Transurethral resection of the prostate
Transurethral resection of the prostate (TURP) is surgery to remove some prostate tissue. Transurethral resection of the prostate (TURP) is done when an overgrown prostate gland is pressing on the urethra and making it hard for a man to urinate.
The prostate gland is a small organ just below a man’s bladder. It makes most of the fluid in semen. The urethra is the tube that carries urine from the bladder out of the body through the penis. It passes through the prostate. When the prostate gets too large, it can press on the urethra.
Transurethral resection of the prostate surgery may be done for:
- Chronic bacterial prostatitis that resists antibiotic treatment, with or without infected prostate stones ( prostatic calculi). Very few studies have been done to see how well this surgery works for prostatitis. It is not usually recommended as a treatment for prostatitis 1
- Repeated urinary tract infections because of another prostate problem for which surgery may be appropriate, such as prostate enlargement (benign prostatic hyperplasia, or BPH).
Transurethral resection of the prostate is done to take pressure off of the urethra. It can help you have better control over starting and stopping your urine stream. You may feel like you get more relief when you urinate.
Most men go home from the hospital 1 or 2 days after surgery. You may be able to go back to work or most of your usual routine in 1 to 3 weeks. But for about 6 weeks, you will need to avoid heavy lifting and activities that might put extra pressure on your bladder.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor or nurse call line if you are having problems. It’s also a good idea to know your test results and keep a list of the medicines you take.
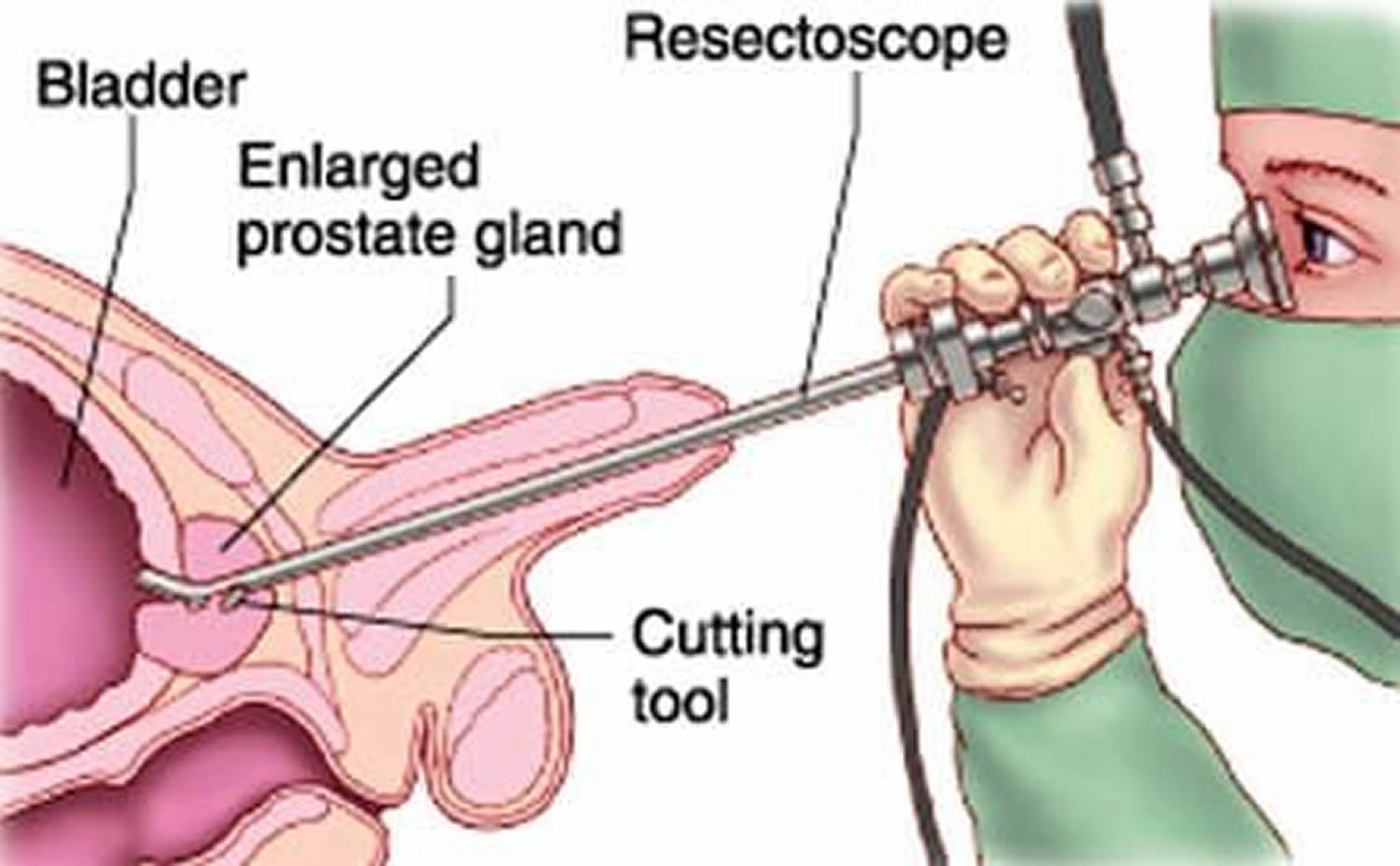
How is the transurethral resection of the prostate surgery done?
Your doctor will give you medicine to make you sleep or feel relaxed. You will be kept comfortable. If you are awake during the surgery, you will get medicine to numb you from the chest down.
The doctor will put a thin, lighted tube, which is called a scope, into your urethra through the opening in your penis. Then the doctor will put small surgical tools or a tiny laser through the scope. He or she will then cut or burn away the section of the prostate that is blocking urine flow. When the surgery is finished, the doctor will take out the scope.
What can you expect after the transurethral resection of the prostate surgery?
You may stay in the hospital for 1 to 2 days after the surgery. You may be able to go back to work and do many of your usual activities in 1 to 3 weeks. But it is important to avoid heavy lifting or strenuous activities for about 6 weeks.
If your surgery was done with a laser, you may feel better faster. Most men go home on the day of laser surgery, then see their doctor soon after. You may be able to go back to work and your usual activities after a few days. And you may be able to return to strenuous activity and heavy lifting after about 2 weeks. But talk to your doctor first.
You may need a urinary catheter for a short time. This is a flexible plastic tube used to drain urine from your bladder when you can’t urinate on your own. If it is still in place when you go home, your doctor will give you instructions for how to care for your catheter.
You may still feel like you need to urinate often in the weeks after your surgery. It often takes up to 6 weeks for this to get better.
After they recover from surgery, most men still can have erections (if they were able to have them before surgery). But they may not ejaculate when they have an orgasm. Semen may go into the bladder instead of out through the penis. This is called retrograde ejaculation. It does not hurt and is not harmful to your health. But it may mean that you will not be able to father a child. If this is a concern, talk to your doctor. You may be able to save your sperm before the surgery.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor or nurse call line if you are having problems. It’s also a good idea to know your test results and keep a list of the medicines you take.
Transurethral resection of the prostate recovery
After transurethral resection of the prostate surgery, you will have a urinary catheter for a short time. It is a flexible plastic tube used to drain urine from your bladder when you can’t urinate on your own. If it is still in place when you go home, your doctor will give you instructions on how to care for it.
For several days after surgery, you may feel burning when you urinate. Your urine may be pink for 1 to 3 weeks after surgery. You also may have bladder cramps, or spasms. Your doctor may give you medicine to help control the spasms.
You may still feel like you need to urinate often in the weeks after your surgery. It often takes up to 6 weeks for this to get better. After you have healed, you may have less trouble urinating. You may have better control over starting and stopping your urine stream. And you may feel like you get more relief when you urinate.
After transurethral resection of the prostate, most men can return to work or many of their usual tasks in a few days. But for about 2 weeks, try to avoid heavy lifting and strenuous activities that might put extra pressure on your bladder.
Most men still can have erections after surgery (if they were able to have them before surgery). But they may not ejaculate when they have an orgasm. Semen may go into the bladder instead of out through the penis. This is called retrograde ejaculation. It does not hurt and is not harmful to your health.
How to care for yourself at home
Activity
- Rest when you feel tired.
- Be active. Walking is a good choice.
- Allow your body to heal. Don’t move quickly or lift anything heavy until you are feeling better.
- Ask your doctor when you can drive again.
- Many people are able to return to work within a few days after surgery.
- Do not put anything in your rectum, such as an enema or suppository, for 4 to 6 weeks after the surgery.
- You may shower and take baths when your doctor says it is okay.
- Ask your doctor when it is okay for you to have sex.
Medicines
- Your doctor will tell you if and when you can restart your medicines. He or she will also give you instructions about taking any new medicines.
- If you take aspirin or some other blood thinner, be sure to talk to your doctor. He or she will tell you if and when to start taking those medicines again. Make sure that you understand exactly what your doctor wants you to do.
- Be safe with medicines. Read and follow all instructions on the label.
- If the doctor gave you a prescription medicine for pain, take it as prescribed.
- If you are not taking a prescription pain medicine, ask your doctor if you can take an over-the-counter medicine.
- Take your antibiotics as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
Diet
- You can eat your normal diet. If your stomach is upset, try bland, low-fat foods like plain rice, broiled chicken, toast, and yogurt.
- If your bowel movements are not regular right after surgery, try to avoid constipation and straining. Drink plenty of water. Your doctor may suggest fiber, a stool softener, or a mild laxative.
Complications of transurethral resection of the prostate
The complications of transurethral resection of prostate include:
- Bleeding.
- Urinary incontinence
- Inability to get or keep an erection (erectile dysfunction)
- Retrograde ejaculation. This means that semen flows the wrong way, from the prostate to the bladder rather than from the prostate through the penis.
Call your local emergency number anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have chest pain, are short of breath, or cough up blood.
Call your doctor or seek immediate medical care if:
- You have pain that does not get better after you take pain medicine.
- You have new or more blood clots in your urine. (It is normal for the urine to be pink for a few days.)
- You can’t pass urine.
- You have symptoms of a urinary tract infection. These may include:
- Pain or burning when you urinate.
- A frequent need to urinate without being able to pass much urine.
- Pain in the flank, which is just below the rib cage and above the waist on either side of the back.
- Blood in your urine.
- A fever.
- You are sick to your stomach or can’t keep down fluids.
- You have signs of a blood clot in your leg (called a deep vein thrombosis), such as:
- Pain in your calf, back of the knee, thigh, or groin.
- Redness or swelling in your leg.
Watch closely for changes in your health, and be sure to contact your doctor or nurse call line if you have problems.
Transurethral resection of bladder
Transurethral resection of the bladder is a surgical procedure that is used both to diagnose bladder cancer and to remove cancerous tissue from the bladder. Transurethral resection of the bladder procedure is also called a transurethral resection for bladder tumor (TURBT). Transurethral resection of bladder tumor (TURBT), performed endoscopically, is the first-line procedure for diagnosis, staging, and treatment of visible tumors. General anesthesia or spinal anesthesia is often used. During transurethral resection surgery, a cystoscope is passed into the bladder through the urethra. A tool called a resectoscope is used to remove the cancer for biopsy and to burn away any remaining cancer cells.
Transurethral resection can be used to diagnose, stage, and treat bladder cancer.
- Diagnosis. transurethral resection is used to examine the inside of the bladder to see whether there are cancer cells in the bladder.
- Staging. transurethral resection can determine whether cancers are growing into the bladder wall.
- Treatment. One or more small tumours can be removed from inside the bladder during transurethral resection.
Transurethral resection is the most common and effective treatment for early-stage bladder cancer. It may also be effective for more advanced cancer if all the cancer is removed and biopsies show that no cancer cells remain. Treatment with transurethral resection may be followed by chemotherapy or immunotherapy.
Transurethral resection of bladder tumor (TURBT) is not effective for carcinoma in situ (CIS) because the disease is often so diffuse and difficult to visualize that surgical removal is not feasible. Therefore, the role of cystoscopy in these cases is to establish the diagnosis so that therapy can be instituted. Obvious areas of carcinoma in situ (CIS) may also be fulgurated, but the benefits of this have not been proven. When a combination of papillary tumor and carcinoma in situ (CIS) is present, the papillary tumor is removed before treatment of the carcinoma in situ (CIS) is initiated.
Bladder cancer can come back after transurethral resection surgery, so repeat transurethral resections are sometimes needed.
Following transurethral resection surgery, a catheter may be placed in the urethra to help stop bleeding and to prevent blockage of the urethra. When the bleeding has stopped, the catheter is removed. You may need to stay in the hospital 1 to 4 days.
You may feel the need to urinate frequently for a while after the surgery, but this should improve over time. You may have blood in your urine for up to 2 to 3 weeks following surgery.
You may be instructed to avoid strenuous activity for about 3 weeks following transurethral resection.
Transurethral resection of bladder tumor recovery
Occasionally, a catheter may need to be left in place for 1-3 days after bladder biopsies. It is usually removed in the urology office.
Within the first 24 hours, a single intravesical instillation of mitomycin-C (40 mg in 20 mL of saline) has been shown to reduce the frequency of tumor recurrence and should be considered the standard of care after transurethral resection of bladder tumor (TURBT) or positive bladder biopsy findings. [10]
A second transurethral resection of bladder tumor (TURBT) should be performed 2-6 weeks after initial TURBT for several patient populations. Indications include the following:
- Incomplete initial resection
- Absence of muscularis propria in the specimen
- T1 tumor
- High-grade tumor
A second TURBT can be omitted for patients with primary carcinoma in situ or for solitary low-grade Ta tumors. The rationale for second TURBT is the risk of understaging, as well as the significant risk of residual tumor after initial TURBT.
Complications of transurethral resection of bladder tumor
The complications of transurethral resection of bladder tumor include:
- Bleeding.
- Bladder infection (cystitis) .
- Perforation of the wall of the bladder.
- Blood in the urine (hematuria).
- Blockage of the urethra by blood clots in the bladder.
Call your local emergency number anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have chest pain, are short of breath, or cough up blood.
Call your doctor or seek immediate medical care if:
- You have pain that does not get better after you take pain medicine.
- You have new or more blood clots in your urine. (It is normal for the urine to be pink for a few days.)
- You can’t pass urine.
- You have symptoms of a urinary tract infection. These may include:
- Pain or burning when you urinate.
- A frequent need to urinate without being able to pass much urine.
- Pain in the flank, which is just below the rib cage and above the waist on either side of the back.
- Blood in your urine.
- A fever.
- You are sick to your stomach or can’t keep down fluids.
- You have signs of a blood clot in your leg (called a deep vein thrombosis), such as:
- Pain in your calf, back of the knee, thigh, or groin.
- Redness or swelling in your leg.
Watch closely for changes in your health, and be sure to contact your doctor or nurse call line if you have problems.