Vaginal yeast infection
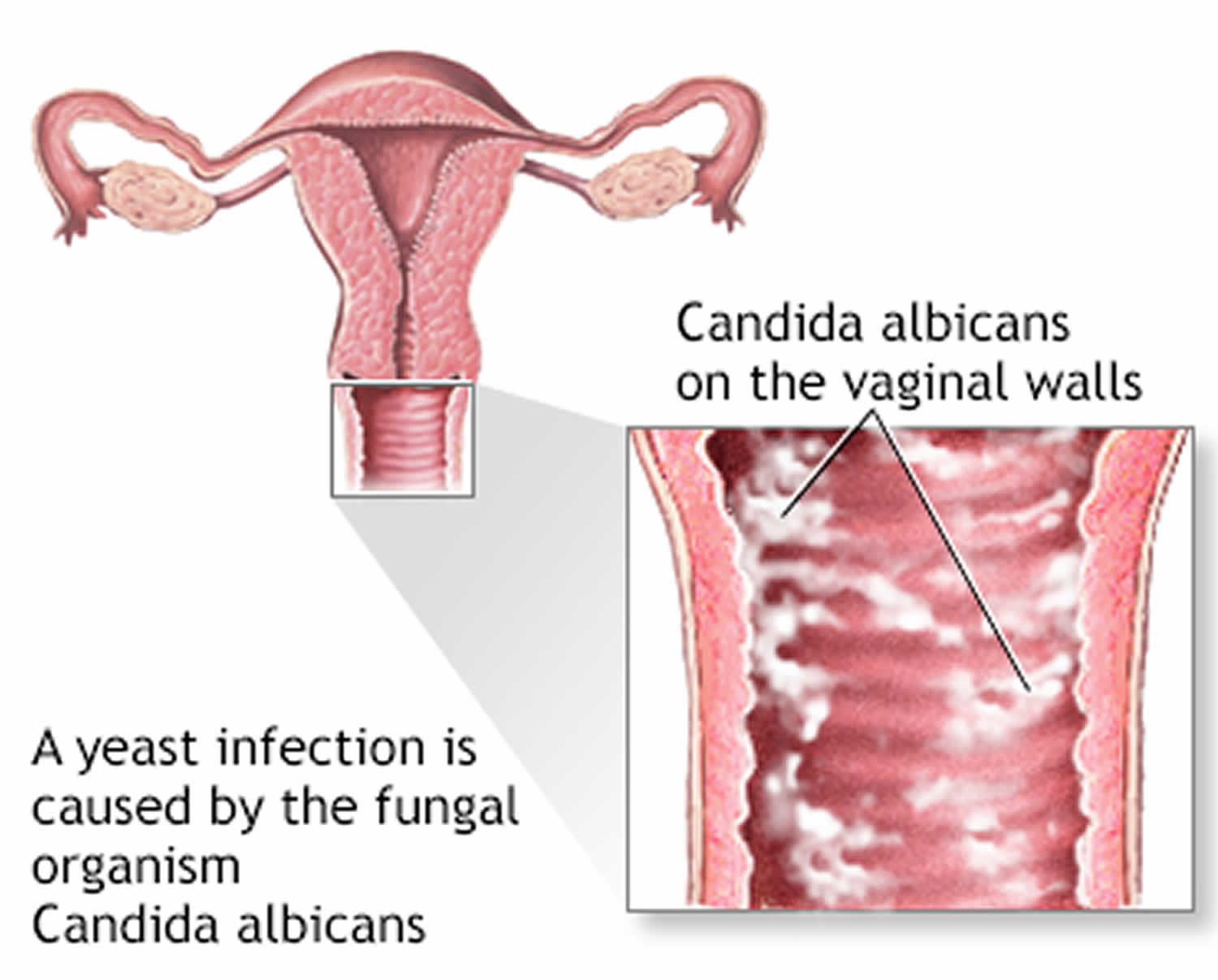
Vaginal yeast infection also known as vaginal thrush, vulvovaginal candidiasis, vaginal candidiasis, vulvovaginal candidosis or monilia, is a fungal infection most commonly caused by an overgrowth of the fungus Candida (mostly Candida albicans) in the the vagina and the vulva (the tissues at the vaginal opening) 1, 2. Symptoms of vaginal yeast infections include burning, itching, and thick, white discharge. Vaginal yeast infections are easy to treat, but it is important to see your doctor if you think you have a vaginal infection, because yeast infection (fungal infection) symptoms are similar to other vaginal infections and sexually transmitted infections (STIs). If you have a more serious infection, and not a yeast infection, it can lead to major health problems.
Vaginal yeast infection is characterized by:
- Itching, soreness and burning discomfort in the vagina and vulva
- Stinging when passing urine (dysuria)
- Pain during sex (dyspareunia)
- Vulval edema (swelling), fissures and excoriations
- Dense white curd or cottage cheese-like vaginal discharge and does not have a bad smell
- Bright red rash affecting inner and outer parts of the vulva, sometimes spreading widely in the groin to include pubic areas, groin and thighs. The rash is thought to be a secondary irritant dermatitis, rather than a primary skin infection.
- You may have only a few of these symptoms. They may be mild or severe.
The most common symptom of a vaginal yeast infection is extreme itchiness in and around your vagina.
Symptoms may last just a few hours or persist for days, weeks, or rarely, months, and can be aggravated by sexual intercourse.
Women and girls of all ages can get vaginal yeast infections. Vaginal yeast infections are rare before puberty and after menopause. Vaginal yeast infection affects up to 3 out of 4 women at some point in their lifetimes. Many women experience at least two or more episodes 3. About 8% of women suffer recurrent yeast infections 4. Recurrent yeast infection (recurrent vulvovaginal candidiasis) is usually defined as four or more episodes within one year. Recurrent yeast infection is more common in women with diabetes or weak immune systems, such as with HIV (human immunodeficiency virus), but it can also happen in otherwise healthy women. Doctors most often treat recurrent yeast infection with antifungal medicine for up to six months.
Chronic, persistent vulvovaginal candidiasis may lead to lichen simplex —a thickened, intensely itchy labia majora (the hair-bearing outer lips of the vulva).
A vaginal yeast infection isn’t considered a sexually transmitted infection (STI). But, there’s an increased risk of vaginal yeast infection at the time of first regular sexual activity. There’s also some evidence that vaginal yeast infections may be linked to mouth to genital contact (oral-genital sex).
Candida albicans is the most common type of fungus to cause yeast infections. Yeast infections caused by other types of Candida fungus can be more difficult to treat, and generally need more-aggressive therapies.
Medications can effectively treat vaginal yeast infections. If you have recurrent yeast infections — four or more within a year — you may need a longer treatment course and a maintenance plan.
Medicines to treat vaginal yeast infections are available as creams, ointments, vaginal tablets or suppositories and oral tablets. Most yeast infection treatment can be bought over the counter without a prescription or without needing to see your doctor. If the treatment is ineffective or symptoms recur, see your doctor for examination and advice in case symptoms are due to another cause or a different treatment is required. If you do need to see your doctor, you may wish to ask them about the use of boric acid for yeast infections.
Boric acid (boron) 600 mg as a vaginal suppository at night for two weeks reduces the presence of albicans and non-albicans Candida in 70% of treated women 5, 6. Boric acid can be irritating and is toxic, so should be stored safely away from children and animals. Twice-weekly use may prevent recurrent yeast infections. Boric acid should NOT be used during pregnancy!
Treating vaginal yeast infection at home is probably OK if:
- Your symptoms are mild and you do not have pelvic pain or a fever
- This is not your first yeast infection and you have not had many yeast infections in the past
- You are not pregnant
- You are not worried about other sexually transmitted infections (STI) from recent sexual contact
Medicines you can buy yourself to treat a vaginal yeast infection are:
- Miconazole
- Clotrimazole
- Tioconazole
- Butoconazole
When using these medicines:
- Read the packages carefully and use them as directed.
- You will need to take the medicine for 1 to 7 days, depending on which medicine you buy. (If you do not get repeated infections, a 1-day medicine might work for you.)
- Do not stop using these medicines early because your symptoms are better.
You doctor can also prescribe a pill that you only take by mouth once.
If your symptoms are worse or you get vaginal yeast infections often, you may need:
- Medicine for up to 14 days
- Azole vaginal cream or fluconazole pill every week to prevent new infections
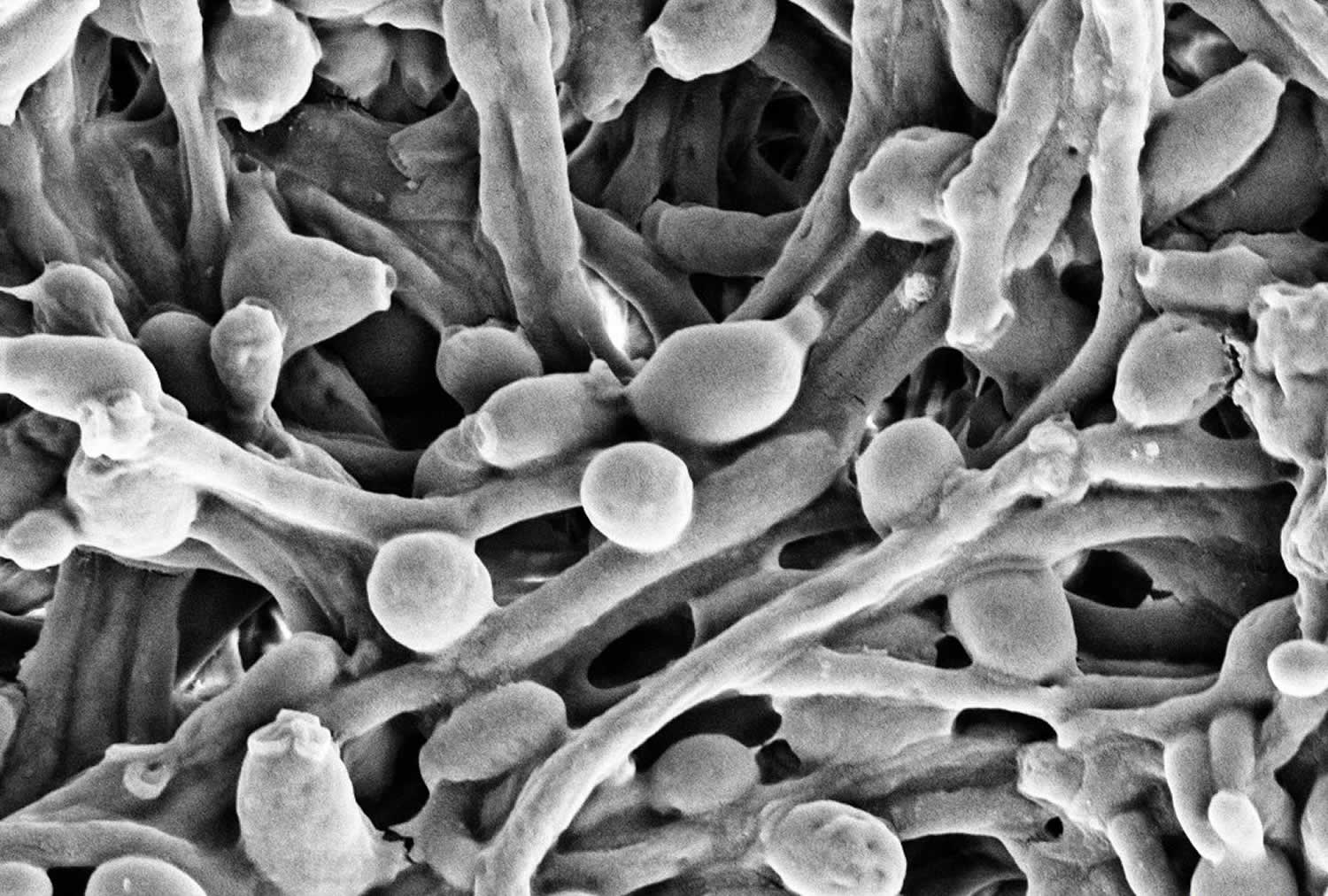
Figure 1. Candida albicans
Footnote: Candida albicans visualized using scanning electron microscopy
Make an appointment with your doctor if:
- This is the first time you’ve had yeast infection symptoms
- You’re not sure whether you have a yeast infection
- Your symptoms aren’t relieved after treating with over-the-counter antifungal vaginal creams or suppositories
- You develop other symptoms
Who gets vaginal yeast infection?
Vulvovaginal candidiasis is most commonly observed in women in the reproductive age group. It is quite uncommon in prepubertal and postmenopausal females. It may be associated with the following factors:
- Flares just before and during menstruation
- Pregnancy
- Higher dose combined oral contraceptive pill (higher doses of estrogen)
- Estrogen-based hormone replacement therapy after the menopause, including vaginal estrogen cream
- A course of broad-spectrum antibiotics such as tetracycline or amoxicillin
- You recently took steroid medicines
- Diabetes and your blood sugar is not under control
- Obesity
- Iron deficiency anemia
- Immunodeficiency such as HIV infection
- An underlying skin condition, such as vulval psoriasis, lichen planus or lichen sclerosus
- You douche or use vaginal sprays
- Other illness.
What does a vaginal yeast infection look like?
The way your vulva looks and feels and the type of discharge that comes from your vagina may change if you have a yeast infection. The area of skin just outside your vaginal opening may itch and burn. The itching and burning can feel worse when you pee or have sex. Your vaginal discharge may become thicker and lumpier, but it shouldn’t smell different. Not everyone experiences symptoms or has the same symptoms.
Can I get a yeast infection from having sex?
Yes. A yeast infection is not considered an sexually transmitted infection (STI), because you can get a yeast infection without having sex. But you can get a yeast infection from your sexual partner. Condoms and dental dams may help prevent getting or passing yeast infections through vaginal, oral, or anal sex.
If I have a yeast infection, does my sexual partner need to be treated?
Maybe. Yeast infections are not sexually transmitted infections (STIs). But it is possible to pass yeast infections to your partner during vaginal, oral, or anal sex.
- If your partner is a man, the risk of infection is low 7. About 15% of men get an itchy rash on the penis if they have unprotected sex with a woman who has a yeast infection. If this happens to your partner, he should see a doctor. Men who haven’t been circumcised and men with diabetes are at higher risk.
- If your partner is a woman, she may be at risk 7. She should be tested and treated if she has any symptoms.
Should I see a doctor if I think I have a yeast infection?
Yes. Seeing your doctor is the only way to know for sure if you have a yeast infection and not a more serious type of infection. Even women who have previously received a diagnosis of vulvovaginal candidiasis by a clinician are not necessarily more likely to be able to diagnose themselves; therefore, any woman whose symptoms persist after using an over-the-counter preparation or who has a recurrence of symptoms <2 months after treatment for vulvovaginal candidiasis should be evaluated clinically and tested.
The signs and symptoms of a yeast infection are a lot like symptoms of other more serious infections, such as sexually transmitted infections (STIs) and bacterial vaginosis (BV). If left untreated, sexually transmitted infections (STIs) and bacterial vaginosis raise your risk of getting other STIs, including HIV, and can lead to problems getting pregnant. Bacterial vaginosis can also lead to problems during pregnancy, such as premature delivery.
Is it safe to use over-the-counter medicines for yeast infections?
Yes, but always see your doctor before treating yourself for a vaginal yeast infection. This is because:
- You may be trying to treat an infection that is not a yeast infection. Studies show that two out of three women who buy yeast infection medicine don’t really have a yeast infection.2 Instead, they may have an sexually transmitted infection (STI) or bacterial vaginosis (BV). Sexually transmitted infections (STIs) and bacterial vaginosis require different treatments than yeast infections and, if left untreated, can cause serious health problems.
- Using treatment when you do not actually have a yeast infection can cause your body to become resistant to the yeast infection medicine. This can make actual yeast infections harder to treat in the future.
- Some yeast infection medicine may weaken condoms and diaphragms, increasing your chance of getting pregnant or an STI when you have sex. Talk to your doctor about what is best for you, and always read and follow the directions on the medicine carefully.
Are yeast infections harmful during pregnancy?
Other than being uncomfortable and sometimes painful, yeast infections do not usually cause complications in pregnancy or for the baby during pregnancy over the background risk. Scientists know that every pregnancy starts out with a 3-5% chance of having a birth defect and 10-15% chance for miscarriage 8. This is called the background risk.
If left untreated, however, a yeast infection could pass to your baby’s mouth during labor and delivery and may cause the baby to have a condition called “thrush”. Baby may then return the yeast infection back to you if the baby breastfeeds (causing yeast infection on the nipples) 8. Very rarely a yeast infection in babies can become serious because their immune systems are not yet well-developed.
Yeast infections can also cause body-wide infections and serious complications in pregnant people, especially those who have a weakened immune system because of other health problems 8.
What should I do if I get repeat yeast infections?
If you get four or more yeast infections in a year, see your doctor. About 5% of women get four or more vaginal yeast infections in one year. This is called recurrent vulvovaginal candidiasis. Recurrent yeast infection is more common in women with diabetes or weak immune systems, such as with HIV, but it can also happen in otherwise healthy women.
Doctors most often treat recurrent yeast infection with antifungal medicine for up to six months.
Chronic, persistent vulvovaginal candidiasis may lead to lichen simplex —a thickened, intensely itchy labia majora (the hair-bearing outer lips of the vulva).
Does yogurt prevent or treat yeast infections?
Maybe. Studies suggest that eating eight ounces of yogurt with “live cultures” daily or taking Lactobacillus acidophilus capsules can help prevent infection 9, 10. But, more research still needs to be done to say for sure if yogurt with Lactobacillus or other probiotics can prevent or treat vaginal yeast infections 9. If you think you have a yeast infection, see your doctor to make sure before taking any over-the-counter medicine.
Vaginal yeast infection causes
The fungus Candida albicans is responsible for most vaginal yeast infections (in about 90% of cases), with most of the remaining cases caused by Candida glabrata 11. Candida glabrata are observed in 10–20% of women with recurrent vulvovaginal candidiasis. The Candida albicans fungus exists naturally in small amounts in the vagina, mouth, digestive tract, and on the skin. About 20% of non-pregnant women aged 15–55 harbor Candida albicans in the vagina without any symptoms. Most of the time, the Candida albicans fungus does not cause infection or symptoms because your vagina naturally contains a balanced mix of yeast, including Candida, and bacteria. Certain bacteria (lactobacillus) act to prevent an overgrowth of yeast. Lactobacillus bacteria produce lactic and acetic acid and hydrogen peroxide, maintaining the vaginal pH around 4.5 or less (acidic), which hamper the growth of pathogenic bacteria and Candida albicans, and are thus considered protective against vulvovaginal candidiasis 12, 9. But that balance can be disrupted, resulting in an overgrowth of Candida fungus or penetration of the fungus into deeper vaginal cell layers causing the signs and symptoms of a yeast infection.
Yeast infection can happen if:
- You are taking antibiotics used to treat another infection. Antibiotics change the normal balance between germs in your vagina.
- You are pregnant
- You are overweight or obese
- You have diabetes or uncontrolled diabetes
- You are taking oral contraceptives or hormone therapy that increase estrogen levels. Estrogen causes the lining of the vagina to mature and to contain glycogen, a substrate on which Candida albicans thrives. Symptoms often occur in the second half of the menstrual cycle when there is also more progesterone. Lack of estrogen makes vulvovaginal candidiasis less common in younger and older postmenopausal women.
- You are taking medicines or have an illness that suppresses your immune system.
A yeast infection is not spread through sexual contact and is not a sexually transmitted infection (STI) and many people already have a small amount of Candida in their bodies before they have sexual contact with a partner. However, sexual activity can worsen thrush and the infection can make sex uncomfortable. Furthermore, some men may develop symptoms after having sexual contact with an infected partner. These symptoms may include itching, rash or irritation of the penis (balanitis and balanoposthitis) 13.
Having many vaginal yeast infections may be a sign of other health problems. Other vaginal infections and discharges can be mistaken for a vaginal yeast infection.
Recurrent vaginal yeast infection
Recurrent vulvovaginal candidiasis, usually defined as three or more episodes of symptomatic vulvovaginal candidiasis in <1 year, affects <5% of women but carries a substantial economic burden 14. Recurrent vulvovaginal candidiasis can be either idiopathic or secondary (related to frequent antibiotic use, diabetes, or other underlying host factors). The pathogenesis of recurrent vulvovaginal candidiasis is poorly understood, and the majority of women with recurrent vulvovaginal candidiasis have no apparent predisposing or underlying conditions. Candida glabrata and other non–albicans Candida species are observed in 10%–20% of women with recurrent vulvovaginal candidiasis 11. Conventional antifungal therapies are not as effective against these non–albicans yeasts as against Candida albicans 15.
Risk factors for developing vaginal yeast infection
Factors that increase your risk of developing a yeast infection include:
- Antibiotic use. Yeast infections are common in women who take antibiotics. Broad-spectrum antibiotics, which kill a range of bacteria, also kill healthy bacteria in your vagina, leading to overgrowth of yeast.
- Increased estrogen levels. Yeast infections are more common in women with higher estrogen levels — such as pregnant women or women taking high-dose estrogen birth control pills or estrogen hormone therapy.
- Uncontrolled diabetes. Women with poorly controlled blood sugar are at greater risk of yeast infections than women with well-controlled blood sugar.
- Impaired immune system. Women with lowered immunity — such as from corticosteroid therapy or HIV infection — are more likely to get yeast infections.
Vaginal yeast infection prevention
To reduce your risk of vaginal yeast infections, wear underwear that has a cotton crotch and doesn’t fit too tightly.
It might also help to AVOID:
- Tight-fitting pantyhose
- Douching, which removes some of the normal bacteria in the vagina that protect you from infection
- Scented feminine products, including bubble bath, pads and tampons
- Hot tubs and very hot baths
- Unnecessary antibiotic use, such as for colds or other viral infections
- Staying in wet clothes, such as swimsuits and workout attire, for long periods of time
To help prevent and treat vaginal discharge:
- Keep your genital area clean and dry. Avoid soap and rinse with water only. Sitting in a warm, but not hot, bath may help your symptoms.
- Avoid douching. Although many women feel cleaner if they douche after their period or intercourse, it may worsen vaginal discharge. Douching removes healthy bacteria lining the vagina that protect you from infection.
- Eat yogurt with live cultures or take Lactobacillus acidophilus tablets when you are on antibiotics. This may help to prevent a yeast infection.
- Use condoms to avoid catching or spreading other infections.
- Avoid using feminine hygiene sprays, fragrances, or powders in the genital area.
- Do not use scented feminine products, including bubble bath, sprays, pads, and tampons.
- Avoid wearing tight-fitting pants or shorts. These can increase body heat and moisture in your genital area.
- Wear cotton underwear or cotton-crotch pantyhose. Cotton underwear helps keep you dry and doesn’t hold in warmth and moisture. Avoid underwear made of silk or nylon. These can increase sweating in the genital area, which leads to growth of more yeast.
- Keep your blood sugar level under good control if you have diabetes.
- Avoid wearing wet bathing suits or exercise clothing for long periods of time. Wash sweaty or wet clothes after each use.
- Change tampons, pads, and panty liners often.
- After using the bathroom, always wipe from front to back.
- Avoid hot tubs and very hot baths.
Vaginal yeast infection signs and symptoms
Vaginal yeast infection symptoms can range from mild to moderate, and include 16, 17:
- Itching and irritation in the vagina and vulva
- A burning sensation, especially during intercourse or while urinating
- Redness and swelling of the skin just outside of the vagina (vulva)
- Vaginal pain and soreness
- Vaginal rash
- Thick, white, odor-free vaginal discharge with a cottage cheese appearance. [Discharge can range from slightly watery, white discharge to thick, white, and chunky (like cottage cheese)]
- Watery vaginal discharge
Complicated yeast infection
You might have a complicated yeast infection if:
- You have severe signs and symptoms, such as extensive redness, swelling and itching that leads to tears, cracks or sores
- You have four or more yeast infections in a year
- Your infection is caused by a less typical type of fungus
- You’re pregnant
- You have uncontrolled diabetes
- Your immune system is weakened because of certain medications or conditions such as HIV infection.
A woman may have diabetes or weak immune system (such as in HIV) if:
- The infection recurs right after treatment
- The yeast infection does not respond well to treatment
Vaginal culture or PCR should be obtained from women with complicated vulvovaginal candidiasis to confirm clinical diagnosis and identify non–albicans Candida. Candida glabrata does not form pseudohyphae or hyphae and is not easily recognized on microscopy. Candida albicans azole resistance is becoming more common in vaginal isolates 18, 19 and non–albicans Candida is intrinsically resistant to azoles; therefore, culture and susceptibility testing should be considered for patients who remain symptomatic.
Vaginal yeast infection complications
A lot of scratching may cause the skin to crack, making you more likely to get a skin infection.
Chronic, persistent vulvovaginal yeast infection may lead to lichen simplex —a thickened, intensely itchy labia majora (the hair-bearing outer lips of the vulva).
Vaginal yeast infection diagnosis
To diagnose a yeast infection, your doctor may:
- Ask questions about your medical history. This might include gathering information about past vaginal infections or sexually transmitted infections.
- Perform a pelvic exam. Your doctor examines your external genitals for signs of infection. Next, your doctor places an instrument (speculum) into your vagina to hold the vaginal walls open to examine the vagina and cervix — the lower, narrower part of your uterus.
- Test vaginal secretions. A small amount of the vaginal discharge is examined using a microscope (best taken four weeks after earlier treatment). This is called a wet mount and KOH test. Your doctor may send a sample of vaginal fluid for culture and testing to determine the type of fungus causing your yeast infection. Identifying the fungus can help your doctor prescribe more effective treatment for the infection that does not get better or for recurrent yeast infections.
- Your doctor may order other tests to rule out other causes of your symptoms. Other tests include culture in Sabouraud chloramphenicol agar or chromagar, the germ tube test, DNA probe testing by polymerase chain reaction (PCR), and spectrometry to identify the specific species of candida.
Researchers debate whether nonalbicans candida species cause disease or not. If nonalbicans candida is detected, the laboratory can perform sensitivity testing using disc diffusion methods to guide treatment. Sensitivity to fluconazole predicts sensitivity to other oral and topical azoles. Candida glabrata is often resistant to standard doses of oral and topical azoles.
Vaginal yeast infection treatment
Treatment for yeast infections depends on the severity and frequency of your infections.
For mild to moderate symptoms and infrequent episodes, your doctor might recommend:
- Short-course vaginal therapy. Taking an antifungal medication for three to seven days will usually clear a yeast infection. Antifungal medications — which are available as creams, ointments, tablets and suppositories — include miconazole (Monistat 3) and terconazole. Some of these medications are available over-the-counter and others by prescription only.
- Single-dose oral medication. Your doctor might prescribe a one-time, single oral dose of fluconazole (Diflucan). Oral medication isn’t recommended if you’re pregnant. To manage more-severe symptoms, you might take two single doses three days apart.
See your doctor again if treatment doesn’t resolve your symptoms or if your symptoms return within two months.
If your symptoms are severe, or you have frequent yeast infections, your doctor might recommend:
- Long-course vaginal therapy. Your doctor might prescribe an antifungal medication taken daily for up to two weeks, followed by once a week for six months.
- Multidose oral medication. Your doctor might prescribe two or three doses of an antifungal medication to be taken by mouth instead of vaginal therapy. However, this therapy isn’t recommended for pregnant women.
- Azole resistant therapy. Your doctor might recommend boric acid, a capsule inserted into your vagina. This medication may be fatal if taken orally and is used only to treat candida fungus that is resistant to the usual antifungal agents. Boric acid (boron) 600 mg as a vaginal suppository at night for two weeks reduces the presence of albicans and non-albicans Candida in 70% of treated women 5, 6. Boric acid can be irritating and is toxic, so should be stored safely away from children and animals. Twice-weekly use may prevent recurrent yeast infections. Boric acid should NOT be used during pregnancy!
Best over the counter yeast infection treatment
Yeast infections are usually treated with antifungal medicine. You can then buy antifungal medicine for yeast infections at a store, without a prescription. Antifungal medicines come in the form of creams, tablets, ointments, or suppositories that you insert into your vagina. You can apply treatment in one dose or daily for up to seven days, depending on the brand you choose.
Short-course topical formulations (i.e., single dose and regimens of 1–3 days) effectively treat uncomplicated vaginal yeast infection. Treatment with azoles results in relief of symptoms and negative cultures in 80%–90% of patients who complete therapy 15.
- Clotrimazole 1% cream 5 g intravaginally daily for 7–14 days
- OR
- Clotrimazole 2% cream 5 g intravaginally daily for 3 days
- OR
- Miconazole 2% cream 5 g intravaginally daily for 7 days
- OR
- Miconazole 4% cream 5 g intravaginally daily for 3 days
- OR
- Miconazole 100 mg vaginal suppository one suppository daily for 7 days
- OR
- Miconazole 200 mg vaginal suppository one suppository for 3 days
- OR
- Miconazole 1,200 mg vaginal suppository one suppository for 1 day
- OR
- Tioconazole 6.5% ointment 5 g intravaginally in a single application
Prescription intravaginal agents
Your doctor can also give you a single dose of antifungal medicine taken by mouth, such as fluconazole. If you get more than four vaginal yeast infections a year, or if your yeast infection doesn’t go away after using over-the-counter treatment, you may need to take regular doses of antifungal medicine for up to six months 15.
- Butoconazole 2% cream (single-dose bioadhesive product) 5 g intravaginally in a single application
- OR
- Terconazole 0.4% cream 5 g intravaginally daily for 7 days
- OR
- Terconazole 0.8% cream 5 g intravaginally daily for 3 days
- OR
- Terconazole 80 mg vaginal suppository one suppository daily for 3 days
Oral agent
- Fluconazole 150 mg orally in a single dose
Severe vaginal yeast infection treatment
Severe vulvovaginal candidiasis (i.e., extensive vulvar erythema, edema, excoriation, and fissure formation) is associated with lower clinical response rates among patients treated with short courses of topical or oral therapy. Either 7–14 days of topical azole or 150 mg of fluconazole in two sequential oral doses (given every 72 hours after initial dose for a total of 2 or 3 doses) is recommended 6.
Recurrent vaginal yeast infection treatment
In about 5–10% of women, Candida albicans infection persists despite adequate conventional therapy. In some women, this may be a sign of iron deficiency, diabetes mellitus or an immune problem, and appropriate tests should be done. The subspecies and sensitivity of the yeast should be determined if treatment-resistance arises.
Recurrent symptoms due to vulvovaginal candidiasis are due to persistent infection, rather than re-infection. Treatment aims to avoid the overgrowth of candida that leads to symptoms, rather than complete eradication.
Most episodes of recurrent vulvovaginal candidiasis caused by Candida albicans respond well to short-duration oral or topical azole therapy. However, to maintain clinical and mycologic control, a longer duration of initial therapy (e.g., 7–14 days of topical therapy or a 100-mg, 150-mg, or 200-mg oral dose of fluconazole every third day for a total of 3 doses [days 1, 4, and 7]) is recommended, to attempt mycologic remission, before initiating a maintenance antifungal regimen 15.
Oral fluconazole (i.e., a 100-mg, 150-mg, or 200-mg dose) weekly for 6 months is the indicated maintenance regimen. If this regimen is not feasible, topical treatments used intermittently can also be considered. Suppressive maintenance therapies are effective at controlling recurrent vulvovaginal candidiasis but are rarely curative long-term 20. Because Candida albicans azole resistance is becoming more common, susceptibility tests, if available, should be obtained among symptomatic patients who remain culture positive despite maintenance therapy. These women should be managed in consultation with a specialist.
The following measures can be helpful:
- Loose-fitting clothing — avoid occlusive nylon pantyhose.
- Soak in a salt bath. Avoid soap — use a non-soap cleanser or aqueous cream for washing.
- Apply hydrocortisone cream intermittently, to reduce itching and to treat secondary dermatitis of the vulva.
- Treat with an antifungal cream before each menstrual period and before antibiotic therapy to prevent relapse.
- A prolonged course of a topical antifungal agent is occasionally warranted (but these may themselves cause dermatitis or result in the proliferation of non-albicans Candida).
- Oral antifungal medication (usually fluconazole), which is taken regularly and intermittently (eg, 150–200 mg once a week for six months). The dose and frequency depend on the severity of symptoms. Relapse occurs in 50% of women with recurrent vulvovaginal candidiasis when they are discontinued, in which case re-treatment may be appropriate. Some women require long-term therapy.
- Oral azoles may require a prescription. Single-dose fluconazole is available over the counter at pharmacies. The manufacturers recommend that fluconazole is avoided in pregnancy.
- Boric acid (boron) 600 mg as a vaginal suppository at night for two weeks reduces the presence of albicans and non-albicans candida in 70% of treated women. It can be irritating and is toxic, so should be stored safely away from children and animals. Twice-weekly use may prevent recurrent yeast infections. Boric acid should not be used during pregnancy.
Non–albicans vulvovaginal candidiasis
Conventional antifungal therapies are not as effective against these non–albicans yeasts as against Candida albicans 15. Because approximately 50% of women with a positive culture for non–albicans Candida might be minimally symptomatic or have no symptoms, and because successful treatment is often difficult, clinicians should make every effort to exclude other causes of vaginal symptoms for women with non–albicans yeast 21. The optimal treatment of non–albicans vulvovaginal candidiasis remains unknown; however, a longer duration of therapy (7–14 days) with a nonfluconazole azole regimen (oral or topical) is recommended 15. If recurrence occurs, 600 mg of boric acid in a gelatin capsule administered vaginally once daily for 3 weeks is indicated 15. This regimen has clinical and mycologic eradication rates of approximately 70% 22. If symptoms recur, referral to a specialist is advised.
Yeast infection while pregnant treatment
You are more likely to get yeast infections during pregnancy than at other times. If you think you have a vaginal yeast infection, it is important to see your healthcare provider to be sure the infection is yeast before trying to treat it on your own. If you have another type of infection, you may need different treatment.
During pregnancy, it’s safe to treat a yeast infection with vaginal creams or suppositories that contain miconazole or clotrimazole 23, 24, 25, 26, 27.
Do NOT take the oral fluconazole tablet to treat a yeast infection during pregnancy. It may cause birth defects 28. Epidemiologic studies indicate a single 150-mg dose of fluconazole might be associated with spontaneous abortion 29 and congenital anomalies; therefore, it should not be used 30. Because of this, the Centers for Disease Control and Prevention (CDC) have posted guidelines for treating vaginal yeast infections in pregnancy and these guidelines recommend topical therapies rather than oral medication 15.
Compromised host
Women with underlying immunodeficiency, those with poorly controlled diabetes or other immunocompromising conditions (e.g., HIV), and those receiving immunosuppression therapy (e.g., corticosteroid treatment) might not respond as well to short-term antifungal therapies. Efforts to correct modifiable conditions should be made, and more prolonged (i.e., 7–14 days) conventional treatment is necessary.
Vaginal Candida colonization rates among women with HIV infection are higher than among women without HIV with similar demographic and risk behavior characteristics, and the colonization rates correlate with increasing severity of immunosuppression 31. Symptomatic vulvovaginal candidiasis is also more frequent among women with HIV infection and similarly correlates with severity of immunodeficiency 32. In addition, among women with HIV, systemic azole exposure is associated with isolation of non–albicans Candida species from the vagina.
Treatment for uncomplicated and complicated vulvovaginal candidiasis among women with HIV infection should not differ from that for women who do not have HIV 15. Although long-term prophylactic therapy with fluconazole 200 mg weekly has been effective in reducing C. albicans colonization and symptomatic vulvovaginal candidiasis 33, this regimen is not recommended for women with HIV infection in the absence of complicated vulvovaginal candidiasis 34. Although vulvovaginal candidiasis is associated with increased HIV seroconversion among HIV-negative women and increased HIV cervicovaginal levels among women with HIV infection, the effect of treatment for vulvovaginal candidiasis on HIV acquisition and transmission remains unknown.
Follow-Up
Follow-up typically is not required. However, women with persistent or recurrent symptoms after treatment should be instructed to return for follow-up visits.
Vaginal yeast infection prognosis
Most of the time, symptoms go away completely with proper treatment.
References- Swidsinski A, Guschin A, Tang Q, Dörffel Y, Verstraelen H, Tertychnyy A, Khayrullina G, Luo X, Sobel JD, Jiang X. Vulvovaginal candidiasis: histologic lesions are primarily polymicrobial and invasive and do not contain biofilms. Am J Obstet Gynecol. 2019 Jan;220(1):91.e1-91.e8. doi: 10.1016/j.ajog.2018.10.023
- Ahangari, F., Farshbaf-Khalili, A., Javadzadeh, Y., Adibpour, M. and Sadeghzadeh Oskouei, B. (2019), Comparing the effectiveness of Salvia officinalis, clotrimazole and their combination on vulvovaginal candidiasis: A randomized, controlled clinical trial. J. Obstet. Gynaecol. Res., 45: 897-907. https://doi.org/10.1111/jog.13918
- Achkar JM, Fries BC. Candida infections of the genitourinary tract. Clin Microbiol Rev. 2010 Apr;23(2):253-73. doi: 10.1128/CMR.00076-09
- Jeanmonod R, Jeanmonod D. Vaginal Candidiasis. [Updated 2022 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459317
- Powell AM, Gracely E, Nyirjesy P. Non-albicans Candida Vulvovaginitis: Treatment Experience at a Tertiary Care Vaginitis Center. J Low Genit Tract Dis. 2016 Jan;20(1):85-9. doi: 10.1097/LGT.0000000000000126
- Peter G. Pappas, Carol A. Kauffman, David R. Andes, Cornelius J. Clancy, Kieren A. Marr, Luis Ostrosky-Zeichner, Annette C. Reboli, Mindy G. Schuster, Jose A. Vazquez, Thomas J. Walsh, Theoklis E. Zaoutis, Jack D. Sobel, Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America, Clinical Infectious Diseases, Volume 62, Issue 4, 15 February 2016, Pages e1–e50, https://doi.org/10.1093/cid/civ933
- Vaginal yeast infections. https://www.womenshealth.gov/a-z-topics/vaginal-yeast-infections
- When Yeast Overgrows: What You Should Know About Vaginal Yeast Infections During Pregnancy. https://mothertobaby.org/baby-blog/when-yeast-overgrows-what-you-should-know-about-vaginal-yeast-infections-during-pregnancy
- Buggio L, Somigliana E, Borghi A, Vercellini P. Probiotics and vaginal microecology: fact or fancy? BMC Womens Health. 2019 Jan 31;19(1):25. doi: 10.1186/s12905-019-0723-4
- Hu H, Merenstein DJ, Wang C, Hamilton PR, Blackmon ML, Chen H, Calderone RA, Li D. Impact of eating probiotic yogurt on colonization by Candida species of the oral and vaginal mucosa in HIV-infected and HIV-uninfected women. Mycopathologia. 2013 Oct;176(3-4):175-81. doi: 10.1007/s11046-013-9678-4
- Mohammed A Farhan, Ahmed M Moharram, Tareq Salah, Omar M Shaaban, Types of yeasts that cause vulvovaginal candidiasis in chronic users of corticosteroids, Medical Mycology, Volume 57, Issue 6, August 2019, Pages 681–687, https://doi.org/10.1093/mmy/myy117
- Reid G, Younes JA, Van der Mei HC, Gloor GB, Knight R, Busscher HJ. Microbiota restoration: natural and supplemented recovery of human microbial communities. Nat Rev Microbiol. 2011;9:27–38. doi: 10.1038/nrmicro2473
- Edwards S. Balanitis and balanoposthitis: a review. Genitourin Med. 1996 Jun;72(3):155-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1195642/pdf/genitmed00009-0009.pdf
- Denning DW, Kneale M, Sobel JD, Rautemaa-Richardson R. Global burden of recurrent vulvovaginal candidiasis: a systematic review. Lancet Infect Dis. 2018 Nov;18(11):e339-e347. https://doi.org/10.1016/S1473-3099(18)30103-8
- Vulvovaginal Candidiasis (VVC). Sexually Transmitted Infections Treatment Guidelines, 2021. https://www.cdc.gov/std/treatment-guidelines/candidiasis.htm
- Gonçalves B, Ferreira C, Alves CT, Henriques M, Azeredo J, Silva S. Vulvovaginal candidiasis: Epidemiology, microbiology and risk factors. Crit Rev Microbiol. 2016 Nov;42(6):905-27. doi: 10.3109/1040841X.2015.1091805
- Sobel JD. Vulvovaginal candidosis. Lancet. 2007 Jun 9;369(9577):1961-71. https://doi.org/10.1016/S0140-6736(07)60917-9
- Marchaim D, Lemanek L, Bheemreddy S, Kaye KS, Sobel JD. Fluconazole-resistant Candida albicans vulvovaginitis. Obstet Gynecol. 2012 Dec;120(6):1407-14. doi: 10.1097/aog.0b013e31827307b2
- Shahid Z, Sobel JD. Reduced fluconazole susceptibility of Candida albicans isolates in women with recurrent vulvovaginal candidiasis: effects of long-term fluconazole therapy. Diagn Microbiol Infect Dis. 2009 Jul;64(3):354-6. doi: 10.1016/j.diagmicrobio.2009.03.021
- Crouss T, Sobel JD, Smith K, Nyirjesy P. Long-Term Outcomes of Women With Recurrent Vulvovaginal Candidiasis After a Course of Maintenance Antifungal Therapy. J Low Genit Tract Dis. 2018 Oct;22(4):382-386. doi: 10.1097/LGT.0000000000000413
- Kennedy MA, Sobel JD. Vulvovaginal Candidiasis Caused by Non-albicans Candida Species: New Insights. Curr Infect Dis Rep. 2010 Nov;12(6):465-70. doi: 10.1007/s11908-010-0137-9
- Sobel JD, Chaim W, Nagappan V, Leaman D. Treatment of vaginitis caused by Candida glabrata: use of topical boric acid and flucytosine. Am J Obstet Gynecol. 2003 Nov;189(5):1297-300. doi: 10.1067/s0002-9378(03)00726-9
- Murase JE, Heller MM, Butler DC. Safety of dermatologic medications in pregnancy and lactation: Part I. Pregnancy. J Am Acad Dermatol. 2014 Mar;70(3):401.e1-14; quiz 415. doi: 10.1016/j.jaad.2013.09.010
- Butler DC, Heller MM, Murase JE. Safety of dermatologic medications in pregnancy and lactation: Part II. Lactation. J Am Acad Dermatol. 2014 Mar;70(3):417.e1-10; quiz 427. doi: 10.1016/j.jaad.2013.09.009
- Daniel S, Rotem R, Koren G, Lunenfeld E, Levy A. Vaginal antimycotics and the risk for spontaneous abortions. Am J Obstet Gynecol. 2018 Jun;218(6):601.e1-601.e7. doi: 10.1016/j.ajog.2018.02.013
- Rotem, R, Fishman, B, Daniel, S, Koren, G, Lunenfeld, E, Levy, A. Risk of major congenital malformations following first-trimester exposure to vaginal azoles used for treating vulvovaginal candidiasis: a population-based retrospective cohort study. BJOG 2018; 125: 1550– 1556. https://doi.org/10.1111/1471-0528.15293
- Miconazole | Clotrimazole. https://mothertobaby.org/fact-sheets/miconazoleclotrimazole-pregnancy
- Soong D, Einarson A. Vaginal yeast infections during pregnancy. Can Fam Physician. 2009 Mar;55(3):255-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2654841
- Mølgaard-Nielsen D, Svanström H, Melbye M, Hviid A, Pasternak B. Association Between Use of Oral Fluconazole During Pregnancy and Risk of Spontaneous Abortion and Stillbirth. JAMA. 2016;315(1):58–67. doi:10.1001/jama.2015.17844
- Bérard A, Sheehy O, Zhao JP, Gorgui J, Bernatsky S, de Moura CS, Abrahamowicz M. Associations between low- and high-dose oral fluconazole and pregnancy outcomes: 3 nested case-control studies. CMAJ. 2019 Feb 19;191(7):E179-E187. doi: 10.1503/cmaj.180963
- Suzanne E. Ohmit, Jack D. Sobel, Paula Schuman, Ann Duerr, Kenneth Mayer, Anne Rompalo, Robert S. Klein, Longitudinal Study of Mucosal Candida Species Colonization and Candidiasis among Human Immunodeficiency Virus (HIV)-Seropositive and At-Risk HIV-Seronegative Women, The Journal of Infectious Diseases, Volume 188, Issue 1, 1 July 2003, Pages 118–127, https://doi.org/10.1086/375746
- Duerr A, Heilig CM, Meikle SF, Cu-Uvin S, Klein RS, Rompalo A, Sobel JD; HER Study Group. Incident and persistent vulvovaginal candidiasis among human immunodeficiency virus-infected women: Risk factors and severity. Obstet Gynecol. 2003 Mar;101(3):548-56. doi: 10.1016/s0029-7844(02)02729-1
- Jose A. Vazquez, Grace Peng, Jack D. Sobel, Lynn Steele-Moore, Paula Schuman, William Holloway, James D. Neaton, Terry Beirn Community Programs for Clinical Research on AIDS (CPCRA), Evolution of Antifungal Susceptibility among Candida Species Isolates Recovered from Human Immunodeficiency Virus—Infected Women Receiving Fluconazole Prophylaxis, Clinical Infectious Diseases, Volume 33, Issue 7, 1 October 2001, Pages 1069–1075, https://doi.org/10.1086/322641
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, AIDSinfo. https://clinicalinfo.hiv.gov/en/news/updates-guidelines-use-antiretroviral-agents-adults-and-adolescents-hiv-3