Tatton-Brown Rahman syndrome
Tatton-Brown Rahman syndrome also known as DNMT3A overgrowth syndrome, Rahman syndrome or TBRS, is a syndrome that produces faster than normal growth both before and after birth, resulting in a severely increased height throughout the child’s life, subtle differences in facial features, and intellectual disability. Tatton-Brown-Rahman syndrome is characterized by tall stature, head size overgrowth (macrocephaly), a distinctive facial appearance, and intellectual disability 1.
Individuals with Tatton-Brown Rahman syndrome are often longer than normal at birth and are taller than their peers throughout life. Many affected individuals become overweight in late childhood or adolescence. They may also have an abnormally large head size (macrocephaly).
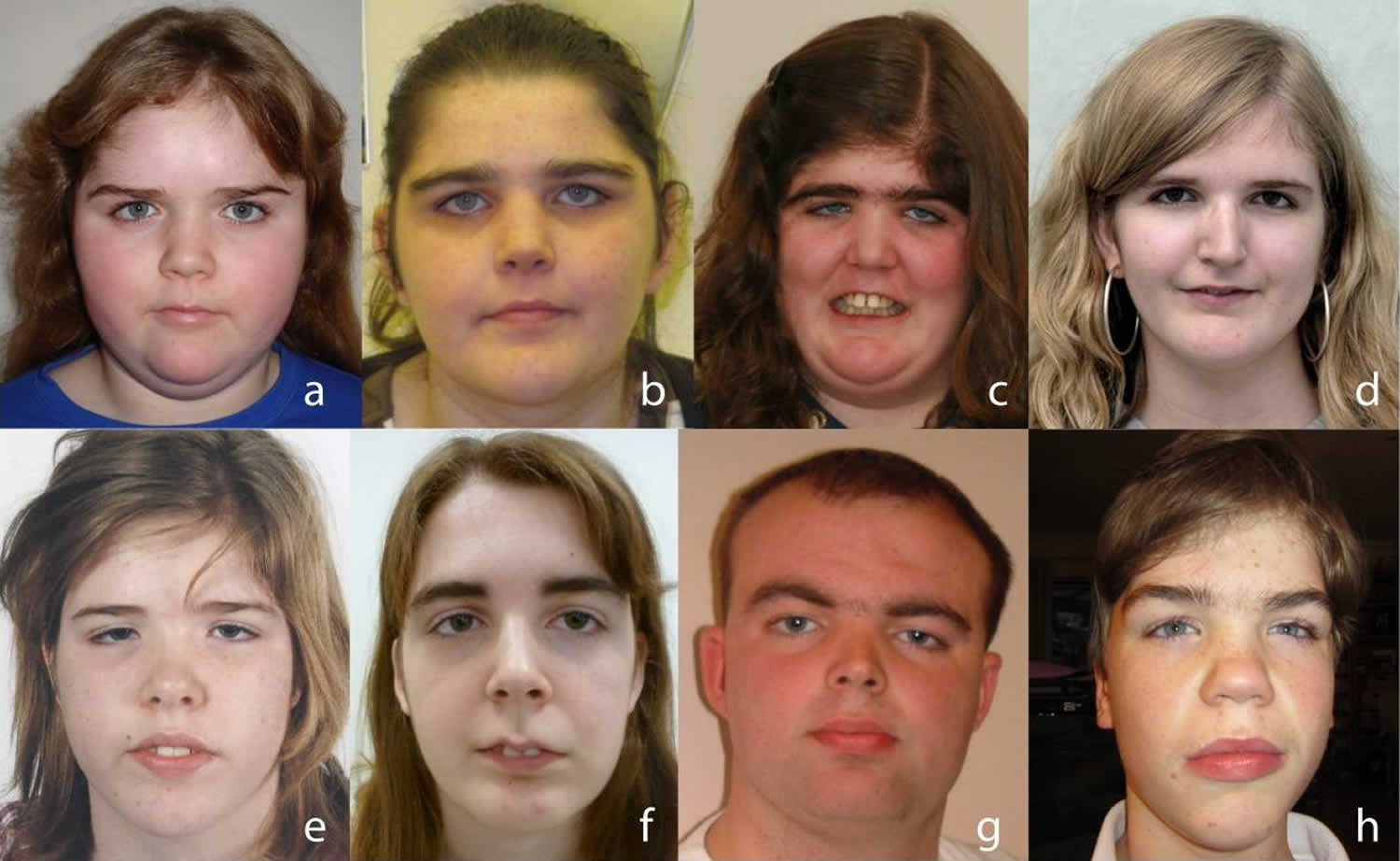
The characteristic facial appearance of individuals with Tatton-Brown Rahman syndrome includes a round face; thick, horizontal eyebrows; and narrowed openings of the eyes (narrowed palpebral fissures). Additionally, the upper front teeth are often larger than normal.
Intellectual disability in Tatton-Brown Rahman syndrome ranges from mild to severe. Individuals may have features of autism spectrum disorder, which are characterized by impaired communication and socialization skills.
Individuals with Tatton-Brown Rahman syndrome may have other signs and symptoms, including a rounded upper back that also curves to the side (kyphoscoliosis), heart defects, flat feet (pes planus), weak muscle tone (hypotonia), or joints that are loose and very flexible (hypermobile joints). Psychological disorders such as depression, anxiety, or obsessive-compulsive disorder can also occur in Tatton-Brown Rahman syndrome.
Some patients may have increased susceptibility to the development of acute myeloid leukemia (AML), particularly if they have DNMT3A mutations affecting the R882 residue 2.
Tatton-Brown Rahman syndrome was first identified in 13 individuals by Dr. Katrina Tatton-Brown, Dr. Nazneen Rahman, and colleagues in 2014 as part of a research study, based in London, into the genetic causes of overgrowth 1. Since then, a number of other clinicians around the world have identified additional Tatton-Brown Rahman syndrome individuals with pathogenic variants in DNMT3A gene. In 2018, Dr. Tatton-Brown and her collaborators described 55 individuals with the syndrome, including the original 13. As of 2020, roughly 150 people have been diagnosed with TBRS 3. It is not clear how common the syndrome is, but many more individuals are likely to be diagnosed as whole genome sequencing methods becomes more accessible.
There is currently no cure for Tatton Brown Rahman syndrome, and clinical care is focused on managing the particular clinical findings in each individual.
Figure 1. Tatton-Brown Rahman syndrome
Footnote: Characteristic facial appearance Tatton-Brown Rahman syndrome (DNMT3A overgrowth syndrome).
[Source 1 ]Tatton-Brown Rahman syndrome causes
Mutations in the DNMT3A (DNA cytosine 5 methyltransferase 3A) gene cause Tatton-Brown Rahman syndrome. The DNMT3A gene provides instructions for making an enzyme called DNA methyltransferase 3 alpha. This enzyme is involved in DNA methylation, which is the addition of methyl groups, consisting of one carbon atom and three hydrogen atoms, to DNA molecules. DNA methylation is important in many cellular functions. These include regulating gene activity and certain chemical reactions and controlling the processing of chemicals that relay signals in the nervous system (neurotransmitters). DNA methyltransferase 3 alpha is particularly important for establishing DNA methylation patterns during development before birth.
Some DNMT3A gene mutations that cause Tatton-Brown Rahman syndrome lead to a decrease in normal enzyme function. As a result, there is a reduction in DNA methylation, particularly affecting DNA methylation before birth. It is unclear how other mutations affect protein function. Decreased DNA methylation likely disrupts the normal regulation of important developmental genes, although how these change cause the specific features of Tatton-Brown Rahman syndrome is unknown.
Tatton-Brown Rahman syndrome inheritance pattern
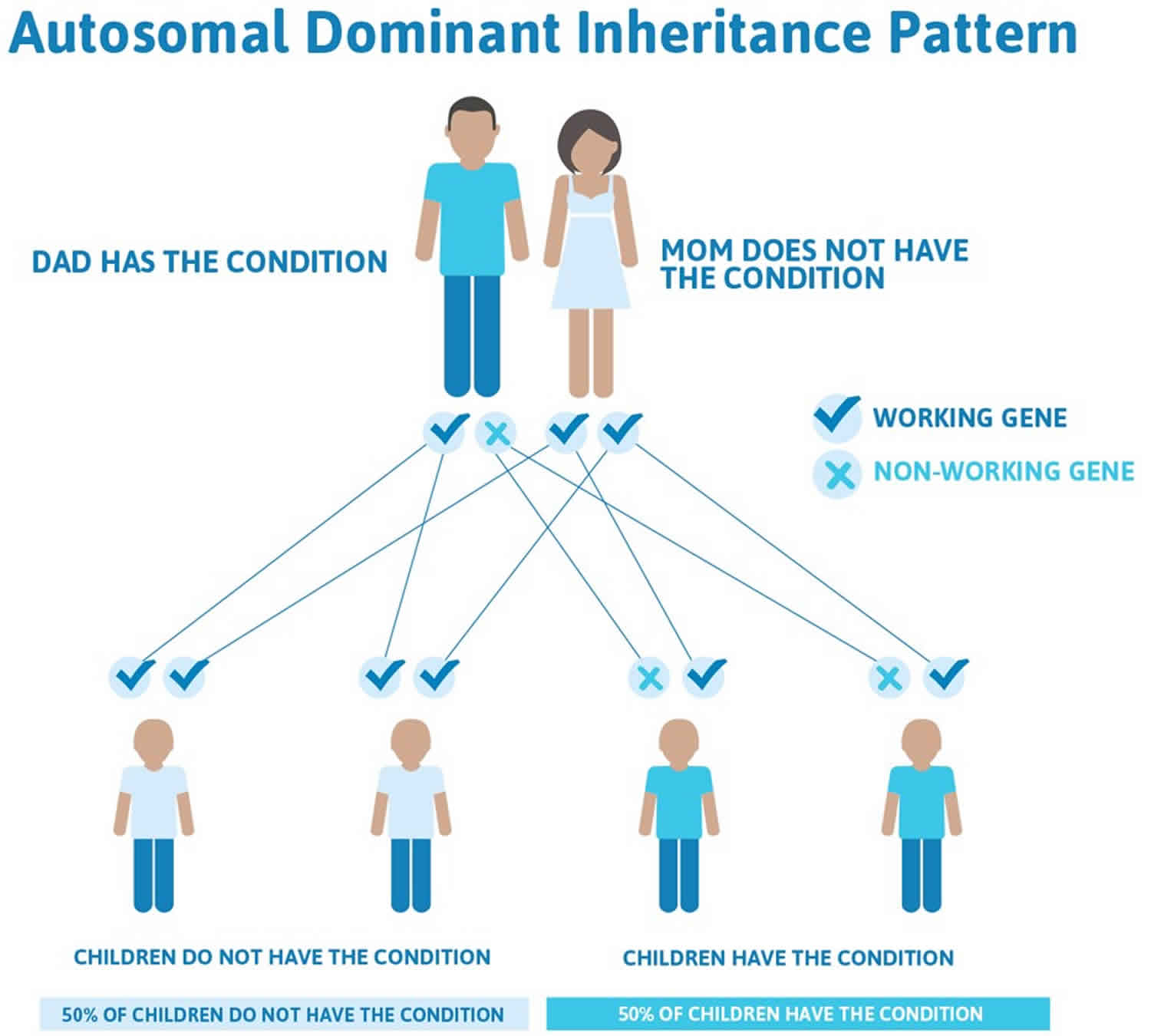
Tatton-Brown Rahman syndrome is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder.
In some cases, an affected person inherits the mutation from one affected parent. Other cases result from new mutations in the gene and occur in people with no history of the disorder in their family (de novo mutation).
Figure 2. Tatton-Brown Rahman syndrome autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Tatton-Brown Rahman syndrome symptoms
The main features of Tatton-Brown Rahman syndrome are overgrowth, intellectual disability, and certain facial characteristics. Children born with Tatton-Brown Rahman syndrome are likely to encounter a number of additional symptoms, aside from the overgrowth. These include a curving of the upper back (kyphoscoliosis), heart defects, flat feet (pes planus), weak muscle tone (hypotonia) and very loose, flexible joints (hypermobile joints). Children with Tatton-Brown Rahman syndrome are also likely to have learning difficulties ranging from mild to severe and there is a high occurrence of difficulties with communication and social skills, similar to those of autism spectrum disorders.
Psychological disorders such as depression, anxiety, or obsessive-compulsive disorder can also occur in Tatton-Brown Rahman syndrome.
Overgrowth
Overgrowth is defined by being at least two standard deviations above average for height and/or head circumference. Overgrowth is the most common aspect of Tatton-Brown Rahman syndrome. Among 55 individuals with Tatton-Brown Rahman syndrome, 44 of them, or 83 percent, had overgrowth, according to a study by Dr. Tatton-Brown and colleagues published in 2018 4. In addition, 67 percent of people in the study were obese.
Intellectual disability
In the 2018 study 5, all 55 individuals had intellectual disability, in 18 percent of them it was mild, in 65 percent moderate, and in 16 percent it was severe. Children with mild intellectual disability needed some supports in school but attended a mainstream classroom and adults with mild intellectual disability could live independently with some additional help. Those with moderate and severe intellectual disability required more intensive special education and supports as adults. A study in 2019 of 18 individuals identified a similar finding, with 15 individuals reported as having intellectual disability (ranging from mild to severe) and three individuals who had borderline intellectual functioning. Learning disability is also common among individuals with Tatton-Brown Rahman syndrome.
Facial characteristics
Certain facial characteristics are associated with Tatton-Brown Rahman syndrome, but these are usually more evident in teens and adults rather than children. These may include horizontal and thick eyebrows, narrow eye slits (also called palpebral fissures) that are occasionally deep set and down-slanting, a round face, broad forehead, and large, protruding front teeth (the top incisors), smooth philtrum, and thin upper lip. For the most part, these are subtle characteristics, although it is not uncommon for individuals with Tatton-Brown Rahman syndrome to require extensive orthodontic interventions to correct dental issues.
Joint hypermobility
One of the most common features of Tatton-Brown Rahman syndrome is joint hypermobility, in which the joints are loose, causing double jointedness. This can occasionally lead to joint dislocation, recurring injuries, and a susceptibility to cartilage, tendon, and ligament tears and joint pain.
Low muscle tone
Low muscle tone, or hypotonia, can lead to delayed physical milestones—such as sitting up, crawling, or walking—and poor posture, coordination, and balance. Although uncommon, some individuals with Tatton-Brown Rahman syndrome use a wheelchair. Others have benefited from physical therapy or orthotics.
Kyphoscoliosis
About one-third of individuals with Tatton-Brown Rahman syndrome have reported having kyphoscoliosis, in which the spine curves from side to side and/or from front to back of the torso.
Mental and behavioral health disorders
In 2019, researchers described seven individuals with Tatton-Brown Rahman syndrome who were identified from the Spanish Overgrowth Syndromes Registry 6. Four had one or more neuropsychiatric disorders, including schizophrenia, attention deficit hyperactivity disorder, psychosis, or aggression.
Also in 2019, Dr. Chloe Lane 7 reported on the analysis of 18 people with Tatton-Brown Rahman syndrome and found a heightened prevalence of autistic traits, with eight scoring on the autism spectrum. Parents of children with Tatton-Brown Rahman syndrome have also reported aggressive outbursts, autistic features, and anxiety.
Seizures
Some people with Tatton-Brown Rahman syndrome have experienced seizures with and without a concurrent fever (those that occur in the presence of a fever are called febrile seizures).
The following are less frequently reported than the conditions above:
- Cardiac defects, such as atrial septal defect (a hole in the heart)
- Brain malformations, such as enlarged ventricles (ventriculomegaly) and Chiari formation (in which the brain dips down into the spinal column)
- Undescended testes (cryptorchidism)
- Strabismus (crossed eye)
- Sleep disorder including sleep apnea
- Hyperphagia, or increased appetite
- Insensitivity to pain
Tatton-Brown Rahman syndrome diagnosis
A genetic test to check the mutation in the DNMT3A gene can confirm a clinical diagnosis in most cases.
Tatton-Brown Rahman syndrome treatment
As Tatton-Brown Rahman syndrome is extremely new, medical understanding is limited, but growing all the time, treatment would focus on symptom management.
Tatton-Brown Rahman syndrome life expectancy
The majority of individuals with Tatton-Brown Rahman syndrome are healthy and do not require intensive clinical follow up. As Tatton-Brown Rahman syndrome is extremely new, there is currently no life expectancy data. If you need medical advice, you can look for doctors or other healthcare professionals who have experience with Tatton-Brown Rahman syndrome. You may want to checkout the Tatton-Brown Rahman syndrome community (https://tbrsyndrome.org).
References- Tatton-Brown K, Seal S, Ruark E, et al. Mutations in the DNA methyltransferase gene DNMT3A cause an overgrowth syndrome with intellectual disability [published correction appears in Nat Genet. 2014 Jun;46(6):657]. Nat Genet. 2014;46(4):385-388. doi:10.1038/ng.2917 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3981653
- Hollink IHIM, van den Ouweland AMW, Beverloo HB, et al. : Acute myeloid leukaemia in a case with Tatton-Brown-Rahman syndrome: the peculiar DNMT3A R882 mutation. 2017;54(12):805–808. 10.1136/jmedgenet-2017-104574
- Tatton Brown Rahman Syndrome. https://tbrsyndrome.org/about-tbrs
- Tatton-Brown K, Zachariou A, Loveday C et al. The Tatton-Brown-Rahman Syndrome: A clinical study of 55 individuals with de novo constitutive DNMT3A variants [version 1; peer review: 3 approved]. Wellcome Open Res 2018, 3:46 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5964628/pdf/wellcomeopenres-3-15708.pdf
- Tatton-Brown K, et al. The Tatton-Brown-Rahman Syndrome: a clinical study of 55 individuals with de novo constitutive DNMT3A variants. Wellcome Open Res. 2018;3:46. doi: 10.12688/wellcomeopenres.14430.1
- Tenorio, J., Alarcón, P., Arias, P. et al. Further delineation of neuropsychiatric findings in Tatton-Brown-Rahman syndrome due to disease-causing variants in DNMT3A: seven new patients. Eur J Hum Genet 28, 469–479 (2020). https://doi.org/10.1038/s41431-019-0485-3
- Lane, C., Tatton‐Brown, K. and Freeth, M. (2020), Tatton‐Brown‐Rahman syndrome: cognitive and behavioural phenotypes. Dev Med Child Neurol, 62: 993-998. doi:10.1111/dmcn.14426