What is a thermal burn
Thermal burns are tissue damage caused by any external heat source. This may be in the form of a naked flame from an open fireplace or house fire, a scald from steam, hot or molten liquid, or via direct contact with a hot object such as a hot oven rack or hot cooking pan. Scalds is caused by something wet like hot liquids and steam. Other types of burns include radiation burns, sunburn from the sun’s ultraviolet rays, chemical burns and electrical burns.
Building fires and flammable liquids and gases are the most common causes of thermal burns. Another kind is an inhalation injury, caused by breathing smoke. Thermal burns can be minor medical problems or life-threatening emergencies. The treatment of thermal burns depends on the location and severity of the damage. Sunburns and small scalds can usually be treated at home. Deep or widespread thermal burns need immediate medical attention. Some people need treatment at specialized burn centers and months long follow-up care.
Acute thermal burns requiring medical treatment affect nearly half a million Americans each year, with approximately 40,000 hospitalizations and 3,400 deaths annually 1. The survival rate for admitted burn patients has improved consistently over the past four decades 2 and is currently a favorable 97 % for patients admitted to burn centers 3.
There are three types of thermal burns:
- First-degree burns (1st-degree burn). This minor burn affects only the outer layer of the skin (epidermis). It may cause redness and pain.
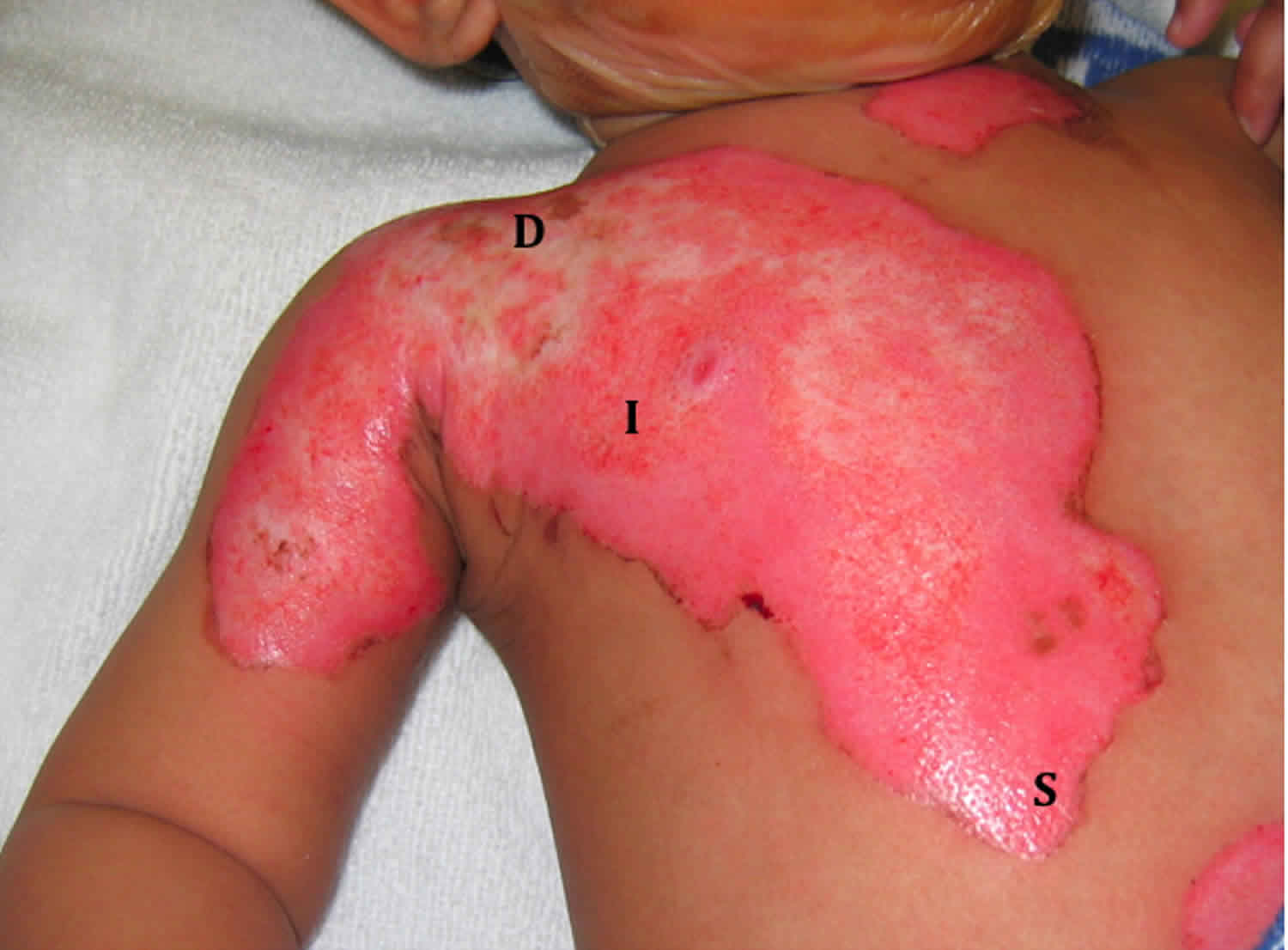
- Second-degree burns (2nd-degree burn). This type of burn affects both the epidermis and the second layer of skin (dermis). It may cause swelling and red, white or splotchy skin. Blisters may develop, and pain can be severe. Deep second-degree burns can cause scarring.
- Third-degree burns (3rd-degree burn). This burn reaches to the fat layer beneath the skin. Burned areas may be black, brown or white. The skin may look leathery. Third-degree burns can destroy nerves, causing numbness.
Burns can cause swelling, blistering, scarring and, in serious cases, shock, and even death. They also can lead to infections because they damage your skin’s protective barrier. Treatment for burns depends on the cause of the burn, how deep it is, and how much of the body it covers. Antibiotic creams can prevent or treat infections. For more serious burns, treatment may be needed to clean the wound, replace the skin, and make sure the patient has enough fluids and nutrition.
Depending on how the burn happened, you may be advised to have an injection to prevent tetanus, a condition caused by bacteria entering a wound. For example, a tetanus injection may be recommended if there’s a chance soil got into the wound.
Your dressing will be regularly checked for signs of infection. It’ll also be regularly changed until the burn’s completely healed.
Minor burns affecting the outer layer of skin and some of the underlying layer of tissue (superficial dermal burns) normally heal in around 14 days, leaving minimal scarring.
If the burn’s moderate or severe, you may be referred to a specialist burn care service.
In some cases, it may be necessary to have surgery to remove the burnt area of skin and replace it with a skin graft taken from another part of your body.
More severe and deeper burns can take months or even years to fully heal, and usually leave some visible scarring.
If someone has a thermal burn or scald:
- Stop the burning process as soon as possible. This may mean removing the person from the area, dousing flames with water, or smothering flames with a blanket. Do not put yourself at risk of getting burnt as well.
- Cool the burn with cool running water for 20 minutes as quickly as possible after the injury. Never use ice, iced water, or any creams or greasy substances like butter.
- While cooling the burn, carefully remove any clothing or jewellery including babies’ nappies, unless it’s attached to the skin. Do not try to remove anything that’s stuck to the burnt skin, as this could cause more damage.
- If you’re cooling a large burnt area, particularly in babies, children and elderly people, be aware that it may cause hypothermia (it may be necessary to stop cooling the burn to avoid hypothermia).
- Call your local emergency services number or seek medical help, if needed.
- Keep yourself or the person warm. Use a blanket or layers of clothing, but avoid putting them on the injured area. Keeping warm will prevent hypothermia, where a person’s body temperature drops below 95 °F (35 °C). This is a risk if you’re cooling a large burnt area, particularly in young children and elderly people.
- Cover the burn loosely with cling film. Put the cling film in a layer over the burn, rather than wrapping it around a limb. A clean clear plastic bag can be used for burns on your hand. If cling film isn’t available, use a clean, dry dressing or non-fluffy material. Do not wrap the burn tightly as swelling may lead to further injury.
- Do not apply creams, lotions or sprays to the burn.
- Treat the pain from a burn with acetaminophen or ibuprofen. Always check the manufacturer’s instructions when using over-the-counter medication. Children under 16 years of age should not be given aspirin.
- Sit upright as much as possible if the face or eyes are burnt. Avoid lying down for as long as possible, as this will help reduce swelling.
For chemical burns, wear protective gloves, remove any affected clothing, and rinse the burn with cool running water for at least 20 minutes to remove the chemical.
If possible, determine the cause of the injury.
In certain situations where a chemical is regularly handled, a specific chemical antidote may be available to use.
Be careful not to contaminate and injure yourself with the chemical, and wear protective clothing if necessary.
Once you have taken these steps, you’ll need to decide whether further medical treatment is necessary.
Seek immediate emergency medical assistance for:
- Burns that cover the hands, arms, feet, face, groin, buttocks, genitals, legs, a major joint or a large area of the body
- Large or deep burns bigger than the affected person’s hand
- Burns of any size that cause white or charred skin
- ALL chemical and electrical burns
- Deep burns, which means burns affecting all layers of the skin or even deeper tissues
- Burns that cause the skin to look leathery
- Burns that appear charred or have patches of black, brown or white
- Difficulty breathing or burns to the airway
Take first-aid measures outlined above while waiting for emergency assistance.
Also get medical help straight away if the person with the burn:
- has other injuries that need treating
- is going into shock – signs include cold, clammy skin, sweating, rapid, shallow breathing, and weakness or dizziness
- is pregnant
- is over the age of 60
- is under the age of 5
- has a medical condition, such as heart, lung or liver disease, or diabetes
- has a weakened immune system (the body’s defence system) – for example, because of HIV or AIDS, or because they’re having chemotherapy for cancer
If someone has breathed in smoke or fumes, they should also seek medical attention.
Some symptoms may be delayed, and can include:
- coughing
- a sore throat
- difficulty breathing
- singed nasal hair
- facial burns
Call your doctor if you experience:
- Signs of infection, such as oozing from the wound, increased pain, redness and swelling
- A burn or blister that’s large or doesn’t heal in two weeks
- New, unexplained symptoms
- Significant scarring
How are thermal burns classified?
To understand the nature and classification of thermal burns it is necessary to have a brief understanding of how skin is made up. Basically, skin consists of an outer layer called the epidermis and an inner layer called the dermis. The epidermis consists of epithelial cells among which are the pigment-containing cells called melanocytes, which absorb some of the potentially dangerous UV rays in sunlight. The epidermis does not contain any blood vessels but is nourished via the blood vessels located in the dermis. Hence, the dermis is richly supplied with blood vessels, lymphatic vessels and nerves. It also contains hair follicles, sebaceous glands and sweat glands. Lying below the dermis is the hypodermis or subcutaneous fat tissue. This is not part of the skin but attaches the skin to underlying bone and muscle as well as supplying it with blood vessels and nerves.
Traditionally thermal injuries were classified as first, second or third degree burns. Nowadays many doctors describe burns according to their thickness (superficial, partial and full). The signs and symptoms experienced by a burn victim depend largely on the severity of the burn and the number of layers of skin that are affected.
Figure 1. Skin anatomy

Figure 2. Skin epidermis structure

What can cause thermal burn
Thermal burns are caused by:
- Fire
- Hot liquid or steam
- Hot metal, glass or other objects
- Electrical currents
- Radiation, such as that from X-rays
- Sunlight or other sources of ultraviolet radiation, such as a tanning bed
- Chemicals such as strong acids, lye, paint thinner or gasoline
- Abuse
Thermal burn prevention
Prevent burns by preventing fires and other accidents that cause burns in your home. Fires and burns often happen unexpectedly. However, you can take precautions to help prevent them. Be prepared and know what to do if a fire or accident causes burns in your home.
Not all burns happen because of fires. Household chemicals, scalding water, and household appliances can also cause burns. Here are some fire and burn prevention and safety tips for your home:
To reduce the risk of common household burns:
- Never leave items cooking on the stove unattended.
- Turn pot handles toward the rear of the stove.
- Don’t carry or hold a child while cooking at the stove.
- Keep hot liquids out of the reach of children and pets.
- Keep electrical appliances away from water.
- Check the temperature of food before serving it to a child. Don’t heat a baby’s bottle in the microwave.
- Never cook while wearing loose fitting clothes that could catch fire over the stove. Wear short, close-fitting or tightly rolled sleeves when cooking.
- If a small child is present, block his or her access to heat sources such as stoves, outdoor grills, fireplaces and space heaters.
- Place objects so that they cannot be pulled down or knocked over.
- Turn pot handles away from the stove’s edge.
- Use dry oven mitts or potholders. Hot cookware can heat moisture in a potholder or hot pad, resulting in a scald burn.
- Have a “kid-free zone” of at least 3 feet around the stove.
- Before placing a child in a car seat, check for hot straps or buckles.
- Unplug irons and similar devices when not in use. Store them out of reach of small children.
- Cover unused electrical outlets with safety caps. Keep electrical cords and wires out of the way so that children can’t chew on them.
- If you smoke, never smoke in bed.
- Be sure you have working smoke detectors on each floor of your home. Check them and change their batteries at least once a year.
- Keep a fire extinguisher on every floor of your house.
- When using chemicals, always wear protective eyewear and clothing.
- Keep chemicals, lighters and matches out of the reach of children. Use safety latches. And don’t use lighters that look like toys.
- Set your water heater’s thermostat to below 120 °F (48.9 °C) to prevent scalding. Test bath water before placing a child in it.
- Be alert to burn risks outside the home, especially if you are in places with open flames, chemicals or superheated materials.
General fire safety
- Put smoke alarms in your home. Check them monthly. If they run on batteries, put in new batteries every 6 months.
- Think about how you would get out of your home in a fire emergency. Make a family escape plan and have regular fire drills at home. Designate a meeting place outside your home in case there is a fire.
- Have a professional electrician check the wiring in your home at least once every 10 years.
- Have a professional inspect and clean your chimney and fireplace once a year.
- Learn how and when to use a fire extinguisher. Keep one or more in your home.
Preventing different types of fires or burns in your home:
- Prevent chemical burns by wearing gloves and other protective clothing when you handle chemicals. Store chemicals, including gasoline, out of the reach of children.
- To prevent electrical burns, put covers on any electrical outlets that are within a child’s reach. Throw out electrical cords that are frayed or damaged.
- Use space heaters carefully. Teach children to stay away from them.
- Store matches and lighters in a locked cabinet, away from children.
- Never leave candles unattended. Blow them out when you leave the room.
- If you smoke, don’t smoke in bed. Get rid of used cigarettes carefully. Fires caused by smoking materials are the leading cause of deaths in house fires.
- Before putting a child younger than age 1 into a car seat, touch the seat to see if it is hot. Hot seat-belt straps or buckles can cause second-degree burns on small children. Cover the car seat with a towel when you park in the sun.
- Don’t let small children play near the stove or help you cook at the stove.
- Don’t wear clothing with long, loose sleeves when you are cooking.
- Cooking fires are the leading cause of house fires. Put out a small fire on a stove by sliding a lid over the flames.
- Do not use a microwave oven to warm baby bottles. The liquid heats unevenly and can scald your baby’s mouth.
- Unplug hot irons (clothing and curling irons). Keep them out of reach of children.
Preventing hot water burns in your home:
- Test the water temperature before you or your children get into the tub or shower. Don’t let young children touch the faucet handles during a bath.
- Set the temperature on your water heater to 120 degrees F (48.9 °C) or use the “low-medium” setting. Water that is hotter than this can cause burns in 2 to 3 seconds.
- Turn the handles of pots and pans toward the side of the stove, or use the back burners.
- Use cool-water humidifiers or vaporizers. If you use hot-steam vaporizers, keep them out of the reach of children.
If there is a fire in your home, your family should:
- Stick to your family escape plan. Get to your meeting place as fast as you can.
- Stay low to the ground. Crawl if you have to. Smoke and heat rise. It will be easier to breathe closer to the floor. (Many more people die from the poisonous gasses caused by house fires than from burns.)
- Check closed doors by touching them with the back of your hand. If the door is hot, don’t open it. It means the fire is nearby. If it is cool, open it slowly and peek out.
- Close doors to separate yourself from the fire and smoke.
- If you or your clothes catch on fire, “stop, drop and roll” your body on the ground.
Thermal burn signs and symptoms
Thermal burn symptoms vary depending on how deep the skin damage is. It can take a day or two for the signs and symptoms of a severe burn to develop.
Superficial or first degree burn signs and symptoms
- Involves only the epidermis skin layer
- May be painful, red and warm, area turns white when touched, no blisters, moist
Partial thickness or second degree burn signs and symptoms
- Involves the epidermis and some portion of the dermis
- Depending on the how much of the dermis is affected the burn is further broken down into superficial or deep
- Superficial partial thickness burns are usually painful, red, moist, with blisters, hair still intact
- Deep partial thickness burns may or may not be painful (nerve endings destroyed), may be moist or dry (sweat glands destroyed), hair is usually gone
Full thickness or third degree burn signs and symptoms
- Most severe burn and involves all layers of skin – epidermis and dermis
- Nerve endings, small blood vessels, hair follicles, sweat glands are all destroyed
- Subcutaneous fat tissue, muscle and bone may also be involved in very severe burns
- Burns are painless with no sensation to touch, skin is pearly white or charred, dry and may appear leathery
Thermal burn complications
Complications of deep or widespread thermal burns can include:
- Bacterial infection, which may lead to a bloodstream infection (sepsis)
- Fluid loss, including low blood volume (hypovolemia)
- Dangerously low body temperature (hypothermia)
- Breathing problems from the intake of hot air or smoke
- Scars or ridged areas caused by an overgrowth of scar tissue (keloids)
- Bone and joint problems, such as when scar tissue causes the shortening and tightening of skin, muscles or tendons (contractures)
Thermal burn diagnosis
If you go to a doctor for burn treatment, he or she will assess the severity of your burn by examining your skin. He or she may recommend that you be transferred to a burn center if your burn covers more than 10 percent of your total body surface area, is very deep, is on the face, feet or groin, or meets other criteria established by the American Burn Association.
Extent of burn
- Estimate the size of the burn.
- Rule of Nines is used to determine the amount of surface area burned (it basically divides the surface area of the body into sections, each roughly 9%).
Depth of burn
- Estimate the depth of the burn (what layers of skin are affected).
- Depth equates to the classification of burns, as described above.
- Estimating the depth of a burn is difficult and often burns are underestimated in depth on initial examination.
Your doctor will check for other injuries and might order lab tests, X-rays or other diagnostic procedures.
Thermal burn treatment
Appropriate first aid must be used to treat any burns or scalds as soon as possible (see thermal burns and scald first aid above). This will limit the amount of damage to your skin.
The management of thermal burn involves several key steps.
- Evaluation of the burn patient
- Evaluation of the burn wound
- Identifying and treating burn wound infections
- Managing the burn wound
Evaluation of the burn patient
Evaluating the total wellbeing of the burn patient is of paramount importance, particularly in patients with large burns. The primary aim is to ensure airway support, gas exchange and circulatory stability is achieved and maintained. Secondarily, a detailed history should be obtained from the patient to determine how the burn injury occurred. This may give clues for further examination, e.g. suspected carbon monoxide poisoning in individuals injured in structural fires.
Evaluation of the burn wound
Evaluation of the burn wound itself should only occur once the patient has been stabilized. The extent and depth of the burn will help guide decisions regarding wound care, inpatient or outpatient care, and monitoring.
Most minor burns can be treated at home. They usually heal within a couple of weeks.
For serious burns, after appropriate first aid and wound assessment, your treatment may involve medications, wound dressings, therapy and surgery. The goals of treatment are to control pain, remove dead tissue, prevent infection, reduce scarring risk and regain function.
People with severe burns may require treatment at specialized burn centers. They may need skin grafts to cover large wounds. And they may need emotional support and months of follow-up care, such as physical therapy.
The main treatment aims of burn wound management are:
- Carefully monitor wound
- Keep wounds clean
- Prevent the wound drying out
- Manage secondary infection.
To treat minor burns, follow these steps:
- Cool the burn. Hold the burned area under cool (not cold) running water or apply a cool, wet compress until the pain eases. Don’t use ice. Putting ice directly on a burn can cause further damage to the tissue.
- Remove rings or other tight items. Try to do this quickly and gently, before the burned area swells.
- DON’T break blisters. Fluid-filled blisters protect against infection. If a blister breaks, clean the area with water (mild soap is optional). Apply an antibiotic ointment. But if a rash appears, stop using the ointment.
- Apply lotion. Once a burn is completely cooled, apply a lotion, such as one that contains aloe vera or a moisturizer. This helps prevent drying and provides relief.
- Commonly used topical antibacterials include 1% silver sulfadiazine cream, 0.5% silver nitrate solution and mafenide acetate 10% cream.
- Bandage the burn. Cover the burn with a sterile gauze bandage (not fluffy cotton). Wrap it loosely to avoid putting pressure on burned skin. Bandaging keeps air off the area, reduces pain and protects blistered skin.
- Take a pain reliever. Over-the-counter medications, such as ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) or acetaminophen (Tylenol, others), can help relieve pain.
- Consider a tetanus shot. Make sure that your tetanus booster is up to date. Doctors recommend that people get a tetanus shot at least every 10 years.
Whether your burn was minor or serious, use sunscreen and moisturizer regularly once the wound is healed.
Identifying and treating burn wound infection
Prompt diagnosis of infection of the burn wound is important to prevent further complication. Two burn wound infections are:
- Burn wound cellulitis – manifests as progressive reddening, swelling and pain in the uninjured skin around a wound, seen in the first few days after burning. Streptococcus pyogenes is the causative bacteria and infection usually responds to penicillin.
- Invasive burn wound infection – rapid growth of bacteria in burn eschar that go on to invade the underlying healthy tissues. A change in colour, new drainage, and sometimes a foul or sickly sweet odour are indicative of infection. Pseudomonas and other gram-negative bacteria are the common causative.
- These infections can be life threatening and usually require combined treatment with surgery and antibiotics.
Managing the burn wound
Any serious burns should be referred to a specialized burns unit, particularly those involving face, hands and genitalia. For less serious burns, management may be in the outpatient or inpatient setting.
- Outpatient wound care strategies
- Teach wound cleansing techniques to patient and family
- Select a suitable wound dressing (topical medication and/or wound membrane)
- Prescribe medication for pain control
- Teach awareness of complications or specific conditions that require prompt medical attention
- Plan short-term follow-up care
- Plan long-term follow-up care
- Inpatient wound care strategies
- Initial evaluation and resuscitation
- Initial wound excision and biologic closure
- Definitive wound closure
- Rehabilitation and reconstruction
Medical treatment
After you have received first aid for a major burn, your medical care may include medications and products that are intended to encourage healing.
- Water-based treatments. Your care team may use techniques such as ultrasound mist therapy to clean and stimulate the wound tissue.
- Fluids to prevent dehydration. You may need intravenous (IV) fluids to prevent dehydration and organ failure.
- Pain and anxiety medications. Healing burns can be incredibly painful. You may need morphine and anti-anxiety medications — particularly for dressing changes.
- Burn creams and ointments. If you are not being transferred to a burn center, your care team may select from a variety of topical products for wound healing, such as bacitracin and silver sulfadiazine (Silvadene). These help prevent infection and prepare the wound to close.
- Dressings. Your care team may also use various specialty wound dressings to prepare the wound to heal. If you are being transferred to a burn center, your wound will likely be covered in dry gauze only.
- Drugs that fight infection. If you develop an infection, you may need IV antibiotics.
- Tetanus shot. Your doctor might recommend a tetanus shot after a burn injury.
Physical and occupational therapy
If the burned area is large, especially if it covers any joints, you may need physical therapy exercises. These can help stretch the skin so that the joints can remain flexible. Other types of exercises can improve muscle strength and coordination. And occupational therapy may help if you have difficulty doing your normal daily activities.
Coping and support
Coping with a serious burn injury can be a challenge, especially if it covers large areas of your body or is in places readily seen by other people, such as your face or hands. Potential scarring, reduced mobility and possible surgeries add to the burden.
Consider joining a support group of other people who have had serious burns and know what you’re going through. You may find comfort in sharing your experience and struggles and meeting people who face similar challenges. Ask your doctor for information on support groups in your area or online.
Surgical and other procedures
You may need one or more of the following procedures:
- Breathing assistance. If you’ve been burned on the face or neck, your throat may swell shut. If that appears likely, your doctor may insert a tube down your windpipe (trachea) to keep oxygen supplied to your lungs.
- Feeding tube. People with extensive burns or who are undernourished may need nutritional support. Your doctor may thread a feeding tube through your nose to your stomach.
- Easing blood flow around the wound. If a burn scab (eschar) goes completely around a limb, it can tighten and cut off the blood circulation. An eschar that goes completely around the chest can make it difficult to breathe. Your doctor may cut the eschar to relieve this pressure.
- Skin grafts. A skin graft is a surgical procedure in which sections of your own healthy skin are used to replace the scar tissue caused by deep burns. Donor skin from deceased donors or pigs can be used as a temporary solution.
- Plastic surgery. Plastic surgery (reconstruction) can improve the appearance of burn scars and increase the flexibility of joints affected by scarring.
- Gibran NS, Wiechman S, Meyer W, Edelman L, Fauerbach J, Gibbons L, et al. American Burn Association consensus statements. J Burn Care Res. 2013;34:361–5. doi: 10.1097/BCR.0b013e31828cb249
- Mann R, Heimbach D. Prognosis and treatment of burns. West J Med. 1996;165:215–20.
- Burn Incidence and Treatment in the United States: 2016. http://ameriburn.org/who-we-are/media/burn-incidence-fact-sheet/