Spondylosis
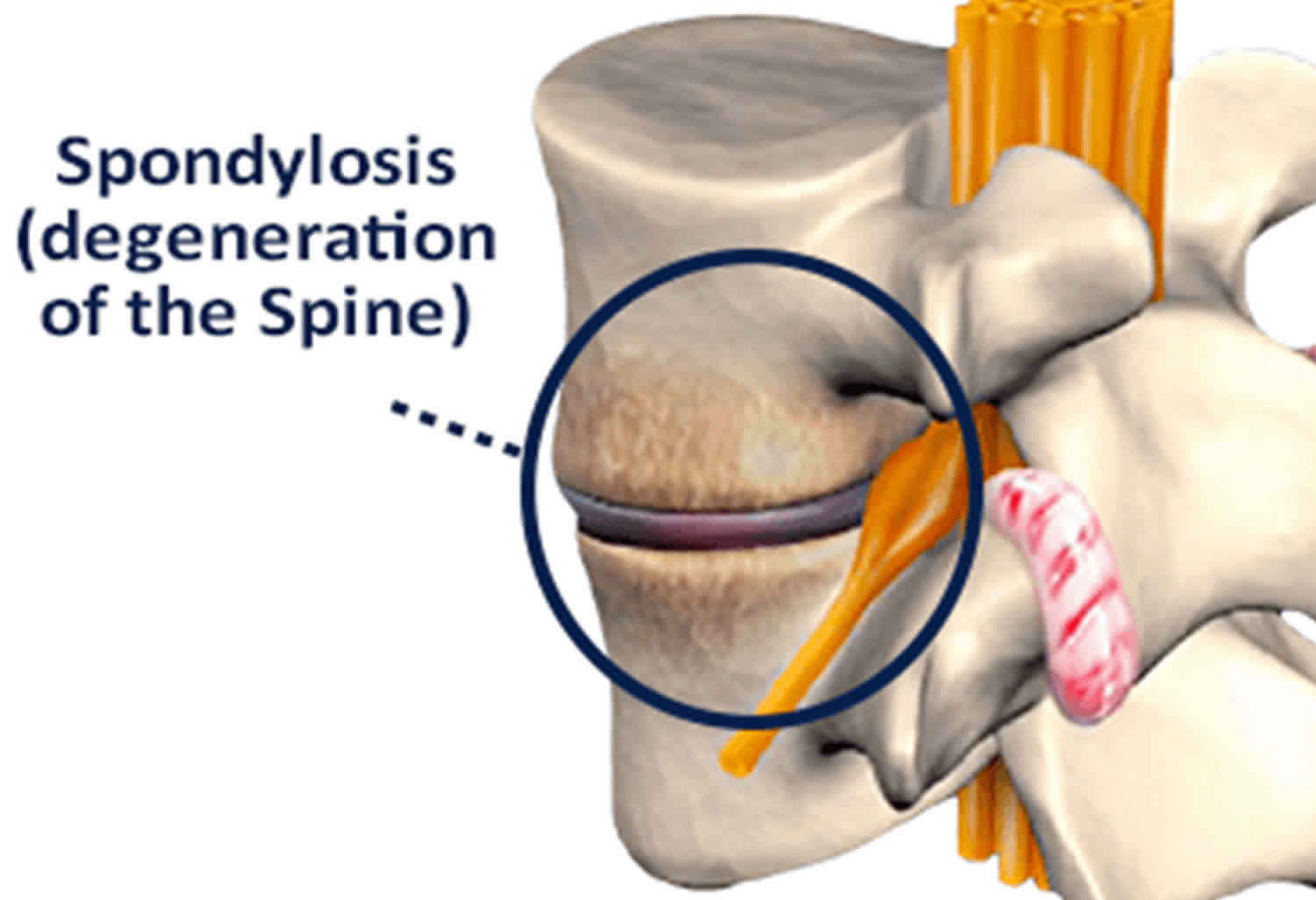
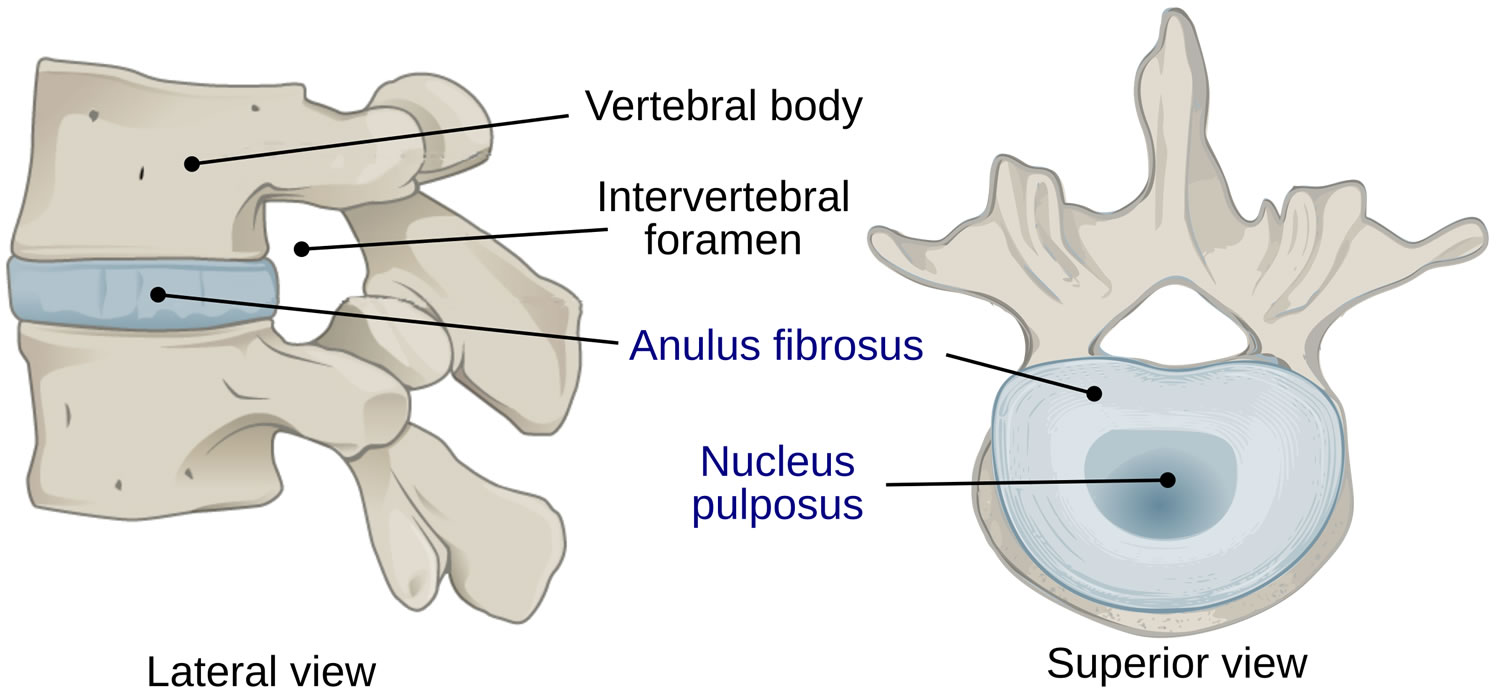
Spondylosis also known as osteoarthritis of the spine, is used as a broad descriptive term referring to a common progressive degenerative (wear and tear) disorder of the human spine from any cause; it is usually further qualified by the part of the spine affected, e.g. cervical spondylosis (neck), thoracic spondylosis (middle back) and lumbar spondylosis (lower back). The lumbar region the most affected, because of the exposure to mechanical stress. Spondylosis is usually caused by wear and tear to the facet joints (zygapophysial joints), intervertebral discs, muscles and bones in your spine resulting in pain and stiffness in your neck (cervical spondylosis), middle back (thoracic spondylosis) and lower back (lumbar spondylosis). Like the rest of your body, the intervertebral disks and facet joints in your spine slowly degenerate as you age. Intervertebral discs consist of three major components: an outer fibrous ring called the anulus fibrosus, which surrounds an inner gel-like center, the nucleus pulposus and the cartilaginous endplates that anchor the discs to adjacent vertebrae (Figure 6) 1. The intervertebral disc (intervertebral disk) is the connecting medium between the vertebrae for the transmission of external force in a physiological environment and is important in the normal functioning of the spine. The intervertebral disc is a cushion of fibrocartilage and the principal joint between two vertebrae in the spinal column. There are 23 discs in the human spine: 6 in the cervical region (neck), 12 in the thoracic region (middle back), and 5 in the lumbar region (lower back). From a biomechanical point of view, the intervertebral discs facilitates spinal mobility by allowing your spine to be flexible without sacrificing a great deal of strength 2. They also provide a shock-absorbing effect within the spine and prevent the vertebrae from grinding together. The intervertebral disc is innervated in the outer few millimeters of the annulus fibrosus 3. Only the outer third of the anulus fibrosus is vascular and innervated in a non-pathologic state. In ageing and states of inflammation, both nerve growth and granulation tissue growth are stimulated. Additionally, the granulation tissue secretes inflammatory cytokines, which further increases sensitivity to pain sensations 1. Spondylosis changes can also result in spinal stenosis (narrowing of the spinal canal) and foraminal stenosis (a condition that results when the spinal nerve roots are compressed at the small openings at every level of the spinal column called foramina).
Patients with facet joint pain may present with symptoms of neck pain, back pain, and pain worsened with hyperextension, bending laterally, and rotation 4.
Many people with spondylosis that is seen on X-rays do not present any symptoms. In fact, lumbar spondylosis is present in 27%-37% of people without symptoms.
Approximately 90% of men ages 50 and older — and 90% of women ages 60 and older — have evidence of degenerative changes in the spine.
Some of the risk factors for spondylosis include:
- Repeated strains and sprains
- Occupation – such as jobs that require repetitive motions involving the neck or back
- Previous injuries
- Genetics
- Smoking
Symptoms of spondylosis may include:
- Tingling, numbness and weakness in the arms, hands, legs or feet
- Lack of coordination and difficulty walking
- Sciatica
- Radiculopathy
- Radiculitis
- Pinched nerves
- Localized pain and regional tenderness
- Muscle spasms
- Pain that worsens with prolonged standing, sitting and forward bending
- Numbness and tingling
- Weakness in one or more limbs
- Loss of bladder or bowel control
Seek immediate medical attention if you notice a sudden onset of numbness or weakness, or loss of bladder or bowel control.
As many people with spondylosis do not present symptoms, specific testing may be needed to get a medical diagnosis. If positive, a physician may use more specific terminology regarding your condition such as cervical degenerative disc disease, cervical spinal stenosis, or lumbar spinal stenosis as they describe the pain more effectively.
A doctor will begin with a physical examination to check your range of motion, reflexes, muscle strength and walk to observe if there are changes in your gait.
Imaging studies, such as an x-ray, MRI scan or CT myelography can provide detailed views of your spine. Electromyography (EMG) may also be performed to measure the electrical activity from your nerves to muscles.
The severity of your symptoms and diagnostic imaging results will determine the spondylosis treatment plan that is best for you. Often, conservative treatments will be suggested to relieve pain and help you get back to everyday life.
In severe cases or when non-surgical treatments for spondylosis fail to provide relief, surgical treatment may be recommended.
Non-surgical treatment
In mild to moderate cases of spondylosis, non-surgical treatment options can be effective. These options include:
- Lifestyle changes
- Rest
- Over-the-counter anti-inflammatory drugs
- Physical therapy
- Cortisone shots
- Chiropractic adjustments
- Prescription pain medication
Surgical treatment
Whether you have cervical (neck), lumbar (lower back), or thoracic (mid-back) spondylosis, surgery is NOT commonly recommended for spondylosis unless your doctor determines that:
- A spinal nerve is being pinched by a herniated disk or bone (cervical radiculopathy), or
- Your spinal cord is being compressed (cervical spondylotic myelopathy)
Patients who have progressive neurologic symptoms, such as arm weakness, numbness, unsteadiness while walking, or falling, are more likely to be helped by surgery.
Sometimes, surgery may be recommended if you have severe neck pain (without nerve compression) that has not been relieved by nonsurgical treatment. However, some patients with severe neck pain will not be candidates for surgery. This may be due to the widespread nature of their arthritis, other medical problems, or other causes for their pain, such as fibromyalgia.
Spine anatomy
The spinal column supports your body, allowing you to stand, bend, twist, lift, and complete everyday activities. It also helps protect your spinal cord from injury. There are 33 individual bones, called vertebra, stacked atop one another in the vertebral column.
The column is divided into different regions, the cervical, thoracic, lumbar, sacrum, and coccyx. The sacrum and coccyx are at the bottom of the column and are fused together. The 24 vertebrae located along the cervical, thoracic and lumbar sections are moveable.
Between each vertebra is an intervertebral disc. The discs keep your vertebrae from rubbing together. The discs have a strong exterior ring called an annulus, while the inside (nucleus) has a mucoprotein gel that acts like a shock absorber for your spine.
Figure 1. Vertebral column
Figure 2. Spinal cord

Figure 3. Spinal cord segments
Figure 4. Spinal cord anatomy
Figure 5. Processing of sensory input and motor output by the spinal cord
Footnote: Sensory input is conveyed from sensory receptors to the posterior gray horns of the spinal cord, and motor output is conveyed from the anterior and lateral gray horns of the spinal cord to effectors (muscles and glands).
Figure 6. Intervertebral disk
Figure 7. Lumbar vertrebrum (looking from above)
Figure 8. Lumbar vertebrae anatomy (looking from behind and from the side)
Figure 9. Thoracic spondylosis
Cervical spondylosis
Cervical spondylosis is a common progressive degenerative disorder of the cervical spine (C1 to C7 vertebrae) often caused by the natural aging process 5. Cervical spondylosis is the most common progressive disorder in the aging cervical spine. In the cervical spine this chronic degenerative process affects the intervertebral discs and facet joints of the cervical spine, and may progress to disk herniation, osteophyte formation, vertebral body degeneration, compression of the spinal cord, or cervical spondylotic myelopathy 6. Cervical spondylosis is defined as “vertebral osteophytosis secondary to degenerative disc disease” due to the osteophytic formations (bone spur or a bony projection associated with the degeneration of cartilage at joints) that occur with progressive spinal segment degeneration 7. Biomechanically, the disc and the facets are the connecting structures between the vertebrae for the transmission of external forces. They also facilitate cervical spine mobility. Symptoms related to myelopathy (disease of the spinal cord) and radiculopathy (disease of the root of a nerve) are caused by the formation of osteophytes, which compromise the diameter of the spinal canal. This compromise may also be partially developmental. The developmental process, together with the degenerative process, may cause mechanical pressure on the spinal cord at one or multiple levels. This pressure may produce direct neurological damage or ischemic changes and, thus, lead to spinal cord disturbances.
The prevalence of cervical spondylosis is similar for both sexes, although the degree of severity is greater for males 8. Repeated occupational trauma may contribute to the development of cervical spondylosis 9.
Symptoms of cervical spondylosis manifest as neck pain and neck stiffness and can be accompanied by radicular symptoms when there is compression of neural structures. If cervical spondylosis severely compresses your spinal cord or nerve roots, the damage can be permanent.
Cervical osteoarthritis (neck arthritis) symptoms may include:
- Neck pain and stiffness that is worse in the morning or at night
- Headaches that mostly occur in the back of the head
- Pain that radiates into shoulders and arms
- Muscle weakness that makes it hard to lift the arms or grasp objects firmly
Although ageing is the primary cause of cervical spondylosis 10, the location and rate of degeneration as well as degree of symptoms and functional disturbance varies and is unique to the individual. The primary risk factor and contributor to the incidence of cervical spondylosis is age-related degeneration of the intervertebral disc and cervical spinal elements. Degenerative changes in surrounding structures, including the uncovertebral joints, facet joints, posterior longitudinal ligament and ligamentum flavum all combine to cause narrowing of the spinal canal and intervertebral foramina. Consequently, the spinal cord, spinal vasculature, and nerve roots can be compressed, resulting in the three clinical syndromes in which cervical spondylosis presents: axial neck pain, cervical myelopathy, and cervical radiculopathy.
In about 10% of patients, cervical spondylosis is due to congenital bony anomalies, blocked vertebrae, malformed laminae that place undue stress on adjacent intervertebral discs 11.
Risk factors for cervical spondylosis include 12:
- Age. Cervical spondylosis occurs commonly as part of aging.
- Occupation. Jobs that involve repetitive neck motions, awkward positioning or a lot of overhead work put extra stress on the neck.
- Neck injuries. Previous neck injuries appear to increase the risk of cervical spondylosis.
- Genetic factors. Some individuals in certain families will experience more of these changes over time.
- Smoking. Smoking has been linked to increased neck pain.
Factors that can contribute to an accelerated disease process and early-onset cervical spondylosis include exposure to significant spinal trauma, a congenitally narrow vertebral canal, dystonic cerebral palsy affecting cervical musculature, and specific athletic activities such as rugby, soccer, and horse riding 13.
Figure 10. Cervical spondylosis
Cervical spondylosis treatment
A thorough understanding of the biomechanics, the pathology, the clinical presentation, the radiological evaluation, is essential for the management of patients with cervical spondylosis.
Treatment for cervical spondylosis depends on its severity. The goal of treatment is to relieve pain, help you maintain your usual activities as much as possible, and prevent permanent injury to the spinal cord and nerves.
Mild cervical spondylosis might respond to:
- Regular exercise. Maintaining activity will help speed recovery, even if you have to temporarily modify some of your exercises because of neck pain. People who walk daily are less likely to experience neck and low back pain.
- Pain relievers you can buy without a prescription. Ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) or acetaminophen (Tylenol, others) is often enough to control the pain associated with cervical spondylosis.
- Heat or ice. Applying heat or ice to your neck can ease sore neck muscles.
- Soft neck brace. This is a padded ring that wraps around the neck and is held in place with velcro. The brace allows your neck muscles to rest. However, a neck brace should be worn for only short periods of time because it can eventually weaken neck muscles and cause neck stiffness.
- Both massage therapy and acupuncture are being studied to treat neck pain. Some early results suggest that both may be helpful.
Medications
If nonprescription pain relievers aren’t enough, your health care provider might prescribe:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve), are commonly available without a prescription. You may need prescription-strength versions to relieve the pain and inflammation associated with cervical spondylosis.
- Corticosteroids. A short course of oral prednisone might help ease pain. If your pain is severe, steroid injections may be helpful.
- Muscle relaxants. Certain drugs, such as cyclobenzaprine (Amrix, Fexmid), can help relieve muscle spasms in the neck.
- Anti-seizure medications. Some epilepsy medications can dull the pain of damaged nerves.
- Antidepressants. Certain antidepressant medications can help ease neck pain from cervical spondylosis.
Physical therapy
A physical therapist can teach you exercises to help stretch and strengthen the muscles in your neck and shoulders. This can be one of the best treatments for the pain and stiffness. Some people with cervical spondylosis benefit from the use of traction, which can help provide more space within the spine if nerve roots are being pinched.
Chiropractic adjustments can help relieve neck pain and stiffness. The chiropractor may manipulate your spine or perform adjustments to relieve symptoms. The treatment is typically done after X-rays of the cervical spine have been completed.
Steroid-based injections
Many patients find short-term pain relief from steroid injections. The most common procedures for neck pain include:
- Cervical epidural block. In this procedure, steroid and anesthetic medicine is injected into the space next to the covering of the spinal cord (epidural space). This procedure is typically used for neck and/or arm pain that may be due to a cervical disk herniation, also known as radiculopathy or a pinched nerve.
- Cervical facet joint block. In this procedure, steroid and anesthetic medicine is injected into the capsule of the facet joint. The facet joints are located in the back of the neck and provide stability and movement. These joints can develop arthritic changes that may contribute to neck pain.
- Medial branch block and radiofrequency ablation. This procedure is used in some cases of chronic neck pain. It can be used to both diagnose and treat a painful joint. During the diagnosis portion of the procedure, the nerve that supplies the facet joint is blocked with a local anesthetic. If your pain is relieved, then your doctor may have pinpointed the source of your neck pain. The next step option may be to block the pain more permanently. This is done by damaging the nerves that supply the joint with a burning technique — a procedure called radiofrequency ablation. Pain relief from an ablation typically lasts for several months. If the nerve regenerates, however, pain can return.
Surgery
Surgery is NOT commonly recommended for cervical spondylosis and neck pain unless your doctor determines that:
- A spinal nerve is being pinched by a herniated disk or bone (cervical radiculopathy), or
- Your spinal cord is being compressed (cervical spondylotic myelopathy)
If conservative treatment fails or if you have progressive neurologic symptoms — such as weakness, numbness, unsteadiness while walking, or falling —you might need surgery to create more room for your spinal cord and nerve roots.
Sometimes, surgery may be recommended if you have severe neck pain (without nerve compression) that has not been relieved by nonsurgical treatment. However, some patients with severe neck pain will not be candidates for surgery. This may be due to the widespread nature of their arthritis, other medical problems, or other causes for their pain, such as fibromyalgia.
The surgery might involve removing a herniated disk, bone spurs or part of a vertebra. A segment of your neck may need to be fused with bone grafts and hardware.
Lumbar spondylosis
Lumbar spondylosis also known as degeneration of the lumbar spine (L1 to L5 vertebrae), may be applied nonspecifically to any and all degenerative conditions affecting the lumbar intervertebral discs, vertebral bodies, and/or associated joints of the lumbar spine 14. Lumbar spondylosis may lead to spinal stenosis (narrowing of the spinal canal), vertebral instability and/or malalignment, which may be associated with back pain and/or leg symptoms 15.
Lumbar spondylosis is a complicated diagnosis because degenerative spine changes are remarkably common in population studies 14. Easy to identify radiographically – its pervasiveness throughout all patient populations makes the exact diagnosis of symptomatic cases extremely difficult. Symmons’ et al 16 study of individuals aged 45–64 years identified 85.5% of participants demonstrate osteophytes within the lumbar spine. Furthermore, degenerative changes may appear in young individuals without decades of spine loading 14. O’Neill et al. 17 explored osteophytosis within a UK adult population over age 50 years, finding 84% of men and 74% of women to demonstrate at least one vertebral osteophyte, with increased incidence among individuals with more physical activity, self reported back pain, or higher body mass index (BMI) scores. Despite marked variability within the population, men appear to have more significant degenerative changes than women, both with regard to number and severity of osteophyte formation 17.
Radiographic evidence of degenerative disease of the lumbar spine among asymptomatic individuals is impressive 14. MRI imaging in asymptomatic patients over age 60 years reveals disk protrusions in 80% 18 and degenerative spinal stenosis in 20% 19. A study comparing radiographic evidence of spine degeneration among categories of men who were without pain, with moderate pain, or with severe lower back pain found similar frequency of disk space narrowing and bone spurs among all three groups 20. Lawrence 21 found 10% of women aged 20–29 to demonstrate evidence of disk degeneration. Lumbar spondylosis, while affecting 80% of patients older than 40 years, nevertheless was found in 3% of individuals aged 20–29 years in one study 22. The high incidence of degeneration among young and asymptomatic individuals highlights the challenge involved in establishing causality between imaging findings and pain symptoms in affected patients.
Figure 11. Lumbar spondylosis
Lumbar spondylosis treatment
Given our limited ability to isolate causative sources of chronic lower back pain, there is a little consensus with regard to a definitive treatment approach 14. Substantial variation in management by conservative and invasive approaches exists between practitioners throughout the country 23.
For radicular low back pain, nonpharmacologic interventions such as exercise, traction, and spinal manipulation have shown some benefits but have relatively weak levels of evidence to support it 24. Non-steroidal anti-inflammatory drugs (NSAIDs) have moderate evidence of benefit. However, other pharmacologic interventions, such as diazepam and systemic steroids, do not seem to provide benefits 25.
For non-radicular acute or subacute low back pain, acetaminophen appears to have weak evidence of no benefit. However, NSAIDs, heat, and muscle relaxants have moderate evidence for positive gain. Massage has weak evidence that leans toward being advantageous 25.
For non-radicular chronic low back pain, there is moderate evidence to support physical therapy 25, particularly utilizing the McKenzie method 26. Acupuncture also has moderate-strength evidence to support its benefit in this population. Tai chi, yoga, psychological techniques (such as biofeedback and progressive relaxation), spinal manipulation, and multidisciplinary rehab all have weak evidence that leans toward benefit 27. Back schools also have some evidence of benefit 28. As far as pharmacologic management of chronic low back pain, NSAIDs and duloxetine demonstrate ongoing benefits, while opioids only demonstrate short-term benefits 25. Gabapentin is a very commonly used anticonvulsant for chronic pain; however, it has not demonstrated a significant benefit for patients with chronic low back pain 29. Topiramate is more effective than a placebo 30. Topical anesthetics such as lidocaine patches and transcutaneous electrical nerve stimulation (TENS) units do not appear more effective than placebo 31.
According to the American Pain Society, surgical referral should be reserved for patients with disabling low back pain impacting the quality of life for greater than one year 32. However, there is mixed evidence, for some of the most commonly performed invasive procedures such as injection therapy of the epidural space, facet joints, or local sites, spinal fusion, or lumbar disk replacement 33.
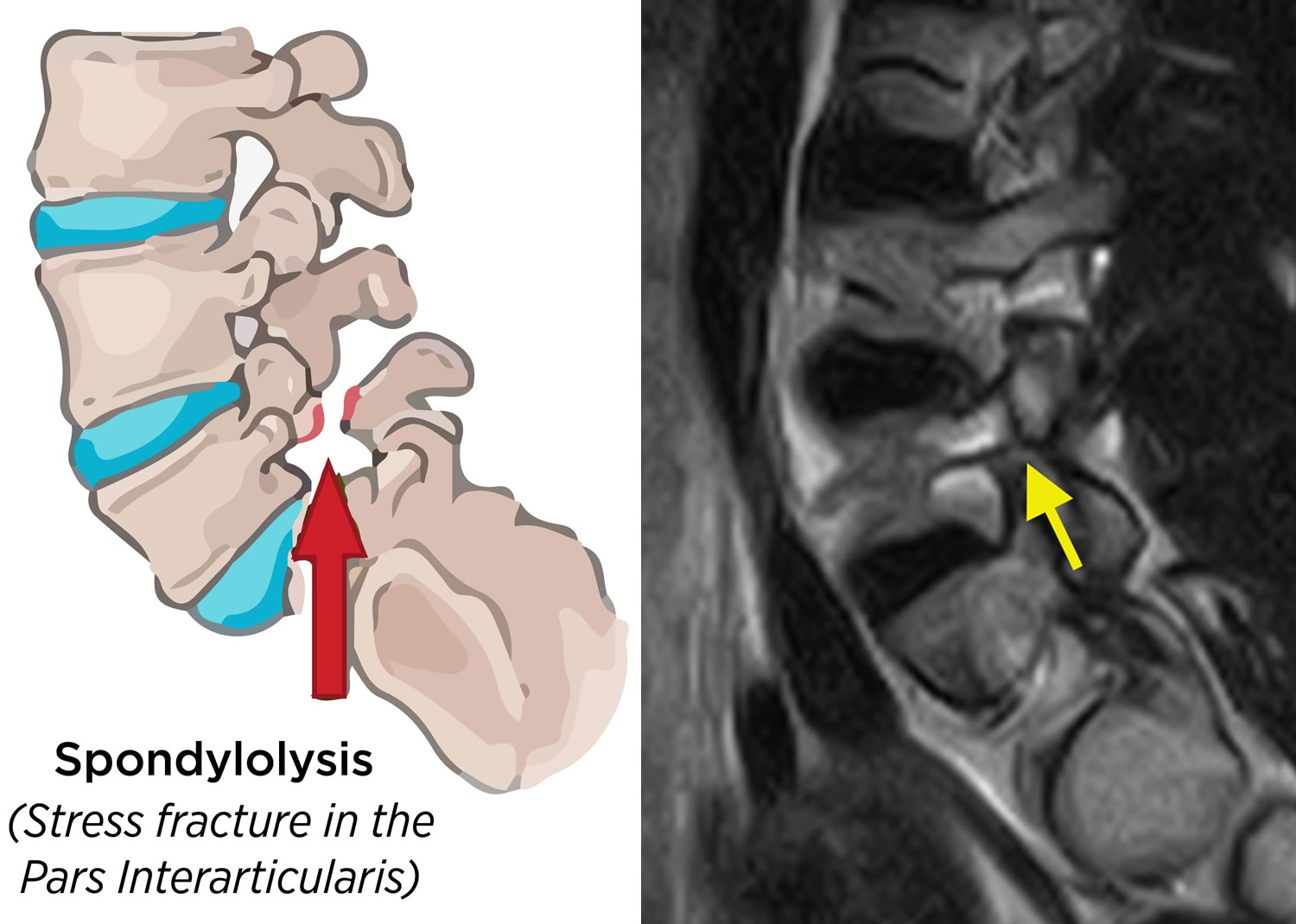
What is spondylolysis?
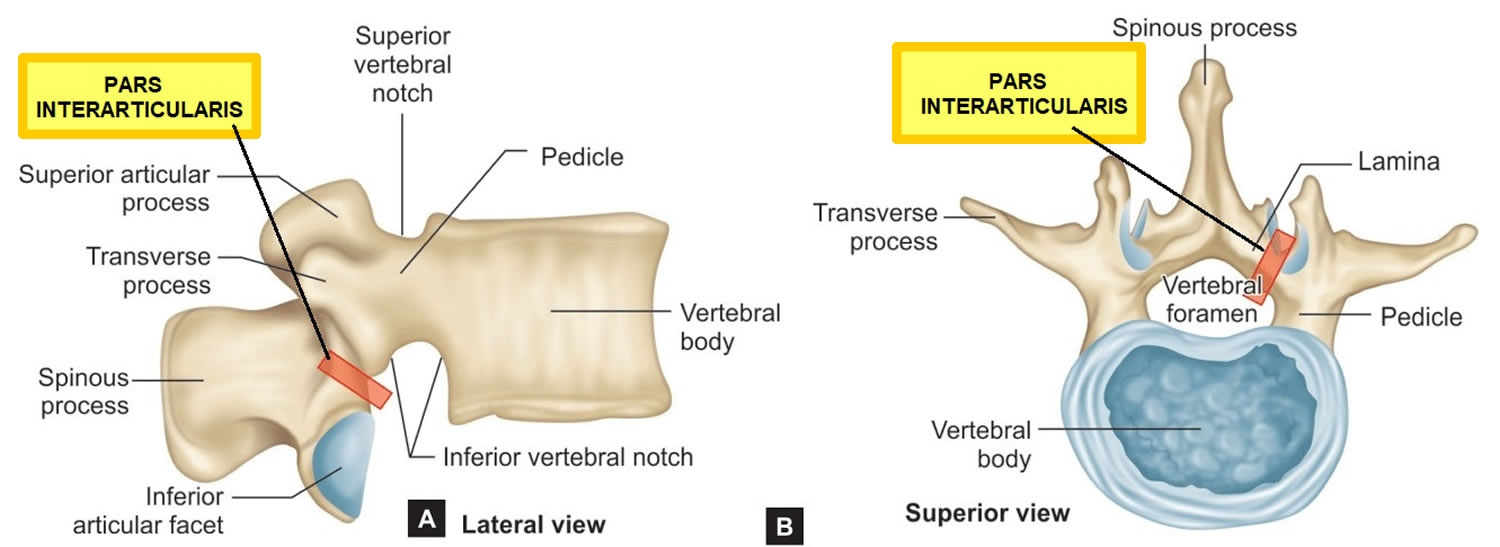
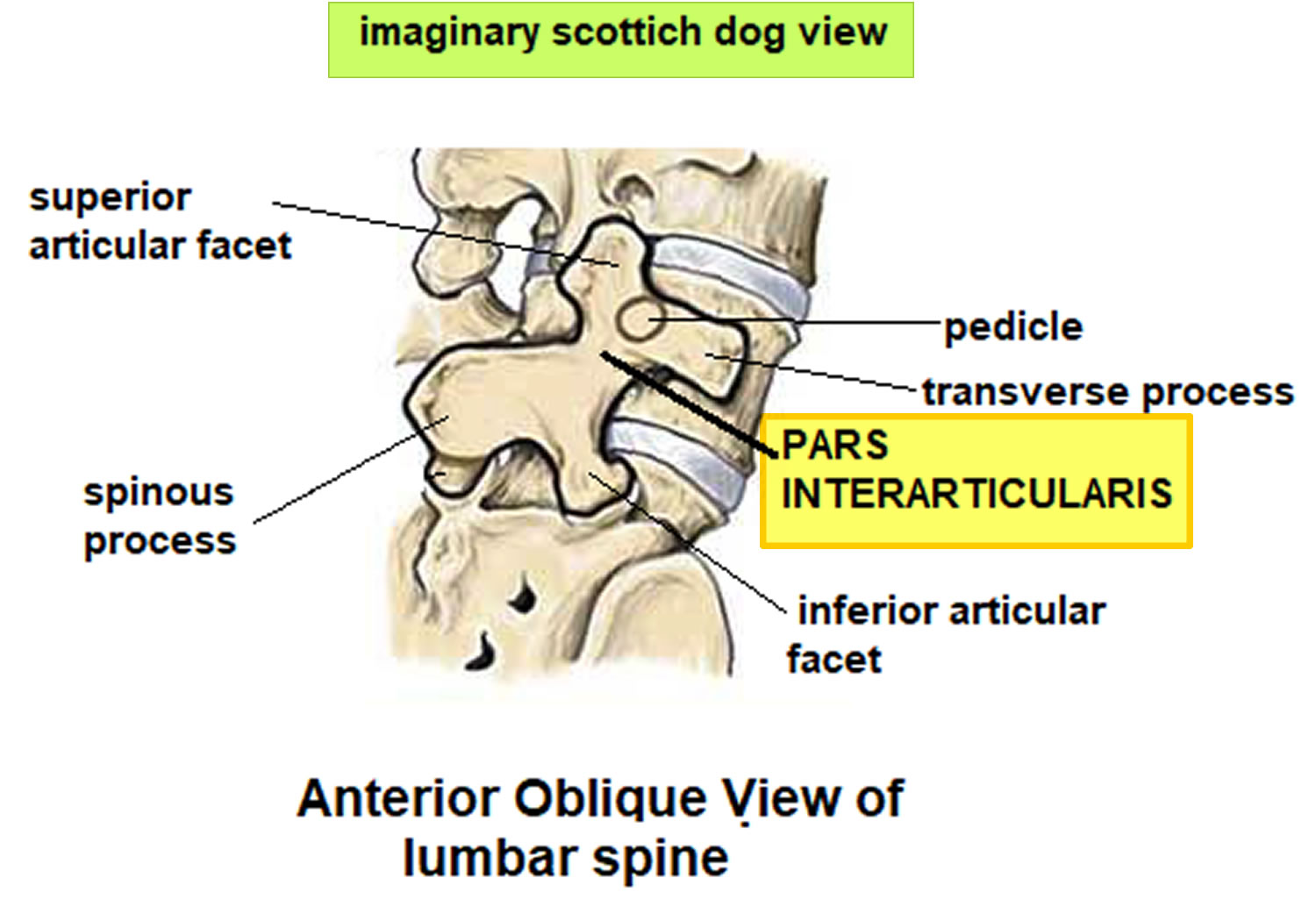
Spondylolysis also known as pars interarticularis defect or pars fracture, is a crack or stress fracture that develops through the pars interarticularis (pars fracture) of the neural arch, the portion of the neural arch that connects connects the upper and lower facet joints. Spondylolysis is present in about 5% of the population 34 and higher in the adolescent athletic population. Spondylolysis is more common in men than in women 35. About 90% of cases of spondylolysis occur at the fifth vertebra of the lumbar spine (L5) and ~10% occurs in the fourth lumbar vertebra (L4) 34. The crack or stress fracture can occur on one side or both sides of the bone.
Spondylolysis is commonly asymptomatic. Symptomatic patients often have pain with extension and/or rotation of the lumbar spine. Approximately 25% of individuals with spondylolysis have symptoms at some time.
Spondylolysis is a common cause of low back pain in children and adolescents and may be the cause of low back pain in about 50% of adolescent athletes 36.
Spondylolysis may be developmental defect or acquired. Developmental defects may develop in children <10 years 36. Acquired defects have two main mechanisms:
- repeated microtrauma, resulting in a stress injury and eventual fracture of the pars interarticularis; a dysplastic pars is usually present.
- traumatic pars defects result from high-energy trauma where there is hyperextension of the lumbar spine and are rare in a congenitally normal vertebra
The pars interarticularis is the weakest portion of the vertebra. For this reason, it is the area most vulnerable to injury from the repetitive stress and overuse that characterize many sports. However, spondylolysis can also occur in people of all ages without injury or sports participation.
85% of patients with spondylolysis will progress to spondylolisthesis 34, which is seen radiographically in ~25% of patients with spondylolysis 37. In most patients this occurs before the age of 16.
Spondylolysis may also be associated with spina bifida occulta and idiopathic scoliosis: ~5% 38.
For most patients with spondylolysis, back pain and other symptoms will improve with nonsurgical treatment.
Spondylolysis nonsurgical treatment may include:
- Rest. Avoiding sports and other activities that place excessive stress on the lower back for a period of time can often help improve back pain and other symptoms.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs such as ibuprofen and naproxen can help reduce swelling and relieve back pain.
- Chiropractic care.
- Physical therapy. Specific exercises can help improve flexibility, stretch tight hamstring muscles, and strengthen muscles in the back and abdomen.
- Bracing. Some patients may need to wear a back brace for a period of time to limit movement in the spine and allow a recent pars fracture the opportunity to heal. Although athletes wtih sudden or acute onset of pain are candidates for brace treatment, patients with longer-term pain are not. In these patients, the stress fracture will have a low chance of healing, even after several months in a brace.
Over the course of treatment, your child’s doctor will take periodic X-rays to determine whether the vertebra is changing position.
Surgery is only considered in rare circumstances as most cases respond to conservative management 34. Incomplete fractures demonstrate good healing rates with conservative management 36.
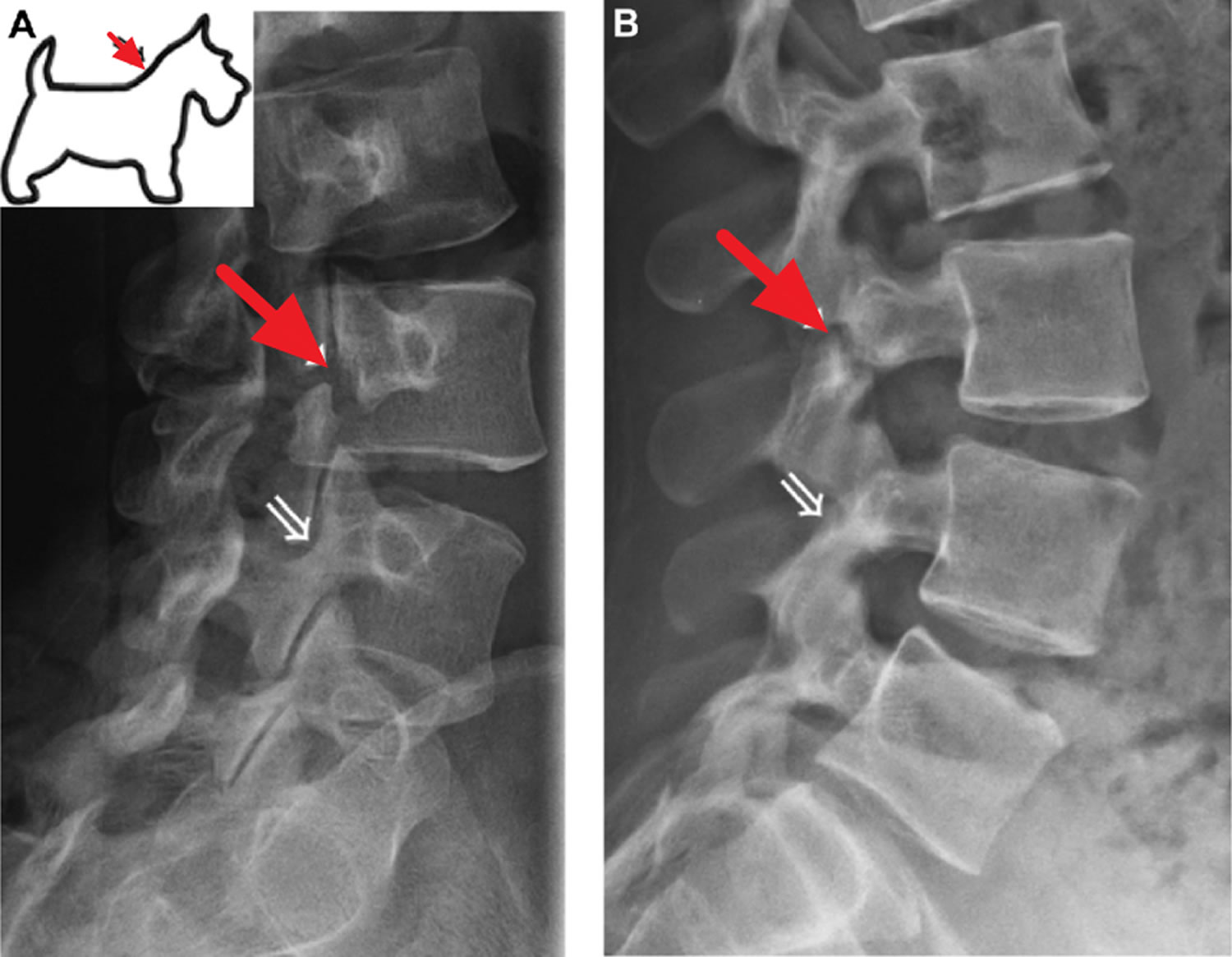
Figure 12. Pars interarticularis
Figure 13. Pars interarticularis oblique view showing the imaginary “Scottish dog”
Figure 14. Spondylolysis
Figure 15. Pars interarticularis defect (the Collar sign in spondylolysis refers to a break in the pars interarticularis of the vertebra on oblique radiographs that can have the appearance of a collar around the Scotty dog’s neck)
Footnote: Right-sided pars interarticularis defect at L3 (red arrow) on oblique (A) and lateral (B) radiographs of the lumbar spine. A normal right L4 pars interarticularis is marked with white arrow on the radiographs and on a representative artistic rendition of the Scottie dog’s neck.
[Source 39 ]What is spondylolisthesis?
Spondylolisthesis denotes the slippage of one vertebra relative to the one below. Spondylolisthesis is used synonymously with anterolisthesis, which refers to anterior displacement (forward slip) of a vertebral body relative to the one below 40. In spondylolisthesis, the fractured pars interarticularis separates, allowing the injured vertebra to shift or slip forward on the vertebra directly below it. In children and adolescents, this slippage most often occurs during periods of rapid growth — such as an adolescent growth spurt.
Spondylolisthesis most commonly occurs in the lower back (lower lumbar spine) but can also occur in the cervical spine and rarely, except for trauma, in the thoracic spine. Spondylolisthesis most commonly occurs at the L5-S1 level with anterior translation of the L5 vertebral body on the S1 vertebral body 41. The L4-5 level is the second most common location for spondylolisthesis 41.
Doctors commonly describe spondylolisthesis as either low grade or high grade, depending upon the amount of slippage. A high-grade slip occurs when more than 50% of the width of the fractured vertebra slips forward on the vertebra below it. Patients with high-grade slips are more likely to experience significant pain and nerve injury and to need surgery to relieve their symptoms and prevent further deterioration.
Spondylolisthesis is classified according to the Meyerding Classification 42. This is a measure of the percent of antero (forward) or retro (backward) slippage/transitional displacement of one vertebral body on the vertebral body below observed on lateral radiographs.
- Grade 1: Less than 25%
- Grade 2: 25 to 50%
- Grade 3: 50 to 75%
- Grade 4: 75 to 100%
- Grade 5 (spondyloptosis): Greater than 100% displacement of the vertebral body.
For most patients with low-grade spondylolisthesis, back pain and other symptoms will improve with nonsurgical treatment.
Spondylolisthesis nonsurgical treatment may include:
- Rest. Avoiding sports and other activities that place excessive stress on the lower back for a period of time can often help improve back pain and other symptoms.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs such as ibuprofen and naproxen can help reduce swelling and relieve back pain.
- Chiropractic care.
- Physical therapy. Specific exercises can help improve flexibility, stretch tight hamstring muscles, and strengthen muscles in the back and abdomen.
- Bracing. Some patients may need to wear a back brace for a period of time to limit movement in the spine and allow a recent pars fracture the opportunity to heal. Although athletes wtih sudden or acute onset of pain are candidates for brace treatment, patients with longer-term pain are not. In these patients, the stress fracture will have a low chance of healing, even after several months in a brace.
Over the course of treatment, your child’s doctor will take periodic X-rays to determine whether the vertebra is changing position.
Surgery may be recommended for spondylolisthesis patients who have:
- Severe or high-grade slippage
- Slippage that is progressively worsening
- Back pain that has not improved after a period of nonsurgical treatment
Spinal fusion between the fifth lumbar vertebra and the sacrum is the surgical procedure most often used to treat patients with spondylolisthesis.
The goals of spinal fusion are to:
- Prevent further progression of the slip
- Stabilize the spine
- Alleviate significant back pain
Figure 16. Spondylolisthesis
Spondylosis signs and symptoms
Most people with spondylosis experience no symptoms. Spondylosis generally begins earlier in men than in women. Many people with spondylosis that is seen on X-rays do not present any symptoms. In fact, lumbar spondylosis is present in 27%-37% of people without symptoms.
When symptoms do occur, they typically include pain and stiffness in your neck (cervical spondylosis), middle back (thoracic spondylosis) and lower back (lumbar spondylosis).
Sometimes spondylosis results in a narrowing of the spinal canal within the bones of the spine (the vertebrae). The spinal canal is the space inside the vertebrae that the spinal cord and the nerve roots pass through to reach the rest of the body. If the spinal cord or nerve roots become pinched, you might experience:
- Tingling, numbness and weakness in the arms, hands, legs or feet
- Lack of coordination and difficulty walking
- Sciatica
- Radiculopathy
- Radiculitis
- Pinched nerves
- Localized pain and regional tenderness
- Muscle spasms
- Pain that worsens with prolonged standing, sitting and forward bending
- Numbness and tingling
- Weakness in one or more limbs
- Loss of bladder or bowel control
Seek immediate medical attention if you notice a sudden onset of numbness or weakness, or loss of bladder or bowel control.
Spondylosis causes
Although age-related wear and tear of the vertebrae are the main cause of spondylosis, there are changes within the spinal anatomy that can lead to pain. Additionally, injuries, such as those from a car accident or while playing sports, can enable disc degeneration.
As people age, the structures that make up your backbone and neck gradually develop wear and tear. These changes can include:
- Disc dehydration. Disks act like cushions between the vertebrae of the spine. By the age of 40, most people’s spinal disks begin drying out and shrinking. As the disks become smaller, there is more bone-on-bone contact between the vertebrae.
- Herniated disks. When cracks appear on the exterior of the spinal disks. The soft interior of a disc can squeeze through these cracks. Sometimes, it presses on the spinal cord and nerve roots.
- Bone spurs. As the disks break down, the body may produce extra amounts of bone in a misguided effort to strengthen the spine. These bone spurs can sometimes pinch the spinal cord and nerve roots.
- Stiff ligaments. Ligaments are cords of tissue that connect bone to bone. Spinal ligaments can stiffen with age, making the neck less flexible.
- Spinal stenosis. Spinal stenosis occurs when the spinal column canal narrows, which leads to compression of the spinal nerves and cord.
- Spondylolisthesis. This condition occurs when a vertebrae slips forward in the spinal column losing its original place.
- Facet syndrome. This is a degenerative condition that occurs when cartilage within the facet joints wear down.
Large studies of osteoarthritis have long recognized the aging process to be the strongest risk factor for bony degeneration, particularly within the spine 43. An extensive autopsy study in 1926 reported evidence of spondylosis deformans (bony outgrowths arising primarily along the anterior and lateral perimeters of the vertebral end-plate apophyses) to increase in a linear fashion from 0% to 72% between the ages of 39 and 70 years 44. A subsequent autopsy study by Miller et al. 45 similarly noted an increase in disk degeneration from 16% at age 20 to about 98% at age 70 years based on macroscopic disk degeneration grades of 600 specimens. Other studies corroborate this finding 46, 17. The associations are nevertheless imperfect. Kramer 47 found increasing age to be significantly associated with osteophyte formation but not predictive of the degree of disk space narrowing observed in a retrospective review of radiographs of women. She observed significant variability, noting “although few younger women have high average scores, some older women have no radiographic sign of OA, while others are severely affected” 47. Multiple studies have also demonstrated the presence of significant lumbar degeneration to be evident even within the first two decades 45, 46. Such variability within members of the same age category suggests the influence of other contributing factors.
Is osteophyte formation inherently pathological? van der Kraan and van den Berg 48 question if osteophyte formation may represent a remodeling process, functionally adapting to the instability or the changes in the demands of the spine. Likewise, Humzah and Soames 49 emphasize the dynamic and reparative qualities of the intervertebral disk, responding to variations in mechanical loading and influencing vertebral kinematics to extend this argument. Osteophytes may form in the absence of other degenerative processes, and cartilaginous damage may exist without corresponding osteophytes 48. Although there remains a strong association between the presence of osteophytes and other degenerative spine changes, isolated instances of one without the other occur, in the absence of overt symptoms.
Disk generation has long been associated with certain activities. Retrospective studies cite Body Mass Index (BMI), incident back trauma, daily spine loading (twisting, lifting, bending, and sustained nonneutral postures), and whole body vibration (such as vehicular driving) to be factors which increase both the likelihood and severity of spondylosis 50. While these correlations exist, a study following progressive radiographic changes in lumber degenerative disk disease did not find significant associations with the extent of physical activity, noting only age, back pain, and associated hip osteoarthritis to be predictive of degenerative disk disease and osteophyte changes 51.
Genetic factors likely influence the formation of osteophytes and disk degeneration. Spector and MacGregor 52 proposed that 50% of the variability found in osteoarthritis can be attributed to heritable factors. Similarly, twin studies evaluating the progression of degenerative changes in lumbar MRI imaging suggest that approximately half (47–66%) of the variance could be explained by genetic and environmental factors, attributing only 2–10% of variance to physical loading and resistance training 53. Another twin study revealed a high degree of similarity in signal intensity, disk height narrowing, disk bulging, and end-plate changes 54. A search for these underlying genetic factors has identified polymorphisms in genes regulating inflammatory pathways and a Vitamin D Receptor allele to correspond to radiographic progression of lumbar disk degeneration 55.
Spondylosis risk factors
As with many other degenerative spine conditions, spondylosis is susceptible to certain risk factors that increase the possibilities of someone developing the condition. Some of the risk factors associated with spondylosis include:
- Age: Since spondylosis is the response of wear and tear, age is a significant factor in its occurrence. With age, the protective cartilage and bones in the spine become prone to wear and tear that can lead to spondylosis.
- Work: Jobs involving repetitive motions or awkward positioning of the spine place additional stress on the spine.
- Sudden injuries: Previous or unexpected injuries to the spine can increase the risk of spondylosis.
- Genetics: In some cases, certain individuals may be genetically predisposed to excessive disc wear and tear or joint damage.
- Abnormal movements: Hypermobility or abnormal spinal movements can lead to bone spurs, degenerative discs, and other spine conditions that can lead to spondylosis.
Spondylosis diagnosis
Your doctor will likely start with a physical exam that includes:
- Checking the range of motion in your spine
- Testing your reflexes and muscle strength to find out if there’s pressure on your spinal nerves or spinal cord
- Watching you walk to see if spinal compression is affecting your gait
Imaging tests
Imaging tests can provide detailed information to guide diagnosis and treatment. Examples include:
- Spine X-ray. An X-ray can show changes in the spine, such as bone spurs, that indicate spondylosis. Spine X-ray can also rule out rare and more serious causes for neck pain and stiffness, such as tumors, cancer, infections or fractures.
- Magnetic Resonance Imaging (MRI). Using radio waves and a strong magnetic field, MRI can produce detailed images that can help pinpoint areas where nerves might be pinched.
- Computed Tomography (CT) Myelography. In this type of CT scan, a dye is injected into the spinal canal to provide more-detailed imaging. This test makes it easier to see the details of the spinal cord, spinal canal and nerve roots, to better evaluate the location and amount of neural compression. CT myelography is more invasive than an MRI but can be a consideration in patients who have a contraindication to MRI (e.g., pacemaker) or have an artifact from the hardware.
Nerve function tests
You may need tests to determine if nerve signals are traveling properly to your muscles. Nerve function tests include:
- Electromyography. This test measures the electrical activity in your nerves as they transmit messages to your muscles when the muscles are contracting and at rest.
- Nerve conduction study. Electrodes are attached to the skin above the nerve to be studied. A small shock is passed through the nerve to measure the strength and speed of nerve signals.
Spondylosis treatment
The treatment for spondylosis depends on the severity of your signs and symptoms. The goals of treatment are to relieve pain, improve functional ability with the return of the patient to sports and other day-to-day activities, and prevent permanent injury to neural structures.
For most patients with spondylosis, neck or back pain and other symptoms will improve with nonsurgical treatment.
Nonsurgical treatment
Nonsurgical treatment may include:
- Rest. Avoiding sports and other activities that place excessive stress on the lower back for a period of time can often help improve back pain and other symptoms.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs such as ibuprofen and naproxen can help reduce swelling and relieve back pain.
- Chiropractic adjustments can help relieve neck and lower back pain and stiffness. The chiropractor may manipulate your spine or perform adjustments to relieve symptoms. The treatment is typically done after X-rays of the whole spine have been completed.
- Physical therapy. Specific exercises can help improve flexibility, stretch tight hamstring muscles, and strengthen muscles in the back and abdomen. Exercise therapy remains one of the conservative mainstays of treatment for chronic lumbar spine pain, and may be tailored to include aerobic exercise, muscle strengthening, and stretching exercises 56. Significant variation in regimen, intensity, and frequency of prescribed programs presents challenges to assessing efficacy among patients 57. One meta-analysis of the current literature exploring the role of exercise therapy in patients with varying duration of symptoms found a graded exercise program implemented within the occupational setting demonstrated some effectiveness in subacute low back pain. Among those suffering chronic pain symptoms, small, but statistically significant improvements were observed among patients, with regard to pain reduction and functional improvement 56. The optimal approach to exercise therapy in chronic low back pain sufferers appears to be those regimens involving an individually-designed exercise program emphasizing stretching and muscle strengthening, administered in a supervised fashion, with high frequency and close adherence. Such results are complemented by other conservative approaches, including NSAIDS, manual therapies, and daily physical activity 57.
- Back school. Back School was introduced first in Sweden with the purpose of minimizing lower back pain symptoms and their reoccurrence through review with patients of lumbar anatomy, concepts of posture, ergonomics, and appropriate back exercises 58. Two meta-analyses concluded that there is moderate evidence for improvement in both pain and functional status for chronic low back pain within short and intermediate time courses, when measured against other modalities such as exercise, joint manipulation, myofascial therapy, and/or other educational therapy 58, 59.
- Lumbar supports. Lumbar back supports may provide benefit to patients suffering chronic low back pain secondary to degenerative processes through several potential, debated mechanisms 14. Supports are designed to limit spine motion, stabilize, correct deformity, and reduce mechanical forces. They may further have effects by massaging painful areas and applying beneficial heat; however, they may also function as a placebo. There is moderate available evidence evaluating efficacy of lumbar supports within a mixed population of acute, subacute, and chronic low back pain sufferers to suggest that lumbar supports are not more effective than other treatment forms; data is conflicting with regard to patient improvement and functional ability to return to work 59.
- Traction. Lumbar traction applies a longitudinal force to the axial spine through use of a harness attached to the iliac crest and lower rib cage to relieve chronic low back pain. The forces, which open intervertebral space and decrease spine lordosis, are adjusted both with regard to level and duration and may closely be measured in motorized and bed rest devices. Temporary spine realignments are theorized to improve symptoms related to degenerative spine disease by relieving mechanical stress, nerve compression, and adhesions of the facet and annulus, as well as through disruption of nociceptive pain signals 59. Nonetheless, patients with chronic symptoms and radicular pain have not found traction to provide significant improvement in pain nor daily functioning 60. Little is known with regard to the risks associated with the applied forces. Isolated case reports cite nerve impingement with heavy forces, and the potential for respiratory constraints or blood pressure changes due to the harness placement and positioning 59.
- Transcutaneous electrical nerve stimulation (TENS). A “TENS” unit is a therapeutic modality involving skin surface electrodes which deliver electrical stimulation to peripheral nerves in an effort to relieve pain noninvasively. Such devices are frequently available in outpatient exercise therapy settings, with up to a third of patients experiencing mild skin irritation following treatment 61. While one small study identified an immediate reduction in pain symptoms 1 hour following TENS application, there remains little evidence of long-term relief. Another larger study did not discover significant improvement with TENS compared with placebo with regard to pain, functional status, or range of motion 62, 59.
- Massage therapy. Massage therapy for chronic low back pain appears to provide some beneficial relief. Weighed against other interventions, it proved less efficacious than TENS and manipulation, comparable with corsets and exercise regimens, and superior to acupuncture and other relaxation therapies, when followed over a 1-year course. Such preliminary results need confirmation, and evaluation for cost-effectiveness, but nevertheless suggest a potential role in certain, interested patients 63.
Medications
Your doctor may prescribe several medications to be used together to address both pain and inflammation.
- Acetaminophen. Mild pain is often relieved with acetaminophen.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Often prescribed with acetaminophen, NSAIDs such as aspirin, ibuprofen, and naproxen are considered first-line medications for neck pain. They relieve both pain and swelling and may be prescribed for a number of weeks, depending on your specific symptoms. Other types of pain medication can be considered if you have serious contraindications to NSAIDs or if your pain is not well controlled.
- Oral corticosteroids. A short course of oral corticosteroids can help relieve pain by reducing inflammation.
- Muscle relaxants. Medications such as cyclobenzaprine or carisoprodol can be used to treat painful muscle spasms.
Steroid-based injections
Although less invasive than surgery, steroid-based injections are prescribed only after a complete evaluation by your doctor. Your doctor will talk with you about the risks and benefits of steroid-based injections for your specific condition. Facet joint injections are commonly performed to diagnose and manage facet joint pain 4. Some patients find short-term pain relief from steroid injections.
Diagnostic blocks of the facet joint with anesthesia directly into the joint space or associated medial branch reveal single diagnostic facet blocks carry a false-positive rate of 22% to 47% 64 and medial branch blocks of 17–47% in the lumbar spine 65.
Subsequent therapeutic injections are similarly performed through either approach, with systematic reviews concluding moderate evidence available for short-term and long-term pain relief with facet blocks 66. This evidence stems from studies such as Fuch’s randomized control trial 67 showing significant pain relief, functional improvement, and quality of life enhancement at 3 and 6 month intervals. By contrast, Carette et al. [88] found no meaningful difference in perceived benefit between patients treated with steroid versus saline (control) injection at 3 and 6 month intervals. Available literature of medial branch block similarly show moderate evidence for short- and long-term relief 68 based on randomized control trial of medial branch block under fluoroscopy, showing significant relief (by means of pain relief, physical health, psychological benefit, reduced narcotic intake, and employment status), with 1–3 injections in 100% patients at 3 months, 75–88% at 6 months, and 17–25% at 1 year 69.
In a 2019 cohort study by El-Yahochouchi et al. 70, the overall incidence of immediate and delayed adverse events following a cervical epidural steroid injection was 2.4% and 4.9%, respectively. Complications include:
- Neurologic injury
- Epidural abscess
- Epidural hematoma
- Increased pain
- Vasovagal reactions
- Central steroid response (e.g., facial flushing, nonpositional headaches)
- Endocrinologic effects (e.g., hyperglycemia, hypothalamic-pituitary axis suppression, decreased bone density)
Surgical treatment
Surgery is NOT commonly recommended for spondylosis and pain unless your doctor determines that:
- A spinal nerve is being pinched by a herniated disk or bone (cervical radiculopathy), or
- Your spinal cord is being compressed (cervical spondylotic myelopathy)
Patients who have progressive neurologic symptoms, such as arm weakness, numbness, unsteadiness while walking, or falling, are more likely to be helped by surgery.
Sometimes, surgery may be recommended if you have severe neck pain (without nerve compression) that has not been relieved by nonsurgical treatment. However, some patients with severe neck pain will not be candidates for surgery. This may be due to the widespread nature of their arthritis, other medical problems, or other causes for their pain, such as fibromyalgia.
For lumbar spondylosis, there is little consensus about the definitive treatment approach due to a lack of information about the sources of chronic lower back pain. Spinal surgery for the management of low back pain, lumbar radiculopathy, and lumbar spinal stenosis is a consideration after the failure of conservative treatments 71.
- Spinal fusion (joining of vertebrae together aimed at limiting the motion between vertebrae stretch on associated nerves). This is the most common surgery for chronic nonspecific back pain with degenerative changes. Several surgical approaches exist. The more traditional approach is that of a posterior spinal fusion implementing rods and pedicular screws. Limitations of this approach include the need for thecal sac and nerve root retraction along with iatrogenic injury of the paraspinal musculature. Interbody fusion involves placing an implant such as a cage or bone graft within the intervertebral space following a discectomy (removing the intervertebral disc). Surgical approaches for interbody fusion are multiple (posterior, transforaminal, oblique, lateral, and anterior). Anterior spinal fusion avoids the canal and nerve roots but does introduce complications such as vascular injury and incisional hernia. There is limited comparative data that one approach is superior to another. Following fusion, chronic postoperative complications include pseudoarthrosis (failure of fusion) and adjacent segment degenerative disc disease above/below the fusion level 72.
- Complications from anterior and posterior cervical spine surgery include 73, 74:
- Injury to spinal cord and nerve roots
- Infection
- Dural tear and CSF leak
- Recurrent laryngeal, superior laryngeal, and hypoglossal nerve injuries
- Esophageal injury and dysphagia
- Vertebral and carotid artery injuries
- Tracheal injury
- Adjacent segment degeneration
- Pseudoarthrosis
- Post-laminectomy kyphosis
- Complications from anterior and posterior cervical spine surgery include 73, 74:
- Laminectomy (surgical removal of the laminae). This is the most common surgery for lumbar spinal stenosis (removal of part of the bone, bone spurs, or ligaments, aimed at relieving pressure on spinal nerves, but can make your spine less stable). If the laminectomy leads to iatrogenic instability, then a spinal fusion is also performed 75
- Foraminotomy. This surgery is used to relieve pain associated with a compressed nerve in the spine.
- Diskectomy.
- Disk replacement.
- Interlaminar implant.
- Waxenbaum JA, Reddy V, Futterman B. Anatomy, Back, Intervertebral Discs. [Updated 2021 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470583
- Patwardhan A, Havey R, Meade K, Lee B, Dunlap B. A follower load increases the load-carrying capacity of the lumbar spine in compression. Spine 1999;4( 10): 1003-9.
- Roberts S, Evans H, Trivedi J, Menage J. Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am. 2006 Apr;88 Suppl 2:10-4. doi: 10.2106/JBJS.F.00019
- Le DT, Alem N. Facet Joint Injection. [Updated 2022 Jun 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572125
- Ferrara LA. The biomechanics of cervical spondylosis. Adv Orthop. 2012;2012:493605. doi: 10.1155/2012/493605
- Xiong W, Li F, Guan H. Tetraplegia after thyroidectomy in a patient with cervical spondylosis: a case report and literature review. Medicine (Baltimore). 2015 Feb;94(6):e524. doi: 10.1097/MD.0000000000000524
- Shedid D, Benzel EC. Cervical spondylosis anatomy: pathophysiology and biomechanics. Neurosurgery. 2007 Jan;60(1 Supp1 1):S7-13. doi: 10.1227/01.NEU.0000215430.86569.C4
- Kelly JC, Groarke PJ, Butler JS, Poynton AR, O’Byrne JM. The natural history and clinical syndromes of degenerative cervical spondylosis. Adv Orthop. 2012;2012:393642. doi: 10.1155/2012/393642
- Moon MS, Yoon MG, Park BK, Park MS. Age-Related Incidence of Cervical Spondylosis in Residents of Jeju Island. Asian Spine J. 2016 Oct;10(5):857-868. doi: 10.4184/asj.2016.10.5.857
- Ferrara LA. The biomechanics of cervical spondylosis. Advances in orthopedics. 2012 Feb 1;2012. https://doi.org/10.1155/2012/493605
- McCormack BM, Weinstein PR. Cervical spondylosis. An update. West J Med. 1996 Jul-Aug;165(1-2):43-51. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1307540/pdf/westjmed00347-0045.pdf
- Cervical spondylosis. https://www.mayoclinic.org/diseases-conditions/cervical-spondylosis/symptoms-causes/syc-20370787
- Kuo DT, Tadi P. Cervical Spondylosis. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551557
- Middleton, K., Fish, D.E. Lumbar spondylosis: clinical presentation and treatment approaches. Curr Rev Musculoskelet Med 2, 94–104 (2009). https://doi.org/10.1007/s12178-009-9051-x
- Gibson JN, Waddell G. Surgery for degenerative lumbar spondylosis. Cochrane Database Syst Rev. 2005 Oct 19;2005(4):CD001352. doi: 10.1002/14651858.CD001352.pub3
- Symmons DP, van Hemert AM, Vandenbroucke JP, Valkenburg HA. A longitudinal study of back pain and radiological changes in the lumbar spines of middle aged women. II. Radiographic findings. Ann Rheum Dis. 1991 Mar;50(3):162-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1004366/pdf/annrheumd00451-0026.pdf
- O’Neill TW, McCloskey EV, Kanis JA, Bhalla AK, Reeve J, Reid DM, Todd C, Woolf AD, Silman AJ. The distribution, determinants, and clinical correlates of vertebral osteophytosis: a population based survey. J Rheumatol. 1999 Apr;26(4):842-8.
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994 Jul 14;331(2):69-73. doi: 10.1056/NEJM199407143310201
- Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990 Mar;72(3):403-8.
- Frymoyer JW, Newberg A, Pope MH, Wilder DG, Clements J, MacPherson B. Spine radiographs in patients with low-back pain. An epidemiological study in men. J Bone Joint Surg Am. 1984 Sep;66(7):1048-55. https://journals.lww.com/jbjsjournal/Abstract/1984/66070/Spine_radiographs_in_patients_with_low_back_pain_.11.aspx
- Lawrence JS. Disc degeneration. Its frequency and relationship to symptoms. Ann Rheum Dis. 1969 Mar;28(2):121-38. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1031120/pdf/annrheumd00235-0028.pdf
- Lumbar Spondylosis. https://emedicine.medscape.com/article/249036-overview
- Deyo R, Cherkin D, Conrad D. Cost, controversy, crisis: low back pain and the health of the public. Annu Rev Publ Health. 1991;12:141–56.
- Casiano VE, Sarwan G, Dydyk AM, et al. Back Pain. [Updated 2022 Feb 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538173
- Noninvasive Treatments for Low Back Pain: Current State of the Evidence. https://effectivehealthcare.ahrq.gov/products/back-pain-treatment/clinician
- Rosedale R, Rastogi R, May S, Chesworth BM, Filice F, Willis S, Howard J, Naudie D, Robbins SM. Efficacy of exercise intervention as determined by the McKenzie System of Mechanical Diagnosis and Therapy for knee osteoarthritis: a randomized controlled trial. J Orthop Sports Phys Ther. 2014 Mar;44(3):173-81, A1-6. doi: 10.2519/jospt.2014.4791
- Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, van Tulder MW. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015 Feb 18;350:h444. doi: 10.1136/bmj.h444
- Straube S, Harden M, Schröder H, Arendacka B, Fan X, Moore RA, Friede T. Back schools for the treatment of chronic low back pain: possibility of benefit but no convincing evidence after 47 years of research-systematic review and meta-analysis. Pain. 2016 Oct;157(10):2160-2172. doi: 10.1097/j.pain.0000000000000640
- Shanthanna H, Gilron I, Rajarathinam M, AlAmri R, Kamath S, Thabane L, Devereaux PJ, Bhandari M. Benefits and safety of gabapentinoids in chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2017 Aug 15;14(8):e1002369. doi: 10.1371/journal.pmed.1002369
- Muehlbacher M, Nickel MK, Kettler C, Tritt K, Lahmann C, Leiberich PK, Nickel C, Krawczyk J, Mitterlehner FO, Rother WK, Loew TH, Kaplan P. Topiramate in treatment of patients with chronic low back pain: a randomized, double-blind, placebo-controlled study. Clin J Pain. 2006 Jul-Aug;22(6):526-31. doi: 10.1097/.ajp.0000192516.58578.a4
- Franke H, Franke JD, Fryer G. Osteopathic manipulative treatment for nonspecific low back pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2014 Aug 30;15:286. doi: 10.1186/1471-2474-15-286
- Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J, Carragee EJ, Grabois M, Murphy DR, Resnick DK, Stanos SP, Shaffer WO, Wall EM; American Pain Society Low Back Pain Guideline Panel. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society. Spine (Phila Pa 1976). 2009 May 1;34(10):1066-77. doi: 10.1097/BRS.0b013e3181a1390d
- Machado GC, Ferreira PH, Yoo RI, Harris IA, Pinheiro MB, Koes BW, van Tulder MW, Rzewuska M, Maher CG, Ferreira ML. Surgical options for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016 Nov 1;11(11):CD012421. doi: 10.1002/14651858.CD012421
- Syrmou E, Tsitsopoulos PP, Marinopoulos D, Tsonidis C, Anagnostopoulos I, Tsitsopoulos PD. Spondylolysis: a review and reappraisal. Hippokratia. 2010 Jan;14(1):17-21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2843565
- Jinkins JR, Matthes JC, Sener RN, Venkatappan S, Rauch R. Spondylolysis, spondylolisthesis, and associated nerve root entrapment in the lumbosacral spine: MR evaluation. AJR Am J Roentgenol. 1992 Oct;159(4):799-803. doi: 10.2214/ajr.159.4.1529846
- Dunn AJ, Campbell RS, Mayor PE, Rees D. Radiological findings and healing patterns of incomplete stress fractures of the pars interarticularis. Skeletal Radiol. 2008 May;37(5):443-50. doi: 10.1007/s00256-008-0449-0
- Standaert CJ, Herring SA. Spondylolysis: a critical review. Br J Sports Med. 2000 Dec;34(6):415-22. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1724260/pdf/v034p00415.pdf
- Mukhopadhyay S, Kamath S, Mukherjee K, Batraa S, Ahuja S. Incidence of pars defects in adolescent idiopathic scoliosis: an MRI study. Acta Orthop Traumatol Turc. 2011;45(4):209-14. doi: 10.3944/AOTT.2011.2555
- Mushtaq, Raza & Porrino, Jack & Guzmán Pérez-Carrillo, Gloria. (2018). Imaging of Spondylolysis: The Evolving Role of Magnetic Resonance Imaging. PM&R. 10. 10.1016/j.pmrj.2018.02.001
- Spondylolisthesis. https://radiopaedia.org/articles/spondylolisthesis-1?lang=us
- Tenny S, Gillis CC. Spondylolisthesis. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767
- McClellan JW 3rd, Vernon BA, White MA, Stamm S, Ryschon KL. Should 25-hydroxyvitamin D and bone density using DXA be tested in adolescents with lumbar stress fractures of the pars interarticularis? J Spinal Disord Tech. 2012 Dec;25(8):426-8. doi: 10.1097/BSD.0b013e31823f324f
- Buckwalter JA, Saltzman C, Brown T. The impact of osteoarthritis: implications for research. Clin Orthop Relat Res. 2004 Oct;(427 Suppl):S6-15. doi: 10.1097/01.blo.0000143938.30681.9d
- Heine, J. Über die Arthritis deformans. Virchows Arch. path Anat. 260, 521–663 (1926). https://doi.org/10.1007/BF01889359
- Miller JA, Schmatz C, Schultz AB. Lumbar disc degeneration: correlation with age, sex, and spine level in 600 autopsy specimens. Spine (Phila Pa 1976). 1988 Feb;13(2):173-8.
- Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt KF, Nerlich AG. Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo Award in basic science. Spine (Phila Pa 1976). 2002 Dec 1;27(23):2631-44. doi: 10.1097/00007632-200212010-00002
- Kramer PA. Prevalence and distribution of spinal osteoarthritis in women. Spine (Phila Pa 1976). 2006 Nov 15;31(24):2843-8. doi: 10.1097/01.brs.0000245854.53001.4e
- van der Kraan PM, van den Berg WB. Osteophytes: relevance and biology. Osteoarthritis Cartilage. 2007 Mar;15(3):237-44. https://doi.org/10.1016/j.joca.2006.11.006
- Humzah MD, Soames RW. Human intervertebral disc: structure and function. Anat Rec. 1988 Apr;220(4):337-56. doi: 10.1002/ar.1092200402
- Videman T, Battié MC. The influence of occupation on lumbar degeneration. Spine (Phila Pa 1976). 1999 Jun 1;24(11):1164-8. doi: 10.1097/00007632-199906010-00020
- Hassett G, Hart DJ, Manek NJ, Doyle DV, Spector TD. Risk factors for progression of lumbar spine disc degeneration: the Chingford Study. Arthritis Rheum. 2003 Nov;48(11):3112-7. doi: 10.1002/art.11321
- Spector TD, MacGregor AJ. Risk factors for osteoarthritis: genetics. Osteoarthritis Cartilage. 2004;12 Suppl A:S39-44. doi: 10.1016/j.joca.2003.09.005
- Videman T, Battié MC, Ripatti S, Gill K, Manninen H, Kaprio J. Determinants of the progression in lumbar degeneration: a 5-year follow-up study of adult male monozygotic twins. Spine (Phila Pa 1976). 2006 Mar 15;31(6):671-8. doi: 10.1097/01.brs.0000202558.86309.ea
- Battié MC, Videman T, Gibbons LE, Fisher LD, Manninen H, Gill K. 1995 Volvo Award in clinical sciences. Determinants of lumbar disc degeneration. A study relating lifetime exposures and magnetic resonance imaging findings in identical twins. Spine (Phila Pa 1976). 1995 Dec 15;20(24):2601-12.
- Videman T, Leppävuori J, Kaprio J, Battié MC, Gibbons LE, Peltonen L, Koskenvuo M. Intragenic polymorphisms of the vitamin D receptor gene associated with intervertebral disc degeneration. Spine (Phila Pa 1976). 1998 Dec 1;23(23):2477-85. doi: 10.1097/00007632-199812010-00002
- Hayden JA, van Tulder MW, Malmivaara AV, Koes BW. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005 May 3;142(9):765-75. doi: 10.7326/0003-4819-142-9-200505030-00013
- Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005 May 3;142(9):776-85. doi: 10.7326/0003-4819-142-9-200505030-00014
- Heymans MW, van Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for nonspecific low back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976). 2005 Oct 1;30(19):2153-63. doi: 10.1097/01.brs.0000182227.33627.15
- van Tulder MW, Koes B, Malmivaara A. Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J. 2006 Jan;15 Suppl 1(Suppl 1):S64-81. doi: 10.1007/s00586-005-1048-6
- Borman P, Keskin D, Bodur H. The efficacy of lumbar traction in the management of patients with low back pain. Rheumatol Int. 2003 Mar;23(2):82-6. doi: 10.1007/s00296-002-0249-0
- Deyo RA, Walsh NE, Martin DC, Schoenfeld LS, Ramamurthy S. A controlled trial of transcutaneous electrical nerve stimulation (TENS) and exercise for chronic low back pain. N Engl J Med. 1990 Jun 7;322(23):1627-34. doi: 10.1056/NEJM199006073222303
- Milne S, Welch V, Brosseau L. Transcutaneous electrical nerve stimulation (TENS) for chronic low back pain, vol. 4. Oxford: The Cochrane Library; 2004.
- Furlan AD, Brosseau L, Imamura M, Irvin E. Massage for low-back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976). 2002 Sep 1;27(17):1896-910. doi: 10.1097/00007632-200209010-00017
- Boswell MV, Singh V, Staats PS, Hirsch JA. Accuracy of precision diagnostic blocks in the diagnosis of chronic spinal pain of facet or zygapophysial joint origin. Pain Physician. 2003 Oct;6(4):449-56. https://www.painphysicianjournal.com/current/pdf?article=MTY3&journal=17
- Sehgal N, Dunbar EE, Shah RV, Colson J. Systematic review of diagnostic utility of facet (zygapophysial) joint injections in chronic spinal pain: an update. Pain Physician. 2007 Jan;10(1):213-28. https://www.painphysicianjournal.com/current/pdf?article=Nzc5&journal=31
- Boswell MV, Colson JD, Sehgal N, Dunbar EE, Epter R. A systematic review of therapeutic facet joint interventions in chronic spinal pain. Pain Physician. 2007 Jan;10(1):229-53. https://www.painphysicianjournal.com/current/pdf?article=Nzgw&journal=31
- Fuchs S, Erbe T, Fischer HL, Tibesku CO. Intraarticular hyaluronic acid versus glucocorticoid injections for nonradicular pain in the lumbar spine. J Vasc Interv Radiol. 2005 Nov;16(11):1493-8. doi: 10.1097/01.RVI.0000175334.60638.3F
- Carette S, Marcoux S, Truchon R, Grondin C, Gagnon J, Allard Y, Latulippe M. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engl J Med. 1991 Oct 3;325(14):1002-7. doi: 10.1056/NEJM199110033251405
- Manchikanti L, Pampati V, Bakhit CE, Rivera JJ, Beyer CD, Damron KS, Barnhill RC. Effectiveness of lumbar facet joint nerve blocks in chronic low back pain: a randomized clinical trial. Pain Physician. 2001 Jan;4(1):101-17. https://www.painphysicianjournal.com/current/pdf?article=Mjk5&journal=6
- Schneider BJ, Maybin S, Sturos E. Safety and Complications of Cervical Epidural Steroid Injections. Phys Med Rehabil Clin N Am. 2018 Feb;29(1):155-169. doi: 10.1016/j.pmr.2017.08.012
- Sassack B, Carrier JD. Anatomy, Back, Lumbar Spine. [Updated 2021 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557616
- Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015 Dec;1(1):2-18. doi: 10.3978/j.issn.2414-469X.2015.10.05
- Rao RD, Currier BL, Albert TJ, Bono CM, Marawar SV, Poelstra KA, Eck JC. Degenerative cervical spondylosis: clinical syndromes, pathogenesis, and management. J Bone Joint Surg Am. 2007 Jun;89(6):1360-78. doi: 10.2106/00004623-200706000-00026
- Cheung JP, Luk KD. Complications of Anterior and Posterior Cervical Spine Surgery. Asian Spine J. 2016 Apr;10(2):385-400. doi: 10.4184/asj.2016.10.2.385
- Williams MG, Wafai AM, Podmore MD. Functional outcomes of laminectomy and laminotomy for the surgical management lumbar spine stenosis. J Spine Surg. 2017 Dec;3(4):580-586. doi: 10.21037/jss.2017.10.08