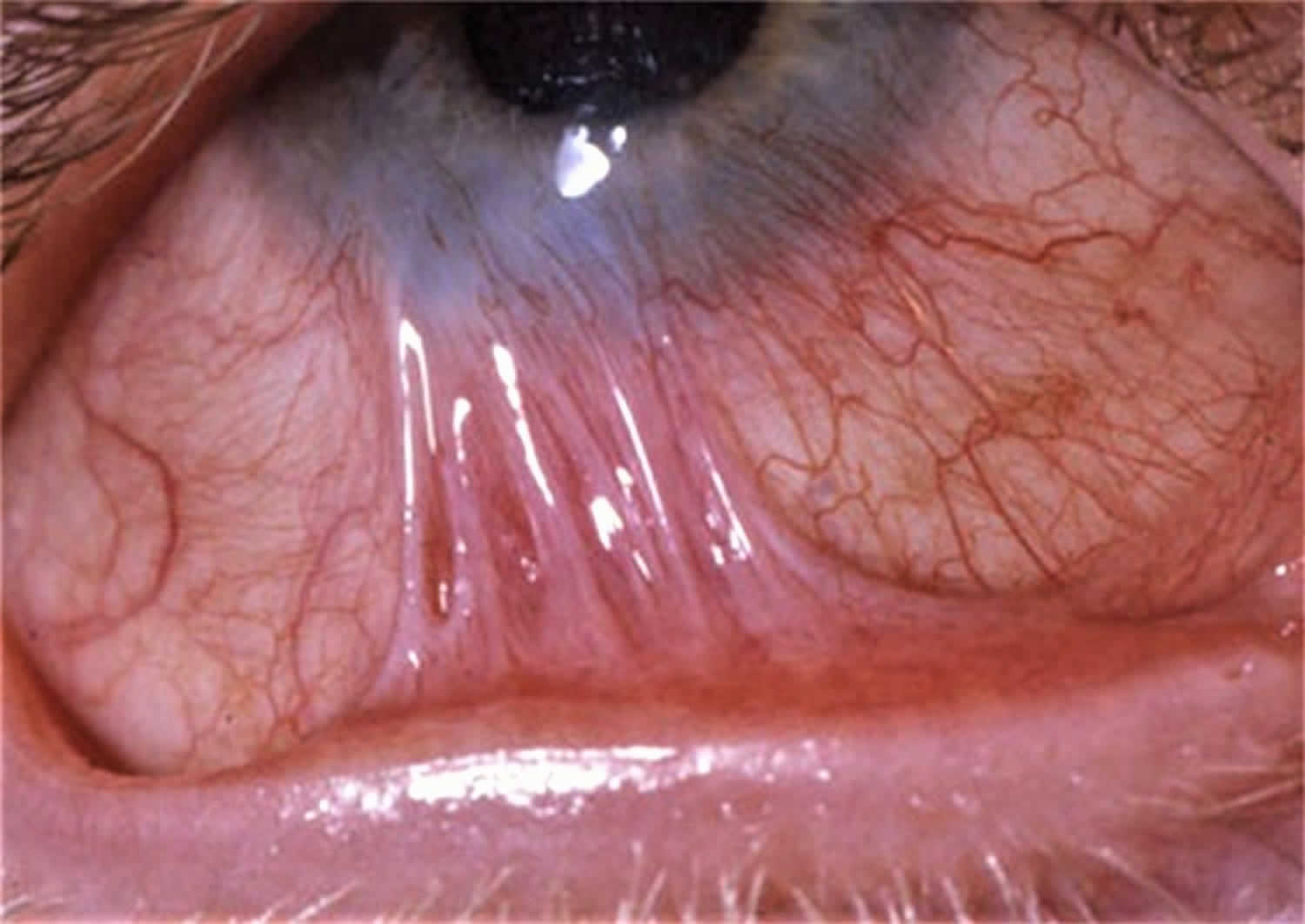
Symblepharon
Symblepharon is the partial or complete adhesion of the palpebral conjunctiva to the bulbar conjunctiva 1. The cornea may or may not be involved, and the conjunctival fornix may become shallow or obliterated. Signs and symptoms of symblepharon include fibrous adhesions between the palpebral conjunctiva and the bulbar conjunctiva, eye redness, burning and tearing, photophobia, diplopia, restricted extraocular motility, lagophthalmos, entropion, and cosmetic considerations 1.
Symblepharon can be caused by some eye diseases (such as trachoma), trauma to the eye 2, chemical burns (alkali burn), keratitis, conjunctival inflammation (bacterial, viral, chlamydial) or sarcoidosis 3.
Symblepharon causes
Symblepharon is an external eye finding in which an adhesion forms between the palpebral conjunctiva and bulbar conjunctiva 4. There are many causes of symblepharon, which is typically a response to trauma or inflammation. In no particular order, here are some of those causes 5:
- Ocular cicatricial pemphigoid
- Pseudopemphigoid conditions
- Stevens-Johnson syndrome
- Trauma
- Conjunctival burns
- Atopic keratoconjunctivitis
- Porphyria cutanea tarda
- Rosacea
- Epidemic keratoconjunctivitis
- Xeroderma pigmentosum
- Squamous papilloma of the conjunctiva
Symblepharon treatment
Conventional management of symptomatic symblepharon varies from frequent ocular lubrication using artificial tears and/or ointment, to occlusion of the tear drainage duct, therapeutic bandage contact or scleral lenses, symblepharon rings or dishes, or bio-tissue bandages.
Symblepharon surgery
Various surgical interventions are used to treat symptomatic symblepharon 6. The conventional surgical approach is reconstruction of the ocular surface by symblepharon lysis and buccal mucosal (palate, lip) graft or amniotic membrane transplantation 7. However, this approach is associated with recurrence.
Surgical intervention involves symblepharon lysis, buccal mucosal grafts, conjunctival autografts, or amniotic membrane transplantation. Buccal mucosal grafts are easily harvested without substantial scarring, and mucous membrane from the lip contains goblet cells that may stabilize the tear film by contributing mucin in the eye 8. Conjunctival autograft is a safe and quick procedure for ocular surface reconstruction that involves resecting conjunctiva and transplanting it to the affected area. Amniotic membrane transplantation supports epithelialization by promoting migration, adhesion, and differentiation of epithelia cells, and it suppresses the immune and inflammatory response 9.
This case report 1 indicates that the combination of buccal mucosal grafts and a reversed split-thickness skin graft represents a novel technique for the treatment of recurrent symblepharon. In the case report, the patient underwent 2 surgeries for reconstruction of the ocular surface. The first surgery used a free conjunctival graft from the contralateral eye, and the second surgery used buccal mucosal transplantation with a graft obtained from the lip. As symblepharon recurred following these 2 approaches, the patient received ocular reconstruction with buccal mucosal and reverse split-thickness skin grafts. The skin graft was slightly smaller than the defect, so as to provide the necessary tension. External pressure, edge stitching, and fixture with percutaneous sutures were used to stabilize the graft. Reversed split-thickness skin grafts are widely applied in reconstructive surgery as they can be harvested in large amounts and have a good survival rate; however, they may lack moisture and contract during healing, and there may be substantial morbidity at the donor site 10. In this case, the groin was large enough to provide a graft that was supportive of the eyelid and nonadhesive. Reversal of the skin graft allowed integration of the mucous surface in the recipient bed. The technique achieved good anatomical and functional reconstruction and provided the opportunity for corneal transplantation and restoration of vision 1.
References- Li T, Shao Y, Lin Q, Zhang D. Reversed skin graft combining with lip mucosa transplantation in treating recurrent severe symblepharon: A case report. Medicine (Baltimore). 2018;97(35):e12168. doi:10.1097/MD.0000000000012168 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6393138
- Symblepharon. https://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/symblepharon.html
- Kelmenson AT, Oliver SC, Durairaj VD. Sarcoid-induced symblepharon. Indian J Ophthalmol. 2008;56(4):344–345. doi:10.4103/0301-4738.41430
- Basic and Clinical Science Course, Section 8: External Disease and Cornea. American Academy of Ophthalmology, 2017-2018 edition.
- Causes of Symblepharon. https://www.ophthalmologyreview.org/articles/causes-of-symblepharon
- Kheirkhah A, Ghaffari R, Kaghazkanani R, et al. A combined approach of amniotic membrane and oral mucosa transplantation for fornix reconstruction in severe symblepharon. Cornea 2013;32:155–60.
- Kheirkhah A, Blanco G, Casas V, et al. Surgical strategies for fornix reconstruction based on symblepharon severity. Am J Ophthalmol 2008;146:266–75.
- Iyer G, Pillai VS, Srinivasan B, et al. Mucous membrane grafting for lid margin keratinization in Stevens–Johnson syndrome: results. Cornea 2010;29:146–51.
- El Gendy NMS. Use of amniotic membrane grafting to cover surgically induced superficial keratectomy during pterygium excision surgery. Egypt Ophthalmol Soc 2013;106:50–3.
- Lee JH, Sa HS, Woo K, et al. Prepuce mucosal graft for forniceal and conjunctival sac reconstruction in surgically intractable symblepharon. Ophthal Plast Reconstr Surg 2011;27:e103–6