Tinnitus
Tinnitus is when you experience ringing, buzzing or other noises (e.g. humming sounds, hissing, whistling, clicking, roaring or whooshing) in one or both of your ears not caused by sounds coming from the outside world 1. Tinnitus is the result of a complex cascade of changes within the auditory and emotional networks of your brain that occur following ear or head injury 2. The noise you hear when you have tinnitus isn’t caused by an external sound, and other people usually can’t hear it. The noise can be faint or loud, and it can occur in one or both ears. Sometimes the noise may feel like a sensation inside the head. Tinnitus can come and go, or you might experience it all the time. Some people find their tinnitus is an irritation they can learn to live with. For others, it can be very distressing and may result in insomnia, cognitive effects, anxiety, psychological distress and lower quality of life 3. Much of the severity of tinnitus relates to the sufferer’s psychological response to abnormal auditory and emotional inputs 4. Stress, anxiety and depression have been shown to occur with tinnitus or contribute to a greater, negative and sustaining reaction to tinnitus 5. Cognitive processes are suspected to affect how dominating tinnitus may or may not become, how easy or difficult it may be to ignore, and whether attention can easily be diverted away from, or is captured by, this internal signal 6.
Both adults and children can experience tinnitus. Older adults are more likely to experience tinnitus because of age-related hearing loss or presbycusis. Tinnitus is a common problem among adults in the United States, with more than 50 million people in the United States having reported experiencing tinnitus, with an estimated prevalence of 10% to 15% and peak incidence between 60 and 69 years of age 1. According to current European guidelines, up to 20% of the population suffer from chronic tinnitus for more than 3 months 7. Prevalence tends to increase with age as presbycusis (age-related hearing loss) is a common cause of tinnitus. Most cases of tinnitus are benign and idiopathic (unknown) and are strongly associated with sensorineural hearing loss 8. However, less common but potentially dangerous causes of tinnitus such as vascular tumors and vestibular schwannoma (acoustic neuroma) should be ruled out.
Tinnitus is not a disease per se, but a common symptom, and because it involves the perception of hearing sound or sounds in one or both ears, it is commonly associated with the hearing system. Tinnitus is usually caused by an underlying condition, such as age-related hearing loss (presbycusis), an ear injury or a problem with the circulatory system. For many people, tinnitus improves with treatment of the underlying cause or with other treatments that reduce or mask the noise, making tinnitus less noticeable.
Secondary tinnitus results from sound generated by a source near the ear or referred to the ear, and is rare, accounting for less than 1% of tinnitus cases 8. Vascular and neuromuscular causes are the more common causes of secondary tinnitus 8.
The onset of tinnitus occurs long after hearing loss in many patients 9 and it may be associated with negative life events such as unwanted retirement, redundancy, divorce 10), emotional stress, psychological factors, bereavement, unemployment, various physical or mental illnesses 11, noise exposure, and other somatic factors 12. The events that lead to tinnitus perception are referred to as “triggering factors” 12. Therefore, cochlear damage alone is not sufficient for the perception of tinnitus, with additional factors such as emotion or memory also making contributions 13.
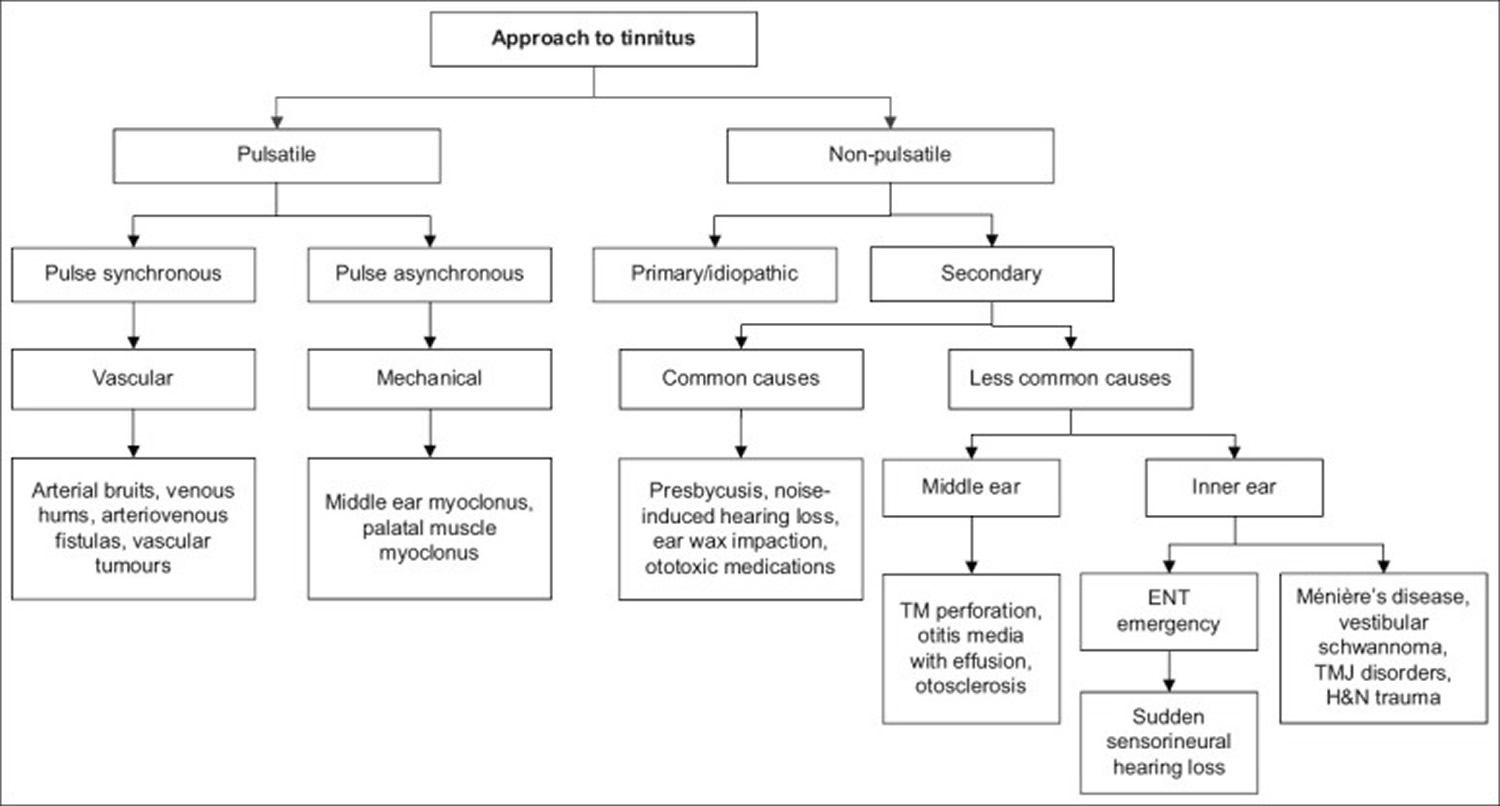
For the purposes of management, it is useful to first categorize tinnitus into pulsatile and non-pulsatile types 3:
- Non-pulsatile tinnitus is more common and can take on various qualities such as buzzing, ringing, crackling, humming or a cicada-like sound. The cause of non-pulsatile tinnitus remains speculative. Current hypotheses revolve around the concept of neural aberrancy in the cochlea, auditory nerve or along central auditory pathways. Common causes of non-pulsatile tinnitus include impacted ear wax, presbycusis, noise-induced hearing loss and ototoxicity. As tinnitus is frequently accompanied by hearing loss, the clinical approach to such tinnitus is similar to that for hearing loss. Other notable associated symptoms include dizziness, aural fullness, aural discharge and otalgia (ear pain).
- Pulsatile tinnitus, which is less frequently encountered with less than 10% of tinnitus patients will present with pulsatile tinnitus 14, can be classified into pulse synchronous and non-pulse synchronous types. The pulse synchronous tinnitus arises largely from vascular causes, while the non-pulse synchronous tinnitus is associated with middle ear or palatal muscle myoclonus. Vascular causes can then be broken down further into arterial vs. venous causes. Many times, this difference is possible with history and physical exam, but there is a crucial role for radiographic imaging as well 15.
If you have tinnitus, the first thing is to see your primary care doctor, who will check if anything, such as ear wax, is blocking the ear canal. Your doctor will ask you about your current health, medical conditions, including any medications you are taking to find out if an underlying condition is causing your tinnitus.
If your doctor cannot find any medical condition responsible for your tinnitus, you may be referred to an otolaryngologist (commonly called an ear, nose, and throat doctor, or an ENT). The ENT will physically examine your head, neck, and ears and test your hearing to determine whether you have any hearing loss along with the tinnitus. You might also be referred to an audiologist who can also measure your hearing and evaluate your tinnitus.
Some people find their tinnitus doesn’t go away or it gets worse. In some cases it may become so severe that you find it difficult to hear, concentrate, or even sleep. Tinnitus does not have a cure yet, but treatments that help many people cope better with tinnitus are available. Your doctor will work with you to help find ways to reduce the severity of the noise and its impact on your life.
Most doctors will offer a combination of the treatments below, depending on the severity of your tinnitus and the areas of your life it affects the most.
- Hearing aids often are helpful for people who have hearing loss along with tinnitus. Using a hearing aid adjusted to carefully control outside sound levels may make it easier for you to hear. The better you hear, the less you may notice your tinnitus.
- Cochlear implants are sometimes used in people who have tinnitus along with severe hearing loss. A cochlear implant bypasses the damaged portion of the inner ear and sends electrical signals that directly stimulate the auditory nerve. The device brings in outside sounds that help mask tinnitus and stimulate change in the neural circuits.
- Counseling helps you learn how to live with your tinnitus. Most counseling programs have an educational component to help you understand what goes on in the brain to cause tinnitus. Some counseling programs also will help you change the way you think about and react to your tinnitus. You might learn some things to do on your own to make the noise less noticeable, to help you relax during the day, or to fall asleep at night.
- Wearable sound generators are small electronic devices that fit in the ear and use a soft, pleasant sound to help mask the tinnitus. Some people want the masking sound to totally cover up their tinnitus, but most prefer a masking level that is just a bit louder than their tinnitus. The masking sound can be a soft “shhhhhhhhhhh,” random tones, or music.
- Tabletop sound generators are used as an aid for relaxation or sleep. Placed near your bed, you can program a generator to play pleasant sounds such as waves, waterfalls, rain, or the sounds of a summer night. If your tinnitus is mild, this might be all you need to help you fall asleep.
- Acoustic neural stimulation is a relatively new technique for people whose tinnitus is very loud or won’t go away. It uses a palm-sized device and headphones to deliver a broadband acoustic signal embedded in music. The treatment helps stimulate change in the neural circuits in the brain, which eventually desensitizes you to the tinnitus. The device has been shown to be effective in reducing or eliminating tinnitus in a significant number of study volunteers.
- Antidepressants and antianxiety drugs might be prescribed by your doctor to improve your mood and help you sleep. Other medications may be available at drugstores and on the Internet as an alternative remedy for tinnitus, but none of these preparations has been proved effective in clinical trials.
Figure 1. Tinnitus types
Abbreviations: ENT = ear, nose and throat; H&N = head & neck; TM = tympanic membrane; TMJ = temporomandibular joint
[Source 3 ]Some people aren’t very bothered by tinnitus. For other people, tinnitus disrupts their daily lives. If you have tinnitus that bothers you, see your doctor.
Red flag signs for tinnitus 16:
- Pulsatile tinnitus
- Unilateral tinnitus with abrupt onset
- Tinnitus with acute hearing difficulty
- Any tinnitus with concomitant neurologic deficit
- Any tinnitus with audible bruit or hums
Make an appointment to see your doctor if:
- You develop tinnitus after an upper respiratory infection, such as a cold, and your tinnitus doesn’t improve within a week.
- You have tinnitus regularly or constantly
- Your tinnitus is getting worse
- Your tinnitus is bothering you – for example, it’s affecting your sleep or concentration, or is making you feel anxious and depressed
- You have tinnitus that beats in time with your pulse
See your doctor as soon as possible if:
- You have hearing loss or dizziness with the tinnitus.
- You are experiencing anxiety or depression as a result of your tinnitus.
Is there a cure for tinnitus?
No. Although there is no one “cure” for tinnitus, there are several options available that can help patients with tinnitus. Because tinnitus is relatively common and not always worrisome, not all patients need an evaluation. If your ENT specialist finds a specific cause for your tinnitus, they may be able to offer specific treatment to eliminate the noise. This may include removing wax or hair from your ear canal, treating middle ear fluid, treating arthritis in the jaw joint, etc. For many patients who have experienced tinnitus for less than six months, its natural course is to improve over time, and most people do not go on to have persistent, bothersome tinnitus.
Some patients with hearing loss and tinnitus have improvement with the use of hearing aids, with or without built-in ear-level maskers. Sound therapies that involve simple things like background music or noise or specialized ear-level maskers may be a reasonable treatment option. The effects of tinnitus on quality of life may also be improved by cognitive behavioral therapy (CBT) counseling, which usually involves a series of weekly sessions led by a trained professional.
Why is my tinnitus so loud at night?
Tinnitus is a sound that is “masked” by external sounds such as office or traffic noise, TV or radio, etc. It is also not perceived when the brain is busy elsewhere, such as at work. At night, when external sounds are at a minimum and the brain is not focused on something else, tinnitus often sounds much louder and becomes more bothersome. In general, use of a sound generator at night is very helpful in decreasing the disturbance of tinnitus. If tinnitus is interfering with your sleep, you should inform your doctor.
Can other people hear the noise in my ears?
Not usually. Most of the time, the tinnitus is “subjective,” meaning that it is only heard by you. In rare cases of “objective tinnitus,” others may be able to use a special in-the-ear microphone to hear what you hear.
Can children be at risk for tinnitus?
It is relatively rare, but not unheard of, for patients under 18-years-old to have tinnitus as a primary complaint. However, it is possible that tinnitus in children is significantly under-reported, in part because young children may not be able to express this complaint. Also, in children with congenital sensorineural hearing loss that may be accompanied by tinnitus, this symptom may be unnoticed because it is something that is constant in their lives. In fact, they may habituate to it; the brain may learn to ignore this internal sound.
In pre-teens and teens, the highest risk for developing tinnitus is associated with exposure to high intensity sounds, specifically listening to music. It can be difficult for parents to monitor the level of sound exposure to teens using personal music devices or hand-held electronic games with ear buds. Therefore, the best and most effective mode of prevention of tinnitus in children is proper education on the risks of excessive sound exposure in combination with proper monitoring by parents or other caregivers. Limits on the maximum volume output can be programmed into many electronic devices.
Anatomy of tinnitus
- Cochlea. The most common cause of tinnitus is noise-induced hearing loss, followed by changes in the central auditory pathway 17. However, some people with tinnitus exhibit normal hearing ability 18, which is probably due to their degree of hearing impairment not being detectable in a standard audiological examination 17. On the other hand, many people with hearing loss never develop tinnitus 18.
- Somatosensory system. Tinnitus may be provoked or modulated by stimulation from the somatosensorial system 19. Somatosensory stimuli disinhibit the ipsilateral cochlear nucleus to produce excitatory neuronal activity within the auditory pathway that results in tinnitus. However, tinnitus without hearing loss following trauma makes the association more tenuous and raises the possibility of trauma only indirectly causing tinnitus, perhaps via a somatic mechanism 20.
- Brain cortex. Damage to the brain cortex related to auditory perception alone can lead to tinnitus without contributions from peripheral influences. Examples include acute hemorrhage of a small cavernous angioma located adjacent to the contralateral primary auditory cortex 21 and a lesion involving the superior temporal gyrus and the inferior portion of the supramarginal gyrus 22.
- Dorsal cochlear nucleus. Several studies have speculated that altered neuronal activity at the level of the dorsal cochlear nucleus is primarily involved in tinnitus induction, due to an interplay between nonauditory brainstem structures and that nucleus 23. However, while the dorsal cochlear nucleus may be necessary for tinnitus initiation, it is not necessary for the maintenance of chronic tinnitus 24.
- Inferior colliculus. Hyperactivity of inferior colliculus neurons might be associated with chronic tinnitus but not with acute tinnitus 24.
- Thalamus. The thalamus is a structure that gaits sensory signals to the cortex to which the limbic structures of the brain are connected 24. The pathway from the medial geniculate body to the amygdala provides a possible key connection between the perception of tinnitus and the associated emotional component 24.
Figure 2. Ear structure
Figure 3. Ear anatomy
Figure 4. Middle ear and auditory ossicles
Figure 5. Parts of the inner ear
Figure 6. The Cochlea (cross section view)
Footnote: a) Cross section of the cochlea. (b) The spiral organ and the tectorial membrane.
Tinnitus classification
Tinnitus has been classified in several ways, such as subjective or objective; primary or secondary; pulsatile or nonpulsatile; tonal or nontonal; and acute or chronic. Tinnitus classification into subjective and objective tinnitus is common. Subjective tinnitus is the most common type, and is audible only to the affected individuals, without internal or external sound input. Whereas objective tinnitus can also be heard by an external observer, such as a bruit, as tinnitus 25. Objective tinnitus is rare, accounting for less than 1% of cases 26. For mechanically induced objective tinnitus to be heard by anyone, the sound intensity needs to exceed a certain threshold. This means that “objective tinnitus” is a misleading term, and experts instead prefer to call it “somatosound” 24. The causes of objective tinnitus are chiefly vascular or muscle dysfunction 27.
While the causes of tinnitus are benign in most cases, the clinical significance of objective tinnitus covers a wide variety that clinicians should be aware of. Somatosound is often generated in various parts of the body, including the ear, head, neck, and other vascular structures such as arteriovenous malformations or fistulas, cavernous hemangiomas, aneurysms, and vascular stenosis 28. Sometimes muscular structures are responsible for somatosound, and symptoms of tinnitus that are abrupt, unilateral, and pulsatile with or without a neurological deficit could be considered as red-flag signs. For example, muscular tremor can be heard in patients with a lesion in the Guillain-Mollaret triangle that could be caused by ischemic, neoplastic, demyelinating, traumatic, inflammatory, or rare neurodegenerative processes such as progressive supranuclear palsy, multiple system atrophy, or amyotrophic lateral sclerosis.
Tinnitus is also classified as either primary or secondary tinnitus 1:
Primary tinnitus is used to describe tinnitus that is idiopathic and may or may not be associated with sensorineural hearing loss. Although there is currently no cure for primary tinnitus, a wide range of therapies has been used and studied in attempts to provide symptomatic relief. These therapies include education and counseling, auditory therapies that include hearing aids and specific forms of sound therapy, cognitive behavioral therapy (CBT), medications, dietary changes and supplements, acupuncture, and transcranial magnetic stimulation (TMS).
Secondary tinnitus is tinnitus that is associated with a specific underlying cause (other than sensorineural hearing loss) or an identifiable organic condition. It is a symptom of a range of auditory and nonauditory system disorders that include simple cerumen impaction of the external auditory canal, middle ear diseases such as otosclerosis or Eustachian tube dysfunction, cochlear abnormalities such as Ménière’s disease, and auditory nerve pathology such as vestibular schwannoma (acoustic neuroma). Nonauditory system disorders that can cause tinnitus include vascular anomalies, myoclonus, and intracranial hypertension. Management of secondary tinnitus is targeted toward identification and treatment of the specific underlying condition and is not the focus of this guideline.
Tinnitus can also be categorized based on the sound being either pulsatile or nonpulsatile 29. This kind of clinical categorization is helpful in the differential diagnosis 29. Nonpulsatile tinnitus is often associated with age-related hearing loss and noise exposure 29. Neurological disorders such as brainstem infarction, cerebellopontine-angle tumor, and multiple sclerosis are known to cause unilateral nonpulsatile tinnitus 30. On the other hand, pulsatile tinnitus can be either subjective or objective depending on its cause and severity 25. Intracranial hypertension is one of the most common causes of subjective pulsatile tinnitus 31. Pulsatile tinnitus often has vascular origins and so is associated with the pulse, leading to so-called vascular tinnitus caused by conditions such as arterial bruits, high jugular bulb with or without diverticulum, systemic hypertension, venous hums, arteriovenous malformation, and vascular tumors 32. The relatively common condition of a high jugular bulb often results in vascular tinnitus that is audible to an examiner 32. The advent of high-resolution computed tomography (CT) scanning in the 1980s led to temporal-bone computed tomography (TBCT), which offers the highest structural resolution of the currently available imaging modalities and enables the identification of many vital structures in the inner ear, temporomandibular joint (TMJ), and adjacent vascular cavities including the carotid canal and jugular bulb 33. A high jugular bulb often causes vascular tinnitus, and TBCT is the first choice for detecting venous anomalies 32. One study found that a high jugular bulb was responsible for 47.4% of vascular tinnitus following venous hum (17.5%).
Another way to classify tinnitus is according to whether the sound is tonal or nontonal 34. Many clinicians use the term “tinnitus” when referring to tonal nonpulsatile tinnitus. Tinnitus can also be classified into acute or chronic depending on the duration of symptoms. Tinnitus that is temporary (lasting for up to 3 months) is referred to as acute tinnitus, while chronic or ongoing tinnitus refers to the condition lasting for longer than 3 months 35. This kind of duration-related classification is neither helpful nor reliable because the description of symptoms is solely based on the patient’s history. Nonetheless, timely management is required when acute-onset tinnitus is accompanied with an unexplained balance problem and focal neurological symptoms, which is one of the red-flag signs prompting diagnostic workups such as TBCT or MRI 36.
Pulsatile tinnitus
Pulsatile tinnitus is a rhythmical noise you hear in your head and/or ears that is usually at the same rate as your heart beat. This is easily checked by feeling your pulse at the same time as listening to the tinnitus. Pulsatile tinnitus is usually due to a change in blood flow or change in awareness of that blood flow, in the vessels near your ear. Pulsatile tinnitus should be investigated and there are a number of different tests which may be suggested.
When doctors investigate cases of tinnitus, it is rare for them to find a single identifiable cause for the problem. With pulsatile tinnitus, the chances of finding a specific cause are more likely than in the non-pulsatile form, but it is still difficult to identify a definite cause. In about 70% of the cases with pulsatile tinnitus, an underlying cause can be identified by adequate diagnostic work-up 37.
If there is a physical reason for the pulsatile tinnitus, treating the underlying cause can help.
Pulsatile tinnitus causes
Pulsatile tinnitus is due to a change in blood flow in the vessels near the ear or to a change in awareness of that blood flow. The involved vessels include the large arteries and veins in your neck and base of the skull and smaller ones in the ear itself. The blood flow can be altered by a variety of factors.
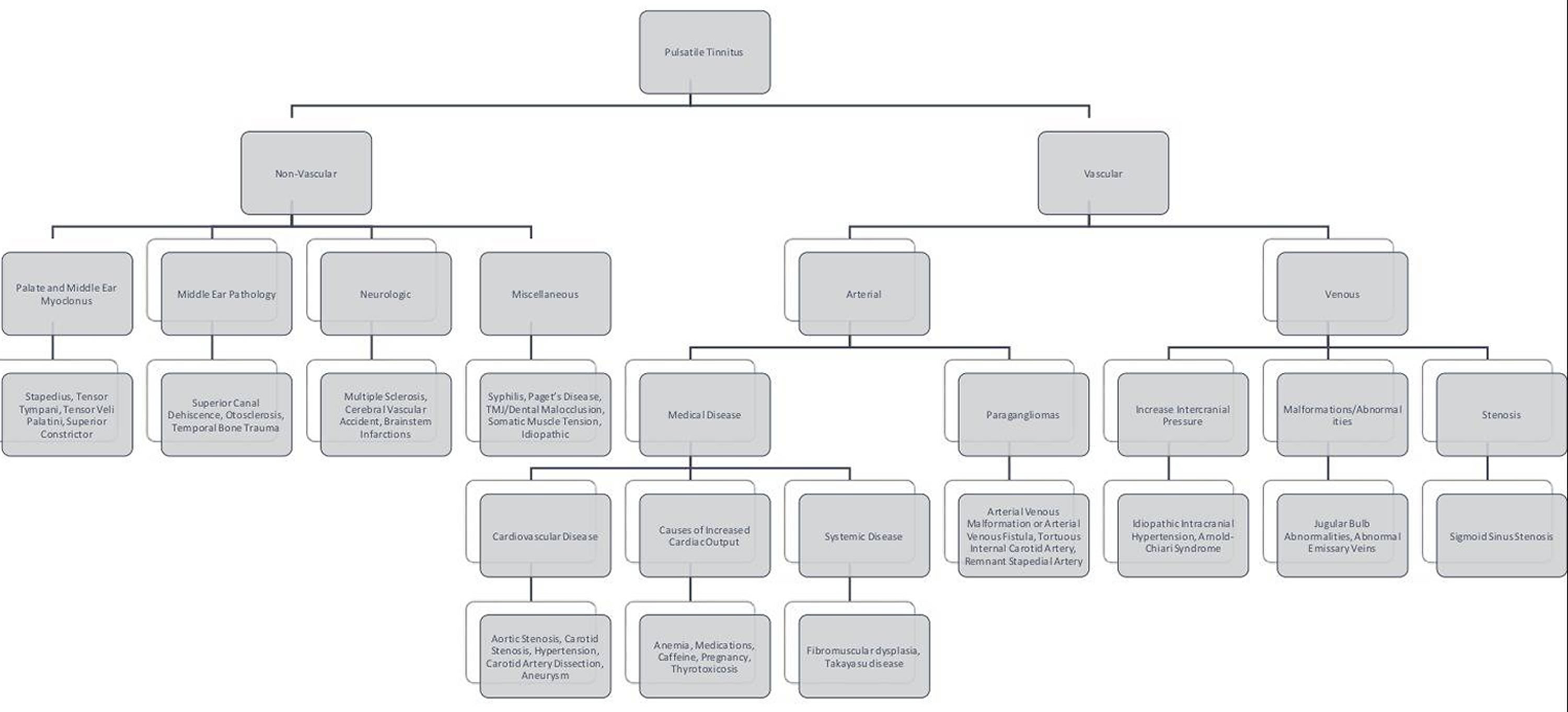
The cause of pulsatile tinnitus can be broadly broken down into two categories: vascular and non-vascular.
Vascular causes can be subcategorized into arterial vs. venous, with arterial causes being more common 38. Vascular causes of pulsatile tinnitus include dural arteriovenous fistula, arteriovenous malformation (AVM), aneurysm, internal carotid artery stenosis or dissection, congenital vascular variants, transverse sinus stenosis, or increased cardiac output 39. However, the most common cause of intermittent pulsatile tinnitus is uncontrolled hypertension, and appropriate management of this condition is paramount before proceeding with further interventions. Another common arterial cause is turbulent flow through arteries, various conditions can disrupt the laminar flow leading to turbulence, and it is this turbulent flow that patients can hear, causing pulsatile tinnitus. The most common cause of pulsatile tinnitus is atherosclerotic carotid disease. Stenosis in the carotid arteries will cause turbulent flow through the carotids, which will be perceived by the patient as ipsilateral pulsatile tinnitus (tinnitus in same side of the carotid artery). Natural variation in the position of the basilar artery can similarly cause pulsatile tinnitus, even in a normotensive patient without atherosclerotic disease 40. Stenosis may also be due to more systemic disease such as fibromuscular dysplasia or Takayasu disease, though these are much rarer. Another vascular cause is paragangliomas, also known as glomus tumors of the jugular foramen and middle ear or of the carotid body. This condition may is observable on otoscopy, and patients will usually present with unilateral pulsatile tinnitus (tinnitus in one ear) that is objectively heard on auscultation of the neck or ear by the examiner. The most common venous cause is idiopathic intracranial hypertension, also known as pseudotumor cerebri. These patients may have bilateral pulsatile tinnitus; this is most commonly seen in young, obese females who may also complain of vision changes and headaches. The proposed pathophysiology is that patients perceive rhythmic changes in cerebrospinal fluid pressure.
- Arterial bruits. Turbulent flow through atherosclerotic vessels in the neck, temporal bone and the cranium produces a bruit. Such patients complain of pulsatile tinnitus in one or both ears, but it is typically louder on the side of the pathology. They also usually have no other otologic complaints such as aural fullness or hearing loss, and their tinnitus is loudest in quiet environments.
- Intracranial vascular malformations. Congenital arteriovenous malformations (AVMs) are rarely associated with tinnitus, while the acquired-type arteriovenous fistula from head trauma or surgery is more symptomatic, ipsilateral to the fistula. Large dural arteriovenous fistula can cause devastating intracranial hemorrhages, and early detection is important.
- Vascular tumors. Tympanojugular glomus tumors are the most common tumors of the middle ear. They arise from paraganglia cells over the jugular bulb or promontory. An important cause of pulsatile tinnitus, they present as a pulsating red mass in the middle ear on otoscopy. Although benign, they are locally aggressive. Management involves watchful waiting, surgery or radiotherapy.
- Venous hums. Venous hums might be heard in patients with idiopathic intracranial hypertension or those with anomalies in their intracranial venous systems, including abnormally high placement of the jugular bulb or diverticulum of the sigmoid sinus. It is often described by patients as a soft, low-pitched hum that stops with a change of head position or compression at the base of the neck 41.
- Non-pulse synchronous pulsatile tinnitus is commonly due to neuromuscular disorders such as middle ear myoclonus and palatal myoclonus. Myoclonus of the muscles of the middle ear (tensor tympani and stapedius muscles) or palate can be idiopathic or secondary to neuromuscular disorders such as multiple sclerosis. Such myoclonus is usually diagnosed from history, as patients are frequently asymptomatic at the time of consultation.
The less common non-vascular causes of pulsatile tinnitus include metabolic diseases causing increase cardiac output (such as pregnancy, anemia, and thyrotoxicosis), myoclonus of palate and middle ear musculature, neoplasm like paraganglioma, osseous pathology (e.g. Paget’s disease, otosclerosis, osseous hemangioma, basal meningeoma, Langerhans cell histiocytosis, or bone metastases) and idiopathic intracranial hypertension (pseudotumor cerebri) 15, 42. Figure 7 is a flowchart with a more extensive list of other causes that can cause pulsatile tinnitus. It organizes in a way that can help narrow down the differential diagnosis, which will, in turn, help guide management decisions 43, 15, 44.
Figure 7. Pulsatile tinnitus causes
[Source 40 ]Pulsatile tinnitus complications
Complications from pulsatile tinnitus will vary based on the etiology. Some pathology will be benign to the patient; however, the patient’s tinnitus may be a symptom of a much more serious disease. Morbidity is possible both from the pathophysiology itself and as a result of attempting to treat the patient with invasive modalities such as surgery and radiation.
Pulsatile tinnitus diagnosis
Your doctor will start by taking a detailed history of the tinnitus and will ask about any other medical conditions that you may have. Your doctor will then examine you, paying particular attention to your ear drums and the blood vessels of your neck. A stethoscope may be used to listen to your neck and skull–if your doctor can hear a pulsatile noise through the stethoscope this is referred to as objective pulsatile tinnitus. Pulsatile tinnitus that cannot be heard by the doctor is called subjective pulsatile tinnitus. People with any form of tinnitus will have a series of hearing tests including pure tone and speech audiometry with tympanograms and pulsatile tinnitus is no different in this respect. If the examiner notes a low-frequency loss of at least 20 dB, it is appropriate to repeat an audiogram with light pressure over the ipsilateral internal jugular vein 38. The resolution of deficit may be suggestive of idiopathic intracranial hypertension (pseudotumor cerebri) 40. Though the results of basic metabolic tests will likely be normal, they can be used to rule out certain medical diseases that may cause elevated cardiac output causing patients to have pulsatile tinnitus.
Blood tests may be needed in the investigation of pulsatile tinnitus. For example, a complete blood count (CBC) may be required to rule out anemia or thyroid function tests may be requested if an overactive thyroid gland is suspected. If benign intracranial hypertension is suspected, the doctor may ask for opinions from other doctors such as ophthalmologists or neurologists who may request their own specialized investigations.
People with pulsatile tinnitus will generally then undergo some form of medical imaging. This has changed dramatically in recent years and a wider range of techniques are now available:
- Ultrasound. Modern ultrasound scanning uses a technique called Doppler, which can show the blood flow within the blood vessels in the neck.
- Magnetic resonance imaging (MRI). This produces pictures of the head and inner ears using magnetic fields rather than X-rays. Some conditions are better shown with MRI; some are better shown with CT. Therefore the tests are complementary and some people may need both CT and MRI scans.
- Magnetic resonance angiography (MRA). MRA can be used to produce images of the inside of arteries or veins and can show up irregularities or narrowing of the vessel.
- Magnetic resonance venography (MRV). An MRV uses magnetic resonance technology and intravenous (IV) contrast dye to visualize the veins. Contrast dye causes the blood vessels to appear opaque on the X-ray image, allowing the physician to visualize the blood vessels being evaluated.
- Computerized tomography (CT). This technique uses computer controlled X-rays to generate detailed images of the body.
- Computerized tomographic angiography (CTA). By giving an injection of a substance that shows up on X-rays (contrast medium) and then performing a CT scan it is possible to obtain images of the inside of blood vessels.
- Angiography. This is a way of looking at the inside of vessels by injecting contrast medium into the vessel under investigation and taking a conventional X-ray. It still produces clearer, more detailed pictures of vessels than any of the other techniques and therefore is still used in selected cases.
Following audiogram and basic labs, clinical suspicion should guide the work-up 15. Doppler ultrasound should be ordered for suspected carotid stenosis before ordering more advanced radiological studies, but may not be helpful in non-carotid arterial causes. In general, both CT and MRI are complementary imaging modalities to identify vascular etiologies of pulsatile tinnitus. Suspected arterial pathologies not well defined by duplex should get a computerized tomographic angiography (CTA). CTA may also identify aneurysms, which may manifest as pulsatile tinnitus. Magnetic Resonance Venography (MRV) better evaluates venous cause. It is appropriate to get a CT of the temporal bones if there is clinical suspicion for temporal bone pathology. Patients with focal nerve deficits are candidates for brain imaging, either CT or MRI, to evaluate for more serious causes of pulsatile tinnitus 45. Other conditions may require further evaluation by specialists such as idiopathic intracranial hypertension (pseudotumor cerebri), which can be diagnosed by normal brain CT/MRI and increased opening pressure on lumbar puncture. Performing an optic exam on these patients may reveal papilledema.
Pulsatile tinnitus treatment
Up to 70% of patients will have an identifiable cause of their pulsatile tinnitus, which will direct management 15. Initial management should be focused on resolving underlying causes. Therapeutic interventions may include a wide variety of medical professionals working together to coordinate care. Treatment can range from observation to medical management and surgery 46.
If a specific cause of pulsatile tinnitus is found, this may point to a specific solution. For example, anemia can be treated with medication or blood transfusion, glue ear can be treated with grommets, perforations can be closed with grafts and narrowed segments of artery can be repaired.
Some causes are less amenable to treatment: if the pulsatile tinnitus is due to a specific blood vessel, these may not be treatable, depending on location.
For those people with pulsatile tinnitus who have no demonstrable abnormality, there are a variety of methods to manage the tinnitus which people find helpful. These include techniques such as sound therapy, relaxation therapy, cognitive behavior therapy (CBT), counseling, mindfulness meditation, or tinnitus retraining therapy, but there are no studies regarding their efficacy specifically in pulsatile tinnitus patients 47.
Some treatments for tinnitus, such as ear syringing to clear ear wax, cessation of ototoxic medication, avoidance of exposure to loud noise and decreasing caffeine intake, may be offered to patients
Patients should also be asked to maintain a healthy lifestyle with regular exercise and proper sleep, as cardiovascular health and stress levels can determine the severity of tinnitus. Although stress itself is not a cause of tinnitus, as in any condition, stress and anxiety can make the condition worse. As most patients are most bothered by their tinnitus in quiet environments, they should be advised on the use of ambient noise from televisions, radios and tinnitus smartphone applications to ‘mask’ their tinnitus in such environments.
Pulsatile tinnitus prognosis
The prognosis for pulsatile tinnitus varies considerably based on the underlying cause. Pulsatile tinnitus due to extensive cardiovascular disease may have a detrimental impact on patient morbidity and mortality. However, other causes may have no serious long-term effects on the patient. It is also possible that patients will have a resolution of their symptoms following treatment of the underlying cause. Early detection and treatment are the optimal means to improve patient outcomes.
Tinnitus causes
A number of health conditions can cause or worsen tinnitus. In many cases, an exact cause is never found.
Tinnitus may occur when there is a problem with the auditory or hearing system, which is made up of the ears and parts of the brain 48. Tinnitus is more common in people who have some hearing loss or other ear problem, but it can also occur in people who have normal hearing. Tinnitus is almost always triggered by hearing loss, but a large proportion of patients with hearing loss do not present symptoms of tinnitus 49. Authors have shown that tinnitus patients had specific inner ear damage that triggers tinnitus.
Although you hear tinnitus in your ears, its source is really in the networks of brain cells (what scientists call neural circuits) that make sense of the sounds your ears hear 50. A way to think about tinnitus is that it often begins in your ear, but it continues in your brain. Scientists still haven’t agreed upon what happens in your brain to create the illusion of sound when there is none. Some think that tinnitus is similar to chronic pain syndrome, in which the pain persists even after a wound or broken bone has healed.
Tinnitus could be the result of your brain’s neural circuits trying to adapt to the loss of sensory hair cells by turning up the sensitivity to sound in the cortical and subcortical auditory regions and also in the nonauditory brain regions involved in attention, emotion, and memory 51. This would explain why some people with tinnitus are oversensitive to loud noise. However, it is still unclear how hearing loss can result in increased central activity. Hearing loss causes a reduction of the afferent drive of auditory impulses, alters the balance between inhibition and excitation, and thus raises spontaneous neural activity in the central auditory system through the activation of neural plasticity 51.
Tinnitus also could be the result of neural circuits thrown out of balance when damage in your inner ear changes signaling activity in the auditory cortex, the part of the brain that processes sound 52. Or it could be the result of abnormal interactions between neural circuits 51. The neural circuits involved in hearing aren’t solely dedicated to processing sound. They also communicate with other parts of the brain, such as the limbic region, which regulates mood and emotion 51.
In many people, tinnitus is caused by one of the following:
- Hearing loss. Most cases of tinnitus are caused by sensorineural hearing loss 29. There are tiny, delicate hair cells in your inner ear (cochlea) that move when your ear receives sound waves (see Figure 6). This movement triggers electrical signals along the nerve from your ear to your brain (auditory nerve). Your brain interprets these signals as sound. If the hairs inside your inner ear are bent or broken — this happens as you age or when you are regularly exposed to loud sounds — they can “leak” random electrical impulses to your brain, causing tinnitus. As sensorineural hearing loss cannot be reversed, primary prevention is vital. High-volume music through headphones from portable listening devices, including smartphones, has a substantial damaging effect on the auditory system 53. Dietary factors, including increased glycemic load and hypercholesterolemia, are associated with increased risk of age-related hearing loss 54. Dietary changes to reduce carbohydrate and cholesterol intake might prevent or delay the onset of sensorineural hearing loss 54.
- Presbycusis also known as age-related hearing loss and occurs in the elderly. It is believed to be caused by an accumulation of insults to the inner ear (e.g. noise, ototoxicity), on a background of genetic predisposition. Typically, the onset and progression of tinnitus and hearing loss are gradual, with high frequencies affected first.
- Noise-induced hearing loss. Noise exposure is another major cause of sensorineural hearing loss and tinnitus. The tinnitus often precedes subjective hearing loss and serves as an early indicator of cochlear hair cell dysfunction 55. Heavy equipment, environmental exposure or portable music devices that are played loudly for long periods of time are common sources of loud noises. Tinnitus from brief exposure, such as attending a loud concert, usually resolves. However, tinnitus from long-term or high-intensity exposure can be permanent. Similar to the perceived effects of smoking, which are distant and intangible, so too are the adverse effects of noise exposure. As noise damage is related to the intensity and duration of exposure, the 80-to-90 rule (volume 80% of maximum, listen for < 90 minutes a day) is recommended to prevent noise damage 56. Using occlusive headphones can also decrease external noise and lessen the intensity of sound delivered 56. To prevent noise damage in the workplace, employers must be aware of occupational exposure limits, employ regular audiometry evaluations, and provide appropriate hearing protection 57.
- Ear infection or ear canal blockage. Your ear canals can become blocked with a buildup of fluid (ear infection), earwax, dirt or other foreign materials. A blockage can change the pressure in your ear, causing tinnitus.
- Middle ear pathologies. Middle ear pathologies such as tympanic membrane perforation, otitis media with effusion, and otosclerosis can also present with tinnitus. Most of these can be treated effectively with surgery. In the local context, adults should be screened for nasopharyngeal carcinoma when they present with otitis media with effusion.
- Head or neck injuries. Head or neck trauma can affect the inner ear, hearing nerves or brain function linked to hearing. Such injuries usually cause tinnitus in only one ear.
- Medications. More than 130 medications have been reported to cause tinnitus or hearing loss 58. Generally, the higher the dose of these medications, the worse tinnitus becomes. Often the unwanted noise disappears when you stop using these drugs. Medications known to cause tinnitus include nonsteroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics (e.g. aminoglycosides, vancomycin, macrolides), cancer drugs (e.g. cisplatin), water pills (diuretics) (e.g. furosemide), antimalarial drugs (e.g. quinine) and antidepressants. Table 1 lists common medications consistently associated with tinnitus 58, 59.
Less common causes of tinnitus include other ear problems, chronic health conditions, and injuries or conditions that affect the nerves in your ear or the hearing center in your brain.
- Meniere’s disease. Tinnitus can be an early indicator of Meniere’s disease, an inner ear disorder that may be caused by abnormal inner ear fluid pressure. Ménière’s disease is a disorder of the inner ear characterized by recurrent episodic vestibular symptoms associated with sensorineural hearing loss, tinnitus and aural fullness 60.
- Eustachian tube dysfunction. In this condition, the tube in your ear connecting the middle ear to your upper throat remains expanded all the time, which can make your ear feel full.
- Ear bone changes. Stiffening of the bones in your middle ear (otosclerosis) may affect your hearing and cause tinnitus. This condition, caused by abnormal bone growth, tends to run in families.
- Muscle spasms in the inner ear. Muscles in the inner ear can tense up (spasm), which can result in tinnitus, hearing loss and a feeling of fullness in the ear. This sometimes happens for no explainable reason, but can also be caused by neurologic diseases, including multiple sclerosis.
- Temporomandibular joint (TMJ) disorders. Problems with the TMJ, the joint on each side of your head in front of your ears, where your lower jawbone meets your skull, can cause tinnitus, but the exact mechanism is unknown. The tinnitus may improve when patients respond favourably to treatment for symptoms of TMJ dysfunction and craniocervical disease 61.
- Blunt head and neck trauma can also affect peripheral and central auditory pathways. Such injuries can cause tinnitus and non-specific dizziness.
- Acoustic neuroma or other head and neck tumors. Acoustic neuroma also known as vestibular schwannoma, is a noncancerous (benign) tumor that develops on the cranial nerve that runs from your brain to your inner ear and controls balance and hearing. Acoustic neuroma (vestibular schwannoma) is confined to the internal auditory canal and/or cerebellopontine angle. Compression of the adjacent cochlear nerve results in unilateral tinnitus and asymmetrical hearing loss. Dizziness is not as pronounced, as these tumors are slow-growing and allow for vestibular compensation. Older patients with acoustic neuroma (vestibular schwannoma) appear to suffer from more disabling tinnitus 62. Other head, neck or brain tumors can also cause tinnitus.
- Blood vessel disorders. Conditions that affect your blood vessels — such as atherosclerosis, high blood pressure, or kinked or malformed blood vessels — can cause blood to move through your veins and arteries with more force. These blood flow changes can cause tinnitus or make tinnitus more noticeable.
- Other chronic conditions. Conditions including diabetes, thyroid problems, migraines, anemia, and autoimmune disorders such as rheumatoid arthritis and lupus have all been associated with tinnitus.
Table 1. Medications associated with tinnitus
| Drug class | Specific agents | Comments |
|---|---|---|
| Anti-inflammatory agents | Aspirin | Especially doses > 2.7 g per day |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | All agents implicated | |
| Sulfasalazine (Azulfidine) | — | |
| Antimalarial agents | Quinine and chloroquine (Aralen) | — |
| Antimicrobial agents | Aminoglycosides | Tinnitus usually is an initial sign of ototoxicity, often with rapid progression to hearing loss; hearing loss or tinnitus that persists two to three weeks after discontinuing the drug is likely permanent |
| Macrolides | Erythromycin: rare at dosages < 2 g per day | |
| Tetracyclines: doxycycline, minocycline (Minocin) | Higher risk in women; symptom onset one to three days after initiation of therapy | |
| Vancomycin | Rare if not used with other ototoxic agents | |
| Other anti-infectives: imipenem/cilastatin (Primaxin), linezolid (Zyvox), sulfonamides, fluoroquinolones, voriconazole (Vfend), amphotericin B, ganciclovir (Cytovene), ribavirin (Rebetol) | — | |
| Antineoplastic agents | Vinca alkaloids, etoposide, protein kinase inhibitors, platinum derivatives | — |
| Loop diuretics | All agents implicated | Highest risk with high doses and/or rapid infusions |
| Miscellaneous agents | Antiarrhythmics, anticonvulsants, antihypertensives, antiulcer drugs, hormones, psychotropic drugs, atorvastatin (Lipitor), bupropion (Wellbutrin), risedronate (Actonel), varenicline (Chantix) | — |
| Regional anesthetics | Lidocaine (Xylocaine), bupivacaine (Marcaine) | — |
| Topical agents | Topical otic preparations containing ototoxic drugs | — |
Figure 8. Causes and mechanisms of tinnitus
Footnotes: The main causes of tinnitus are hearing loss, somatosensory system dysfunction, and auditory cortex lesions. 1) The most common cause of tinnitus is hearing loss. 2) Somatosensory stimuli disinhibit the ipsilateral cochlear nucleus, producing excitatory neuronal activity within the auditory pathway that results in tinnitus. 3) Damage to the brain cortex related to auditory perception alone can lead to tinnitus without contributions from peripheral influences such as hearing loss. 4) The socalled inhibitory gating mechanism blocks the tinnitus signal at the level of the thalamus. 5) An inhibitory feedback loop originates in paralimbic structures.
[Source 16 ]Risk factors for developing tinnitus
Anyone can experience tinnitus, but these factors may increase your risk:
- Loud noise exposure. Loud noises, such as those from heavy equipment, chain saws and firearms, are common sources of noise-related hearing loss. Portable music devices, such as MP3 players, also can cause noise-related hearing loss if played loudly for long periods. People who work in noisy environments — such as factory and construction workers, musicians, and soldiers — are particularly at risk.
- Age. As you age, the number of functioning nerve fibers in your ears declines, possibly causing hearing problems often associated with tinnitus.
- Sex. Men are more likely to experience tinnitus.
- Tobacco and alcohol use. Smokers have a higher risk of developing tinnitus. Drinking alcohol also increases the risk of tinnitus.
- Certain health problems. Obesity, cardiovascular problems, high blood pressure, and a history of arthritis or head injury all increase your risk of tinnitus.
Tinnitus pathophysiology
Most people with chronic tinnitus have some degree of hearing loss 63 and the prevalence of tinnitus increases with greater hearing loss 64. The varying theories of tinnitus generation involve changes in either function or activity of the peripheral (cochlea and auditory nerve) or central auditory nervous systems 10). Theories involving the peripheral systems include the discordant damage theory, which predicts that the loss of outer hair cell function, where inner hair cell function is left intact, leads to a release from inhibition of inner hair cells and aberrant activity (typically hyperactivity) in the auditory nerve 65. Such aberrant auditory nerve activity can also have a biochemical basis, resulting from excitotoxicity or stress‐induced enhancement of inner hair cell glutamate release with up‐regulation of N‐methyl‐D‐aspartate (NMDA) receptors 66.
In the central auditory system, structures implicated as possible sites of tinnitus generation include the dorsal cochlear nucleus 67, the inferior colliculus 68 and the auditory and non‐auditory cortex. There is a strong rationale that tinnitus is a direct consequence of maladaptive neuroplastic responses to hearing loss 69. This process is triggered by sensory deafferentation and a release from lateral inhibition in the central auditory system allowing irregular spontaneous hyperactivity within the central neuronal networks involved in sound processing 70. As a consequence of this hyperactivity, a further physiological change noted in tinnitus patients is increased spontaneous synchronous activity occurring at the cortical level, measurable using electroencephalography (EEG) or magnetoencephalography (MEG) 71. Another physiological change thought to be involved in tinnitus generation is a process of functional reorganisation, which amounts to a change in the response properties of neurons within the primary auditory cortex to external sounds. This effect is well demonstrated physiologically in animal models of hearing loss 72. Evidence in humans, however, is limited to behavioural evidence of cortical reorganization after hearing loss, demonstrating improved frequency discrimination ability at the audiometric edge 73, although Buss 1998 74 did not find this effect.
It is also proposed that spontaneous hyperactivity could cause an increase in sensitivity or ‘gain’ at the level of the cortex, whereby neural sensitivity adapts to the reduced sensory inputs, in effect stabilising mean firing and neural coding efficiency 75. Such adaptive changes would be achieved at the cost of amplifying ‘neural noise’ due to the overall increase in sensitivity, ultimately resulting in the generation of tinnitus.
Increasingly, non‐auditory areas of the brain, particularly areas associated with emotional processing, are also implicated in bothersome tinnitus 76. Vanneste 76 describes tinnitus as “an emergent property of multiple parallel dynamically changing and partially overlapping sub‐networks”, implicating the involvement of many structures of the brain more associated with memory and emotional processing in tinnitus generation. However, identification of the structural components of individual neural networks responsible for either tinnitus generation or tinnitus intrusiveness, which are independent of those for hearing loss, remains open to future research 77.
One further complication in understanding the pathophysiology of tinnitus is that not all people with hearing loss have tinnitus and not all people with tinnitus have a clinically significant hearing loss. Other variables, such as the profile of a person’s hearing loss, may account for differences in their tinnitus report. For example, König 78 found that the maximum slope within audiograms was higher in people with tinnitus than in people with hearing loss who do not have tinnitus, despite the ‘non‐tinnitus’ group having the greater mean hearing loss. This suggests that a contrast in sensory inputs between regions of normal and elevated threshold may be more likely to result in tinnitus.
Tinnitus prevention
In many cases, tinnitus is the result of something that can’t be prevented. However, some precautions can help prevent certain kinds of tinnitus.
- Use hearing protection. Over time, exposure to loud sounds can damage the nerves in the ears, causing hearing loss and tinnitus. Try to limit your exposure to loud sounds. And if you cannot avoid loud sounds, use ear protection to help protect your hearing. If you use chain saws, are a musician, work in an industry that uses loud machinery or use firearms (especially pistols or shotguns), always wear over-the-ear hearing protection.
- Turn down the volume. Long-term exposure to amplified music with no ear protection or listening to music at very high volume through headphones can cause hearing loss and tinnitus.
- Take care of your cardiovascular health. Regular exercise, eating right and taking other steps to keep your blood vessels healthy can help prevent tinnitus linked to obesity and blood vessel disorders.
- Limit alcohol, caffeine and nicotine. These substances, especially when used in excess, can affect blood flow and contribute to tinnitus.
Tinnitus symptoms
Tinnitus is most often described as “ringing in the ears”, even though no external sound is present. However, tinnitus can also cause other types of phantom noises in your ears, including:
- Buzzing
- Roaring
- Clicking
- Hissing
- Humming
- Whooshing
- Music or singing
- Throbbing
You may hear these sounds in 1 or both ears, or in your head. They may come and go, or you might hear them all the time.
Most people who have tinnitus have subjective tinnitus, or tinnitus that only you can hear. The noises of tinnitus may vary in pitch from a low roar to a high squeal, and you may hear it in one or both ears. In some cases, the sound can be so loud it interferes with your ability to concentrate or hear external sound. Tinnitus may be present all the time, or it may come and go.
In rare cases, tinnitus can occur as a rhythmic pulsing or whooshing sound, often in time with your heartbeat. This is called pulsatile tinnitus. If you have pulsatile tinnitus, your doctor may be able to hear your tinnitus when he or she does an examination (objective tinnitus).
Tinnitus may result in insomnia, cognitive effects, anxiety, psychological distress and poorer quality of life 3. The reasons for the drop in quality of life cited in this series were a lack of control over tinnitus, frustration and stress. Interestingly, middle-aged patients aged 40–50 years are most bothered by their tinnitus 79. It is believed that although tinnitus is more common in older patients, having competing health issues reduces the relative burden of tinnitus on their quality of life.
Tinnitus carries economic consequences as well. It can reduce productivity and, together with hearing loss, result in significant disability and loss of income 80.
Tinnitus complications
Tinnitus affects people differently. For some people, tinnitus can significantly affect quality of life. If you have tinnitus, you may also experience:
- Fatigue
- Stress
- Sleep problems
- Trouble concentrating
- Memory problems
- Depression
- Anxiety and irritability
- Headaches
- Problems with work and family life
Treating these linked conditions may not affect tinnitus directly, but it can help you feel better.
Tinnitus diagnosis
When a patient presents with tinnitus, the most critical step is to obtain a thorough medical history. One of the most important distinctions to make is if the tinnitus is pulsatile or non-pulsatile. The next step is to determine if the tinnitus is unilateral (one ear) or bilateral (both ears). This distinction will help with directing your questioning and eventually guide your workup. Both pulsatile and non-pulsatile tinnitus can be unilateral or bilateral. Other important questions include the onset of symptoms, aggravating or alleviating factors, duration, and change in symptom quality or severity 79.
Do your best to describe for your doctor what kind of tinnitus noises you hear. The sounds you hear can help your doctor identify a possible underlying cause.
- Clicking. This type of sound suggests that muscle contractions in and around your ear might be the cause of your tinnitus.
- Pulsing, rushing or humming. These sounds usually stem from blood vessel (vascular) causes, such as high blood pressure, and you may notice them when you exercise or change positions, such as when you lie down or stand up.
- Low-pitched ringing. This type of sound may point to ear canal blockages, Meniere’s disease or stiff inner ear bones (otosclerosis).
- High-pitched ringing. This is the most commonly heard tinnitus sound. Likely causes include loud noise exposure, hearing loss or medications. Acoustic neuroma can cause continuous, high-pitched ringing in one ear.
Common tests include:
- Hearing (audiological) exam. During the test, you’ll sit in a soundproof room wearing earphones that transmit specific sounds into one ear at a time. You’ll indicate when you can hear the sound, and your results will be compared with results considered normal for your age. This can help rule out or identify possible causes of tinnitus.
- Movement. Your doctor may ask you to move your eyes, clench your jaw, or move your neck, arms and legs. If your tinnitus changes or worsens, it may help identify an underlying disorder that needs treatment.
- Imaging tests. Depending on the suspected cause of your tinnitus, you may need imaging tests such as CT or MRI scans.
- Lab tests. Your doctor may draw blood to check for anemia, thyroid problems, heart disease or vitamin deficiencies.
Palpation can also help to evaluate if compression changes the patient’s symptoms, which may help differentiate venous vs. arterial etiologies. If compression of arterial structures decreases symptoms, it suggests an arterial cause. Compression of ipsilateral venous structures may decrease symptoms in venous etiologies such as a high-riding jugular bulb, while compression of the contralateral side may increase symptoms. Rotation of the head to the ipsilateral side of the tinnitus may also decrease symptoms in patients with pulsatile tinnitus due to venous pathology. Similarly, the Valsalva maneuver may reduce symptoms with a venous cause 14.
Tinnitus treatment
Treatment for tinnitus depends on whether your tinnitus is caused by an underlying health condition. If so, your doctor may be able to reduce your symptoms by treating the underlying cause. Examples include:
- Earwax removal. Removing an earwax blockage can decrease tinnitus symptoms.
- Treating a blood vessel condition. Underlying blood vessel conditions may require medication, surgery or another treatment to address the problem.
- Hearing aids. If your tinnitus is caused by noise-induced or age-related hearing loss, using hearing aids may help improve your symptoms. Hearing aids have been used as tinnitus management tools since at least the late 1940s 81 and this continued with the arrival of fully digital aids in the mid 1990s.
- Cochlear implants. Cochlear implants are surgical acoustic-electrical transducers that comprise a digital signal processor similar to a hearing aid and a multiple electrode array that is inserted into the cochlear 82. Cochlear implant provides direct stimulation of the auditory nerve through the tonotopic electrode array when hearing aid amplification would be insufficient to improve hearing. Cochlear implants replace the role of hearing aids when hearing loss is severe 82. Cochlear implants provide electrical stimulation based on sound patterns, but can be considered a sound therapy device because they activate auditory pathways. Interest in cochlear implants for tinnitus therapy began in the 1980s 83, but early experience with implantation for tinnitus showed limited success 84. Cochlear implants are becoming more common therapy options when tinnitus accompanies a severe unilateral hearing loss 85.
- Changing your medication. If a medication you’re taking appears to be the cause of tinnitus, your doctor may recommend stopping or reducing the drug, or switching to a different medication.
Hearing aids for tinnitus
Good-quality, properly fitted hearing aids reduce and can even eliminate most tinnitus associated with hearing loss. Hearing aids reduce the strain of listening and distract you from the tinnitus by bringing you more sound from the environment around you. Some hearing aids come with built-in soothing or masking sounds.
Many people get used to the sounds — they are said to ‘habituate’ so their brain doesn’t notice the tinnitus any more.
Some audiologists run specialist tinnitus clinics to help patients manage their tinnitus and they fit hearing aids and/or therapeutic noise generators if needed.
Noise suppression
Many times, tinnitus can’t be cured. But there are treatments that can help make your symptoms less noticeable. Your doctor may suggest using an electronic device to suppress the noise. Devices include:
- White noise machines. These devices, which produce a sound similar to static, or environmental sounds such as falling rain or ocean waves, are often an effective treatment for tinnitus. You may want to try a white noise machine with pillow speakers to help you sleep. Fans, humidifiers, dehumidifiers and air conditioners in the bedroom also produce white noise and may help make tinnitus less noticeable at night.
- Masking devices. Worn in the ear and similar to hearing aids, these devices produce a continuous, low-level white noise that suppresses tinnitus symptoms. There are various forms of masking. Essentially these masking sounds take the attention away from the internal tinnitus sound and replace it with relaxing sounds.
- Introduction of the same sound
- Introduction of an altered sound
- Music with the tinnitus sound removed
- White noise or pleasant sounds
Counseling
Behavioral treatment options aim to help you live with tinnitus by helping you change the way you think and feel about your symptoms. Over time, your tinnitus may bother you less. Counseling options include:
Tinnitus retraining therapy
Tinnitus retraining therapy (TRT) involves “retraining” the brain to become accustomed to the tinnitus sound and thereby encourage the patient to experience the tinnitus as a neutral stimulus 86. Tinnitus retraining therapy (TRT) has two main components 86:
- An educational counseling approach and
- Sound therapy in the form of masking or white noise, with the sound intensity of the device set slightly below that of the tinnitus perceived by the patient .
Tinnitus retraining therapy (TRT) is an individualized program that is usually administered by an audiologist or at a tinnitus treatment center. Tinnitus retraining therapy (TRT) combines sound masking and counseling from a trained professional. Typically, you wear a device in your ear that helps mask your tinnitus symptoms while you also receive directive counseling. Over time, TRT may help you notice tinnitus less and feel less distressed by your symptoms.
Sound therapy
Sound therapy is a tinnitus retraining therapy (TRT) that involves applying external sound to suppress the perception of tinnitus or the reaction to tinnitus for clinical benefit 1. The intensity of the external sound can be increased to the point where it does not interfere with the environment sounds that a patient needs to hear 87. Sound therapy can be applied using sound (noise) generators, hearing aids, or a combination of a hearing aid and a noise generator 88. The sound generators produce a broadband sound that can reduce (partial masking) or even eliminate (complete masking) the perception of tinnitus 10). Patients undergoing masking are also advised to use various sound sources for the masking, such as a CD player, radio, or tabletop sound generator 89. Sound therapy should be combined with some form of counseling, even if this simply involves providing information 90. A systemic review found that the efficacy of sound therapy against tinnitus was inconclusive, and currently, there is still no reliable evidence for the efficacy of sound-therapy devices 91.
Cognitive-behavioral therapy
Cognitive-behavioral therapy (CBT) is a relatively brief psychological treatment modality directed at identifying and modifying maladaptive behaviors and thoughts through behavioral changes and cognitive restructuring 92. Cognitive-behavioral therapy teaches skills to identify the negative thoughts that result in distress and restructure them such that the thoughts are more accurate or helpful 1. A licensed mental health professional or psychologist can help you learn coping techniques to make tinnitus symptoms less bothersome. Counseling can also help with other problems often linked to tinnitus, including anxiety and depression. Many mental health professionals offer CBT for tinnitus in individual or group sessions, and CBT programs are also available online e.g., digital CBT. Digital CBT is a form of CBT delivered using digital technology, such as a computer, tablet or phone. Common components of digital tinnitus-related CBT are similar to those used in face-to-face CBT (for example, positive imagery and learning to identify and challenge unhelpful thoughts). People using digital CBT are more likely to have less direct contact with healthcare professionals during the intervention compared with face-to-face interventions. Although cognitive-behavioral therapy does not reduce the subjectively reported loudness of tinnitus, it improves the well-being of affected patients 1.
Medications
Although no medicines have been approved to date by the FDA, several classes of medication are often used to treat patients with tinnitus (Table 2). Drugs can’t cure tinnitus, but in some cases they may help reduce the severity of symptoms or complications. The official guidelines stress that no medication cures tinnitus. Current tinnitus guidelines recommend against the routine use of antidepressant, anticonvulsant, or anxiolytic medication for bothersome tinnitus 1. However, for patients with pre-existing anxiety and depression, doctors may prescribe medication to help treat the anxiety and depression that often accompany tinnitus 29, 36. The use of tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitors (SSRIs) has been shown to be effective in managing tinnitus symptoms, decreasing the level of annoyance 93.
Moreover, various combinations of magnesium, alpha-lipoic acid, N-acetyl cysteine, and others have been tested for protection of hearing from noise. When these are effective, it is difficult to differentiate from the placebo effect or from the impact of having a program where the patient feels they are in charge bringing the brain into the healing process.
Table 2. Off-label drugs used in the treatment of tinnitus
| Anesthetics | Antihistamines |
| Flecainide acetate | Chlorpheniramine |
| Lidocaine/lignocaine | Dexchlorpheniramine |
| Mexiletine—oral lidocaine analog | Meclizine |
| Procaine | Terfenadine |
| Tocaine—oral lidocaine analog | Calcium Channel Blockers |
| Antiarrhythmics | Flunarizine |
| Flecainide | Nifedipine |
| Lidocaine | Nimodipine |
| Mexiletine | Diuretics |
| Tocainide | Chlorothiazide |
| Antianxiety | Furosemide |
| Benzodiazepines | Glutamate receptor antagonists |
| Alprazolam | Acamprosate |
| Amylobarbitone | Caroverine |
| Clonazepam | Memantine |
| Diazepam | Muscle relaxants |
| Flurazepam | Baclofen |
| Oxazepam | Cyclobenzaprine |
| Protriptyline | Eperisone hydrochloride |
| Anticonvulsants | Others |
| Amino-oxyacetic acid | Aniracetam |
| Carbamazepine | Arlidin |
| Gabapentin | Atorvastatin |
| Lamotrigine | Clonidine |
| Phenytoin | Cyclandelate |
| Pregabalin | Glutamic acid diethylester |
| Primidone | Herbal products |
| Valproic acid | Melatonin |
| Antidepressants | Minerals |
| Amitriptyline | Naltrexone |
| Bupropion | Nicotinamide |
| Fluoxetine | Oxpentifylline/pentoxifylline |
| Nortriptyline | Cinnarizine |
| Paroxetine | Sulpiride |
| Sertraline | Vardenafil |
| Trimipramine | Vitamin |
Footnotes: These medicines can be classified by their sites of action, including those that directly or indirectly control responses within the cochlea; those that affect responses of the nervous system; those simultaneously acting on both the cochlea and nervous system; and others.
[Source 94 ]Lifestyle and home remedies
Often, tinnitus can’t be treated. Some people, however, get used to it and notice it less than they did at first. For many people, certain adjustments make the symptoms less bothersome. These tips may help:
- Use hearing protection. Over time, exposure to loud sounds can damage the nerves in the ears, causing hearing loss and tinnitus. To keep your tinnitus from getting worse, take steps to protect your hearing. Wear ear plugs or over-the-ear hearing protection if you are using noise-generating equipment (such as a lawn mower, chain saws), work in an industry that uses loud machinery or use firearms (especially pistols or shotguns) or in a loud environment, such as a rock concert.
- Turn down the volume. Listening to music at very high volume through headphones can contribute to hearing loss and tinnitus.
- Use white noise. If tinnitus is especially noticeable in quiet settings, try using a white noise machine to mask the noise from tinnitus. If you don’t have a white noise machine, a fan, soft music or low-volume radio static also may help.
- Relax and avoid stress, as this will make tinnitus worse.
- Limit alcohol, caffeine and nicotine. These substances, especially when used in excess, can affect blood flow and contribute to tinnitus.
- Sleep improvement. Tinnitus can affect normal sleep and therapy should be directed to better sleep hygiene.
Coping and support
In addition to any treatment options offered by your doctor, here are some suggestions to help you cope with tinnitus:
- Support groups. Sharing your experience with others who have tinnitus may be helpful. There are tinnitus groups that meet in person, as well as internet forums. To ensure that the information you get in the group is accurate, it’s best to choose a group facilitated by a physician, audiologist or other qualified health professional.
- Education. Learning as much as you can about tinnitus and ways to alleviate symptoms can help. And just understanding tinnitus better makes it less bothersome for some people.
- Stress management. Stress can make tinnitus worse. Stress management, whether through relaxation therapy, biofeedback or exercise, may provide some relief.
Alternative medicine
There’s little evidence that alternative medicine treatments work for tinnitus 1. However, some alternative therapies that have been tried for tinnitus include:
- Acupuncture. Acupuncture may or may not be help your tinnitus; there are not enough quality studies of this type of treatment to make a recommendation.
- Ginkgo biloba. Ginkgo biloba extract has a mechanism of action associated with neurotransmitters involved in blood circulation, metabolism, blood viscosity, and aging. Ginkgo biloba extract increases the permeability of capillaries and venous blood pressure and enhances ATP and blood glucose concentrations following metabolic damage to cerebral metabolism. In addition, ginkgo biloba extract reduces platelet agglutination and affects the acetocholinergic system by acting as a neurotransmitter. Treatment usually consists of administration of about 100 mg/kg per day for about 3 weeks. Some studies have suggested that ginkgo biloba extract affects nucleus-derived and peripheral tinnitus, whereas others do not 95. Although a number of reports have indicated that ginkgo biloba may be effective in the management of tinnitus, the benefits of this agent remain unclear 96.
- Vitamins. Vitamin B12 deficiency is associated with axonal degeneration, demyelination, and subsequent apoptotic neuronal death, and may cause the demyelination of neurons in the cochlear nerve, resulting in hearing loss. In addition, low levels of vitamin B12 and folate are associated with the destruction of the microvasculature of the stria vascularis, which might result in decreased endocochlear potential and in hearing loss and tinnitus. A pilot study reported a high prevalence of vitamin B12 deficiency in a North Indian population and improvements in tinnitus severity scores and VAS in cobalamin-deficient patients receiving intramuscular vitamin B12 weekly for 6 weeks 97. In contrast, vitamin B12 replacement treatment was not effective in 100 patients with non-pulsatile tinnitus and vitamin B12 deficiency 98. Nicotinic acid is a water-soluble vitamin found in meats, milk, eggs, and other foods. It is necessary to maintain skin, nerves, and digestive function, and its deficiency may result in pellagra. Nicotinic acid is used to control tinnitus, as it enhances blood flow in the labyrinth. For example, 50% of patients with tinnitus were reported to benefit from nicotinic acid administration 99. In a double-blind, controlled trial performed in 48 patients, the value of the related drug nicotinamide was assessed and compared with the effect of a placebo. The results obtained with nicotinamide were not better than those observed for placebo 100. Its side-effects included gastric ulcers, hypotension, headache, and hepatic failure.
- Melatonin. Melatonin controls circadian rhythms through a combination of circadian hormones that occur naturally with melatonin receptors. As a strong oxidizing agent, melatonin has been shown to prevent noise- and medicine-induced tinnitus by protecting mitochondrial and nuclear DNA. Prospective clinical trials of the treatment of tinnitus patients with 3.0 mg/day melatonin found that melatonin was associated with a statistically significant decrease in tinnitus intensity and improved sleep quality in patients with chronic tinnitus 101.
- Zinc supplements. Many cellular metabolic processes require zinc, with this metal ion playing important roles in growth and development, immune responses, neurological functions, and reproduction. Zinc has been found to catalyze chemical responses necessary for maintaining life, to be involved in the structure of proteins and cell membranes, and to regulate gene expression by acting as a transcription factor. Zinc concentrations are higher in the cochlea and vestibular sites than in other parts of the body, suggesting that zinc may be effective in treating tinnitus. Zinc deficiency is reported to induce senile hearing loss, whereas administration of zinc improved hearing loss and tinnitus in one-third of elderly patients with low zinc concentrations. Zinc deficiency is associated with tinnitus and sensorineural hearing loss, as well as with nail fragility, depilation, taste disorders, olfactory disturbances, nyctalopia, and prostate diseases. The blood concentration of zinc is inversely proportional to the concentration of copper. Good outcomes have been reported in patients with tinnitus treated with 150 mg/day zinc and 600 mg/day zinc sulfate, amounts ten times higher than required by normal adults. Serum zinc concentrations differed significantly between control subjects and patients with tinnitus, with the latter showing improvement following oral administration of 34 to 68 mg/day zinc for 2 weeks. Zinc, however, was ineffective in tinnitus patients with normal zinc concentrations 102.
Surgical management
Surgical management is very rarely used in patients with tinnitus, and is only used for treatable underlying causes 103. These can include the surgical resection of acoustic neuroma or other brainstem or cerebellopontine angle tumours and lesions, endolymphatic sac shunting for Ménière disease, or stapedectomy for otosclerosis. Tensor tympani and stapedius myoclonus syndromes are also correctable with surgery by sectioning the affected muscles 104.
Potential future treatments
Researchers are investigating whether magnetic or electrical stimulation of the brain can help relieve symptoms of tinnitus. Examples include transcranial magnetic stimulation (TMS) and deep brain stimulation. Recently beneficial results have been reported using deep brain stimulation. The current model of tinnitus centers on the overstimulation of the subcortical auditory pathway, and it has been suggested that low-frequency electromagnetic pulses from transcranial magnetic stimulation help reduce the neural activity in the directly stimulated and structurally connected regions of the patient’s brain 105.
- Electrical or magnetic stimulation of brain areas involved in hearing. Implantable devices already exist to reduce the trembling of Parkinson’s disease and the anxieties of obsessive-compulsive disorder. Similar devices could be developed to normalize the neural circuits involved in tinnitus.
- Repetitive transcranial magnetic stimulation (rTMS). This technique, which uses a small device placed on the scalp to generate short magnetic pulses, is already being used to normalize electrical activity in the brains of people with epilepsy. Preliminary trials of repetitive transcranial magnetic stimulation (rTMS) in humans, are helping researchers pinpoint the best places in the brain to stimulate in order to suppress tinnitus 106, 107. Researchers are also looking for ways to identify which people are most likely to respond well to stimulation devices. A recent Cochrane review identified 5 randomized control trials of rTMS for tinnitus, totaling 233 patients concluded that there was limited support for the use of rTMS to treat tinnitus but also noted that 5 additional trials were ongoing at the time of their review 108. Peng et al 109 performed a systematic review of randomized control trials of rTMS that included 5 trials, 3 of which were included in the aforementioned Cochrane review and 2 were not. Long-term benefits of rTMS for treatment of tinnitus were not demonstrated.
- Hyperactivity and deep brain stimulation. Researchers have observed hyperactivity in neural networks after exposing the ear to intense noise. Understanding specifically where in the brain this hyperactivity begins and how it spreads to other areas could lead to treatments that use deep brain stimulation to calm the neural networks and reduce tinnitus.
- Resetting the tonotopic map. Researchers are exploring how to take advantage of the tonotopic map, which organizes neurons in the auditory cortex according to the frequency of the sound to which they respond. Previous research has shown a change in the organization of the tonotopic map after exposing the ear to intense noise. By understanding how these changes happen, researchers could develop techniques to bring the map back to normal and relieve tinnitus.
Tinnitus prognosis
The incidence of tinnitus has been reported in 2 large cohort studies. In 1 study of 3753 adults, there was an 8.2% baseline prevalence of tinnitus, with a new incidence of 5.7% after 5 years, rising to a 12.7% cumulative incidence at the 10-year follow-up 110. Another study of 1292 adults found that the incidence of new tinnitus after 5 years was 18.0% 111. Risk factors were not consistent among studies but included male sex, history of arthritis or head injury, preexisting hearing loss, and any history of tobacco use.
Tinnitus may improve spontaneously. In 1 cohort study, nearly 50% of patients with significant tinnitus (moderate severity, sleep problems, or both) improved after 5 years, with 43% of those improved reporting complete resolution and the remaining 57% reporting only mild symptoms 112. In another study 113, 82% of patients who reported tinnitus at baseline had persistent tinnitus after 5 years, suggesting close to a 20% rate of spontaneous improvement. Similarly, subjects assigned to the “wait-list” control groups of some clinical trials show small, but significant, improvements in tinnitus distress 114. The largest spontaneous improvement is seen with short duration tinnitus, younger age, and longer intervals between pre- and post-assessment. For example, in 1 study, 28% of subjects with acute tinnitus (lasting < 6 months) improved spontaneously in a control group that received only educational information 115.
The severity of tinnitus can fluctuate. Hallam et al 116 reviewed the psychological aspects of tinnitus and described a natural habituation process that improves tinnitus tolerance. An observational study of 528 patients seen in otolaryngology clinics found that, regardless of symptom duration, tinnitus severity declined over time in 3% to 7% of patients 117. Another large cohort study found that 55% of patients with severe tinnitus reported only moderate, or mildly bothersome, symptoms 5 years later 113. Conversely, 45% of tinnitus patients in the same cohort progressed from mildly annoying symptoms at baseline to moderate or severely annoying symptoms after 5 years. Those with persistent tinnitus, defined in the study as having had symptoms at baseline and at 5 years, were significantly more likely to report moderately or extremely bothersome symptoms compared to their counterparts with newly reported tinnitus.
Living with tinnitus
For many people with tinnitus, the condition is just a mild distraction. But for some, tinnitus causes distress and negatively affects their quality of life. It can cause anxiety, depression, sleep disturbances, and poor concentration. To lessen the impact of tinnitus on your life, try the following:
- Avoid exposure to loud sounds and noises.
- Get your blood pressure checked; if it’s high, get your doctor’s help to control it.
- Exercise daily to improve your circulation.
- Get adequate rest and avoid fatigue.
- Take the focus off your tinnitus. Use techniques such as sound generators and counseling to push it to the background. Remember that the more you think about tinnitus, the more bothersome it will become.
- Use background music/noise or a sound machine to help dampen or eliminate the tinnitus.
- Use mental techniques to push the perception of tinnitus to the background; the more you think about the tinnitus, the louder it will seem.
- Take steps to reduce stress.
- Reduce or eliminate your caffeine consumption.
- Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham ER Jr, Archer SM, Blakley BW, Carter JM, Granieri EC, Henry JA, Hollingsworth D, Khan FA, Mitchell S, Monfared A, Newman CW, Omole FS, Phillips CD, Robinson SK, Taw MB, Tyler RS, Waguespack R, Whamond EJ. Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg. 2014 Oct;151(2 Suppl):S1-S40. https://doi.org/10.1177/0194599814545325
- Searchfield GD, Zhang J, Biswas R, De Ridder D, Deutsch B, Hall DA, Hébert S, Kleinjung T, Kleinstäuber M, Langguth B, Lopez-Escamez JA, Maslin MRD, Mazurek B, Piccirillo JF, Salvi R, Schlee W, Shulman A, Shore S, Szczepek AJ, Smith PF, Theodoroff SM, Vajsakovic D, Weise C, Zheng Y. Emerging Topics in the Behavioral Neuroscience of Tinnitus. Curr Top Behav Neurosci. 2021;51:461-483. doi: 10.1007/7854_2020_217
- Chan, H., Low, D., Yuen, H. W., & How, C. H. (2020). Tinnitus – ringing in the ears. Singapore medical journal, 61(9), 448–452. https://doi.org/10.11622/smedj.2020128
- Searchfield, G. D., Sanders, P. J., Doborjeh, Z., Doborjeh, M., Boldu, R., Sun, K., & Barde, A. (2021). A State-of-Art Review of Digital Technologies for the Next Generation of Tinnitus Therapeutics. Frontiers in digital health, 3, 724370. https://doi.org/10.3389/fdgth.2021.724370
- Kleinstäuber M, Weise C. Psychosocial Variables That Predict Chronic and Disabling Tinnitus: A Systematic Review. Curr Top Behav Neurosci. 2021;51:361-380. doi: 10.1007/7854_2020_213
- Searchfield GD, Morrison-Low J, Wise K. Object identification and attention training for treating tinnitus. Prog Brain Res. 2007;166:441-60. doi: 10.1016/S0079-6123(07)66043-9
- Cima RFF, Mazurek B, Haider H, Kikidis D, Lapira A, Noreña A, Hoare DJ. A multidisciplinary European guideline for tinnitus: diagnostics, assessment, and treatment. HNO. 2019 Mar;67(Suppl 1):10-42. English. doi: 10.1007/s00106-019-0633-7
- Tinnitus: Diagnosis and Management. Am Fam Physician. 2021 Jun 1;103(11):663-671. https://www.aafp.org/afp/2021/0601/p663.html
- Luxon L. M. (1993). Tinnitus: its causes, diagnosis, and treatment. BMJ (Clinical research ed.), 306(6891), 1490–1491. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1677927/pdf/bmj00023-0008.pdf
- Henry JA, Dennis KC, Schechter MA. General review of tinnitus: prevalence, mechanisms, effects, and management. J Speech Lang Hear Res. 2005 Oct;48(5):1204-35. https://doi.org/10.1044/1092-4388(2005/084
- Jastreboff PJ, Hazell JWP. Tinnitus retraining therapy (TRT): clinical implementation of the model. In: Jastreboff PJ, Hazell JWP, editors. Tinnitus retraining therapy: implementing the neurophysiological model. New York, NY: Cambridge University Press; 2004. pp. 64–144.
- Dobie RA. Overview: suffering from tinnitus. In: Snow JB, editor. Tinnitus: theory and management. Lewiston, NY: BC Decker; 2004. pp. 1–7.
- Eggermont, J. J., & Roberts, L. E. (2015). Tinnitus: animal models and findings in humans. Cell and tissue research, 361(1), 311–336. https://doi.org/10.1007/s00441-014-1992-8
- Hofmann, E., Behr, R., Neumann-Haefelin, T., & Schwager, K. (2013). Pulsatile tinnitus: imaging and differential diagnosis. Deutsches Arzteblatt international, 110(26), 451–458. https://doi.org/10.3238/arztebl.2013.0451
- Pegge, S., Steens, S., Kunst, H., & Meijer, F. (2017). Pulsatile Tinnitus: Differential Diagnosis and Radiological Work-Up. Current radiology reports, 5(1), 5. https://doi.org/10.1007/s40134-017-0199-7
- Han, B. I., Lee, H. W., Ryu, S., & Kim, J. S. (2021). Tinnitus Update. Journal of clinical neurology (Seoul, Korea), 17(1), 1–10. https://doi.org/10.3988/jcn.2021.17.1.1
- Rauschecker, J. P., Leaver, A. M., & Mühlau, M. (2010). Tuning out the noise: limbic-auditory interactions in tinnitus. Neuron, 66(6), 819–826. https://doi.org/10.1016/j.neuron.2010.04.032
- Elgoyhen AB, Langguth B. Pharmacological approaches to the treatment of tinnitus. Drug Discov Today. 2010 Apr;15(7-8):300-5. doi: 10.1016/j.drudis.2009.11.003
- Sanchez, T. G., & Rocha, C. B. (2011). Diagnosis and management of somatosensory tinnitus: review article. Clinics (Sao Paulo, Brazil), 66(6), 1089–1094. https://doi.org/10.1590/s1807-59322011000600028
- Levine RA. Somatic (craniocervical) tinnitus and the dorsal cochlear nucleus hypothesis. Am J Otolaryngol. 1999 Nov-Dec;20(6):351-62. doi: 10.1016/s0196-0709(99)90074-1
- Yoneoka Y, Fujii Y, Nakada T. Central tinnitus: a case report. Ear Nose Throat J. 2001 Dec;80(12):864-6.
- Hurst RW, Lee SI. Ictal tinnitus. Epilepsia. 1986 Nov-Dec;27(6):769-72. doi: 10.1111/j.1528-1157.1986.tb03608.x
- Knipper M, Zimmermann U, Müller M. Molecular aspects of tinnitus. Hear Res. 2010 Jul;266(1-2):60-9. doi: 10.1016/j.heares.2009.07.013
- Henry, J. A., Roberts, L. E., Caspary, D. M., Theodoroff, S. M., & Salvi, R. J. (2014). Underlying mechanisms of tinnitus: review and clinical implications. Journal of the American Academy of Audiology, 25(1), 5–126. https://doi.org/10.3766/jaaa.25.1.2
- Chari DA, Limb CJ. Tinnitus. Med Clin North Am. 2018 Nov;102(6):1081-1093. doi: 10.1016/j.mcna.2018.06.014
- Folmer RL, Martin WH, Shi Y. Tinnitus: questions to reveal the cause, answers to provide relief. J Fam Pract. 2004;53(7):532–540.
- Sismanis A. Pulsatile tinnitus. Otolaryngol Clin North Am. 2003;36(2):389–402, viii.
- Ahmad N, Seidman M. Tinnitus in the older adult: epidemiology, pathophysiology and treatment options. Drugs Aging. 2004;21(5):297-305. doi: 10.2165/00002512-200421050-00002
- Wu, V., Cooke, B., Eitutis, S., Simpson, M., & Beyea, J. A. (2018). Approach to tinnitus management. Canadian family physician Medecin de famille canadien, 64(7), 491–495. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6042678
- Diagnostic Approach to Tinnitus. Am Fam Physician. 2004 Jan 1;69(1):120-126. https://www.aafp.org/afp/2004/0101/p120.html
- Wall M. (2010). Idiopathic intracranial hypertension. Neurologic clinics, 28(3), 593–617. https://doi.org/10.1016/j.ncl.2010.03.003
- Bae, S. C., Kim, D. K., Yeo, S. W., Park, S. Y., & Park, S. N. (2015). Single-center 10-year experience in treating patients with vascular tinnitus: diagnostic approaches and treatment outcomes. Clinical and experimental otorhinolaryngology, 8(1), 7–12. https://doi.org/10.3342/ceo.2015.8.1.7
- Fujii N, Inui Y, Katada K. Temporal bone anatomy: correlation of multiplanar reconstruction sections and three-dimensional computed tomography images. Jpn J Radiol. 2010 Nov;28(9):637-48. doi: 10.1007/s11604-010-0479-0
- Han, B. I., Lee, H. W., Kim, T. Y., Lim, J. S., & Shin, K. S. (2009). Tinnitus: characteristics, causes, mechanisms, and treatments. Journal of clinical neurology (Seoul, Korea), 5(1), 11–19. https://doi.org/10.3988/jcn.2009.5.1.11
- Wallhäusser-Franke, E., D’Amelio, R., Glauner, A., Delb, W., Servais, J. J., Hörmann, K., & Repik, I. (2017). Transition from Acute to Chronic Tinnitus: Predictors for the Development of Chronic Distressing Tinnitus. Frontiers in neurology, 8, 605. https://doi.org/10.3389/fneur.2017.00605
- Bauer CA. Tinnitus. N Engl J Med. 2018 Mar 29;378(13):1224-1231. doi: 10.1056/NEJMcp1506631
- Mattox DE, Hudgins P. Algorithm for evaluation of pulsatile tinnitus. Acta Otolaryngol. 2008 Apr;128(4):427-31. doi: 10.1080/00016480701840106
- Sismanis A. Pulsatile tinnitus: contemporary assessment and management. Curr Opin Otolaryngol Head Neck Surg. 2011 Oct;19(5):348-57. doi: 10.1097/MOO.0b013e3283493fd8
- Yardley MP, Knight LC. Extra cranial arteriovenous malformations presenting as pulsatile tinnitus. Br J Clin Pract. 1992 Spring;46(1):71-2.
- Lenkeit CP, Al Khalili Y. Pulsatile Tinnitus. [Updated 2022 Jan 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553153
- Yeo WX, Xu SH, Tan TY, Low YM, Yuen HW. Surgical management of pulsatile tinnitus secondary to jugular bulb or sigmoid sinus diverticulum with review of literature. Am J Otolaryngol. 2018 Mar-Apr;39(2):247-252. doi: 10.1016/j.amjoto.2017.12.019
- Sismanis A. Pulsatile tinnitus. A 15-year experience. Am J Otol. 1998 Jul;19(4):472-7.
- Villaça Avoglio JL. Dental occlusion as one cause of tinnitus. Med Hypotheses. 2019 Sep;130:109280. doi: 10.1016/j.mehy.2019.109280
- Keidar E, De Jong R, Kwartowitz G. Tensor Tympani Syndrome. [Updated 2022 Jan 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519055
- Esmaili AA, Renton J. A review of tinnitus. Aust J Gen Pract. 2018 Apr;47(4):205-208. doi: 10.31128/AJGP-12-17-4420
- Nicholson P, Brinjikji W, Radovanovic I, Hilditch CA, Tsang ACO, Krings T, Mendes Pereira V, Lenck S. Venous sinus stenting for idiopathic intracranial hypertension: a systematic review and meta-analysis. J Neurointerv Surg. 2019 Apr;11(4):380-385. doi: 10.1136/neurintsurg-2018-014172
- Langguth B. Treatment of tinnitus. Curr Opin Otolaryngol Head Neck Surg. 2015 Oct;23(5):361-8. doi: 10.1097/MOO.0000000000000185
- Nicolas-Puel C, Akbaraly T, Lloyd R, Berr C, Uziel A, Rebillard G, Puel JL. Characteristics of tinnitus in a population of 555 patients: specificities of tinnitus induced by noise trauma. Int Tinnitus J. 2006;12(1):64-70.
- Tan, C. M., Lecluyse, W., McFerran, D., & Meddis, R. (2013). Tinnitus and patterns of hearing loss. Journal of the Association for Research in Otolaryngology : JARO, 14(2), 275–282. https://doi.org/10.1007/s10162-013-0371-6
- Wu, C., Stefanescu, R. A., Martel, D. T., & Shore, S. E. (2016). Tinnitus: Maladaptive auditory-somatosensory plasticity. Hearing research, 334, 20–29. https://doi.org/10.1016/j.heares.2015.06.005
- Shore, S. E., Roberts, L. E., & Langguth, B. (2016). Maladaptive plasticity in tinnitus–triggers, mechanisms and treatment. Nature reviews. Neurology, 12(3), 150–160. https://doi.org/10.1038/nrneurol.2016.12
- Salvi RJ, Wang J, Ding D. Auditory plasticity and hyperactivity following cochlear damage. Hear Res. 2000 Sep;147(1-2):261-74. doi: 10.1016/s0378-5955(00)00136-2
- Portnuff C. D. (2016). Reducing the risk of music-induced hearing loss from overuse of portable listening devices: understanding the problems and establishing strategies for improving awareness in adolescents. Adolescent health, medicine and therapeutics, 7, 27–35. https://doi.org/10.2147/AHMT.S74103
- Agrawal Y, Platz EA, Niparko JK. Risk factors for hearing loss in US adults: data from the National Health and Nutrition Examination Survey, 1999 to 2002. Otol Neurotol. 2009 Feb;30(2):139-45. doi: 10.1097/MAO.0b013e318192483c
- Le, T. N., Straatman, L. V., Lea, J., & Westerberg, B. (2017). Current insights in noise-induced hearing loss: a literature review of the underlying mechanism, pathophysiology, asymmetry, and management options. Journal of otolaryngology – head & neck surgery = Le Journal d’oto-rhino-laryngologie et de chirurgie cervico-faciale, 46(1), 41. https://doi.org/10.1186/s40463-017-0219-x
- Portnuff CD, Fligor BJ, Arehart KH. Teenage use of portable listening devices: a hazard to hearing? J Am Acad Audiol. 2011 Nov-Dec;22(10):663-77. doi: 10.3766/jaaa.22.10.5
- Canadian Centre for Occupational Health and Safety [website]. Noise – occupational exposure limits in Canada. Hamilton, ON: Canadian Centre for Occupational Health and Safety; 2017. https://www.ccohs.ca/oshanswers/phys_agents/exposure_can.html
- Seligmann H, Podoshin L, Ben-David J, Fradis M, Goldsher M. Drug-induced tinnitus and other hearing disorders. Drug Saf. 1996;14(3):198–212.
- Cianfrone G, Pentangelo D, Cianfrone E, et al. Pharmacological drugs inducing ototoxicity, vestibular symptoms and tinnitus: a reasoned and updated guide. Eur Rev Med Pharmacol Sci. 2011;15(6):601–636.
- Goebel JA. 2015 Equilibrium Committee Amendment to the 1995 AAO-HNS Guidelines for the Definition of Ménière’s Disease. Otolaryngol Head Neck Surg. 2016 Mar;154(3):403-4. doi: 10.1177/0194599816628524
- Ren YF, Isberg A. Tinnitus in patients with temporomandibular joint internal derangement. Cranio. 1995 Apr;13(2):75-80. doi: 10.1080/08869634.1995.11678048
- Baguley, D. M., Humphriss, R. L., Axon, P. R., & Moffat, D. A. (2006). The clinical characteristics of tinnitus in patients with vestibular schwannoma. Skull base : official journal of North American Skull Base Society … [et al.], 16(2), 49–58. https://doi.org/10.1055/s-2005-926216
- Ratnayake SA, Jayarajan V, Bartlett J. Could an underlying hearing loss be a significant factor in the handicap caused by tinnitus? Noise Health. 2009 Jul-Sep;11(44):156-60. doi: 10.4103/1463-1741.53362
- Martines, F., Bentivegna, D., Di Piazza, F., Martines, E., Sciacca, V., & Martinciglio, G. (2010). Investigation of tinnitus patients in Italy: clinical and audiological characteristics. International journal of otolaryngology, 2010, 265861. https://doi.org/10.1155/2010/265861
- Jastreboff PJ. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res. 1990 Aug;8(4):221-54. doi: 10.1016/0168-0102(90)90031-9
- Guitton, M. J., Caston, J., Ruel, J., Johnson, R. M., Pujol, R., & Puel, J. L. (2003). Salicylate induces tinnitus through activation of cochlear NMDA receptors. The Journal of neuroscience : the official journal of the Society for Neuroscience, 23(9), 3944–3952. https://doi.org/10.1523/JNEUROSCI.23-09-03944.2003
- Pilati, N., Large, C., Forsythe, I. D., & Hamann, M. (2012). Acoustic over-exposure triggers burst firing in dorsal cochlear nucleus fusiform cells. Hearing research, 283(1-2), 98–106. https://doi.org/10.1016/j.heares.2011.10.008
- Mulders, W. H., Seluakumaran, K., & Robertson, D. (2010). Efferent pathways modulate hyperactivity in inferior colliculus. The Journal of neuroscience : the official journal of the Society for Neuroscience, 30(28), 9578–9587. https://doi.org/10.1523/JNEUROSCI.2289-10.2010
- Moller AR. Similarities between severe tinnitus and chronic pain. J Am Acad Audiol. 2000 Mar;11(3):115-24.
- Eggermont JJ, Roberts LE. The neuroscience of tinnitus. Trends Neurosci. 2004 Nov;27(11):676-82. doi: 10.1016/j.tins.2004.08.010
- Tass PA, Adamchic I, Freund HJ, von Stackelberg T, Hauptmann C. Counteracting tinnitus by acoustic coordinated reset neuromodulation. Restor Neurol Neurosci. 2012;30(2):137-59. doi: 10.3233/RNN-2012-110218
- Engineer, N. D., Riley, J. R., Seale, J. D., Vrana, W. A., Shetake, J. A., Sudanagunta, S. P., Borland, M. S., & Kilgard, M. P. (2011). Reversing pathological neural activity using targeted plasticity. Nature, 470(7332), 101–104. https://doi.org/10.1038/nature09656
- Moore BC, Vinay SN. Enhanced discrimination of low-frequency sounds for subjects with high-frequency dead regions. Brain. 2009 Feb;132(Pt 2):524-36. doi: 10.1093/brain/awn308
- Buss E, Hall JW 3rd, Grose JH, Hatch DR. Perceptual consequences of peripheral hearing loss: do edge effects exist for abrupt cochlear lesions? Hear Res. 1998 Nov;125(1-2):98-108. doi: 10.1016/s0378-5955(98)00131-2
- Noreña AJ. An integrative model of tinnitus based on a central gain controlling neural sensitivity. Neurosci Biobehav Rev. 2011 Apr;35(5):1089-109. doi: 10.1016/j.neubiorev.2010.11.003
- Vanneste, S., & De Ridder, D. (2012). The auditory and non-auditory brain areas involved in tinnitus. An emergent property of multiple parallel overlapping subnetworks. Frontiers in systems neuroscience, 6, 31. https://doi.org/10.3389/fnsys.2012.00031
- Melcher JR, Knudson IM, Levine RA. Subcallosal brain structure: correlation with hearing threshold at supra-clinical frequencies (>8 kHz), but not with tinnitus. Hear Res. 2013 Jan;295:79-86. doi: 10.1016/j.heares.2012.03.013
- König O, Schaette R, Kempter R, Gross M. Course of hearing loss and occurrence of tinnitus. Hear Res. 2006 Nov;221(1-2):59-64. doi: 10.1016/j.heares.2006.07.007
- McCormack A, Edmondson-Jones M, Somerset S, Hall D. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res. 2016 Jul;337:70-9. doi: 10.1016/j.heares.2016.05.009
- Kim K. S. (2010). Occupational hearing loss in Korea. Journal of Korean medical science, 25(Suppl), S62–S69. https://doi.org/10.3346/jkms.2010.25.S.S62
- SALTZMAN M, ERSNER MS. A hearing aid for the relief of tinnitus aurium. Laryngoscope. 1947 May;57(5):358-66. doi: 10.1288/00005537-194705000-00005
- Boisvert, I., Reis, M., Au, A., Cowan, R., & Dowell, R. C. (2020). Cochlear implantation outcomes in adults: A scoping review. PloS one, 15(5), e0232421. https://doi.org/10.1371/journal.pone.0232421
- Brackmann DE. Reduction of tinnitus in cochlear-implant patients. J Laryngol Otol Suppl. 1981;(4):163-5.
- Thedinger B, House WF, Edgerton BJ. Cochlear implant for tinnitus. Case reports. Ann Otol Rhinol Laryngol. 1985 Jan-Feb;94(1 Pt 1):10-3. doi: 10.1177/000348948509400102
- Arts RA, George EL, Stokroos RJ, Vermeire K. Review: cochlear implants as a treatment of tinnitus in single-sided deafness. Curr Opin Otolaryngol Head Neck Surg. 2012 Oct;20(5):398-403. doi: 10.1097/MOO.0b013e3283577b66
- Jastreboff PJ, Hazell JW. A neurophysiological approach to tinnitus: clinical implications. Br J Audiol. 1993 Feb;27(1):7-17. doi: 10.3109/03005369309077884
- Folmer RL, Martin WH, Shi Y, Edlefsen LL. Tinnitus sound therapy. In: Tyler RS, editor. Tinnitus treatment: clinical protocols. New York, NY: Thieme; 2006. pp. 176–186.
- Henry JA, Schechter MA, Nagler SM, Fausti SA. Comparison of tinnitus masking and tinnitus retraining therapy. J Am Acad Audiol. 2002 Nov-Dec;13(10):559-81.
- Henry JA, Schechter MA, Loovis CL, Zaugg TL, Kaelin C, Montero M. Clinical management of tinnitus using a “progressive intervention” approach. J Rehabil Res Dev. 2005 Jul-Aug;42(4 Suppl 2):95-116. doi: 10.1682/jrrd.2005.01.0005
- Tyler RS. Neurophysiological models, psychological models, and treatments for tinnitus. In: Tyler RS, editor. Tinnitus treatment: clinical protocols. New York, NY: Thieme; 2006. pp. 1–22.
- Hobson, J., Chisholm, E., & El Refaie, A. (2012). Sound therapy (masking) in the management of tinnitus in adults. The Cochrane database of systematic reviews, 11(11), CD006371. https://doi.org/10.1002/14651858.CD006371.pub3
- Andersson G, Kaldo V. Cognitive-behavioral therapy with applied relaxation. In: Tyler RS, editor. Tinnitus treatment: clinical protocols. New York, NY: Thieme; 2006. pp. 96–115.
- Fornaro, M., & Martino, M. (2010). Tinnitus psychopharmacology: A comprehensive review of its pathomechanisms and management. Neuropsychiatric disease and treatment, 6, 209–218. https://doi.org/10.2147/ndt.s10361
- Kim, S. H., Kim, D., Lee, J. M., Lee, S. K., Kang, H. J., & Yeo, S. G. (2021). Review of Pharmacotherapy for Tinnitus. Healthcare (Basel, Switzerland), 9(6), 779. https://doi.org/10.3390/healthcare9060779
- Morgenstern C, Biermann E. The efficacy of Ginkgo special extract EGb 761 in patients with tinnitus. Int J Clin Pharmacol Ther. 2002 May;40(5):188-97. doi: 10.5414/cpp40188
- Hilton MP, Zimmermann EF, Hunt WT. Ginkgo biloba for tinnitus. Cochrane Database Syst Rev. 2013 Mar 28;(3):CD003852. doi: 10.1002/14651858.CD003852.pub3
- Singh, C., Kawatra, R., Gupta, J., Awasthi, V., & Dungana, H. (2016). Therapeutic role of Vitamin B12 in patients of chronic tinnitus: A pilot study. Noise & health, 18(81), 93–97. https://doi.org/10.4103/1463-1741.178485
- Berkiten G, Yildirim G, Topaloglu I, Ugras H. Vitamin B12 levels in patients with tinnitus and effectiveness of vitamin B12 treatment on hearing threshold and tinnitus. B-ENT. 2013;9(2):111-6.
- ATKINSON M. Vitamin A in treatment of tinnitus and chronic progressive deafness: results of an investigation. AMA Arch Otolaryngol. 1954 Feb;59(2):192-4. doi: 10.1001/archotol.1954.00710050204010
- Hulshof JH, Vermeij P. The effect of nicotinamide on tinnitus: a double-blind controlled study. Clin Otolaryngol Allied Sci. 1987 Jun;12(3):211-4. doi: 10.1111/j.1365-2273.1987.tb00189.x
- Hurtuk A, Dome C, Holloman CH, Wolfe K, Welling DB, Dodson EE, Jacob A. Melatonin: can it stop the ringing? Ann Otol Rhinol Laryngol. 2011 Jul;120(7):433-40. doi: 10.1177/000348941112000703
- Person, O. C., Puga, M. E., da Silva, E. M., & Torloni, M. R. (2016). Zinc supplementation for tinnitus. The Cochrane database of systematic reviews, 11(11), CD009832. https://doi.org/10.1002/14651858.CD009832.pub2
- McFerran DJ, Phillips JS. Tinnitus. J Laryngol Otol. 2007 Mar;121(3):201-8. doi: 10.1017/S0022215106002714
- Bhimrao SK, Masterson L, Baguley D. Systematic review of management strategies for middle ear myoclonus. Otolaryngol Head Neck Surg. 2012 May;146(5):698-706. doi: 10.1177/0194599811434504
- Folmer RL, Theodoroff SM, Casiana L, Shi Y, Griest S, Vachhani J. Repetitive Transcranial Magnetic Stimulation Treatment for Chronic Tinnitus: A Randomized Clinical Trial. JAMA Otolaryngol Head Neck Surg. 2015 Aug;141(8):716-22. doi: 10.1001/jamaoto.2015.1219
- Piccirillo, JF, Kallogjeri, D, Nicklaus, J. Low-frequency transcranial magnetic stimulation to the temporoparietal junction for tinnitus; four-week stimulation trial. JAMA Otolaryngol Head Neck Surg. 2013;139:388-395
- Anders, M, Dvorakova, J, Rathova, L. Efficacy of repetitive transcranial magnetic stimulation for the treatment of refractory chronic tinnitus; a randomized placebo controlled study. Neuroendocrin Lett. 2010;31:238-249.
- Meng, Z, Liu, S, Zheng, Y, Phillips, JS. Repetitive transcranial magnetic stimulation for tinnitus. Cochrane Database Syst Rev. 2011;(10):CD007946.
- Peng, Z, Chen, Z, Gong, S. Effectiveness of repetitive transcranial magnetic stimulation for chronic tinnitus; a systematic review. Otolaryngol Head Neck Surg. 2012;147:817-825.
- Nondahl, DM, Cruickshanks, KJ, Wiley, TL. The ten-year incidence of tinnitus among older adults. Int J Audiol. 2010;49(8):580-585.
- Sindhusake, D, Mitchell, P, Newall, P, Golding, M, Rochtchina, E, Rubin, G. Prevalence and characteristics of tinnitus in older adults: the Blue Mountains Hearing Study. Int J Audiol. 2003;42(5):289-294.
- Nondahl, DM, Cruickshanks, KJ, Wiley, TL. Prevalence and 5-year incidence of tinnitus among older adults: the epidemiology of hearing loss study. J Am Acad Audiol. 2002;13(6):323-331.
- Gopinath, B, McMahon, CM, Rochtchina, E, Karpa, MJ, Mitchell, P. Incidence, persistence, and progression of tinnitus symptoms in older adults: the Blue Mountains Hearing Study. Ear Hear. 2010;31(3):407-412.
- Hesser, H, Weise, C, Rief, W, Andersswon, G. The effect of waiting: a meta-analysis of wait-list control groups in trials for tinnitus distress. J Psychosom Res. 2010;70:378-384.
- Nyenhuis, N, Zastrutzki, S, Weise, C, Jager, B, Kroner-Herwig, B. Efficacy of minimal contact interventions for acute tinnitus: a randomised controlled study. Cogn Behav Ther. 2013;42:127-138.
- Hallam, RS, Rachman, S, Hinchcliffe, R. Psychological aspects of tinnitus. In: Rachman, S , ed. Contributions to Medical Psychology. Vol. 3. Oxford, UK: Pergamon Press; 1984:31-53.
- Stouffer, JL, Tyler, RS, Kileny, PR, Dalzell, LE. Tinnitus as a function of duration and etiology: counseling implications. Am J Otol. 1991;12:188-194.