and asthma, arthritis, or other medical conditions with symptoms that tend to be troublesome at night. Some people who have chronic insomnia also appear to be more “revved up” than normal, so it is harder for them to fall asleep.
What is sleep?
Sleep can be defined as a temporary state of unconsciousness from which (in contrast to coma) one can awaken when stimulated. Sleep is an active state of unconsciousness produced by the body where the brain is in a relative state of rest and is reactive primarily to internal stimulus 11. Sleep is one of many bodily functions that occur in cycles called circadian rhythms, so named because they are marked by events that reoccur at intervals of about 24 hours. Sleep is characterized by a stereotyped posture (usually lying down with the eyes closed) and inhibition of muscular activity (sleep paralysis). It superficially resembles other states of prolonged unconsciousness such as coma and animal hibernation, except that individuals cannot be aroused from those states by sensory stimulation.
However, the exact purpose of sleep has not been fully elucidated 11. There are several prominent theories currently which have explored the brain and attempt to identify a purpose for why you sleep which includes the Inactivity theory, Energy conservation theory, Restoration theory, and the Brain plasticity theory.
Inactivity theory is based on the concept of evolutionary pressure where creatures that were inactive at night were less likely to die from the predation of injury in the dark, thus creating an evolutionary and reproductive benefit to be inactive at night.
Energy conservation theory posits that the main function of sleep is to reduce a person’s energy demand during part of the day and night when it is least efficient to hunt for food. This theory is supported by the fact that the body has decreased metabolism of up to 10% during sleep.
The restorative theory states that sleep allows for the body to repair and replete cellular components necessary for biological functions that become depleted throughout an awake day. This is backed by the findings many functions in the body such as muscle repair, tissue growth, protein synthesis, and release of many of the important hormones for growth occur primarily during sleep.
Brain plasticity theory is that sleep is necessary for neural reorganization and growth of the brain’s structure and function. It is clear that sleep plays a role in the development of the brain in infants and children and explains why it is necessary that infants sleep upwards of 14 hours per day.
These theories are not exhaustive or all-inclusive of the prevalent ideas; rather, they serve to frame the concept that scientists do not fully understand sleep yet. It is more accepted that no single theory explains it all, and a combination of these ideas is more likely to hold the key to sleep 11.
Although sleep is essential to the normal functioning of the body, the exact functions of sleep are still unclear. Studies have shown that sleep deprivation impairs attention, memory, performance, and immunity; if the lack of sleep lasts long enough, it can lead to mood swings, hallucinations, and even death.
There has been considerable debate in the scientific community about the importance of sleep, but some proposed functions of sleep are widely accepted:
- Restoration, providing time for the body to repair itself;
- Consolidation of memories;
- Enhancement of immune system function; and
- Maturation of the brain.
Sleep deprivation impairs attention, learning, and performance.
Nerve-signaling chemicals called neurotransmitters control whether you are asleep or awake by acting on different groups of nerve cells, or neurons, in your brain 12. Neurons in your brainstem, which connects your brain with your spinal cord, produce neurotransmitters such as serotonin and norepinephrine that keep some parts of your brain active while you are awake. Other neurons at the base of the brain begin signaling when you fall asleep. These neurons appear to “switch off” the signals that keep you awake. Research also suggests that a chemical called adenosine builds up in your blood while you are awake and causes drowsiness. This chemical gradually breaks down while you sleep 12.
A good night’s sleep is when you fall asleep quite easily, do not fully wake up during the night, do not wake up too early, and feel refreshed in the morning. Regularly having difficulty falling asleep or sleeping through the night is not normal for healthy people of any age. But not everyone needs the same amount of sleep, and quality of sleep is different in different phases of life.
Young children and older people sleep more lightly than adults and teenagers. The length of time spent in deep sleep phases changes over a person’s lifetime. Babies and toddlers need to sleep a lot more than older children and adults. By the time they reach the age of five, most children have the typical sleep patterns of an adult: they are awake during the day and then sleep through the night. The amount of time spent sleeping gradually decreases until the age of 80 12.
Sleep stages
During sleep, you usually pass through five phases of sleep: stages 1, 2, 3, 4, and REM (rapid eye movement) sleep 12. These sleep stages progress in a cycle from stage 1 to REM sleep, then the cycle starts over again with stage 1. You spend almost 50 percent of your total sleep time in stage 2 sleep, about 20 percent in REM sleep, and the remaining 30 percent in the other stages. The first two phases of light sleep make up about half of the total sleep cycle. Phases 3 and 4 are the deep sleep phases. You dream in phase 4. When this phase ends, you sleep more lightly again before a new full sleep cycle starts. Some people completely or partially wake up after the sleep cycle ends, while others stay asleep until morning. Total sleep time ends when you wake up and then stay awake and get up.
The first REM sleep period usually occurs about 70 to 90 minutes after you fall asleep. A complete sleep cycle takes 90 to 110 minutes on average. The first sleep cycles each night contain relatively short REM periods and long periods of deep sleep. As the night progresses, REM sleep periods increase in length while deep sleep decreases. By morning, people spend nearly all their sleep time in stages 1, 2, and REM.
People awakened after sleeping more than a few minutes are usually unable to recall the last few minutes before they fell asleep. This sleep-related form of amnesia is the reason people often forget telephone calls or conversations they’ve had in the middle of the night. It also explains why you often do not remember your alarms ringing in the morning if you go right back to sleep after turning them off.
Infants, by contrast, spend about half of their sleep time in REM sleep 13. The quality of your sleep is impacted by your sleep cycle through the various phases.
When measuring total sleep time, sleep is considered to start when you close your eyes to fall asleep. The period between first closing your eyes and entering phase or stage 1 is known as sleep onset.
Stage One Sleep
Stage 1 (phase 1) is very light sleep, where you are drifting in and out of consciousness and can be awakened easily. Your eyes move very slowly and muscle activity slows. People awakened from stage 1 sleep often remember fragmented visual images. Many also experience sudden muscle contractions called hypnic myoclonia or hypnic jerks, often preceded by a sensation of starting to fall. These sudden movements are similar to the “jump” you make when startled. Some people experience a sleep disorder known as Periodic Leg Movement during Sleep (PLMS) where they experience recurring leg movements movements.
Stage Two Sleep
When you enter stage 2 sleep, your eye movements stop and your brain waves (fluctuations of electrical activity that can be measured by electrodes) become slower but there are still short bursts of activity, with occasional bursts of rapid waves called sleep spindles.
Stage Three, Four and REM Sleep
In stage 3, extremely slow brain waves called delta waves begin to appear, interspersed with smaller, faster waves. By stage 4, the brain produces delta waves almost exclusively. It is very difficult to wake someone during stages 3 and 4, which together are called deep sleep. There is no eye movement or muscle activity. People awakened during deep sleep do not adjust immediately and often feel groggy and disoriented for several minutes after they wake up. Some children experience bedwetting, night terrors, or sleepwalking during deep sleep.
When you switch into REM sleep, your breathing becomes more rapid, irregular, and shallow, your eyes jerk rapidly in various directions, and your limb muscles become temporarily paralyzed during sleep. Your heart rate increases, your blood pressure rises, and males develop penile erections. When people awaken during REM sleep, they often describe bizarre and illogical tales – dreams.
Normal sleep cycles
Sleep cycles usually repeat every 90 to 110 minutes. Each cycle is made up of a sequence of different sleep phases.
Normal sleep consists of two components:
- Non-rapid eye movement (NREM) sleep and
- Rapid eye movement (REM) sleep.
REM is short for “rapid eye movement.” This name describes the quick eye movements that can be observed during deep sleep. When children and adults are in deep sleep their eyes move back and forth quickly but their eyelids remain closed. You only dream during the REM phases 12.
During rapid eye movement (REM) sleep, the eyes move rapidly back and forth under closed eyelids. REM sleep is also known as paradoxical sleep because electroencephalography (EEG) readings taken during this time show high-frequency, small amplitude waves, which are similar to those of a person who is awake. Surprisingly, neuronal activity is high during REM sleep—brain blood flow and oxygen use are actually higher during REM sleep than during intense mental or physical activity while awake!
In spite of this high amount of neuronal activity, it is even more difficult to awaken a person during REM sleep than during any of the stages of NREM sleep.
Rapid eye movement (REM) sleep is associated with several physiological changes. For example, heart rate, respiratory rate, and blood pressure increase during REM sleep. In addition, most somatic motor neurons are inhibited during REM sleep, which causes a significant decrease in muscle tone and even paralyzes the skeletal muscles. The main exceptions to this inhibition are those somatic motor neurons that govern breathing and eye movements. REM sleep is also the period when most dreaming occurs.
Brain imaging studies on people going through REM sleep reveal that there is increased activity in both the visual association area (which is involved in recognition of visual images) and limbic system (which plays a major role in generation of emotions) and decreased activity in the prefrontal cortex (which is concerned with reasoning). These studies help to explain why dreams during REM sleep are often full of vivid imagery, emotional responses, and situations that may be illogical or even bizarre. Erection of the penis and enlargement of the clitoris may also occur during REM sleep, even when dream content is not sexual. The presence of penile erections during REM sleep in a man with erectile dysfunction (inability to attain an erection while awake) indicates that his problem has a psychological, rather than a physical cause.
Several physiological changes occur during non-rapid eye movement (NREM) sleep. There are decreases in heart rate, respiratory rate, and blood pressure. Muscle tone also decreases, out only slightly. As a result, there is a moderate amount of muscle tone during NREM sleep, which allows the sleeping person to shift body positions while in bed.
Dreaming sometimes takes place during NREM sleep but only occasionally. However, most dreaming occurs during rapid eye movement (REM) sleep. When dreaming does occur during NREM sleep, the dreams are usually less vivid, less emotional, and more logical than REM dreams. Most nightmares, however, occur during NREM sleep.
Intervals of NREM and REM sleep alternate throughout the night. Initially, a person falls asleep by sequentially going through the stages of NREM sleep (from stage 1 to stage 4) in about 45 minutes. Then the person goes through the stages of NREM sleep in reverse order (from stage 4 to stage 1) in about the same amount of time before entering a period of REM sleep. Afterward, the person again descends through the stages of NREM sleep, and then ascends back through the stages of NREM sleep to enter another period of REM sleep. During a typical 8-hour sleep period, there are four or five of these NREM-to-REM cycles. The first episode of REM sleep lasts 10–20 minutes. REM periods, which occur approximately every 90 minutes, gradually lengthen, with the final one lasting about 50 minutes. In adults, REM sleep totals 90–120 minutes during a typical 8-hour sleep period. As a person ages, the average total time spent sleeping decreases, and the percentage of REM sleep declines. As much as 50% of an infant’s sleep is REM sleep, as opposed to 35% for 2-year-olds and 25% for adults.
Figure 1. Sleep stages and brain activity – one sleep cycle
Figure 2. Sleep stages and brain activity – 8 hour sleep cycle
Although we do not yet understand the function of REM sleep, the high percentage of REM sleep in infants and children is thought to be important for the maturation of the brain.
Different parts of the brain mediate NREM and REM sleep. NREM sleep is induced by NREM sleep centers in the hypothalamus and basal forebrain, whereas REM sleep is promoted by a REM sleep center in the pons and midbrain. Several lines of evidence suggest the existence of sleep-inducing chemicals in the brain. One apparent sleep-inducer is adenosine, which accumulates during periods of high usage of ATP (adenosine triphosphate) by the nervous system. Adenosine inhibits neurons of the RAS that participate in arousal. Adenosine binds to specific receptors, called A1 receptors and inhibits certain cholinergic (acetylcholine-releasing) neurons of the RAS that participate in arousal. Thus, activity in the RAS during sleep is low due to the inhibitory effect of adenosine.
Caffeine (in coffee or chocolate) and theophylline (in tea)—substances known for their ability to maintain wakefulness—bind to and block the A1 receptors, preventing adenosine from binding and inducing sleep.
Why is sleep important ?
Sleep plays a vital role in good health and well-being throughout your life. Getting enough quality sleep at the right times can help protect your mental health, physical health, quality of life, and safety 9.
The way you feel while you’re awake depends in part on what happens while you’re sleeping 9. During sleep, your body is working to support healthy brain function and maintain your physical health. In children and teens, sleep also helps support growth and development.
The damage from sleep deficiency can occur in an instant (such as a car crash), or it can harm you over time. For example, ongoing sleep deficiency can raise your risk for some chronic health problems. It also can affect how well you think, react, work, learn, and get along with others.
Healthy Brain Function and Emotional Well-Being
Sleep helps your brain work properly. While you’re sleeping, your brain is preparing for the next day. It’s forming new pathways to help you learn and remember information.
Studies show that a good night’s sleep improves learning 9. Whether you’re learning math, how to play the piano, how to perfect your golf swing, or how to drive a car, sleep helps enhance your learning and problem-solving skills. Sleep also helps you pay attention, make decisions, and be creative.
Studies also show that sleep deficiency alters activity in some parts of the brain. If you’re sleep deficient, you may have trouble making decisions, solving problems, controlling your emotions and behavior, and coping with change. Sleep deficiency also has been linked to depression, suicide, and risk-taking behavior 9.
Children and teens who are sleep deficient may have problems getting along with others. They may feel angry and impulsive, have mood swings, feel sad or depressed, or lack motivation. They also may have problems paying attention, and they may get lower grades and feel stressed 9.
Physical Health
Sleep plays an important role in your physical health. For example, sleep is involved in healing and repair of your heart and blood vessels. Ongoing sleep deficiency is linked to an increased risk of heart disease, kidney disease, high blood pressure, diabetes, and stroke 9.
A lack of sleep also puts your body under stress and may trigger the release of more adrenaline, cortisol, and other stress hormones during the day. These hormones keep your blood pressure from dipping during sleep, which increases your risk for heart disease. Lack of sleep also may trigger your body to produce more of certain proteins thought to play a role in heart disease. For example, some studies find that people who repeatedly don’t get enough sleep have higher than normal blood levels of C-reactive protein, a sign of inflammation. High levels of this protein may indicate an increased risk for a condition called atherosclerosis, or hardening of the arteries.
Sleep deficiency also increases the risk of obesity. For example, one study of teenagers showed that with each hour of sleep lost, the odds of becoming obese went up. Sleep deficiency increases the risk of obesity in other age groups as well 9.
Sleep helps maintain a healthy balance of the hormones that make you feel hungry (ghrelin) or full (leptin) 9. When you don’t get enough sleep, your level of ghrelin goes up and your level of leptin goes down. This makes you feel hungrier than when you’re well-rested 9.
Evidence is growing that sleep is a powerful regulator of appetite, energy use, and weight control. During sleep, the body’s production of the appetite suppressor leptin increases and the appetite stimulant grehlin decreases. Studies find that the less people sleep, the more likely they are to be overweight or obese and prefer eating foods that are higher in calories and carbohydrates. People who report an average total sleep time of 5 hours a night, for example, are much more likely to become obese, compared with people who sleep 7–8 hours a night.
Sleep also affects how your body reacts to insulin, the hormone that controls your blood glucose (sugar) level. Sleep deficiency results in a higher than normal blood sugar level, which may increase your risk for diabetes 9. One study found that, when healthy young men slept only 4 hours a night for 6 nights in a row, their insulin and blood sugar levels matched those seen in people who were developing diabetes. Another study found that women who slept less than 7 hours a night were more likely to develop diabetes over time than those who slept between 7 and 8 hours a night.
Sleep also supports healthy growth and development 9. Deep sleep triggers the body to release the hormone that promotes normal growth in children and teens. This hormone also boosts muscle mass and helps repair cells and tissues in children, teens, and adults. Sleep also plays a role in puberty and fertility.
Your immune system relies on sleep to stay healthy 9. This system defends your body against foreign or harmful substances. Ongoing sleep deficiency can change the way in which your immune system responds. For example, if you’re sleep deficient, you may have trouble fighting common infections.
During sleep, your body creates more cytokines—cellular hormones that help the immune system fight various infections. Lack of sleep can reduce your body’s ability to fight off common infections. Research also reveals that a lack of sleep can reduce the body’s response to the flu vaccine. For example, sleep-deprived volunteers given the flu vaccine produced less than half as many flu antibodies as those who were well rested and given the same vaccine.
Daytime Performance and Safety
Getting enough quality sleep at the right times helps you function well throughout the day. People who are sleep deficient are less productive at work and school 9. They take longer to finish tasks, have a slower reaction time, and make more mistakes.
After several nights of losing sleep—even a loss of just 1–2 hours per night—your ability to function suffers as if you haven’t slept at all for a day or two.
Lack of sleep also may lead to microsleep 9. Microsleep refers to brief moments of sleep that occur when you’re normally awake.
You can’t control microsleep and you might not be aware of it 9. For example, have you ever driven somewhere and then not remembered part of the trip ? If so, you may have experienced microsleep.
Even if you’re not driving, microsleep can affect how you function. If you’re listening to a lecture, for example, you might miss some of the information or feel like you don’t understand the point. In reality, though, you may have slept through part of the lecture and not been aware of it.
Some people aren’t aware of the risks of sleep deficiency. In fact, they may not even realize that they’re sleep deficient. Even with limited or poor-quality sleep, they may still think that they can function well.
Several studies show that lack of sleep causes thinking processes to slow down. Lack of sleep also makes it harder to focus and pay attention. Lack of sleep can make you more easily confused. Studies also find that a lack of sleep leads to faulty decision making and more risk taking. A lack of sleep slows down your reaction time, which is particularly important to driving and other tasks that require quick response. When people who lack sleep are tested on a driving simulator, they perform just as poorly as people who are drunk.
For example, drowsy drivers may feel capable of driving. Yet, studies show that sleep deficiency harms your driving ability as much as, or more than, being drunk. It’s estimated that driver sleepiness is a factor in about 100,000 car accidents each year, resulting in about 1,500 deaths 9.
Drivers aren’t the only ones affected by sleep deficiency. It can affect people in all lines of work, including health care workers, pilots, students, lawyers, mechanics, and assembly line workers.
As a result, sleep deficiency is not only harmful on a personal level, but it also can cause large-scale damage. For example, sleep deficiency has played a role in human errors linked to tragic accidents, such as nuclear reactor meltdowns, grounding of large ships, and aviation accidents.
Lack of sleep causes
Common causes of sleep deprivation:
- Sleep disorders that reduce sleep time like insomnia, sleep apnea, restless legs syndrome, and others.
- Inadequate sleep hygiene.
- Sleep disorders that interfere with the brain’s ability to stay awake, including narcolepsy and primary hypersomnia.
- Insufficient total sleep time.
- Distractions during sleep from a bed partner. There is data to suggest that bed partner snoring can cause disruption to sleep. (A snoring mouthpiece could stop the snore sounds.)
Excessive daytime sleepiness causes
Excessive daytime sleepiness can occur secondary to sleep deprivation, medication effects, illicit substance use, obstructive sleep apnea (OSA), and other medical and psychiatric conditions 14. Excessive sleepiness caused by a primary hypersomnia of central origin (e.g., narcolepsy, idiopathic hypersomnia) is less common.
Common causes of excessive daytime sleepiness:
- Primary hypersomnias of central origin
- Narcolepsy (0.02 to 0.18 percent of population)
- Idiopathic hypersomnia (10 percent of patients with suspected narcolepsy)
- Other rare primary hypersomnias (example: Kleine-Levin syndrome)
- Secondary hypersomnias
- Sleep disorders
- Sleep-related breathing disorders
- Excessive daytime sleepiness secondary to obstructive sleep apnea (general population prevalence is 2 percent of women and 4 percent of men)
- Behavioral sleep deprivation
- Especially common in adolescents and shift workers
- Other sleep disorders: Includes circadian rhythm sleep disorders, sleep-related movement disorders
- Sleep disorders
- Medical or psychiatric conditions
- Medication effects: Includes prescription, nonprescription, and drugs of abuse
- Psychiatric conditions: Especially depression
- Medical conditions: Includes head trauma, stroke, cancer, inflammatory conditions, encephalitis, neurodegenerative conditions
Hypersomnia due to secondary causes is much more common than primary hypersomnia 14.
Sleep disorders
At least 40 million Americans each year suffer from chronic, long-term sleep disorders each year, and an additional 20 million experience occasional sleeping problems. These disorders and the resulting sleep deprivation interfere with work, driving, and social activities. They also account for an estimated $16 billion in medical costs each year, while the indirect costs due to lost productivity and other factors are probably much greater. Doctors have described more than 70 sleep disorders, most of which can be managed effectively once they are correctly diagnosed. The most common sleep disorders include insomnia, sleep apnea, restless legs syndrome, and narcolepsy.
Insomnia
Almost everyone occasionally suffers from short-term insomnia. This problem can result from stress, jet lag and other circadian rhythm problems, diet, or many other factors. Insomnia almost always affects job performance and well-being the next day. About 60 million Americans a year have insomnia frequently or for extended periods of time, which leads to even more serious sleep deficits. Insomnia tends to increase with age and affects about 40 percent of women and 30 percent of men. It is often the major disabling symptom of an underlying medical disorder.
For short-term insomnia, doctors may prescribe sleeping pills. Most sleeping pills stop working after several weeks of nightly use, however, and long-term use can actually interfere with good sleep. Mild insomnia often can be prevented or cured by practicing good sleep habits . For more serious cases of insomnia, researchers are experimenting with light therapy and other ways to alter circadian cycles.
Sleep Apnea
Sleep apnea is a disorder of interrupted breathing during sleep. It usually occurs in association with fat buildup or loss of muscle tone with aging. These changes allow the windpipe to collapse during breathing when muscles relax during sleep. This problem, called obstructive sleep apnea, is usually associated with loud snoring (though not everyone who snores has this disorder). Sleep apnea also can occur if the neurons that control breathing malfunction during sleep.
During an episode of obstructive sleep apnea, the person’s effort to inhale air creates suction that collapses the windpipe. This blocks the air flow for 10 seconds to a minute while the sleeping person struggles to breathe. When the person’s blood oxygen level falls, the brain responds by awakening the person enough to tighten the upper airway muscles and open the windpipe. The person may snort or gasp, then resume snoring. This cycle may be repeated hundreds of times a night. The frequent awakenings that sleep apnea patients experience leave them continually sleepy and may lead to personality changes such as irritability or depression. Sleep apnea also deprives the person of oxygen, which can lead to morning headaches, a loss of interest in sex, or a decline in mental functioning. It also is linked to high blood pressure, irregular heartbeats, and an increased risk of heart attacks and stroke. Patients with severe, untreated sleep apnea are two to three times more likely to have automobile accidents than the general population. In some high-risk individuals, sleep apnea may even lead to sudden death from respiratory arrest during sleep.
An estimated 18 million Americans have sleep apnea. However, few of them have had the problem diagnosed. Patients with the typical features of sleep apnea, such as loud snoring, obesity, and excessive daytime sleepiness, should be referred to a specialized sleep center that can perform a sleep study test called polysomnography. This test records the patient’s brain waves, heartbeat, and breathing during an entire night. If sleep apnea is diagnosed, several treatments are available. Mild sleep apnea frequently can be overcome through weight loss or by preventing the person from sleeping on his or her back. Other people may need special devices or surgery to correct the obstruction. People with sleep apnea should never take sedatives or sleeping pills, which can prevent them from awakening enough to breathe.
Restless Legs Syndrome
Restless legs syndrome (RLS), a familial disorder causing unpleasant crawling, prickling, or tingling sensations in the legs and feet and an urge to move them for relief, is emerging as one of the most common sleep disorders, especially among older people. This disorder, which affects as many as 12 million Americans, leads to constant leg movement during the day and insomnia at night. Severe Restless Legs Syndrome is most common in elderly people, though symptoms may develop at any age. In some cases, it may be linked to other conditions such as anemia, pregnancy, or diabetes.
Many Restless Legs Syndrome patients also have a disorder known as periodic limb movement disorder or, PLMD, which causes repetitive jerking movements of the limbs, especially the legs. These movements occur every 20 to 40 seconds and cause repeated awakening and severely fragmented sleep. In one study, Restless Legs Syndrome and periodic limb movement disorder accounted for a third of the insomnia seen in patients older than age 60.
Restless Legs Syndrome and periodic limb movement disorder often can be relieved by drugs that affect the neurotransmitter dopamine, suggesting that dopamine abnormalities underlie these disorders’ symptoms. Learning how these disorders occur may lead to better therapies in the future.
Narcolepsy
Narcolepsy affects an estimated 250,000 Americans. People with narcolepsy have frequent “sleep attacks” at various times of the day, even if they have had a normal amount of night-time sleep. These attacks last from several seconds to more than 30 minutes. People with narcolepsy also may experience cataplexy (loss of muscle control during emotional situations), hallucinations, temporary paralysis when they awaken, and disrupted night-time sleep. These symptoms seem to be features of REM sleep that appear during waking, which suggests that narcolepsy is a disorder of sleep regulation. The symptoms of narcolepsy typically appear during adolescence, though it often takes years to obtain a correct diagnosis. The disorder (or at least a predisposition to it) is usually hereditary, but it occasionally is linked to brain damage from a head injury or neurological disease.
Once narcolepsy is diagnosed, stimulants, antidepressants, or other drugs can help control the symptoms and prevent the embarrassing and dangerous effects of falling asleep at improper times. Naps at certain times of the day also may reduce the excessive daytime sleepiness.
In 1999, a research team working with canine models identified a gene that causes narcolepsy–a breakthrough that brings a cure for this disabling condition within reach. The gene, hypocretin receptor 2, codes for a protein that allows brain cells to receive instructions from other cells. The defective versions of the gene encode proteins that cannot recognize these messages, perhaps cutting the cells off from messages that promote wakefulness. The researchers know that the same gene exists in humans, and they are currently searching for defective versions in people with narcolepsy.
Who is at risk for sleep deprivation and deficiency ?
Sleep deficiency, which includes sleep deprivation, affects people of all ages, races, and ethnicities. Certain groups of people may be more likely to be sleep deficient. Examples include people who:
- Have limited time available for sleep, such as caregivers or people working long hours or more than one job
- Have schedules that conflict with their internal body clocks, such as shift workers, first responders, teens who have early school schedules, or people who must travel for work
- Make lifestyle choices that prevent them from getting enough sleep, such as taking medicine to stay awake, abusing alcohol or drugs, or not leaving enough time for sleep
- Have undiagnosed or untreated medical problems, such as stress, anxiety, or sleep disorders
- Have medical conditions or take medicines that interfere with sleep
Certain medical conditions have been linked to sleep disorders. These conditions include heart failure, heart disease, obesity, diabetes, high blood pressure, stroke or transient ischemic attack (mini-stroke), depression, and attention-deficit hyperactivity disorder (ADHD).
If you have or have had one of these conditions, ask your doctor whether you might benefit from a sleep study.
A sleep study allows your doctor to measure how much and how well you sleep. It also helps show whether you have sleep problems and how severe they are.
If you have a child who is overweight, talk with the doctor about your child’s sleep habits.
Sleep deprivation effects
Lack of sleep side effects:
- Excessive daytime sleepiness
- Accidents from lack of attention
- Moodiness
- Hunger
- Other health dangers listed below
Side effects of sleep deprivation
Diabetes
It’s now believed that people who experience short-term sleep restriction are not able to process glucose as efficiently as those who get eight hours of sleep; which means that they have an increased likelihood of developing type 2 diabetes. A study of more than 1400 participants conducted in 2005 showed that people who habitually slept for only a few hours were more prone to experience symptoms of type 2 diabetes.
Sleep deprivation ages you quicker
A study done by UCLA researchers discovered that just a single night of insufficient sleep can make an older adults’ cells age quicker 15. This might not seem like a big deal, but it has the potential to bring on a lot of other diseases. Multiple sclerosis, heart disease and cancer are just a few of them 16.
The UCLA study results show that one night of partial sleep deprivation activates gene expression patterns in peripheral blood mononuclear cells (PBMCs) consistent with increasing accumulation of damage that initiates cell cycle arrest and increases susceptibility to senescence 15. These findings causally link sleep deprivation to the etiology of biological aging, and further supports the hypothesis that sleep deprivation may be associated with elevated disease risk because it promotes molecular processes involved in biological aging.
Insufficient sleep means that you get less than the 7 hours of nightly sleep that the American Academy of Sleep Medicine recommends for adults. People in the study were allowed only four hours of sleep from 3 a.m. to 7 a.m. This type of sleep restriction is actually the most common form of sleep deprivation 15. Long work hours may prevent you from getting the sleep you need. Or you simply stay up too late at night, failing to make sleep a top priority.
Getting a healthy night’s sleep isn’t just a way to keep the wrinkles away for a little longer — it will actually make you healthier.
Life Length
Again, many studies have been completed on the relation to longevity to sleep. Professor Kevin Morgan from Loughborough University’s sleep research team says that “those that sleep 7-9 hours live longer than those who sleep shorter or even longer” 17. You are 12% more likely to die over a 25 year period if you are not getting enough or too much sleep.
Healing and Sleep
In the year 2005, a study was conducted on a group of rats: for five days the rats were deprived of REM sleep and, compared to a group of rats which were not deprived of ‘dream’ sleep, the results showed no significant changes in their wound-healing ability. These rats were allowed NREM (deep) sleep.
Sleep’s impact on the immune system
Neurons that control sleep interact closely with the immune system. As anyone who has had the flu knows, infectious diseases tend to make us feel sleepy. This probably happens because cytokines,chemicals our immune systems produce while fighting an infection, are powerful sleep-inducing chemicals. Sleep may help the body conserve energy and other resources that the immune system needs to mount an attack.
The Brain
Scientists now know that sleep deprivation adversely affects the brain and cognitive function. A study completed by the VAHS in San Diego and the UCSD School of Medicine in the year 2000 monitored activity in the brains of sleep-deprived people whilst they performed basic verbal learning tasks by using functional magnetic resonance imaging (fMRI).
The results of the study showed that, in sleepier subjects, more activity was found in certain areas of the prefrontal cortex of the brain: The prefrontal cortex is an area of the brain that supports such mental faculties as logical and practical (‘means-ends’) reasoning and working memory. These results were interpreted by the researchers as indicating that, in order to complete a specific task, the average non-sleep-deprived subject’s brain needed to exert a lot more effort than the brain of an average non-sleep deprived person. They were able to infer from these results that the brains of sleep-deprived people were trying to compensate for the adverse effects created by sleep deprivation.
Growth
A survey conducted in 1999 revealed that sleep deprivation caused reduced cortisol secretion the following day – the result of increased slow-wave sleep. It was also revealed that, whilst suppressing growth hormones, sleep deprivation enhanced activity on the hypothalamus-pituitary-adrenal axis: this is the regulator of body functions such as the immune system, digestion, sex, mood, or energy usage; in addition to controlling reactions to stress. This study supports the findings of previous studies where adrenal insufficiency was observed in idiopathic hypersomnia.
Working Memory and Attention
Besides the many physical consequences of insufficient sleep, perhaps the most important consequences of sleep deprivation are deficits in working memory and attention. Lapses in ordinary mundane routines can cause worrying results; from missing words or sentences while taking notes to omitting important ingredients while cooking. It appears that carrying out tasks that require attention is in direct correlation to the number of hours the person sleeps each night; with these functions declining with the number hours of sleep deprivation. Methods such as choice-reaction time tasks are used to test working memory. Sadly, these attentional lapses can move into critical domains whereby the consequences could well result in life or death: industrial accidents and car crashes can be the result of inattentiveness, directly attributable to sleep deprivation.
Researchers typically use the (PVT) psychomotor vigilance task in order to measure the magnitude of attention deficits: this simply requires the patient to press a button at pseudo-random intervals in response to a light. An error is recorded when the patient fails to press the button in response to the light (stimulus), and this is noted as being attributable to the micro-sleeps occurring due to sleep deprivation.
The Heart
This statistic is overwhelming, but the University of Warwick did a study and they found that getting less than 6 hours of sleep on a continuous basis makes you 48% more likely to die of heart disease and 15% more likely in developing a stroke. Professor Cappuccio, co-author of the study, said “the trend for late nights and early mornings is like a ticking time bomb for your health”.
If you are over 65, you are 83% more likely to have high blood pressure which increases the risk of heart attack and stroke.
Sleep deprivation signs and symptoms
Lack of sleep can cause you to feel very tired during the day. You may not feel refreshed and alert when you wake up. Sleep deprivation also can interfere with work, school, driving, and social functioning.
How sleepy you feel during the day can help you figure out whether you’re having symptoms of problem sleepiness. You might be sleep deficient if you often feel like you could doze off while:
- Sitting and reading or watching TV
- Sitting still in a public place, such as a movie theater, meeting, or classroom
- Riding in a car for an hour without stopping
- Sitting and talking to someone
- Sitting quietly after lunch
- Sitting in traffic for a few minutes
When a patient has continuous muscular activity, but insufficient rest, scientists see other issues becoming more prevalent in sleep-deprived patients; such as cramping. Muscle fascia tears, hernias, and other problems usually associated with physical overexertion have been reported in extreme cases of sleep deprivation. At the extreme end of the scale, sleep deprivation can mimic psychosis, where distorted perceptions can lead to inappropriate behavioral and emotional responses 18.
Lack of sleep can cause problems with learning, focusing, and reacting. You may have trouble making decisions, solving problems, remembering things, controlling your emotions and behavior, and coping with change. You may take longer to finish tasks, have a slower reaction time, and make more mistakes.
The signs and symptoms of lack of sleep may differ between children and adults. Children who are sleep deficient might be overly active and have problems paying attention. They also might misbehave, and their school performance can suffer.
Sleep-deficient children may feel angry and impulsive, have mood swings, feel sad or depressed, or lack motivation.
You may not notice how lack of sleep affects your daily routine. A common myth is that people can learn to get by on little sleep with no negative effects. However, research shows that getting enough quality sleep at the right times is vital for mental health, physical health, quality of life, and safety.
To find out whether you’re sleep deficient, try keeping a sleep diary for a couple of weeks. Write down how much you sleep each night, how alert and rested you feel in the morning, and how sleepy you feel during the day.
Compare the amount of time you sleep each day with the average amount of sleep recommended for your age group, as shown in Table 1 above. If you often feel very sleepy, and efforts to increase your sleep don’t help, talk with your doctor.
Figure 3. Sleep diary
Depression
Interestingly, there have been studies that show sleep restriction might have potential when it comes to treating depression. Scientists know that people suffering from depression experience earlier incidences of REM sleep plus increased rapid eye movements; and monitoring a patient’s EEG and waking them during bouts of REM sleep appears to produce a therapeutic effect, thus alleviating symptoms of depression. When sleep deprived, up to 60% of patients show signs of immediate recovery; however, most relapse the next night. It’s believed that this effect is linked to increases in the brain-derived neurotrophic factor (BDNF). It’s also been shown that, in normal people, chronotype is related to the effect that sleep deprivation has on mood: following sleep deprivation, people who prefer mornings become more depressed, while those who prefer evenings show a marked improvement in their mood.
In 2014, a thorough evaluation of the human metabolome in sleep deprivation discovered that 27 metabolites are increased following 24 waking hours, with suggestions that tryptophan, serotonin, and taurine may be contributing to the antidepressive effect.
Weight Gain or Weight Loss
When rats were exposed to prolonged sleep deprivation the result was that both food intake and energy expenditure increased, resulting in a net weight loss, and ultimately leading to death. The hypothesis of this study is that when moderate chronic sleep debt goes hand-in-hand with habitual short sleep, energy expenditure and increased appetite are encouraged; and, in societies where high-calorie food is freely available the equation is tipped towards food intake rather than expenditure. Nationally representative samples used in several large studies suggest that one of the causes of the United States obesity problem could possibly be due to the corresponding decrease in the average number of hours that people sleep. If you do not believe sleep is all that important, but your weight is, then you are not helping your weight problem by not getting the proper sleep (7-9 hours).
These findings indicate that the hormones that regulate appetite and glucose metabolism could be disrupted because of sleep deprivation. It appears that the association between obesity and sleep deprivation is strongest in young and middle-age adults. The reasoning for weight gain is the longer you are awake the hungrier you will become. Your body needs energy to keep going and if you are staying up long hours, the more energy it will require. On the other hand, there are scientists who believe that related problems, such as sleep apnea, together with the physical discomfort of obesity, reduce a person’s likelihood of getting a good night’s sleep.
Sleep Problems and Mental Disorders
Sleeping problems occur in almost all people with mental disorders, including those with depression and schizophrenia. People with depression, for example, often awaken in the early hours of the morning and find themselves unable to get back to sleep. The amount of sleep a person gets also strongly influences the symptoms of mental disorders. Sleep deprivation is an effective therapy for people with certain types of depression, while it can actually cause depression in other people. Extreme sleep deprivation can lead to a seemingly psychotic state of paranoia and hallucinations in otherwise healthy people, and disrupted sleep can trigger episodes of mania (agitation and hyperactivity) in people with manic depression.
Sleeping problems are common in many other disorders as well, including Alzheimer’s disease, stroke, cancer, and head injury. These sleeping problems may arise from changes in the brain regions and neurotransmitters that control sleep, or from the drugs used to control symptoms of other disorders. In patients who are hospitalized or who receive round-the-clock care, treatment schedules or hospital routines also may disrupt sleep. The old joke about a patient being awakened by a nurse so he could take a sleeping pill contains a grain of truth. Once sleeping problems develop, they can add to a person’s impairment and cause confusion, frustration, or depression. Patients who are unable to sleep also notice pain more and may increase their requests for pain medication. Better management of sleeping problems in people who have other disorders could improve these patients’ health and quality of life.
Sleep deprivation diagnosis
Your health care provider may recommend a polysomnogram or other test to diagnose a sleep disorder. A polysomnogram typically involves spending the night at a sleep lab or sleep center. It records your breathing, oxygen levels, eye movements, muscle movement of chin and legs, nasal pressure and airflow, chest and thorax movement, and pulse oximetry, heart rate, and EEG (brain waves) throughout the night. Your sleep is also video and audio recorded. These tests are performed overnight and usually require a minimum of 6 hours of monitoring. The data can help a sleep specialist determine if you are reaching and proceeding properly through the various sleep stages. Results may be used to develop a treatment plan or determine if further tests are needed.
Figure 4. Electroencephalogram (EEG)
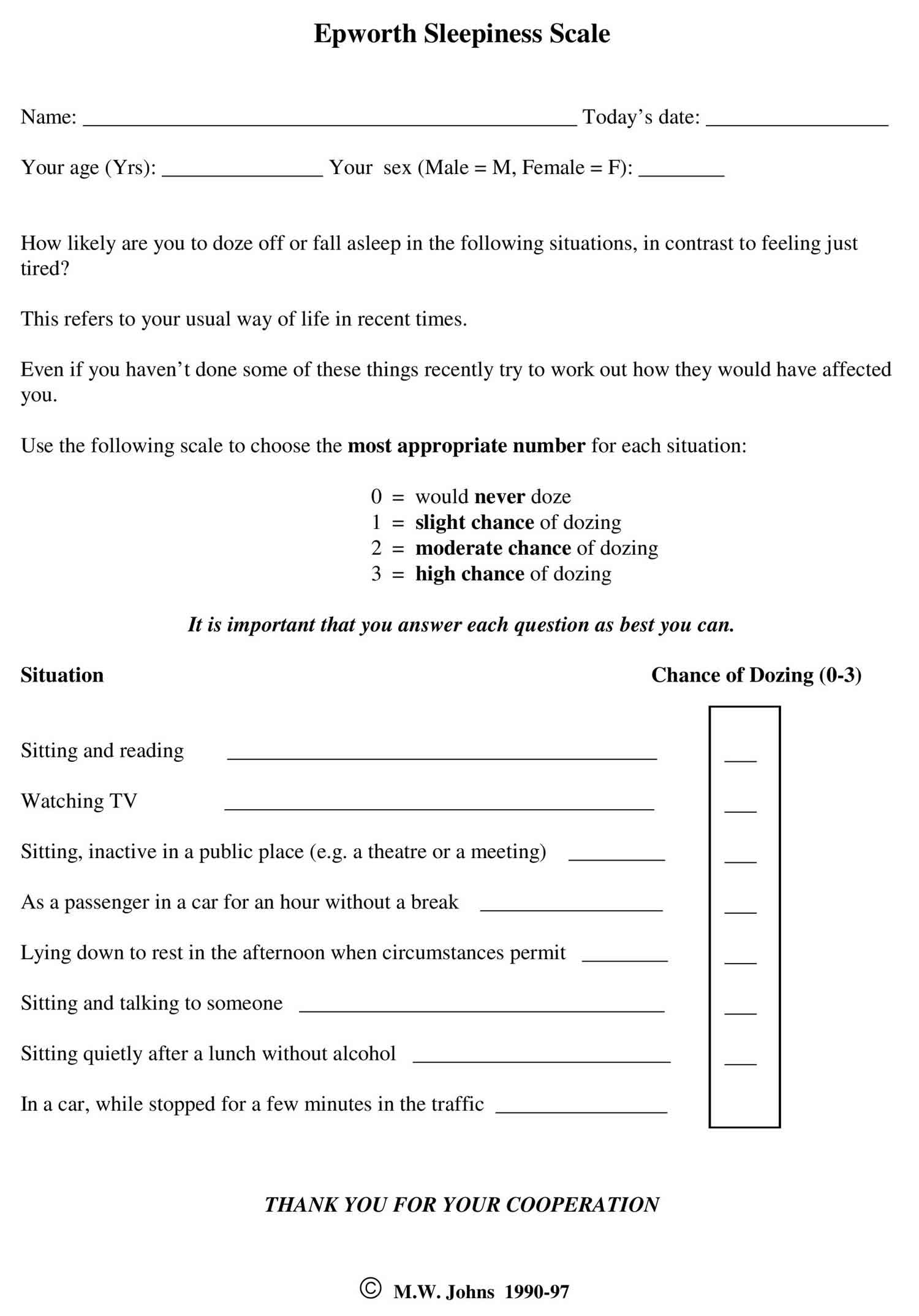
Epworth sleepiness scale
Epworth Sleepiness Scale (ESS) is a scale intended to measure ‘daytime sleepiness’ that is measured by use of a very short questionnaire. This can be helpful in diagnosing sleep disorders. Epworth Sleepiness Scale was introduced in 1991 by Dr Murray Johns of Epworth Hospital in Melbourne, Australia and subsequently modified it slightly in 1997.
Epworth Sleepiness Scale is a self-administered questionnaire with 8 questions. The questionnaire asks the subject to rate his or her probability of falling asleep on a scale of increasing probability from 0 to 3 (0 = no chance of dozing 1 = slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing) for eight different situations that most people engage in during their daily lives, though not necessarily every day. The scores for the eight questions are added together to obtain a single number. A number in the 0–9 range is considered to be normal while a number in the 10–24 range indicates that expert medical advice should be sought. For instance, scores of 11-15 are shown to indicate the possibility of mild to moderate sleep apnea, where a score of 16 and above indicates the possibility of severe sleep apnea or narcolepsy. Certain questions in the scale were shown to be better predictors of specific sleep disorders, though further tests may be required to provide an accurate diagnosis.
Figure 5. Epworth Sleepiness Scale (ESS)
Epworth Sleepiness Scale score
Epworth Sleepiness Scale is a scale intended to measure daytime sleepiness that is measured by use of a very short questionnaire. Epworth Sleepiness Scale can be helpful in diagnosing sleep disorders.
Sitting and reading
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Watching television
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Sitting, inactive in a public place (e.g. a theater or meeting)
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
As a passenger in a car for an hour without a break
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Lying down to rest in the afternoon when circumstances permit
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Sitting and talking to someone
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Sitting quietly after a lunch without alcohol
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
In a car, while stopped for a few minutes in the traffic
- 0 – no chance of dozing
- 1 – slight chance of dozing
- 2 – moderate chance of dozing
- 3 – high chance of dozing
Add up all the scores and write in the designated “total score box”.
Interpret the results as per the scale below.
- Score: 1- 6 = Enough Sleep
- Score: 7-8 = Tend to be sleepy during the day
- Score: 9- 15 = Very sleepy
- Score: 16+ = Dangerously sleepy
Your Score is less than 9 and in considered normal
Your Score is above 9 and its recommended that you should seek medical advice.
Epworth Sleepiness Scale interpretation
Epworth Sleepiness Scale is a self-administered questionnaire with 8 questions. Respondents are asked to rate, on a 0-3 scale (0 = no chance of dozing 1 = slight chance of dozing 2 = moderate chance of dozing 3 = high chance of dozing), their usual chances of dozing off or falling asleep while engaged in eight different activities. Most people engage in those activities at least occasionally, although not necessarily every day. The Epworth Sleepiness Scale score (the sum of 8 item scores, 0-3) can range from 0 to 24. The higher the Epworth Sleepiness Scale score, the higher that person’s average sleep propensity in daily life, or their ‘daytime sleepiness’. A number in the 0–9 range is considered to be normal while a number in the 10–24 range indicates that expert medical advice should be sought. For instance, scores of 11-15 are shown to indicate the possibility of mild to moderate sleep apnea, where a score of 16 and above indicates the possibility of severe sleep apnea or narcolepsy. Certain questions in the Epworth Sleepiness Scale were shown to be better predictors of specific sleep disorders, though further tests may be required to provide an accurate diagnosis.
Sleep deprivation treatment
The primary treatment of sleep deprivation is to increase total sleep time. Treating the cause of sleep deprivation is generally the solution to the problem. If a sleep disorder is interrupting sleep, the problem will need to be addressed in order to improve sleep duration and quality. Inadequate sleep hygiene or insufficient sleep is often a cause that needs to be addressed 19.
Many things can make sleeping difficult too, like alcohol, drugs and medication. Mental or physical illness can reduce your quality of sleep just as much as stress or working shifts at odd hours. Some people’s sleep is disturbed by nightly pauses in breathing (sleep apnea) or restless legs syndrome. Others wake up several times each night to go to the bathroom. During menopause many women find that their sleep is interrupted by hot flashes.
Grinding your teeth (bruxism), talking in your sleep or sleepwalking (somnambulism) can also affect how well you sleep. Nightmares can also make you wake with a start and influence how long and deeply you sleep. Jetlag is another factor that can really confuse your sleep-wake cycle for a while. Almost half of us snore. You often do not notice it yourself, but it can disturb others’ sleep.
Lack of sleep not only affects your quality of life. It can also be dangerous because it increases your chances of having accidents. This makes it important to find out the underlying cause if you are regularly sleeping poorly.
How to get better sleep at night
You can take steps to improve your sleep habits. First, make sure that you allow yourself enough time to sleep. With enough sleep each night, you may find that you’re happier and more productive during the day.
Sleep often is the first thing that busy people squeeze out of their schedules. Making time to sleep will help you protect your health and well-being now and in the future.
Getting enough sleep is good for your health. Here are a few tips to improve your sleep:
- Set a schedule. Go to bed and wake up at the same time every day. For children, have a set bedtime and a bedtime routine. Don’t use the child’s bedroom for timeouts or punishment.
- Try to keep the same sleep schedule on weeknights and weekends. Limit the difference to no more than about an hour. Staying up late and sleeping in late on weekends can disrupt your body clock’s sleep–wake rhythm.
- Use the hour before bed for quiet time. Avoid strenuous exercise and bright artificial light, such as from a TV or computer screen. The light may signal the brain that it’s time to be awake.
- Create a room for sleep – avoid bright lights and loud sounds, keep the room at a comfortable temperature, and don’t watch TV or have a computer in your bedroom.
- Avoid nicotine (for example, cigarettes) and caffeine (including caffeinated soda, coffee, tea, and chocolate). Nicotine and caffeine are stimulants, and both substances can interfere with sleep. The effects of caffeine can last as long as 8 hours. So, a cup of coffee in the late afternoon can make it hard for you to fall asleep at night.
- Avoid heavy and/or large meals within a couple hours of bedtime. (Having a light snack is okay.) Also, avoid alcoholic drinks before bed.
- Exercise 20 to 30 minutes a day but no later than a few hours before going to bed.
- Relax before bed – try a warm bath, reading, or another relaxing routine.
- Don’t lie in bed awake. If you can’t get to sleep, do something else, like reading or listening to music, until you feel tired.
- Spend time outside every day (when possible) and be physically active.
- Keep your bedroom quiet, cool, and dark (a dim night light is fine, if needed).
Napping during the day may provide a boost in alertness and performance. However, if you have trouble falling asleep at night, limit naps or take them earlier in the afternoon. Adults should nap for no more than 20 minutes.
Napping in preschool-aged children is normal and promotes healthy growth and development.
See a doctor if you have a problem sleeping or if you feel unusually tired during the day. Most sleep disorders can be treated effectively.
How to Sleep Better if You Are a Shift Worker
Some people have schedules that conflict with their internal body clocks. For example, shift workers and teens who have early school schedules may have trouble getting enough sleep. This can affect how they feel mentally, physically, and emotionally.
If you’re a shift worker, you may find it helpful to:
- Increase your total amount of sleep by adding naps and lengthening the amount of time you allot for sleep.
- Keep the lights bright at work
- Minimize the number of shift changes so that your body’s biological clock has a longer time to adjust to a nighttime work schedule.
- Limit caffeine use to the first part of your shift to promote alertness at night.
- Remove sound and light distractions in your bedroom during daytime sleep (for example, use light-blocking curtains)
If you’re still not able to fall asleep during the day or have problems adapting to a shift-work schedule, talk with your doctor about other options to help you sleep.
When possible, employers and schools might find it helpful to consider options to address issues related to sleep deficiency.
Here are some potentially life-saving tips for avoiding drowsy driving
- Be well rested before hitting the road. If you have several nights in a row of fewer than 7–8 hours of sleep, your reaction time slows. Restoring that reaction time to normal can take more than one night of good sleep, because a sleep debt accumulates after each night you lose sleep. It may take several nights of being well rested to repay that sleep debt and make you ready for driving on a long road trip.
- Avoid driving between midnight and 7 a.m. Unless you are accustomed to being awake then, this period of time is when we are naturally the least alert and most tired.
- Don’t drive alone. A companion who can keep you engaged in conversation might help you stay awake while driving.
- Schedule frequent breaks on long road trips. If you feel sleepy while driving, pull off the road and take a nap for 15–20 minutes.
- Don’t drink alcohol. Just one beer when you are sleep deprived will affect you as much as two or three beers when you are well rested.
- Don’t count on caffeine or other tricks. Although drinking a cola or a cup of coffee might help keep you awake for a short time, it won’t over come extreme sleepiness or relieve a sleep debt.
- Hershner SD, Chervin RD. Causes and Consequences of sleepiness among college students. Nat Sci Sleep. 2014;6:73–84.
- Sleep Deprivation: Symptoms, Causes, Treatments. https://www.sleepassociation.org/sleep-disorders/sleep-deprivation
- Dai XJ, Gong HH, Wang YX. Gender differences in brain regional homogeneity of healthy subjects after normal sleep and after sleep deprivation: a resting-state fMRI study. Sleep Med. 2012;13:720–27.
- Kaliyaperumal D, Elango Y, Alagesan M, Santhanakrishanan I. Effects of Sleep Deprivation on the Cognitive Performance of Nurses Working in Shift. J Clin Diagn Res. 2017;11(8):CC01–CC03. doi:10.7860/JCDR/2017/26029.10324 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5620757
- Drowsy Driving: Asleep at the Wheel. https://www.cdc.gov/features/dsdrowsydriving/
- Hanson JA, Huecker MR. Sleep Deprivation. [Updated 2019 Nov 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547676
- Stimpfel AW, Sloane DM, Aiken LH. The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Affairs. 2012;31(11):2501–09.
- Chang YS, Wu YH, Hsu CY, Tang SH, Yang LL, Su SF. Impairment of perceptual and motor abilities at the end of a night shift is greater in nurses working fast rotating shifts. Sleep Medicine. 2011;12(9):866–69.
- Why Is Sleep Important ? National Heart, Lung and Blood Institute. https://www.nhlbi.nih.gov/health/health-topics/topics/sdd/why
- Brain Basics: Understanding Sleep. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep
- Brinkman JE, Sharma S. Physiology, Sleep. [Updated 2018 Dec 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482512
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. What is “normal” sleep? 2013 Sep 18 [Updated 2016 Dec 30]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279322
- The process of falling asleep. Sleep Med Rev. 2001 Jun;5(3):247-270. DOI:10.1053/smrv.2001.0145 https://doi.org/10.1053/smrv.2001.0145
- American Academy of Sleep Medicine. The International Classification of Sleep Disorders: Diagnostic & Coding Manual. 2nd ed. Westchester, Ill.: American Academy of Sleep Medicine; 2005.
- Carroll JE, Cole SW, Seeman TE, et al. Partial sleep deprivation activates the DNA damage response (DDR) and the senescence-associated secretory phenotype (SASP) in aged adult humans. Brain Behav Immun. 2016;51:223–229. doi:10.1016/j.bbi.2015.08.024 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4679552
- Codd, V., Nelson, C., Albrecht, E. et al. Identification of seven loci affecting mean telomere length and their association with disease. Nat Genet 45, 422–427 (2013). https://doi.org/10.1038/ng.2528
- Sleep Matters. The impact of sleep on health and wellbeing Mental Health Awareness Week 2011 https://www.mentalhealth.org.uk/sites/default/files/MHF-Sleep-Report-2011.pdf
- Alhola P, Polo-Kantola P. Sleep deprivation: Impact on cognitive performance. Neuropsychiatr Dis Treat. 2007;3(5):553–567.
- Consequences of sleep deprivation. Int J Occup Med Environ Health. 2010;23(1):95-114. DOI 10.2478/v10001-010-0004-9