Sutton disease 2
Sutton disease 2 also known as recurrent aphthous ulcers, canker sores or aphthous stomatitis, is characterized by the recurring eruption of painful inflamed ulcers in the mouth (stomatitis) 1. There may be one or several discrete, shallow, painful ulcers of varying sizes that are visible on the unattached oral mucous membranes (lips, soft palate, and throat). Individual ulcers typically last 7-10 days and heal without scarring. Larger ulcers may last several weeks to months and can scar when healing 2. The exact cause of Sutton disease 2 is not fully understood, although it may be due to an abnormal immune response to the bacteria that are normally in the mouth.
Sutton disease 2 affects more adult females than males. However, before puberty, males and females are equally affected 1. Sutton disease 2 occurs most frequently in malnourished children or adults whose immune systems are suppressed (i.e., by chemotherapy) or compromised (i.e., acquired immune deficiency syndrome).
Various kinds of medications can be used to treat aphthous ulcers. They can be applied to the sores in the form of a gel, cream, paste or spray. Some are also available as a mouthwash or lozenges:
- Local anesthetics: Local anesthetics like lidocaine or benzocaine can dull the pain. They are typically applied to the sores as a gel or cream.
- Anti-inflammatory drugs: Some medicines contain the painkiller diclofenac, which is an nonsteroidal anti-inflammatory drug (NSAID). Diclofenac can relieve pain and reduce inflammation.
- Antiseptic drugs: Mouthwashes with germ-killing ingredients like chlorhexidine or triclosan are used to stop germs from growing in the wound and delaying the healing process or making the inflammation worse.
- Plant-based remedies (astringents): Tinctures made from myrrh or rhubarb root help some people. These plant-based remedies cause the blood vessels in the mucous membranes to become narrower, which is believed to relieve the pain.
If treating aphthous ulcers with local anesthetics, painkillers or antiseptic medications doesn’t help, you can apply steroid creams. If those aren’t effective or if the sores are very severe, it’s a good idea to see a doctor or dentist. They can cauterize (destroy) the inflamed tissue – for instance, using a silver nitrate solution or laser treatment.
What is the differential diagnosis of Sutton disease 2?
Other causes of mouth ulcer should be considered, including:
- Herpes simplex
- Herpangina
- Erythema multiforme
- Fixed drug eruption.
Primary oral herpes simplex may mimic recurrent aphthous stomatitis but usually occurs in younger children, always involves the gingiva and may affect any keratinized mucosa (hard palate, attached gingiva, dorsum of tongue), and is associated with systemic symptoms. Viral culture can be done to identify herpes simplex. Recurrent herpetic lesions are usually unilateral.
Similar recurrent episodes, often with multiple ulcers, can occur with Behçet disease, inflammatory bowel disease, celiac disease, HIV infection, periodic fevers with aphthous stomatitis, pharyngitis, and adenitis (PFAPA) syndrome, and nutritional deficiencies; these conditions generally have systemic symptoms and signs. Isolated recurrent oral ulcers can occur with herpes infection, HIV, and, rarely, nutritional deficiency. Viral testing and serum hematologic tests can identify these conditions.
Drug reactions may mimic Sutton disease 2 but are usually temporally related to ingestion. However, reactions to foods or dental products may be difficult to identify; sequential elimination may be necessary.
Sutton disease 2 causes
The exact cause of Sutton disease 2 is not known, but recurrent aphthous stomatitis tends to run in families 3. Approximately 40% of people who get aphthous ulcers have a family history of aphthous ulcer. Several studies suggest that aphthous stomatitis may occur because of an abnormal immune response to the bacteria that are normally present in the mouth. The damage is predominately T–cell-mediated. Cytokines, such as IL-2, IL-10, and particularly TN-alpha, play a role 3. Deficiencies of iron (Fe), vitamin B12, and folic acid seem to increase an individual’s susceptibility to Sutton disease 2. Stress and local injury may also be involved. There seems to be no relationship between Sutton disease 2 and menstruation, pregnancy, and/or menopause, nor is it caused by herpes virus, which is the main cause of common canker sores 1.
Predisposing factors include 3:
- Oral trauma
- Stress
- Foods, particularly chocolate, coffee, peanuts, eggs, cereals, almonds, strawberries, cheese, and tomatoes
Allergy does not seem to be involved.
Sutton disease 2 symptoms
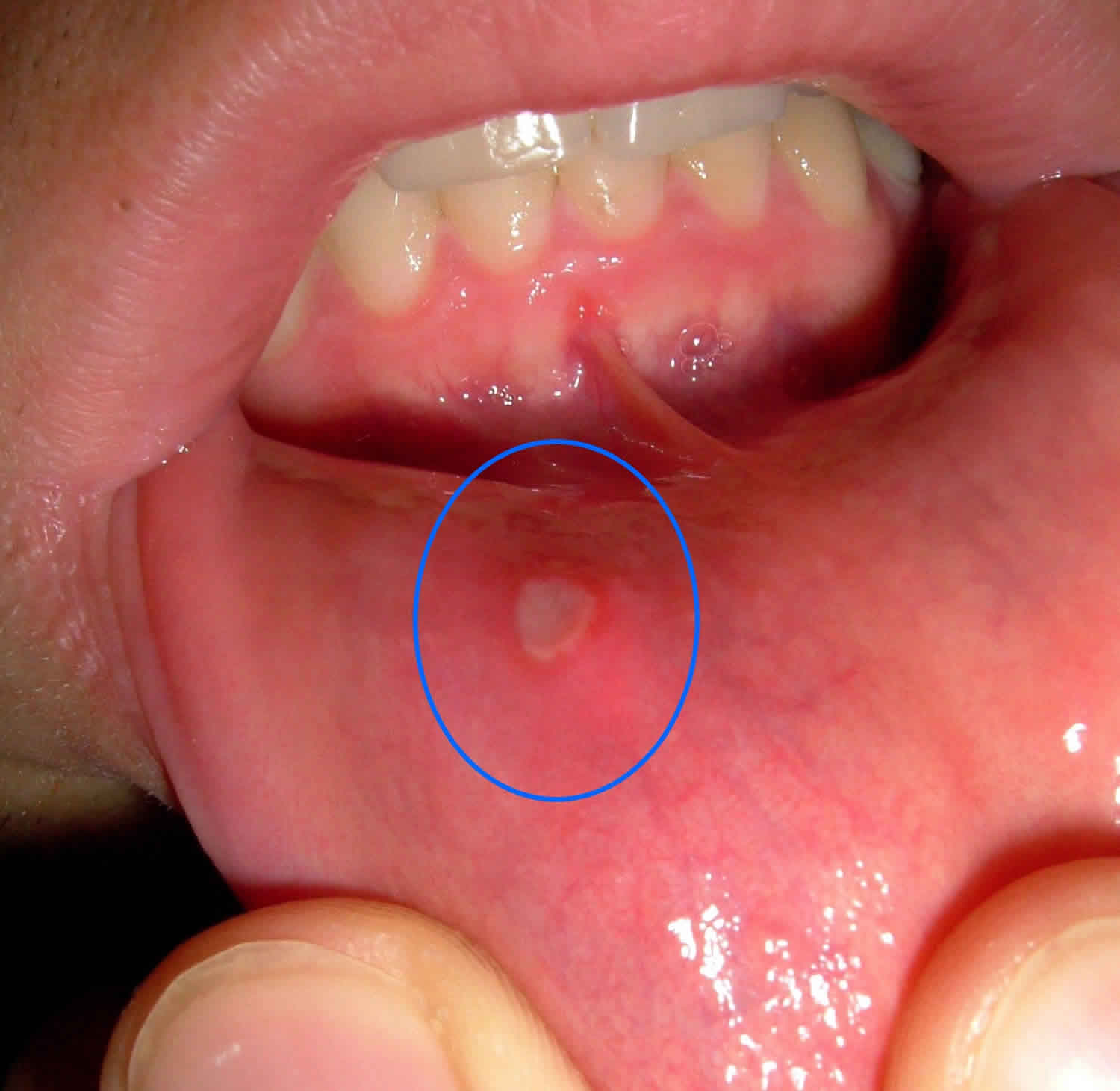
The symptoms of Sutton disease 2 include red, painful ulcers that may appear on the tongue, the lining of the cheeks (buccal mucosa), floor of the mouth, and back of the throat (soft palate). Ulcers may develop in clusters or appear as single lesions scattered throughout the mouth. As many as 15 sores may be present at once. Individuals with Sutton disease 2 typically experience recurring episodes of mouth sores, usually with 2 to 3 sores during each attack.
The ulcers associated with Sutton disease 2 may vary in size. When the mouth ulcers associated with Sutton disease first erupt, they usually appear as red (inflamed) shallow erosions. Sores less than 1 centimeter in size are considered small or “minor” ulcers. These smaller sores are the most common form of the disease and usually last for 10 to 14 days. Smaller lesions do not usually leave scars. In some cases larger or “major” ulcers may develop lasting for weeks or months. Typically, these larger sores leave scars.
In severe cases, other symptoms of Sutton disease 2 may include a general feeling of weakness (malaise), fever, and swollen lymph nodes around the neck and head (lymphadenopathy).
Sutton disease 2 diagnosis
Medical history
History of present illness should ascertain the duration of symptoms and whether the patient ever had them previously. Presence and severity of pain should be noted. The relation of symptoms to food, drugs, oral hygiene materials (eg, toothpaste, mouth rinses), and other substances (particularly occupational exposure to chemicals, metals, fumes, or dust) is sought.
Review of systems seeks symptoms of possible causes, including chronic diarrhea and weakness (inflammatory bowel disease, celiac disease); genital lesions (Behçet disease, syphilis); eye irritation (Behçet disease); and weight loss, malaise, and fever (nonspecific chronic illness).
Past medical history should ascertain known conditions that cause oral lesions, including herpes simplex, Behçet disease, inflammatory bowel disease, and risk factors for oral lesions, including immunocompromised state (eg, cancer, diabetes, organ transplant, use of immunosuppressants, HIV infection). Whether chemotherapy or radiation therapy has ever been used to manage cancer needs to be determined. Drug history should note all recent drugs used. History of tobacco use should be noted. Social history should include sexual contact, particularly oral sex, unprotected sex, and sex with multiple partners.
Physical examination
Vital signs are reviewed for fever. The patient’s general appearance is noted for lethargy, discomfort, or other signs of significant systemic illness.
The mouth is inspected for the location and nature of any lesions.
The skin and other mucosal surfaces (including the genitals) are inspected for any lesions, rash, petechiae, or desquamation. Any bullous lesions are rubbed for the Nikolsky sign (upper layers of epidermis move laterally with slight pressure or rubbing of skin adjacent to a blister).
Red flags
The following findings are of particular concern:
- Fever
- Cutaneous bullae
- Ocular inflammation
- Immunocompromise
Laboratory tests
Most people affected by occasional minor aphthous ulceration do not require tests. They are undertaken if there are recurrent attacks of multiple or severe oral ulcers or complex aphthosis.
Blood tests may include:
- Blood count, iron, B12 and folate studies
- Gluten antibody tests for coeliac disease
- Fecal calprotectin test for Crohn disease
Swabs for microbiology evaluate the presence of Candida albicans, Herpes simplex virus and Vincent’s organisms.
Sutton’s disease treatment
Most recurrent minor aphthous ulcers heal within 1–2 weeks without any treatment. The main goal of treatment is to lessen pain and discomfort and promote healing. The symptomatic treatment of Sutton disease 2 involves the application of topical anesthetic (i.e., lidocaine viscous) directly on the affected areas or a thorough mouth rinsing with a special anesthetic solution that helps to reduce irritation and pain. The application of topical steroids may also give symptomatic relief. A dental protective paste (i.e., triamcinolone acetonide or Orabase) may prevent teeth, dental appliances and oral fluids from irritating the ulcers. Tinctures made from myrrh or rhubarb root help some people. These plant-based remedies cause the blood vessels in the mucous membranes to become narrower, which is believed to relieve the pain 4.
In severe cases of Sutton disease 2, oral and topical steroids may be administered. A mouth rinse that contains the antibiotic tetracycline may also be prescribed to heal painful mouth sores. However, the use of antibiotics and steroids may promote the development of the fungus candida that can cause thrush or oral candidiasis.
If treatment is started early, symptomatic relief may occur during the first day of treatment and new lesions may be healed. Recurring oral ulcers generally require renewed efforts at treatment. Other treatment is symptomatic and supportive.
Prescribed medicines for aphthous ulcer
Topical prescription medicines include:
- Tetracycline suspension as a mouthwash
- Topical corticosteroids as lotions, creams or paste, often triamcinolone in dental paste
- Calcineurin inhibitors: topical pimecrolimus or tacrolimus.
In severe cases, particularly if there are systemic symptoms, anti-inflammatory oral medications may be considered (off-label use):
- Tetracycline, e.g. doxycycline 50-100mg daily for 3-6 months or longer.
- Dapsone
- Colchicine
- Systemic steroids
- Immunosuppressive agents such as azathioprine, methotrexate, ciclosporin
- Apremilast, which has been approved in the USA to treat oral ulcers in Behçet disease
- Tumor necrosis factor (TNF) antagonists (adalimumab, etanercept, infliximab)
- Thalidomide.
- Sutton Disease II. https://rarediseases.org/rare-diseases/sutton-disease-ii
- Aphthous Stomatitis. https://emedicine.medscape.com/article/1075570-overview
- Recurrent Aphthous Stomatitis. https://www.msdmanuals.com/en-kr/professional/dental-disorders/symptoms-of-dental-and-oral-disorders/recurrent-aphthous-stomatitis
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Canker sores (mouth ulcers): What can you do if you have a canker sore? 2019 Aug 15. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546251