Urethral sling
Urethral sling surgery also called mid urethral sling is the gold standard in stress urinary incontinence treatment 1. Urethral sling surgery is suitable for women who are having their first operation to prevent urinary incontinence, and also women who have had unsuccessful surgery previously. In a mid‐urethral sling operation a strip of material (a “sling”) is placed underneath the bladder neck or the urethra which is the tube that carries urine out of the bladder and the skin of the vagina. Normally the muscle and ligaments, which support the urethra, close firmly when straining or exercising to prevent leakage. Damage or weakening of these structures by childbirth and/or the aging process can result in this mechanism failing, leading to urine leakage. Placing a sling underneath the urethra improves the support and reduces or stops leaking. The sling improves support of the bladder neck and/or urethra to help prevent urine leaks. Slings can be made from your own tissue (autologous graft), donor tissue (typically skin or fascia) or surgical polypropylene mesh about 1cm wide (suture material that is woven together). Today, surgical mesh is made of type 1, macroporous, monofilament and non-carcinogenic polypropylene. The open-weave mesh stabilizes and promotes ingrowth of the collagen over time. When the woman coughs, the tape or surgical mesh compresses the tube, thus providing the support necessary to prevent urine leakage.
Stress incontinence is the leakage of urine with every day activities such as coughing, sneezing or exercise. Stress urinary incontinence is a very common and embarrassing problem affecting up to 1 in 3 women. Stress urinary incontinence may be cured or improved with pelvic floor exercises and lifestyle modifications, but if these strategies fail then surgery may be recommended for you. The most frequently offered type of operation is a mid-urethral sling procedure, a simple day case procedure that has been performed for more than 3 million women worldwide to date.
The effectiveness of the urethral sling procedure is estimated for 70–98%; nevertheless, the risk of reoperation reaches even 9% 2. Indications for reoperations are usually lack of effectiveness, voiding dysfunctions, overactive bladder syndrome, pain, or recurrent infections 3.
How do urethral sling work?
The sling (or tape) prevents leakage by supporting the urethra and mimicking the ligaments that have been weakened by having babies and the aging process. Once the sling is in position your tissues grow through the holes in the weave and so anchor it in position. This may take 3 to 4 weeks.
Do I need an anesthetic for the mid urethral sling procedure?
Although it is possible to do the urethral sling procedure just with local anesthetic, most surgeons would supplement this with a strong sedative or, sometimes, a full general anesthetic. Occasionally, the surgery is done using a spinal or an epidural anesthetic, depending on the preference of the patient, anesthetist and surgeon.
When will I be able to go home after the urethral sling procedure?
Most surgeons will allow patients to go home after a mid-urethral sling procedure once they are emptying their bladders efficiently and after any pain has been adequately controlled. Normally this time will vary from a few hours to a couple of days depending on the facilities available.
What are the chances of success of the urethral sling procedure?
Research tells us that, in the short term, mid-urethral sling procedure is as successful as any more invasive procedure used for controlling stress incontinence, but with a quicker recovery and less chance of needing surgery for prolapse in the first two years after the surgery 1. Between 80 – 90% of women are happy with their operation and feel that their incontinence is either cured or much better. However, there are a small group of women for whom the operation does not seem to work. The mid-urethral sling procedure is less likely to be a success if you have had previous surgery to your bladder (such as a repair operation).
The most common retropubic operation to be carried out is the TVT (Tension-free Vaginal Tape). This is also the operation that has been done for the longest time, and research suggests that if it is initially successful in controlling stress incontinence then it is still likely to be working up to at least 17 years later. The other retropubic and transobturator mid-urethral sling procedures are likely to have similar long term success rates.
My bladder isn’t too bad at the moment, but should I have an operation now to prevent it getting worse in the future?
It is difficult to predict what will happen to your bladder in the future; doing regular pelvic floor exercises improves stress incontinence in up to 75% of women and may mean surgery is never required. You should have the mid urethral sling procedure only if you feel the stress incontinence is affecting the quality of your life now, not to prevent it deteriorating in the future.
I haven’t finished having my family yet, can I still have a mid urethral sling procedure?
Many surgeons would want to avoid surgery until a woman’s family is complete because future pregnancy may compromise the results of the initial surgery.
How will the operation affect my sex life?
Experts usually advise you to wait for 4 weeks after the operation before having sexual intercourse. In the long term there is no evidence that the operation will make any difference to your sex life. If you previously leaked urine during intercourse, the mid urethral sling procedure might make this better, but this is not always the case.
If a patient has mid urethral sling surgery with mesh, do they need to have it removed?
Surgical mesh is designed to be a permanent implant. If a patient has had this surgery and is not having any side effects, there is no need to remove the mesh. Mesh removal could have its own side effects, including injury to tissues near the mesh or recurrent incontinence.
Is there anything else I can do instead of mid urethral sling surgery?
Pelvic Floor exercises
Pelvic floor exercises can be a very effective way of improving symptoms of stress urinary incontinence. Up to 75 % of women show an improvement in leakage after pelvic floor exercise training. Like all training the benefits of pelvic floor exercises are maximized if practice is carried out regularly over a period of time. Maximum benefit usually occurs after 3 to 6 months of regular exercising. You may be referred to a physical therapist (physiotherapist) specializing in teaching pelvic floor exercises to supervise this.
If you also have a problem with urge urinary incontinence your doctor may also advise bladder retraining exercises.
Continence Devices
Continence devices are available which fit in the vagina and help control leakage, these can be inserted prior to exercise or in the case of a vaginal pessary can be worn continuously. Some women find inserting a large tampon prior to exercise may prevent or reduce leakage. These types of device are most suitable for women with more minor degrees of urinary incontinence or who are waiting definitive surgical treatment
Lifestyle Changes
Being overweight can make stress and urge incontinence worse whilst reducing weight can result in an improvement in incontinence symptoms. Maintaining a good general health, quitting smoking having good control of medical conditions such as asthma can also be helpful.
Mid urethral sling procedure
Tension-free mid urethral sling
No stitches are used to attach the tension-free sling, which is made from a strip of synthetic mesh tape. Instead, body tissue holds the sling in place. Eventually scar tissue forms in and around the mesh to keep it from moving.
There are three main routes for placing the mid urethral tension-free sling: the retropubic route (behind the pubic bone through the abdomen), the trans-obturator route (through the groin) and the “single incision” or “mini-sling”. There is no clear advantage of one over the other, except for some women with severe stress incontinence where the retropubic route appears to be more successful. Mini-slings are still in the initial phases of investigation. Although they are less invasive than the other methods they may not be quite as effective in controlling stress incontinence in the longer term, or in women with severe incontinence. The sling procedure that’s best for you depends on your situation. Discussing the risks and benefits of each type of sling procedure with your doctor can help you make the right choice.
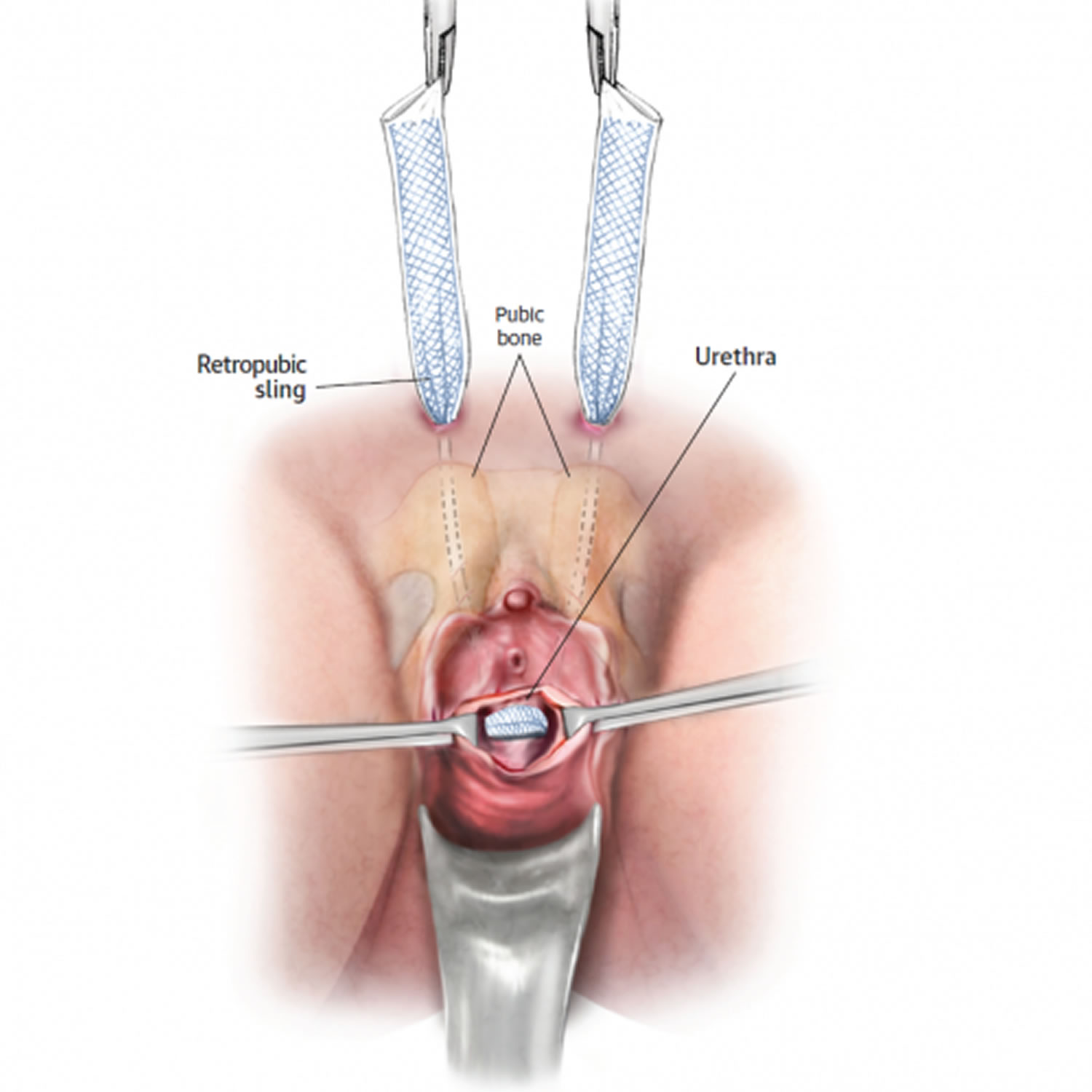
Retropubic urethral sling placement
With the retropubic approach, your surgeon makes a small cut (incision) inside your vagina over the mid point of the urethra. Your surgeon also makes two small openings above your pubic bone just large enough for a needle to pass through. Your surgeon then uses a needle to pass the two ends of the sling from the vagina, passing either side of the urethra to exit through two small cuts made just above the pubic bone in the hairline, about 4-6 cm apart. The surgeon will then use a camera (cystoscope) to check that the sling is correctly positioned and not sitting within the bladder. The sling is then adjusted so that it sits loosely underneath the urethra and the vaginal cut stitched to cover the sling over. The ends of the sling are cut off and they too are covered over. A few absorbable stitches close the vaginal incision, and the needle sites may be sealed with skin glue or stitches.
Figure 1. Retropubic mid urethral sling placement
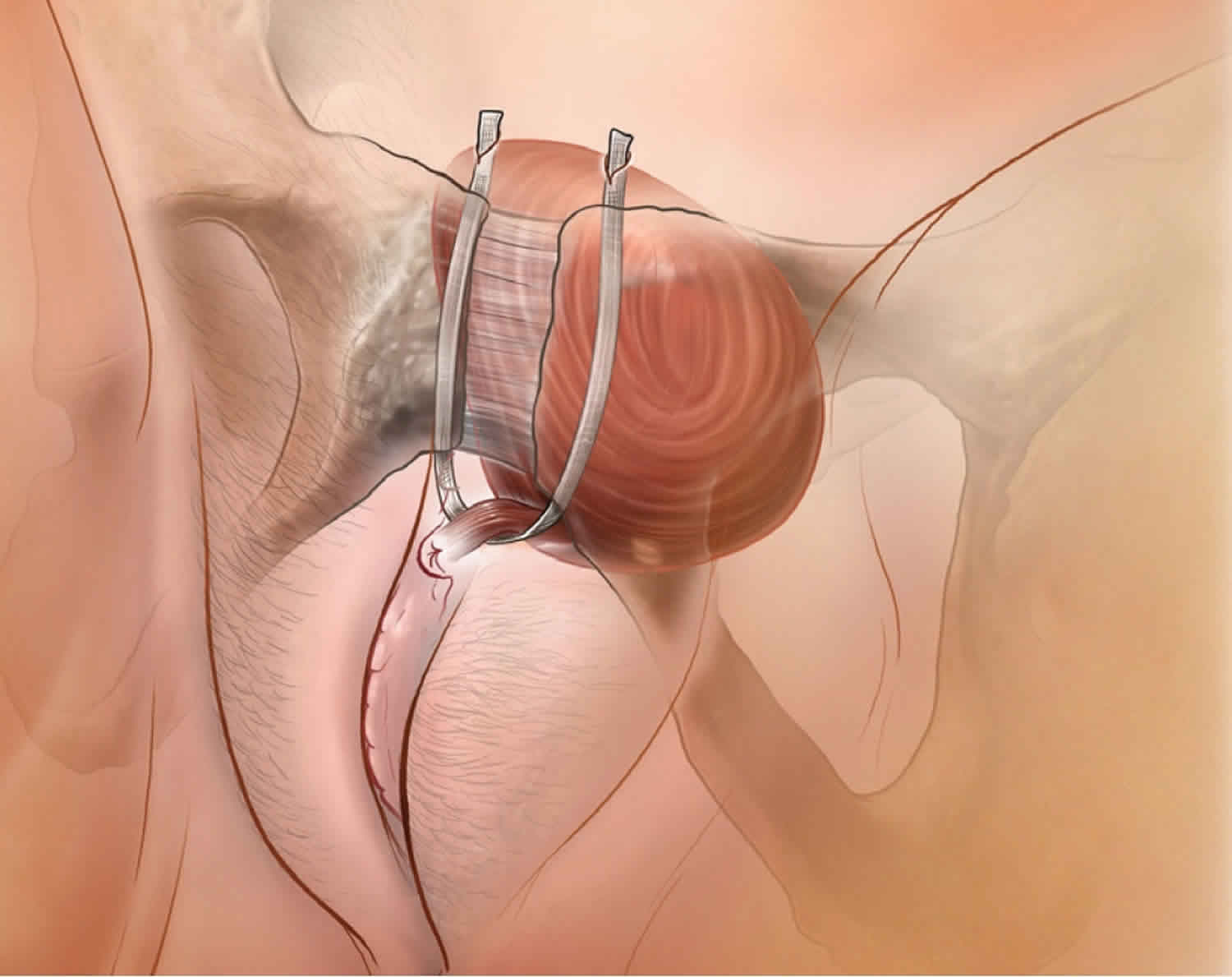
Transobturator urethral sling placement
The transobturator approach to the operation also requires a small incision to be made in the vagina at the same place as for the retro-pubic operation. The ends of the sling are through two small incisions made, this time, in the groin. Each end of the sling passes through the obturator foramen, which is a gap between the bones of the pelvis. The ends are cut off once the sling is confirmed to be in the in the correct position and the skin closed over them. Your surgeon closes the vaginal incision with absorbable stitches and the needle site with skin glue or stitches.
Figure 2. Transobturator mid urethral sling placement
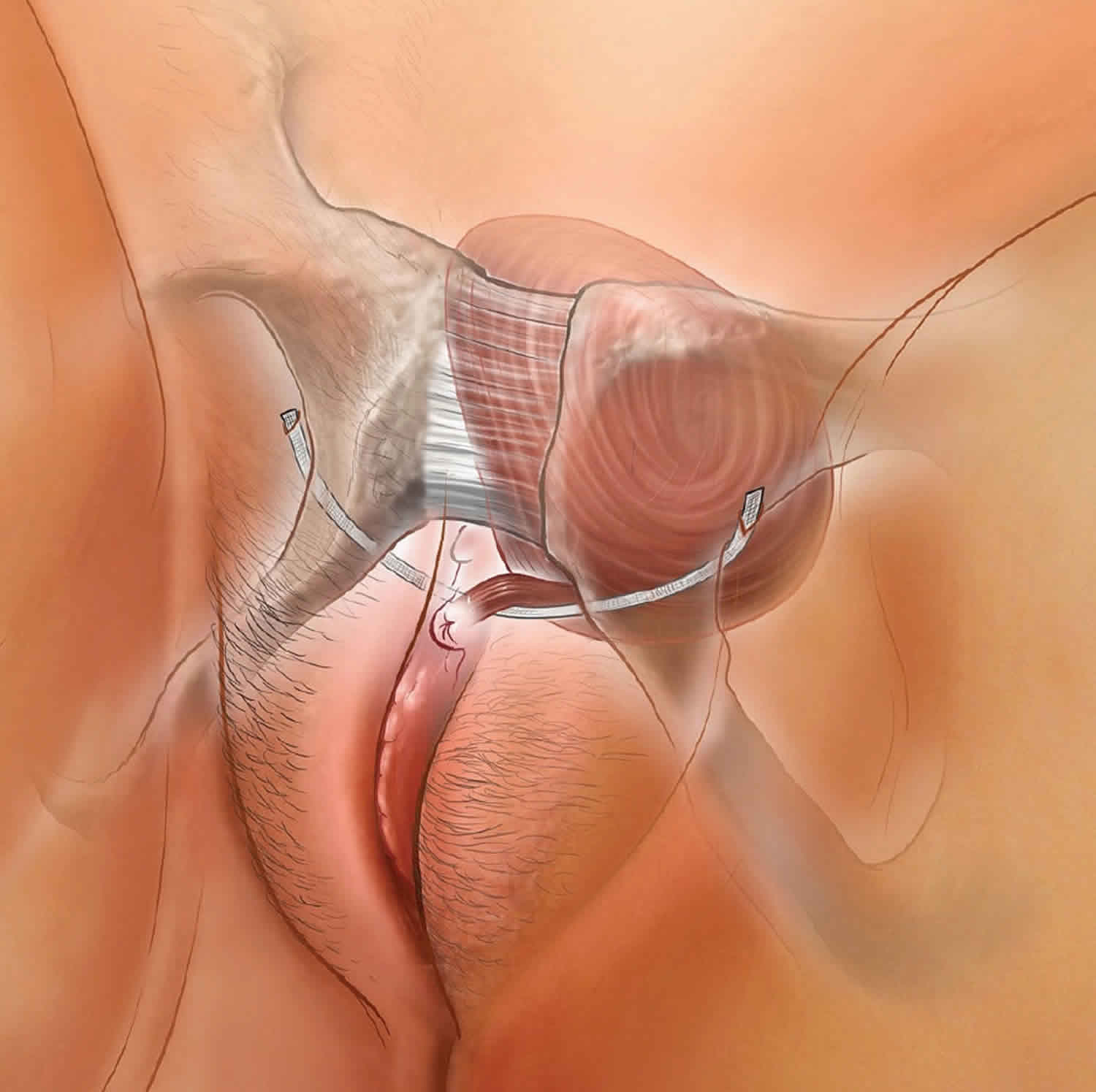
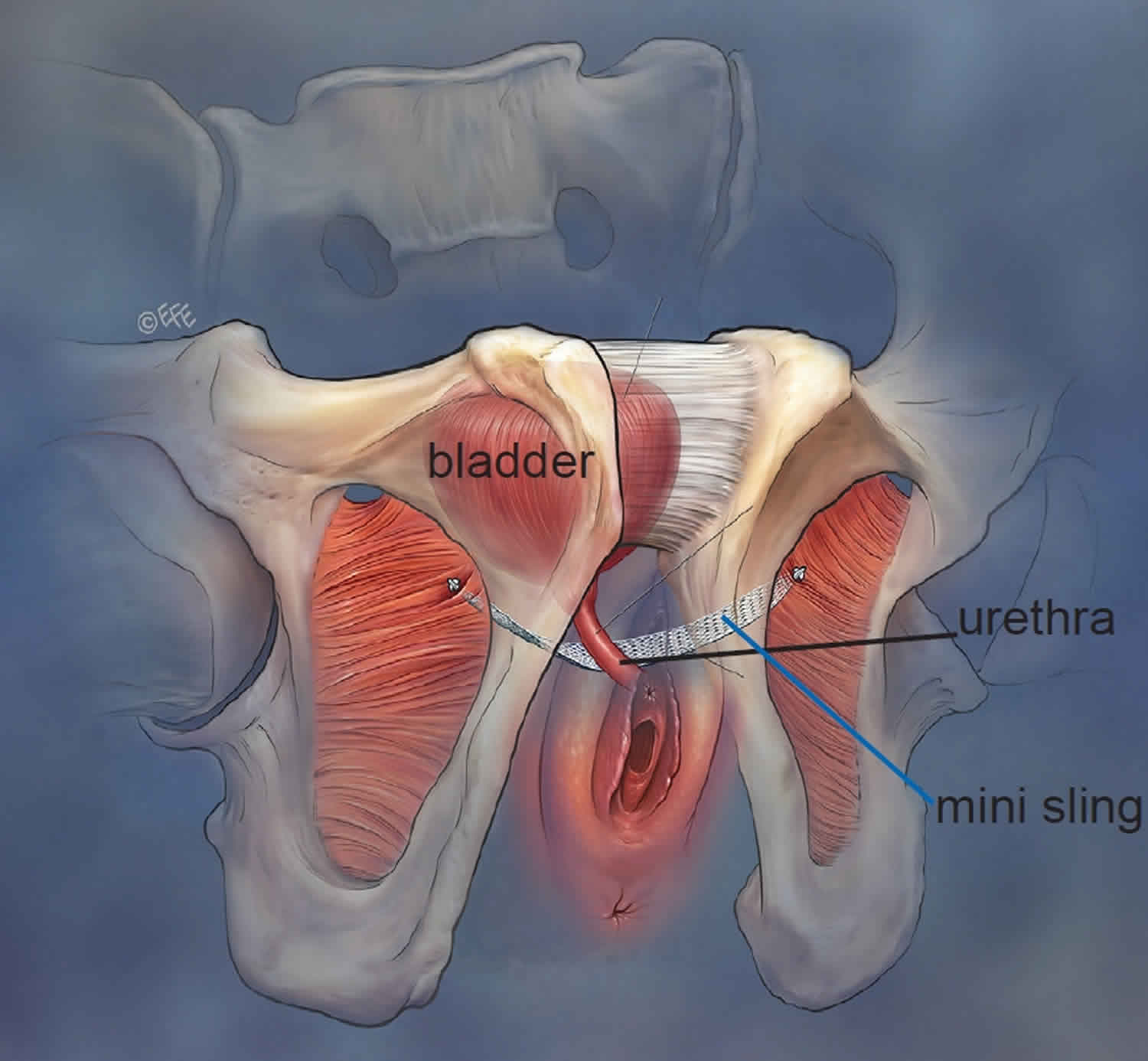
Single-incision mini-sling procedure
With mini-sling procedure, your surgeon makes only one small incision in your vagina to perform the procedure. Through this single incision, your surgeon places the sling in a manner similar to the retropubic and transobturator approaches. No other incisions or needle sites are needed. The ends of the sling do not come out onto the skin and are anchored in position by one of a number of different fixation techniques.
Figure 3. Single-incision mini-sling procedure
Conventional mid urethral sling surgery
With a conventional approach, your surgeon makes an incision in your vagina and places a sling made of synthetic mesh tape — or possibly your own tissue or tissue from an animal or deceased donor — under the neck of your bladder. Through another incision in your abdomen, your surgeon pulls the sling to achieve the right amount of tension and attaches each end of the sling to pelvic tissue (fascia) or your abdominal wall using stitches.
A conventional sling sometimes requires a larger incision than does a tension-free sling. You might need an overnight stay in a hospital and usually a longer recovery period. You may also need a temporary catheter after surgery while you heal.
Mid urethral sling recovery
Recovery time for tension-free urethral sling surgery varies. Your doctor may recommend two to four weeks of healing before returning to activities that include heavy lifting or strenuous exercise. It may be up to six weeks before you’re able to resume sexual activity.
Using surgical mesh can be a safe and effective way to treat stress urinary incontinence. However, serious complications occur in some women, including erosion of the material, infection and pain.
When can I return to my usual routine?
You should be able to drive and be fit enough for usual daily activities within a week of surgery. Experts advise you to avoid heavy lifting and sport for 6 weeks to allow the wounds to heal and the sling to be firmly held in place.
Mid urethral sling risks and complications
There is no completely “risk free” operation for stress incontinence. The three methods of placing the sling have their own specific risks but all can be complicated by:
- Urinary tract infections – these are not uncommon after any procedure and should respond to antibiotics. Symptoms of a urinary tract infection include burning, stinging, the need to pass urine frequently and in some cases bloody, cloudy or offensive smelling urine. If you notice these symptoms contact your doctor.
- Bleeding – bleeding, sufficient to require a blood transfusion, is very rare. Sometimes bleeding can happen where the tape from a retro-pubic operation passes behind the pelvic bones. This is normally self limiting and only very rarely needs an operation to fix.
- Difficulty passing urine (voiding difficulty). Some women have difficulty emptying their bladder following sling surgery; this is often because of swelling around the urethra or discomfort and will usually settle quickly (within a week). During this time your doctor may recommend a fine tube or urinary catheter be used to drain the bladder. If your urine stream remains very slow or you cannot empty the bladder well even after the swelling has settled then your surgeon will discuss other possibilities, such as cutting or stretching the sling, with you.
- Sling exposure – very occasionally the sling can appear in the wall of the vagina a few weeks, months or years after an operation. Your partner may notice a rough area during intercourse, or you may feel an uncomfortable prickling sensation in the vagina. Occasionally there can be some blood stained discharge. In this case you should consult your surgeon who will be able to advise which method of resolving the situation; usually this would involve either re-covering the tape or removing the section of tape that is exposed. The risks of this happening are about 1 in 100 after a retro-pubic operation or mini-sling and more slightly frequently than this after a transobturator operation.
- Bladder or urethral perforation: Bladder perforation occurs most often during a retro-pubic operation, whilst the urethra is most at risk of damage during a trans-obturator procedure. Your surgeon will check for damage during the operation by looking inside the bladder and urethra using a special telescope (cystoscope). Removing and correctly relocating the needle to which the sling is attached should resolve the situation. The bladder is normally then drained by a catheter for 24 hours to allow the hole in the bladder to heal itself. Damage to the urethra is more difficult to deal with, and should be discussed with your surgeon should it occur. Both are relatively rare, and bladder perforation, as long as it is recognized, does not affect the success of the operation.
- Urgency and urge incontinence. Women who have bad stress incontinence often experience urgency and urge incontinence, the leakage of urine associated with the sensation of urgency. About 50% of women notice an improvement in urgency symptoms but for about 5% the symptoms may worsen following a mid urethral sling procedure.
- Pain: Long term pain following urethral sling surgery is unusual, studies suggest that after the retro-pubic mid urethral sling surgery about 1 in 100 (1%) will develop vaginal or groin pain. Similar pain in the vagina or at the site of the cuts where the tape is put in can occur in as many as 1 in 10 women after a transobturator approach. In most cases pain is short lived and does not occur for more than 1 to 2 weeks. Rarely pain may not settle and removal of the sling is required.
Risks of any surgery are:
- Bleeding
- Blood clots in the legs that may travel to the lungs
- Breathing problems
- Infection in the surgical cut or opening of the cut
- Other infection
Risks of mid urethral sling surgery are:
- Injury to nearby organs
- Breaking down of the synthetic material used for the sling
- Erosion of the synthetic material through your normal tissue
- Changes in the vagina (prolapsed vagina)
- Damage to the urethra, bladder, or vagina
- Abnormal passage (fistula) between the bladder or urethra and vagina
- Irritable bladder, causing the need to urinate more often
- More difficulty emptying your bladder, and the need to use a catheter
- Worsening of urine leakage
- Ford AA, Rogerson L, Cody JD, Aluko P, Ogah JA. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2017;7(7):CD006375. Published 2017 Jul 31. doi:10.1002/14651858.CD006375.pub4 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6483329
- Fialkow M., Symons R. G., Flum D. Reoperation for urinary incontinence. American Journal of Obstetrics and Gynecology. 2008;199(5):546.e1–546.e8. doi: 10.1016/j.ajog.2008.04.047
- Kociszewski J., Kolben S., Barski D., Viereck V., Barcz E. Complications following tension-free vaginal tapes: accurate diagnosis and complications management. BioMed Research International. 2015;2015:5. doi: 10.1155/2015/538391.538391