Third heart sound
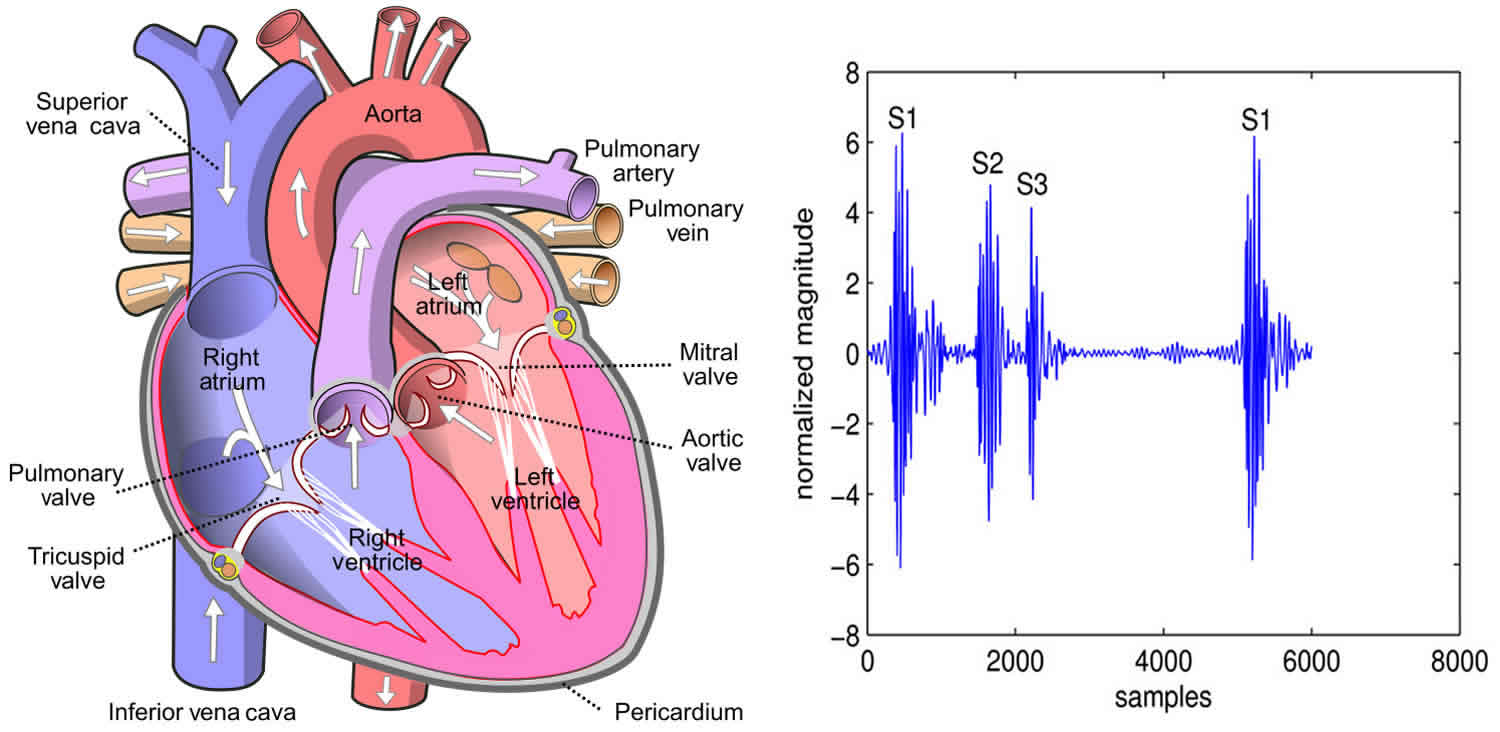
Third heart sound (S3) also known as the “ventricular gallop” that occurs 120 to 180 milliseconds after the second heart sound (S2), is a series of low frequency vibrations in early diastole best heard with the bell of the stethoscope at the cardiac apex 1. Third heart sound is mainly created by the early-diastolic rapid distension of the left ventricle that accompanies rapid ventricular filling and abrupt deceleration of the atrioventricular blood flow 2. Third heart sound is normal in children and young adults but usually disappears after 40 1. Third heart sound also occurs in patients with high cardiac output caused by anemia, fever, pregnancy, and thyrotoxicosis. If the patient is over 40, the third heart sound nearly always shows that something is wrong, usually left ventricular failure or left heart failure with a low ejection fraction, restrictive diastolic filling, but less commonly mitral regurgitation or constrictive pericarditis 3. The timing and quality of the third heart sound remain remarkably constant regardless of its cause, except in constrictive pericarditis, when the “pericardial knock” is early and high pitched 1. Recognition of the third heart sound is therefore crucial for prompt treatment. However, auscultation of the third heart sound requires training, experience, and dedication, because it is often the most difficult heart sound to hear.
This is caused by several factors 4:
- The third heart sound (S3) is usually of very low intensity and is easily obscured by extraneous room sounds, lung or abdominal noise, or tightening of the chest wall muscles.
- The third heart sound (S3) does not radiate widely and is audible only over a small area of the chest wall.
- The usual frequency (pitch) of the sound is near the lowest level that the human ear can detect. The inexperienced ear is unaccustomed to listening for a sound of this low frequency.
All extraneous noises—radio, television, visitors, hall noises—should be excluded so that the room is as quiet as possible.
The bed should be elevated to a comfortable level for the examiner. The patient is examined supine and then turned to a 30° left lateral position with the left arm extended upward away from the chest and the weight comfortably supported by the left hip, lateral chest, and left arm. The left lateral position is of critical importance because the ventricular gallop is often heard only with the patient turned to the side. After the apical impulse is located by careful palpation, the bell of the stethoscope is placed lightly over the apex. The examiner then listens selectively for the third heart sound—tuning in to early diastole for low-frequency sounds while ignoring all other heart sounds and murmurs. The patient should be asked to exhale and suspend respiration temporarily in order to provide maximal silence to listen. The bell of the stethoscope is then glided around the apical and lower sternal area seeking for a left ventricular gallop. Simultaneous palpation and inspection of the apex is useful; however, a third heart sound is rarely palpable or visible when it is not audible.
The third heart sound is a very low-frequency vibration, in the range of 25 to 50 Hz, and has a dull, thudding quality. At times it may be difficult to tell if it is an actual sound or more of a sensation imparted to the ear of the listener. When intense, a few after-vibrations may add to its duration and suggest a short diastolic murmur. Techniques that increase venous return or the size of the ventricular cavity—recumbent position, elevation of the legs, exercise, squatting, volume expansion—augment the intensity of third heart sound (S3). Conversely, the sound becomes softer or disappears with standing, diuresis, hemorrhage, or dialysis.
A right ventricular third heart sound is an uncommon finding heard in association with right ventricular dysfunction from a variety of causes. It is usually heard best while listening along the right or left lower sternal edge, in the epigastrium, or rarely over the jugular veins. An inspiratory increase in its intensity identifies a right ventricular gallop. This diagnostic feature may be absent, however, when right ventricular distention or failure prevents inspiratory augmentation of venous return.
The third heart sound must be differentiated from other diastolic sounds. Competing possibilities include: splitting of the second heart sound, an opening snap of the mitral or tricuspid valve, a diastolic click related to mitral valve prolapse, a tumor “plop” from a left atrial myxoma, a pericardial knock, a summation gallop, and an atrial gallop. The distinguishing features of each of these sounds are listed in Table 1. With experience, the third heart sound should not be confused with other diastolic sounds because of its very low pitch and late timing relative to the aortic closure sound.
Table 1. Comparison of third heart sound (S3) with other diastolic sounds
| Sound | Location best heard | Interval after A2 (sec) | Pitch | Miscellaneous |
|---|---|---|---|---|
| Third heart sound (S3) | Apex | 0.10 to 0.20 (usually 0.14 to 0.16) | Very low | See text. |
| Split S2 | Upper left sternal border | 0.02 to 0.06 | Medium to high | Split varies with respiration. |
| Opening snap | Lower left sternal border or apex | 0.06 to 0.12 | Medium to high | Associated murmur of mitral stenosis. Loud S1 usually present |
| Mitral valve prolapse | Lower left sternal border | 0.06 to 0.08 | Medium to high | Associated systolic click(s) and/or murmur. |
| Pericardial knock | Apex | 0.09 to 0.12 | Medium to high | Usually loud and palpable. Associated jugular venous findings of constriction. |
| Tumor plop | Apex | 0.08 to 0.13 | Low | May vary with position. Associated loud S1. Diastolic murmur may be heard. |
| Summation gallop | Apex | Depends on PR interval and rate | Low | Often louder than S1 and S2. Cannot be distinguished from loud S3. |
| Atrial gallop | Apex | Depends on PR interval and rate | Low | Close to S1. Often palpable. Higher pitch than S3. |
Third heart sound causes
During ventricular contraction, the mitral and tricuspid valves are closed, and atrial pressure rises (V wave) from the continuing influx of venous blood into the atria. In early diastole, when ventricular pressure falls below atrial pressure, the atrioventricular valves open wide, and the blood rapidly drains from the atria (Y descent) into the ventricles. The ventricles quickly become distended, moving toward the chest wall, until the elastic distensibility of the ventricular wall is reached and the rapid inflow of blood is checked. At the termination of this early diastolic filling period, a third heart sound may occur. The genesis of this sound is controversial. Previously, it was thought to be an intracardiac sound arising from vibrations in the valve cusps or ventricular wall as diastolic inflow suddenly decelerated. Recent studies, however, have shown that the third heart sound is loudest external to the left ventricular cavity, implying that the sound is not radiating from an intracardiac source. Possible explanations include impact of the ventricle against the inner chest wall or a sound originating within the ventricular apex due to sudden limitation of longitudinal expansion.
Factors that seem to relate to the presence and intensity of the third heart sound include age, atrial pressure, unimpeded flow across the atrioventricular valve, rate of early diastolic relaxation and distensibility of the ventricle, blood volume, ventricular cavity size, diastolic momentum of the heart, degree of contact (coupling) with the chest wall, thickness and character of the chest wall, and the position of the patient.
Third heart sound clinical significance
Children and adults up to age 35 to 40 may have a normal third heart sound 4. The explanation for this “physiologic S3”, which is identical in timing and frequency with its pathologic counterpart, is unknown. Before age 40, the significance of the third heart sound must be judged by the presence or absence of significant heart disease. After age 40, a third heart sound is usually abnormal and correlates with dysfunction or volume overload of the ventricles.
Any cause of ventricular dysfunction, including ischemic heart disease, dilated or hypertrophic cardiomyopathy, myocarditis, cor pulmonale, or acute valvular regurgitation, may qualify. Myocardial ischemia without ventricular dysfunction or volume overload is not a cause of a third heart sound (S3). The presence of an third heart sound (S3) is the most sensitive indicator of ventricular dysfunction.
Any cause of a significant increase in the volume load on the ventricle(s) can cause a third heart sound (S3). Examples include valvular regurgitation, high-output states (anemia, pregnancy, arteriovenous fistula, or thyrotoxicosis), left-to-right intracardiac shunts, complete A-V block, renal failure, and volume overload from excessive fluids or blood transfusion.
Although the third heart sound is a very important clue to heart failure or volume overload, it does not appear until the problem is relatively far advanced. In some patients, for reasons that are not clear or because of chest size, obesity, or lung disease, a third heart sound (S3) may never be heard despite severe hemodynamic impairment. Therefore, the absence of a third heart sound cannot be used to exclude ventricular dysfunction or volume overload. In addition, the intensity of the third heart sound is influenced by several factors and correlates only roughly with the clinical status of the patient.
References- Timmis AJ. The third heart sound. Br Med J (Clin Res Ed). 1987;294(6568):326–327. doi:10.1136/bmj.294.6568.326-a https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1245345/pdf/bmjcred00006-0004b.pdf
- Diastolic properties of the left ventricle in normal adults and in patients with third heart sounds. Van de Werf F, Boel A, Geboers J, Minten J, Willems J, De Geest H, Kesteloot H. Circulation. 1984 Jun; 69(6):1070-8.
- Shono A, Mori S, Yatomi A, et al. Ultimate Third Heart Sound. Intern Med. 2019;58(17):2535–2538. doi:10.2169/internalmedicine.2731-19 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6761354
- Silverman ME. The Third Heart Sound. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 24. Available from: https://www.ncbi.nlm.nih.gov/books/NBK342