Thyroplasty
Thyroplasty is a surgical procedure done to change the position of the vocal cord to improve a your voice and ability to cough. Thyroplasty is done to move your paralyzed vocal cord towards the non-paralyzed one so the vocal cords can touch better. This allows for improved voice, swallow function and a stronger ability to cough. The paralyzed vocal cord is moved over with a permanent implant. Once you are under general anesthesia, a small cut is made on your neck and the voice box is identified by the surgeon.
The surgeon will make a small hole in the voice box, then place an implant to move the vocal cord into the proper position.
After the implant is in place, you will be wakened and asked to speak. This is so the voice box can be “fine tuned.”
After surgery, you will remain in the hospital overnight.
How long does thyroplasty surgery take?
Thyroplasty surgery takes about 2 hours. You will stay the night in the hospital.
When will my voice be better?
The recovery of your voice happens with time. Your voice will likely be worse before it gets better, so be patient. If your voice does not improve, then you should let your surgeon know.
Why should I work with the voice therapist (speech-language pathologist)?
It is very important! They will teach you skills and give you advice on how to restore your voice. Meeting with them before and after your thyroplasty procedure will assure your best outcome.
Thyroplasty types
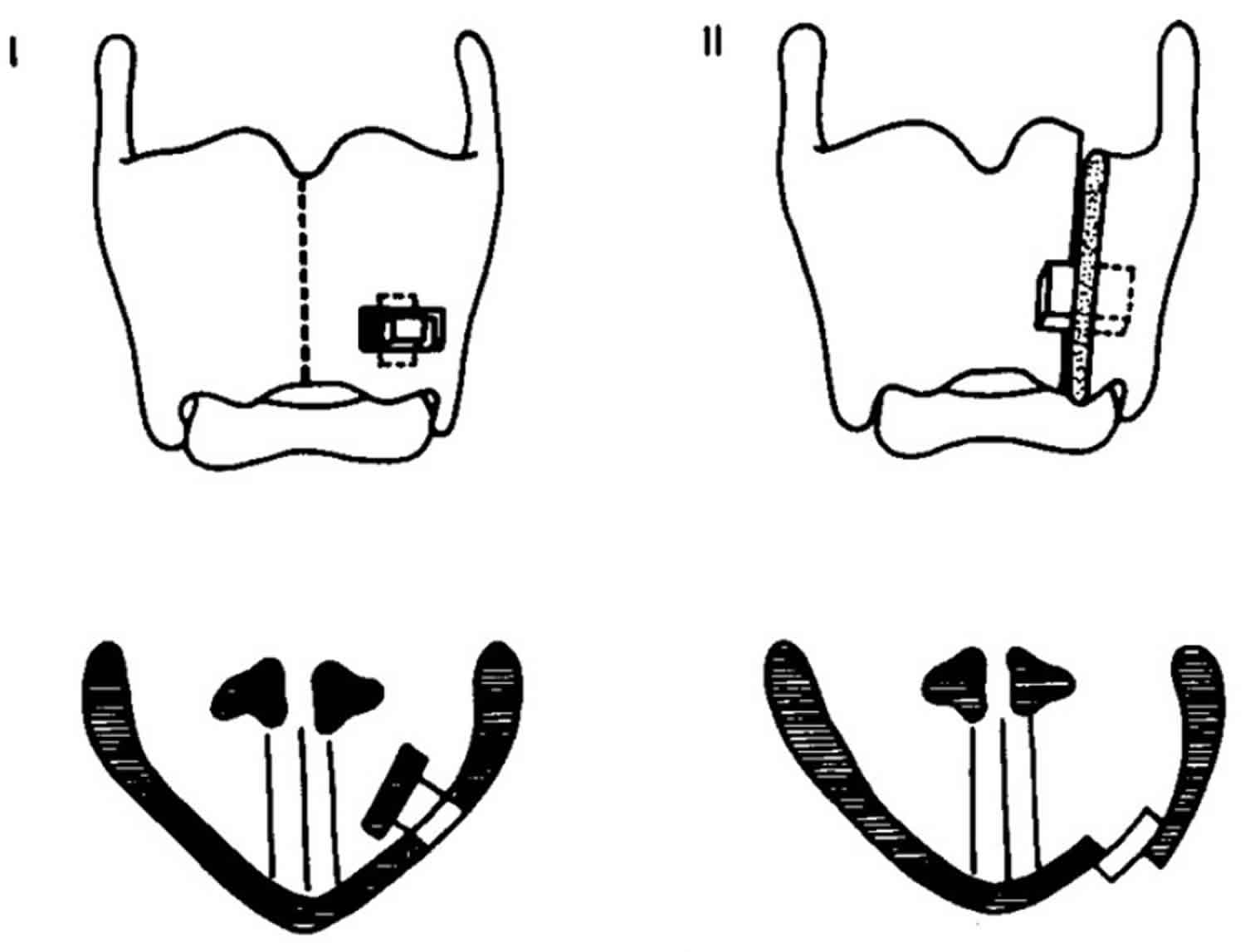
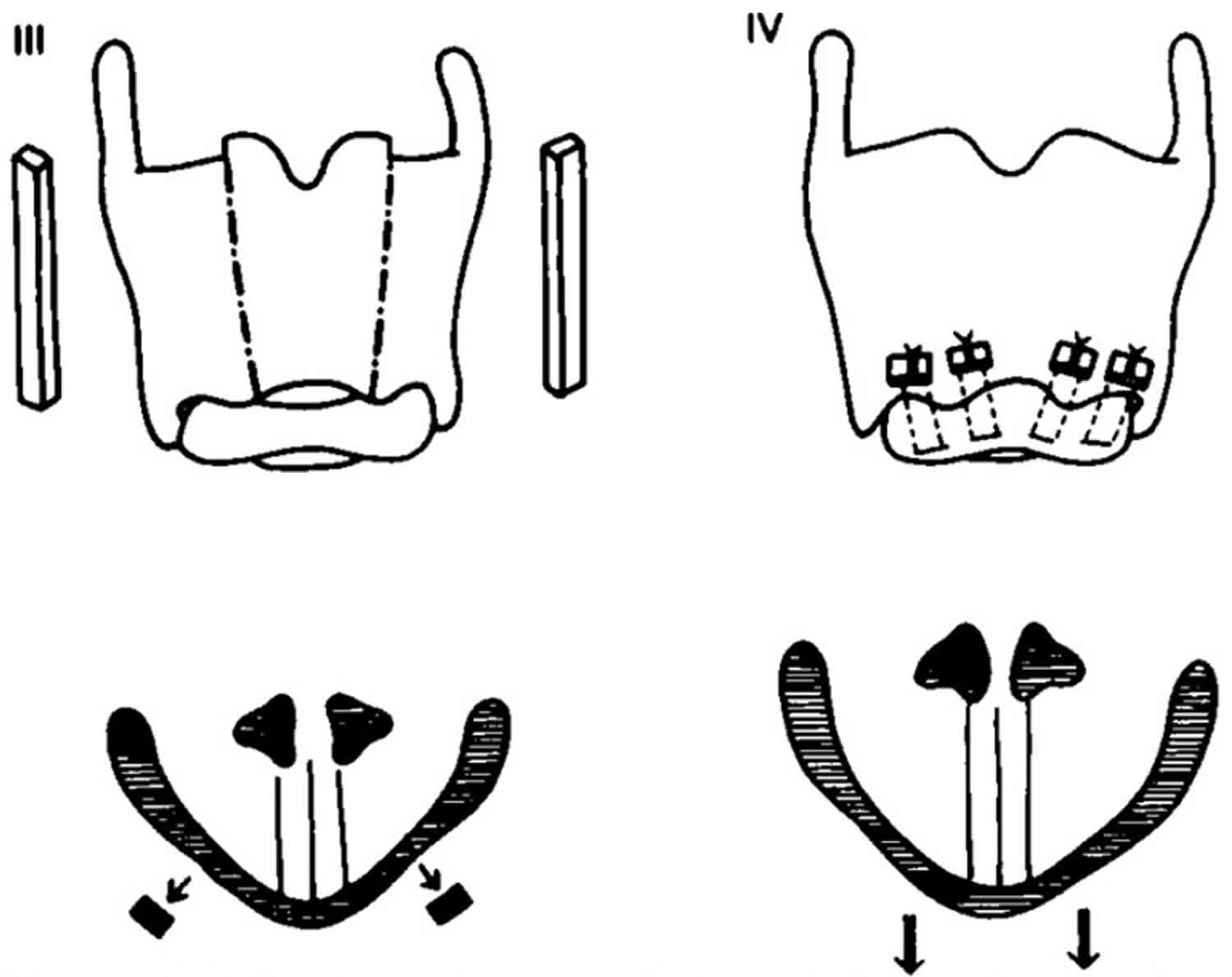
There are four different types of thyroplasty procedures described by Isshiki 1:
- Type 1 thyroplasty – Medialization of the vocal folds (most common surgery for unilateral vocal cord paralysis).
- Type 2 thyroplasty – Lateralization of the vocal folds (in case of airway insufficiency after Laryngeal trauma).
- Type 3 thyroplasty – Shortening of the vocal folds (done to lower the vocal pitch).
- Type 4 thyroplasty – Lengthening of the vocal folds (done to raise the vocal pitch). 2
Figure 1. Type 1 and type 2 thyroplasty
Figure 2. Type 3 and type 4 thyroplasty
Type 1 thyroplasty (medialization thyroplasty)
Type 1 thyroplasty is the most commonly used surgical procedure to correct unilateral vocal cord paralysis (a condition where the vocal cord of one side is paralyzed). In type 1 thyroplasty, a rectangular portion of the thyroid cartilage is mobilized and pushed towards the medial side using a piece of silastic block of proper shape under light sedation and local anesthesia in the operating room 3.
Earlier, the piece of the thyroid cartilage was kept along with implant and the stitches were taken, but nowadays, the piece of the thyroid cartilage is cut and removed to avoid complications.
Currently, there are four types of implant procedures which are used to perform type 1 thyroplasty.
- Montgomery Thyroplasty Implant system. Montgomery Thyroplasty Implant system was discovered after years of research and the main advantage of this implant system is that it eliminates the process of customizing the implant at the time of surgery. This system consists of different sizes and shapes of shims made of silastic. It has the most proven success rate and the duration of the procedure is slow in comparison to other implant system. The other advantage is that it does not require suturing. It has reduced incidence of trauma.
- VoCoM system (vocal fold medialization). VoCoM system (vocal fold medialization) system consists of different sizes and shapes of implants made from hydroxyapatite (a naturally occurring mineral form of calcium apatite). It helps in achieving accurate vocal fold medialization. This procedure is technically reversible. But it should be used in candidates of permanent implantation due to its biocompatible clinical use lasting for nearly a decade.
- Titanium Vocal Fold Medializing Implant (TVFMI) system. Titanium Vocal Fold Medializing Implant (TVFMI) system generally consists of two sizes of implants made out of pure titanium. It has a lot of advantages and the main one is that it reduces the operative time. Titanium is more safe than other implants. It has great biocompatibility. The implants are available in only two variants and they are designed in such a way that they ensure optimal fixation. The implant can be easily made as the titanium sheet is easy to shape. The technique is relatively simple and does not require expensive instruments.
- Gore-Tex Implant system. Gore-Tex Implant system system, the implant is made of homopolymer of polytetrafluoroethylene in form of minute beads arranged in a fine fiber mesh. It is malleable and can be inserted through a small window 4.
Type 1 thyroplasty indications
- Unilateral vocal cord paralysis where one vocal cord out of the two is paralyzed.
- Symptomatic glottic insufficiency (dysphonia, aspiration) which leads to incomplete glottic closure which in turn results in failure to produce proper sound.
- Age-related vocal fold atrophy leading to glottic insufficiency 5.
Type 1 thyroplasty contraindications
- Malignant diseases of the endolaryngeal mucosa.
- Previous history of radiation therapy to the larynx for treatment of laryngeal and hypolaryngeal cancers.
- Poor abduction of the contralateral vocal folds.
Type 1 thyroplasty complications
- Airway obstruction is the most common complication.
- Implant migration or extrusion in cases where proper stitches are not taken.
- Wound infection.
- Penetration of the endolaryngeal mucosa.
- Incomplete glottal closure in 10–15% of patients 6.
Type 1 thyroplasty advantages
- The most important advantage is that this procedure is reversible.
- It is long-lasting.
- It can be performed with minimal anesthesia.
- No discomfort to the patient.
Type 1 thyroplasty disadvantages
- It is an open procedure.
- It is technically more difficult.
- There may be limited closure of the posterior glottis.
Limitations
- There is increase in average phonation time (from 4.6 seconds to 15 seconds).
- It provides static change to the laryngeal framework but does not have any effect on the dynamic function 7.
Type 2 thyroplasty (lateralization thyroplasty)
Type 2 thyroplasty or lateralization thyroplasty, is a surgical procedure used in conditions like adductor spasmodic dysphonia (a condition in which there is distortion of the voice due to excessively tight closure of the glottis on phonation). Generally, lateralization thyroplasty is intended to prevent this tight closure of the glottis at the terminal stage of phonation by lateralizing the position of the vocal cord. This is a completely mechanical process.
An incision is made at midline of the thyroid cartilage. A silicon wedge is used to fix the incised thyroid cartilage in the newly abducted position.
Modified technique
A specially devised titanium bridge is used instead of silicon wedge. Nowadays, instead of one titanium bridge, two titanium bridges are used for permanent fixation of the thyroid cartilage.
Type 2 thyroplasty or lateralization thyroplasty indications
The only known indication for type 2 thyroplasty is adductor spasmodic dysphonia, a condition characterized by involuntary movements of muscles of the larynx during speech.
Type 2 thyroplasty or lateralization thyroplasty contraindications
It is contraindicated in irradiated larynx (when the larynx is exposed to radiation) 8.
Type 3 thyroplasty (relaxation thyroplasty)
Type 3 thyroplasty or relaxation thyroplasty procedure is generally done to lower the vocal pitch by shortening the thyroid ala.
In type 3 thyroplasty or relaxation thyroplasty, the relaxation of the vocal cords is done by antero-posterior shortening of the thyroid ala.
Type 3 thyroplasty or relaxation thyroplasty indications
- It is most commonly indicated in males with high-pitch voices and those who are resistant to voice therapy.
- In people with spasmodic dysphonia.
- In people who have stiff vocal folds with high-pitched breathy voices.
Type 4 thyroplasty (stretching thyroplasty)
Type 4 thyroplasty or stretching thyroplasty procedure is done to elevate the vocal pitch. This procedure consists of lengthening of the thyroid cartilage. It includes cricothyroid approximation.
Type 4 thyroplasty or stretching thyroplasty indications
- It is done in people with bow-shaped vocal folds.
- Androphonia (condition characterized by low vocal pitch) 9.
- Gender dysphonia, linked to gender dysphoria.
Combination thyroplasty
In some specific conditions, different types of thyroplasties are combined for the desired results.
Medialization thyroplasty with arytenoid adduction (rotation technique)
The main purpose of this combination is the medialization of the entire vocal cord (anterior and posterior).
Medialization thyroplasty with arytenoid adduction (rotation technique) indications:
- Open posterior glottis.
- In people with high vagal paralysis.
- Recurrent laryngeal nerve paralysis with lateralized arytenoid.
- Non-rotating aarytenoid.
Medialization thyroplasty with arytenoid adduction (fixation technique)
Medial vocal cord fixation.
Medialization thyroplasty with arytenoid adduction (fixation technique) indications:
- Arytenoid fracture where there is anterior dislocation of the arytenoid cartilage.
- In cricoarytenoid joint ankylosis where there is failed arytenoid adduction.
Medialization thyroplasty (type 1) with stretching thyroplasty (type 4)
The main purpose of this combination is stretching of the vocal cord with medialization of the affected side.
Medialization thyroplasty (type 1) with stretching thyroplasty (type 4) indications:
- Unilateral superior laryngeal nerve weakness.
Medialization thyroplasty (type 1) with relaxation thyroplasty (type 3)
The main aim of this combination is relaxation and increased mass of one vocal cord.
Medialization thyroplasty (type 1) with relaxation thyroplasty (type 3) indications:
In males with high-pitched, presbyphonic voice.
Bilateral medialization thyroplasty
Medialization of both the vocal cords.
Bilateral medialization thyroplasty indications:
- Open anterior glottis.
- In presbyphonia where there is bilateral vocal cord weakness.
- When there is bilateral loss of muscle mass.
- Tremor-induced abductor spasmodic dysphonia.
Bilateral relaxation thyroplasty
Relaxation of both the vocal cords.
Bilateral relaxation thyroplasty indications:
- In males who have an overly high-pitched voice.
- Stable abductor spasmodic dysphonia 3.
Thyroplasty recovery
After thyroplasty surgery
- You will wake up with a bandage around your neck. Do not move it.
- You may have a small drainage tube under the dressing; this will be removed the day after surgery before you go home.
- You are encouraged to get out of bed and take short walks with assistance.
- Do not use your voice for three days after surgery, including talking, whispering or laughing. Avoid coughing, if possible to prevent bleeding and to help swelling decrease. This will help to heal your vocal cords.
- After a week, it is okay to use your voice normally.
- Two weeks after your thyroplasty surgery, you will have a follow-up visit in your doctor’s office.
At home
- Medication. Take your pain medicine as directed. Take acetaminophen (Tylenol®) as needed for pain. Do not take anti-inflammatory medicine such as ibuprofen or Aleve for 2 days after surgery. Use your prescribed pain medicine, if needed. Side effects may include drowsiness, or nausea and vomiting.
- Be sure to take your reflux medicine, if prescribed.
- Laxatives. Occasionally patients become constipated with pain medications. If this occurs, over the counter Colace can be taken.
- Incision care. Leave the bandages on your skin alone. Do not wet the neck for three days after surgery. After this you may allow a small amount of water on the neck during shower. After one week, the bandages will fall off on their own, and you can cut any that no longer sticks to the skin. Clean around your incision with mild soap and water, rinse and pat dry. You can leave your incision open to the air. If you have stitches, they will be removed at your first post-op visit.
- Check your incision daily for any signs of infection. If your incision becomes red, swollen or tender, call your physician immediately.
- Pus-like drainage or fever over 100.5 °F is a sign of infection, call your physician immediately.
- Some blood-tinged drainage from your incision is normal for the first 2-3 days.
- Keep your head raised at least 30⁰ on 2-3 pillows when sleeping or resting for 3 days after surgery. Do not lie flat in bed.
- Limit activity. For the first two weeks after surgery, do not exert yourself or lift objects heavier than 15 pounds. Walking is okay during this period.
- If you have trouble breathing, shortness of breath, bleeding or a fever occurs.
- If you have pain not relieved with pain medicine.
- If you cough up bright red blood or blood clots.
- If you have any sign of infection at the incision site.
Visit the emergency room or call your local emergency services number.
Diet
Drink plenty of fluids, even if you cannot eat much solid food. Advance your diet slowly from liquids to soft foods. Avoid spicy foods for 2-3 days after surgery. Eat slowly to avoid choking or coughing.
Follow-Up Visits
You will see a speech-language pathologist about one week after surgery and have a member of the ENT clinic check your neck. A full follow-up with your surgeon and a speech-language pathologist will take place in about 6 weeks.
Thyroplasty side effects
Risks of thyroplasty:
- Neck soreness after surgery
- Worsening of the voice
- Infection
- Difficulty swallowing
- Bleeding
- Skin and neck numbness
- Difficulty breathing
- Reactions to anesthesia.
- Isshiki N. Mechanical and Dynamic Aspects of Voice Production as Related to Voice Therapy and Phonosurgery. Otolaryngol Head Neck Surg. 2000; 122(6):782-793.
- Sataloff, Robert T.; Chowdhury, Farhad; Portnoy, Joel E.; Hawkshaw, Mary J.; Joglekar, Shruti (30 September 2013). Surgical Techniques in Otolaryngology – Head & Neck Surgery: Laryngeal Surgery. JP Medical Ltd. p. 208. ISBN 9789350906521.
- Remacle, Marc; Eckel, Hans Edmund. Surgery of Larynx and Trachea. Springer Science & Business Media. ISBN 9783540791362.
- Remacle, Marc; Eckel, Hans Edmund. Surgery of Larynx and Trachea. Springer Science & Business Media. p. 59. ISBN 9783540791362.
- Bailey, Byron J. Atlas of Head & Neck Surgery–otolaryngology (Second ed.). Lippincott Williams & Wilkins. p. 636. ISBN 9780781729079
- Flint, Paul W.; Haughey, Bruce H.; Robbins, K. Thomas; Thomas, J. Regan; Niparko, John K.; Lund, Valerie J.; Lesperance, Marci M. Cummings Otolaryngology – Head and Neck Surgery. Elsevier Health Sciences. pp. 930–945. ISBN 9780323278201
- Lin, Harrison W.; Roberts, Daniel S.; Harris, Jeffrey P. Cummings Review of Otolaryngology. Elsevier Health Sciences. ISBN 9780323427999.
- Hathiram, Bachi T.; Khattar, Vicky S. Atlas of Operative Otorhinolaryngology and Head & Neck Surgery: Voice and Laryngotracheal Surgery. JP Medical Ltd. ISBN 9789350904824
- Phonosurgery. http://www.alexorl.edu.eg/alexorlfiles/pptorl2007/141001.pdf