What is thioridazine
Thioridazine is an antipsychotic medicine called a phenothiazine. Thioridazine was withdrawn worldwide in 2005 due to it’s association with cardiac arrythmias and is no longer in common use. Thioridazine was used in the management of psychoses, including schizophrenia, and in the control of severely disturbed or agitated behavior. Thioridazine is usually given after other antipsychotic medicines have been tried without success. Thioridazine is in a group of medications called conventional antipsychotics.
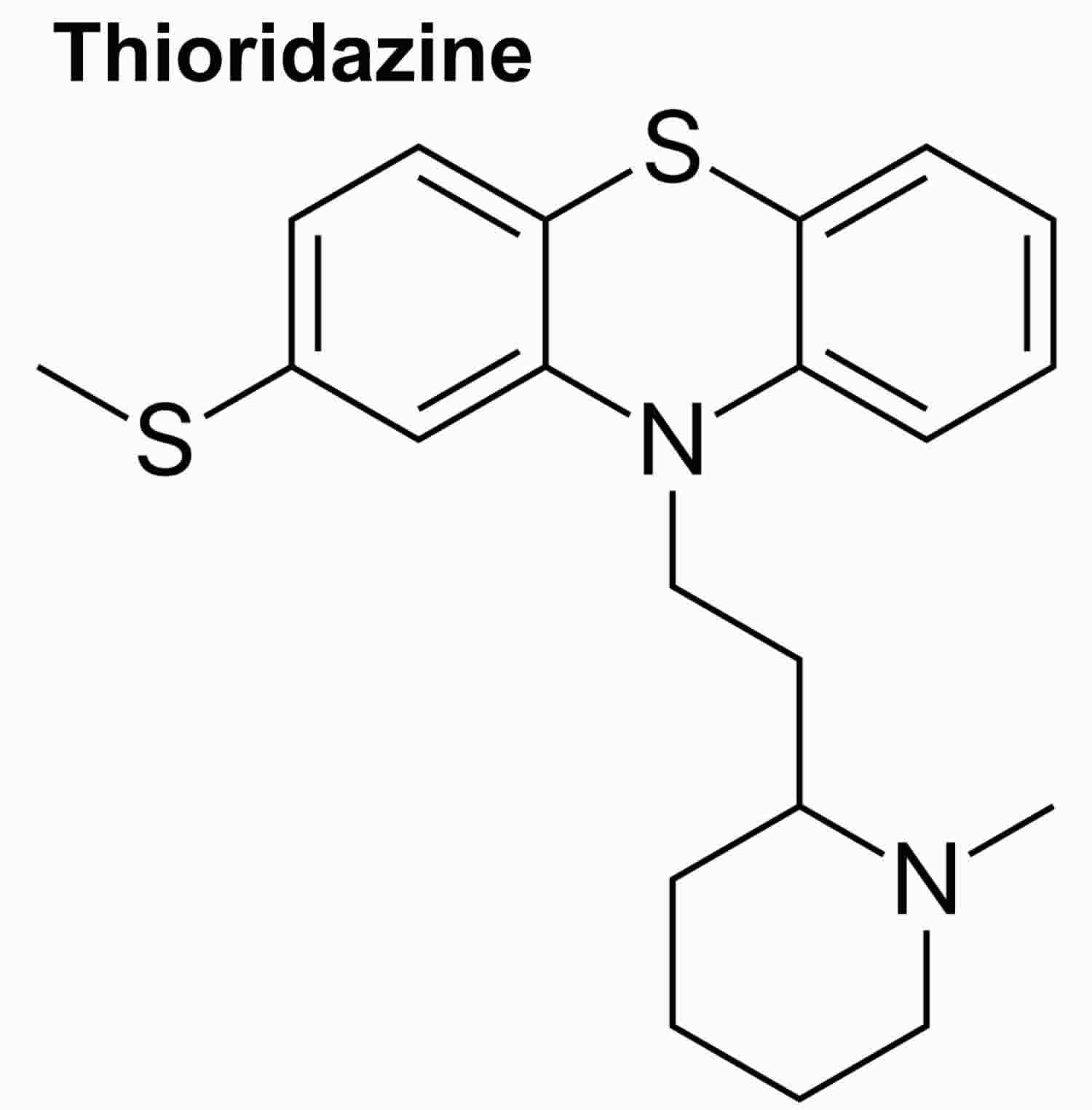
Thioridazine is a piperazine phenothiazine derivative which acts by postsynaptic inhibition of dopamine receptors. Thioridazine has other peripheral and central nervous system effects, producing both alpha adrenergic stimulation and blocking histamine- and serotonin-mediated effects.
Thioridazine is indicated for the therapy of acute and chronic psychosis. Thioridazine was approved for use in the United States in 1978 and was formerly a commonly prescribed antipsychotic medication, but in recent years has been replaced in large part by the atypical antipsychotics, which have fewer extrapyramidal side effects. Use of thioridazine is also restricted because of its propensity to cause prolongation of the QTc interval and increased risk of sudden death.
Thioridazine is available as tablets of 10, 25, 50 and 100 mg in generic forms and previously under the brand name Mellaril. The usual recommended dose in adults is 50 to 100 mg three times daily, increasing based upon effect and tolerance to a maximum of 800 mg daily. Common side effects include drowsiness, dizziness, headache, blurred vision, dry mouth, constipation, tremor, restlessness, muscle spasms and weight gain.
Thioridazine is used to treat the symptoms of schizophrenia (a mental illness that causes disturbed or unusual thinking, loss of interest in life, and strong or inappropriate emotions) in people who have already been treated with at least 2 other medications and have not been helped or who have experienced severe side effects.
Thioridazine has a higher incidence of antimuscarinic effects, but a lower incidence of extrapyramidal symptoms, than chlorpromazine. Thioridazine has little antiemetic activity. Thioridazine has a higher incidence of antimuscarinic effects, but a lower incidence of extrapyramidal symptoms, than chlorpromazine.
Thioridazine may help to control your symptoms but will not cure your condition. Continue to take thioridazine even if you feel well. Do not stop taking thioridazine without talking to your doctor.
For ALL Patients:
Thioridazine can cause a serious type of irregular heartbeat that may cause sudden death. There are other medications that can be used to treat your condition that are less likely to cause this life-threatening side effect. Therefore, you should not take thioridazine unless you have already been treated with at least 2 other medications for your condition and these medications did not work well or caused side effects that you could not tolerate.
Tell your doctor if you have or have ever had long QT syndrome (condition that increases the risk of developing an irregular heartbeat that may cause loss of consciousness or sudden death), a slow or irregular heartbeat, high or low blood pressure, heart disease, or a low level of potassium in your blood. Also tell your doctor if you are taking or plan to take any of the following medications: amiodarone (Cordarone), cisapride (Propulsid) (not available in the US), disopyramide (Norpace), dofetilide (Tikosyn), erythromycin (E.E.S., E-Mycin, Erythrocin), fluoxetine (Prozac, Sarafem), fluvoxamine (Luvox), moxifloxacin (Avelox), paroxetine (Paxil, Pexeva), pimozide (Orap), pindolol (Visken), procainamide, propranolol (Inderal), quinidine, sotalol (Betapace, Betapace AF), and sparfloxacin (Zagam) (not available in the US). Your doctor will probably tell you not to take thioridazine if you are taking any of these medications or if you have any of these conditions.
In addition to the medications listed above, there are other medications that may increase the risk that thioridazine will cause you to develop a serious irregular heartbeat. Before you begin to take any new medication, tell the doctor who is prescribing the medication that you are taking thioridazine.
If you experience any of the following symptoms, call your doctor immediately: fast, irregular, or pounding heartbeat; dizziness; lightheadedness; or fainting.
Keep all appointments with your doctor and the laboratory. Your doctor may order certain laboratory tests and electrocardiograms (tests to measure the electrical activity of the heart) before and during your treatment with thioridazine, especially when your dose is changed.
Talk to your doctor about the risks of taking thioridazine.
For older adults:
Studies have shown that older adults with dementia (a brain disorder that affects the ability to remember, think clearly, communicate, and perform daily activities and that may cause changes in mood and personality) who take antipsychotics (medications for mental illness) such as thioridazine have an increased chance of death during treatment.
Thioridazine is not approved by the Food and Drug Administration (FDA) for the treatment of behavior problems in older adults with dementia. Talk to the doctor who prescribed this medication if you, a family member, or someone you care for has dementia and is taking thioridazine. For more information, visit the FDA website: https://www.fda.gov/Drugs/default.htm
Thioridazine special precautions
Before taking thioridazine
You should not use thioridazine if you are allergic to it, or if you have:
- a heart rhythm disorder, or history of Long QT syndrome;
- untreated or uncontrolled high blood pressure;
- very low blood pressure; or
- if you have drowsiness, slow breathing, weak pulse, or decreased alertness (such as after drinking alcohol or taking medicines that make you sleepy).
- tell your doctor and pharmacist if you are allergic to thioridazine, other phenothiazines such as chlorpromazine, fluphenazine, perphenazine, prochlorperazine (Compro), promethazine (Phenergan), or trifluoperazine; or any other medications.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements and herbal products you are taking or plan to take. Be sure to mention the medications listed in the IMPORTANT WARNING section or any of the following: antidepressants; antihistamines; atropine (in Motofen, in Lomotil, in Lonox); barbiturates such as pentobarbital (Nembutal), phenobarbital (Luminal), and secobarbital (Seconal); epinephrine (Epipen); ipratropium (Atrovent); medications for anxiety or mental illness, irritable bowel disease, motion sickness, Parkinson’s disease, seizures, ulcers, or urinary problems; narcotic medications for pain; sedatives; sleeping pills; and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you are thinking about killing yourself or planning or trying to do so and if you have or have ever had any of the conditions listed in the IMPORTANT WARNING section or either of the following: seizures or breast cancer. Also tell your doctor if you have ever had to stop taking a medication for mental illness due to severe side effects or if you plan to work with organophosphorus insecticides (a type of chemical used to kill insects).
- tell your doctor if you are pregnant, especially if you are in the last few months of your pregnancy, or if you plan to become pregnant or are breast-feeding. If you become pregnant while taking thioridazine, call your doctor. Thioridazine may cause problems in newborns following delivery if it is taken during the last months of pregnancy.
- talk to your doctor about the risks and benefits of taking thioridazine if you are 65 years of age or older. Older adults should not usually take thioridazine because it is not as safe as other medications that can be used to treat the same condition.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking thioridazine.
- you should know that this medication may make you drowsy and may affect your thinking and movements. Tell your doctor if you plan to drive a car or operate machinery. Your doctor will tell you if these activities are safe for you and may increase the dose of your medication very gradually so that your body can adjust to these side effects.
- ask your doctor about the safe use of alcohol while you are taking thioridazine. Alcohol can make the side effects of thioridazine worse.
Thioridazine can cause a life-threatening heart rhythm disorder, especially if you use certain other medicines at the same time. Many medicines should not be taken together with thioridazine because they may cause this heart rhythm disorder or other serious medical problems. This includes:
- antibiotics;
- antidepressants;
- blood pressure medicine;
- cancer medicine;
- certain HIV/AIDS medicines;
- heart rhythm medicine;
- medicine to treat or prevent malaria; or
- other antipsychotic medicines.
Long-term use of thioridazine can cause a serious movement disorder that may not be reversible. Symptoms of this disorder include uncontrollable muscle movements of your lips, tongue, eyes, face, arms, or legs. The longer you take thioridazine, the more likely you are to develop this movement disorder. The risk of this side effect is higher in women and older adults.
To make sure thioridazine is safe for you, tell your doctor if you have:
- heart disease, high blood pressure, or a heart rhythm disorder;
- a history of slow heartbeats that have caused you to faint;
- past or present breast cancer;
- liver or kidney disease;
- a history of seizures;
- Parkinson’s disease;
- enlarged prostate or urination problems;
- low levels of potassium in your blood (hypokalemia); or
- if you have ever had a serious side effect while using thioridazine or another phenothiazine.
Tell your doctor if you are pregnant or plan to become pregnant while using thioridazine.
Taking antipsychotic medication during the last 3 months of pregnancy may cause problems in the newborn, such as withdrawal symptoms, breathing problems, feeding problems, fussiness, tremors, and limp or stiff muscles. However, you may have withdrawal symptoms or other problems if you stop taking your medicine during pregnancy. If you become pregnant while taking thioridazine, do not stop taking it without your doctor’s advice.
It is not known whether thioridazine passes into breast milk or if it could harm a nursing baby. Tell your doctor if you are breast-feeding a baby.
Thioridazine uses
Thioridazine is used to treat the symptoms of schizophrenia (a mental illness that causes disturbed or unusual thinking, loss of interest in life, and strong or inappropriate emotions) in people who have already been treated with at least 2 other medications and have not been helped or who have experienced severe side effects.
Thioridazine dosage
Thioridazine comes as a tablet to take by mouth. It is usually taken two to four times a day. Take thioridazine at around the same times every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take thioridazine exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Your doctor will probably start you on a low dose of thioridazine and gradually increase your dose until your symptoms are controlled. Once your symptoms have been controlled for some time, your doctor may decrease your dose. Be sure to tell your doctor how you are feeling during your treatment with thioridazine.
Adult Dose for Schizophrenia
Use: Patients with schizophrenia who failed to respond to treatment with other antipsychotic agents
- Initial dose: 50 to 100 mg orally 3 times a day
- Maintenance dose: 200 to 800 mg/day, divided into 2 to 4 doses
- Maximum dose: 800 mg/day
Comment:
- Once control is attained, the dose should be gradually lowered to determine the minimum effective maintenance dose.
Pediatric Dose for Schizophrenia
Use: Patients with schizophrenia who have failed to respond to treatment with other antipsychotic agents
- Initial dose: 0.5 mg/kg/day orally, in divided doses
- Maximum dose: 3 mg/kg/day, in divided doses
Comment:
- The dose should be increased gradually until therapeutic effects are observed and/or the maximum dose is reached.
Renal Dose Adjustments
- Data not available
Dialysis
- Data not available
Liver Dose Adjustments
Data not available
Dose Adjustments
Patients at risk of QT Prolongation and/or CYP450 2D6 poor metabolizers:
- QT interval greater than 450 msec at baseline: Not recommended
- QT interval greater than 500 msec during treatment: Discontinue use
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for your next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Thioridazine side effects
Thioridazine may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- blurred vision
- dry mouth
- nausea
- vomiting
- diarrhea
- constipation
- changes in appetite
- weight gain
- stuffed nose
- pale skin
- darkening of the skin or eyes
- swelling of the arms, hands, feet, ankles, or lower legs
- blank facial expression
- shuffling walk
- unusual, slowed, or uncontrollable movements of any part of the body
- restlessness
- unusual dreams
- breast milk production
- breast enlargement
- missed menstrual periods
- decreased sexual ability in men
- difficulty urinating
Some side effects may be serious. If you experience any of the following symptoms or the ones listed in the IMPORTANT WARNING section, call your doctor immediately:
- fever
- muscle stiffness
- confusion
- sweating
- neck cramps
- tightness in the throat
- difficulty breathing or swallowing
- tongue that sticks out of the mouth
- fine, worm-like tongue movements
- uncontrollable, rhythmic face, mouth, or jaw movements
- vision loss, especially at night
- seeing everything with a brown tint
- yellowing of the skin and eyes
- rash
- hives
- erection that lasts for hours
Thioridazine may cause other side effects. Call your doctor if you have any unusual problems while you are taking thioridazine.
Thioridazine overdose
In case of thioridazine overdose, call the poison control helpline at 1-800-222-1222. Information is also available online at https://www.poisonhelp.org/help. If the victim has collapsed, had a seizure, has trouble breathing, or can’t be awakened, immediately call your local emergency services number.
Symptoms of thioridazine overdose may include:
- slow, fast, or irregular heartbeat
- drowsiness
- slowed or unusual movements
- confusion
- agitation
- high or low body temperature
- seizures
- restlessness
- coma (loss of consciousness for a period of time)
- widened or narrowed pupils (black circles in the middle of the eyes)
- dry mouth
- stuffed nose
- difficulty urinating
- blurred vision
- slowed breathing
- constipation
Below are symptoms of an overdose of thioridazine in different parts of the body.
BLADDER AND KIDNEYS
- Cannot completely empty the bladder
EYES, EARS, NOSE, AND THROAT
- Blurred vision
- Drooling
- Dry mouth
- Nasal congestion
- Swallowing difficulties
- Ulcers in the mouth, on the tongue, or in the throat
- Vision color changes (brown tinge)
- Yellow eyes
HEART AND BLOOD
- Rapid heartbeat
- Slow heartbeat
- Irregular heartbeat
- High or very low blood pressure
LUNGS
- Difficulty breathing
- Fluid buildup in the lungs
- Breathing may stop in severe cases
MOUTH, STOMACH, AND INTESTINAL TRACT
- Constipation
- Loss of appetite
- Nausea
MUSCLES AND BONES
- Muscle spasms
- Muscle stiffness
- Neck or face stiffness
NERVOUS SYSTEM
- Drowsiness, coma
- Difficulty walking
- Dizziness
- Fever
- Hypothermia (body temperature is lower than normal)
- Seizures
- Tremor
- Weakness, lack of coordination
OTHER
- Menstrual changes
- Skin discoloration, bluish (changing to a purplish color)
What to expect at the emergency room
Take the container with you to the hospital, if possible.
Your doctor will measure and monitor the person’s vital signs, including temperature, pulse, breathing rate, and blood pressure. Symptoms will be treated. The person may receive:
- Activated charcoal
- Blood and urine tests
- Breathing support, including oxygen and a tube through the mouth into the lungs
- CT scan (advanced imaging) of the brain
- ECG (electrocardiogram, or heart tracing)
- Intravenous fluids (given through a vein)
- Laxative
- Medicine (sodium bicarbonate) to help reverse the effect of the poison
- Tube through the mouth into the stomach to empty the stomach (gastric lavage)
- X-rays
Thioridazine overdose prognosis
Recovery depends on the amount of damage to the person’s body. Survival past 2 days is usually a good sign. The most serious side effects are usually due to damage to the heart. If heart damage can be stabilized, recovery is likely. But if breathing has been depressed for a long period before treatment, brain injury may occur.