Vein of Galen malformation
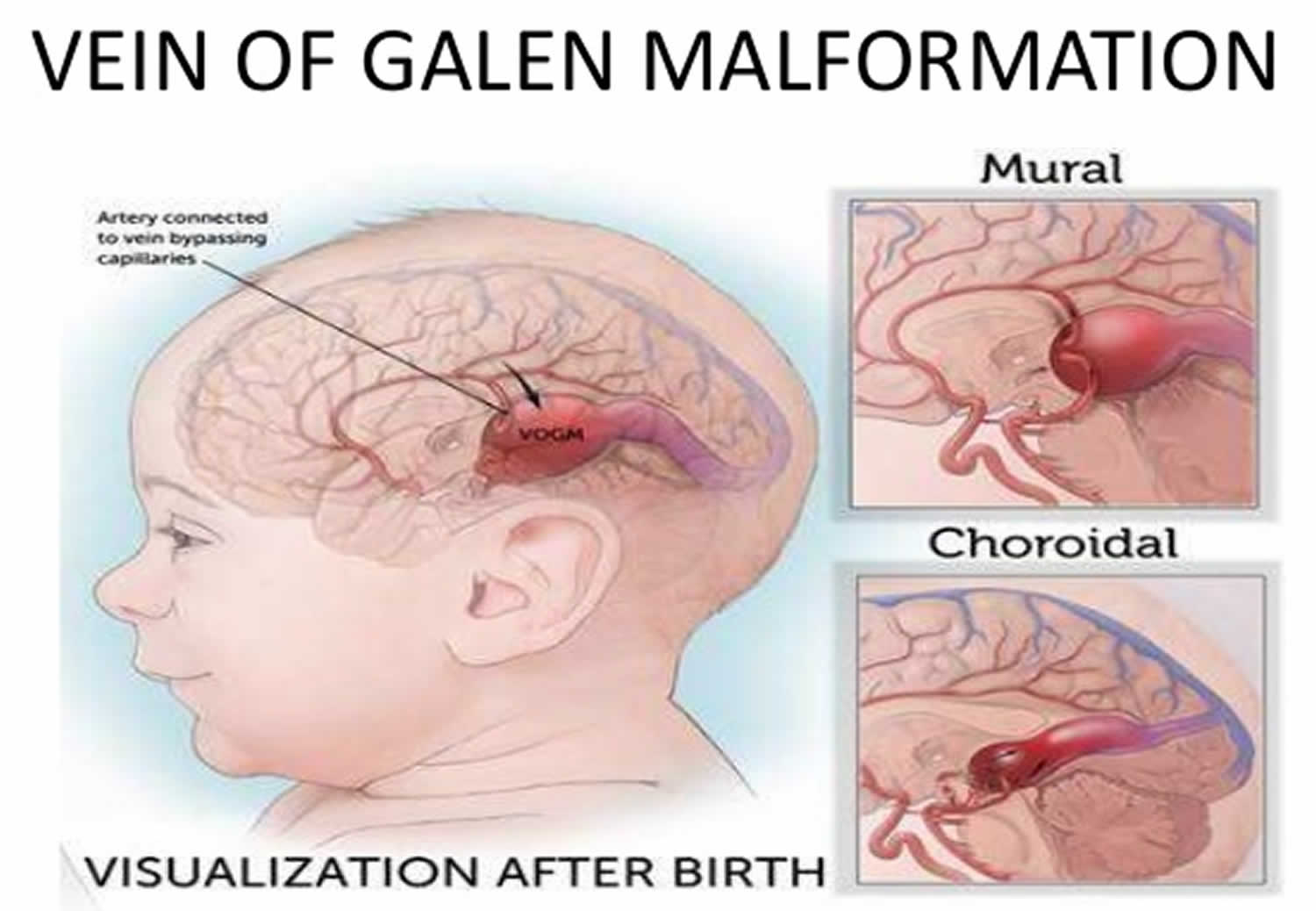
Vein of Galen malformation also called vein of Galen aneurysmal malformation, is a rare form of arteriovenous malformation (abnormal network of arteries and veins) located deep within the brain, in which the embryonic precursor to the vein of Galen, a vein at the base of the brain dilates causing too much blood to rush to the heart and brain. This can lead to rapid heart failure, spontaneous bleeding in the brain, or seizures. In a patient with a vein of Galen malformation, some of the tiny capillaries that normally distribute oxygen-rich blood throughout the brain are missing. Since those capillaries intercept blood coming in from an artery and slow down the flow of blood back to the heart, when they’re missing or malformed the blood rushes into the vein of Galen with too much force and little resistance to flow. This causes a rush of high-pressure blood into the veins. This relative lack of resistance sometimes leads to overworking of the heart, with the potential of heart failure. The increased blood flow into the veins can also disrupt the normal balance between cerebrospinal fluid (CSF) production and absorption, resulting in hydrocephalus. Other complications might include brain dysfunction, with developmental delay, spontaneous bleeding in the brain, or seizures.
This extra pressure in the veins can cause a number of problems:
- The rush of blood toward the heart and lungs forces the heart to work overtime to get blood to the rest of the body. This can lead to congestive heart failure in some infants.
- Blood pressure in the arteries from the heart to the lungs may rise, causing a serious condition called pulmonary hypertension.
- The high pressure in the veins can prevent the infant’s brain from draining adequately. This can lead to widespread brain injury and sometimes causes severe loss of tissue in the brain.
- Some infants can develop hydrocephalus (an enlarged head) if the VOGM blocks the normal flow of fluid in the brain.
Vein of Galen malformation consists of a saccular dilatation of the vein of Galen pooling blood shunted directly from abnormally enlarged cerebral arteries and often causing congestive heart failure, hypoxic respiratory failure, and/or persistent pulmonary hypertension of the newborn 1. Other features may include increased head circumference resulting from hydrocephalus, unusually prominent veins on the face and scalp, developmental delay, persistent headache, and other neurological findings 2. Patients with vein of Galen malformation can sometimes be diagnosed before birth while others are discovered later in childhood. Early diagnosis is essential in order to preserve and protect neurologic function and organ development.
Vein of Galen arteriovenous malformations account for less than 1% of the arteriovenous malformations (AVMs) which are estimated to be seen in only 2.5 out of 100,000 live births 3. It is also the most common antenatally-diagnosed intracranial vascular malformation. There may be an increased male predilection 4.
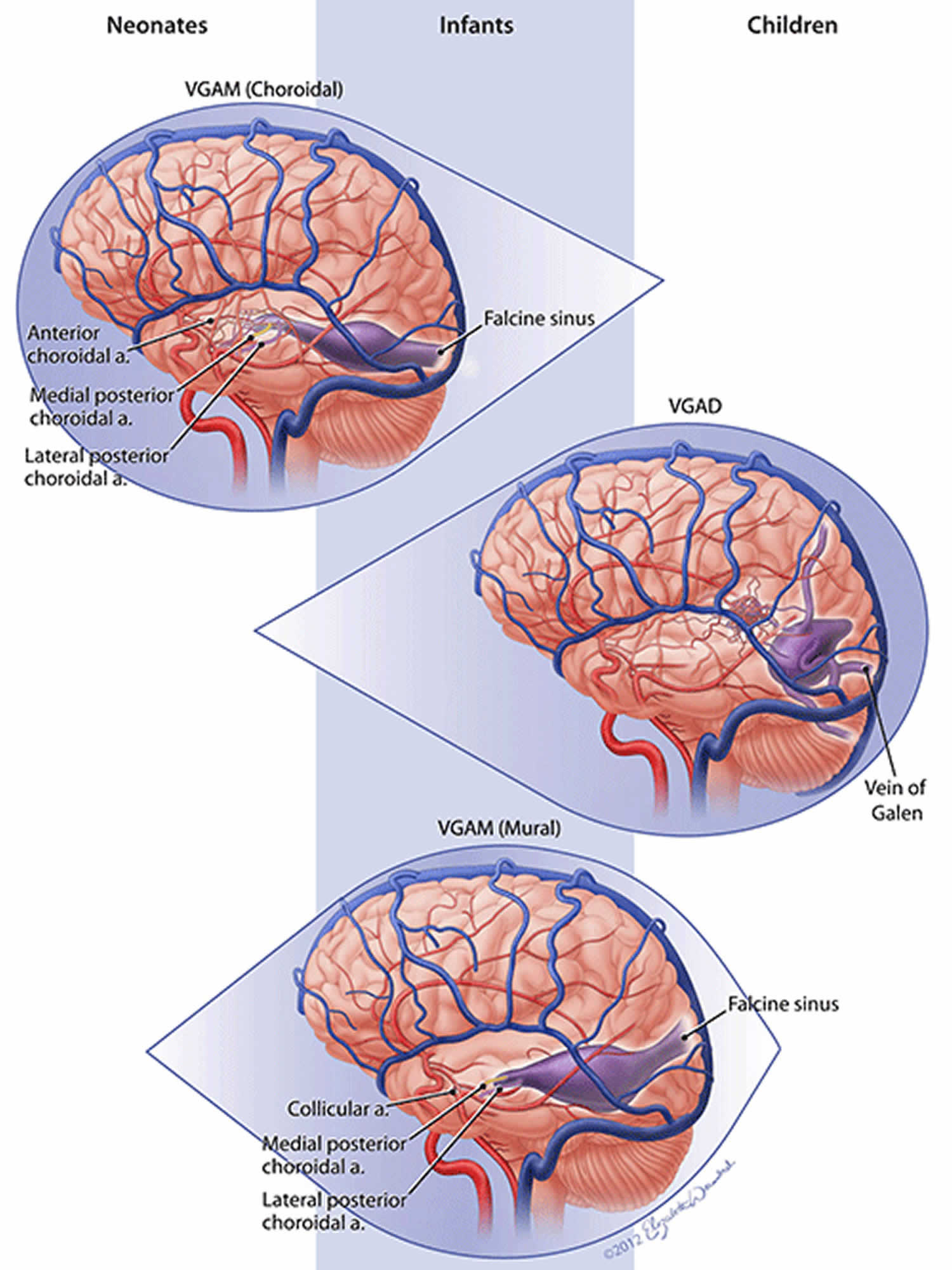
Increasingly the diagnosis of vein of Galen malformation is being made antenatally with third-trimester antenatal ultrasound. Presentation is often with high-output cardiac failure in the neonatal period, although low-flow aneurysms may remain undetected into adulthood. As much as 80% of cardiac output may shunt through the fistula. The presentation does, however, vary with the type of malformation, and different types present at different ages:
- Neonate
- usually choroidal type
- high output cardiac failure
- cranial bruit
- Infant
- usually mural type
- hydrocephalus may occur due to venous hypertension or aqueduct stenosis
- Child
- usually mural type
- developmental delay
- hydrocephalus
When a vein of Galen malformation is apparent on a prenatal ultrasound or at birth, the condition is usually more serious and has a higher likelihood of heart failure. Older babies and children found to have vein of Galen malformation have a more optimistic prognosis, with mild or moderate neurological impairment and manageable symptoms.
A vein of Galen malformation can be fatal, but the prognosis has greatly improved with newer endovascular techniques performed by highly trained experts.
There are a variety of approaches used to treat vein of Galen malformations and most involve a catheter based approach. With the advancement of these techniques it is quite rare that open surgery is necessary.
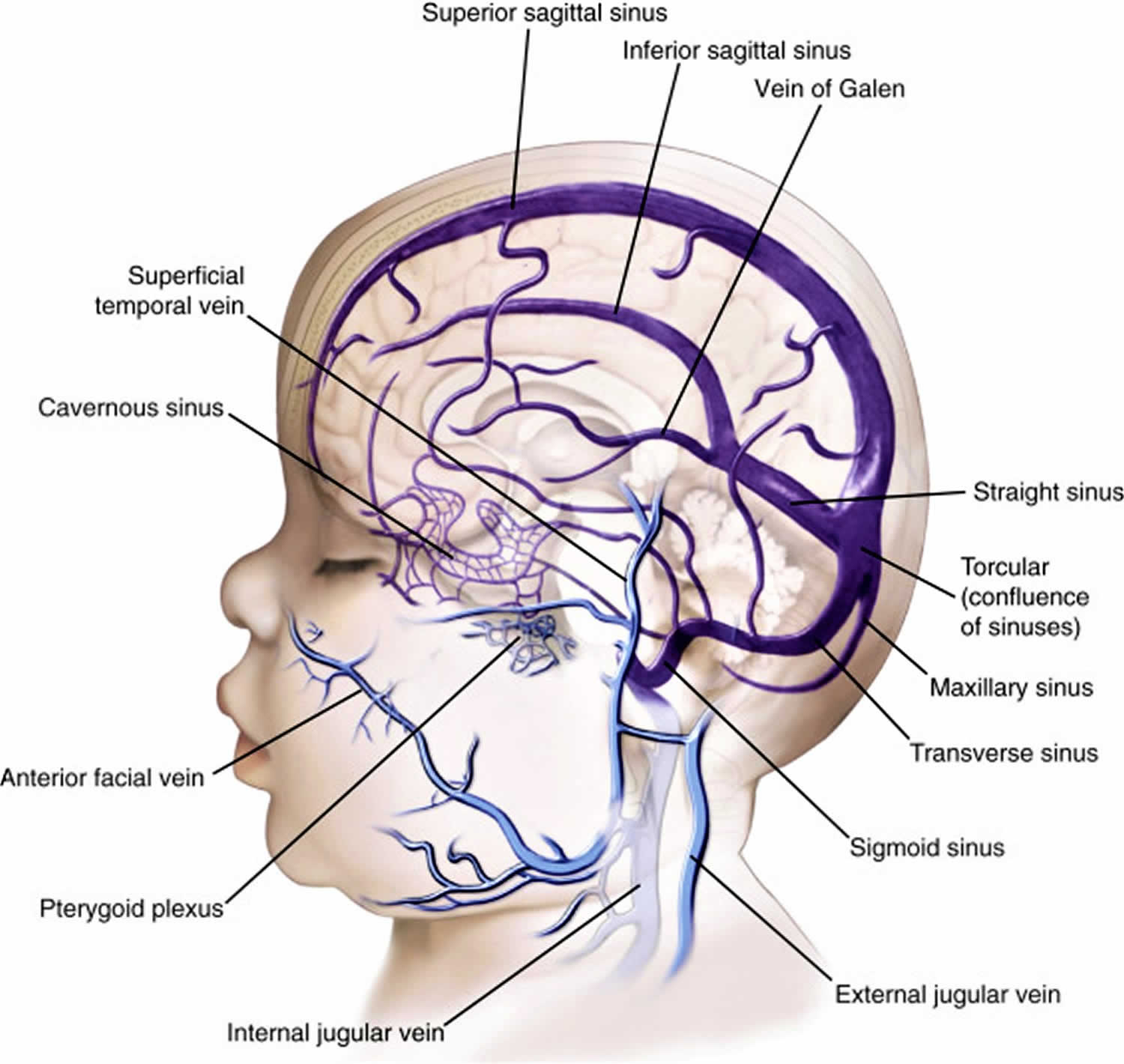
Figure 1. Vein of Galen (also called great cerebral vein) – is one of the large veins that returns blood from the brain to the heart
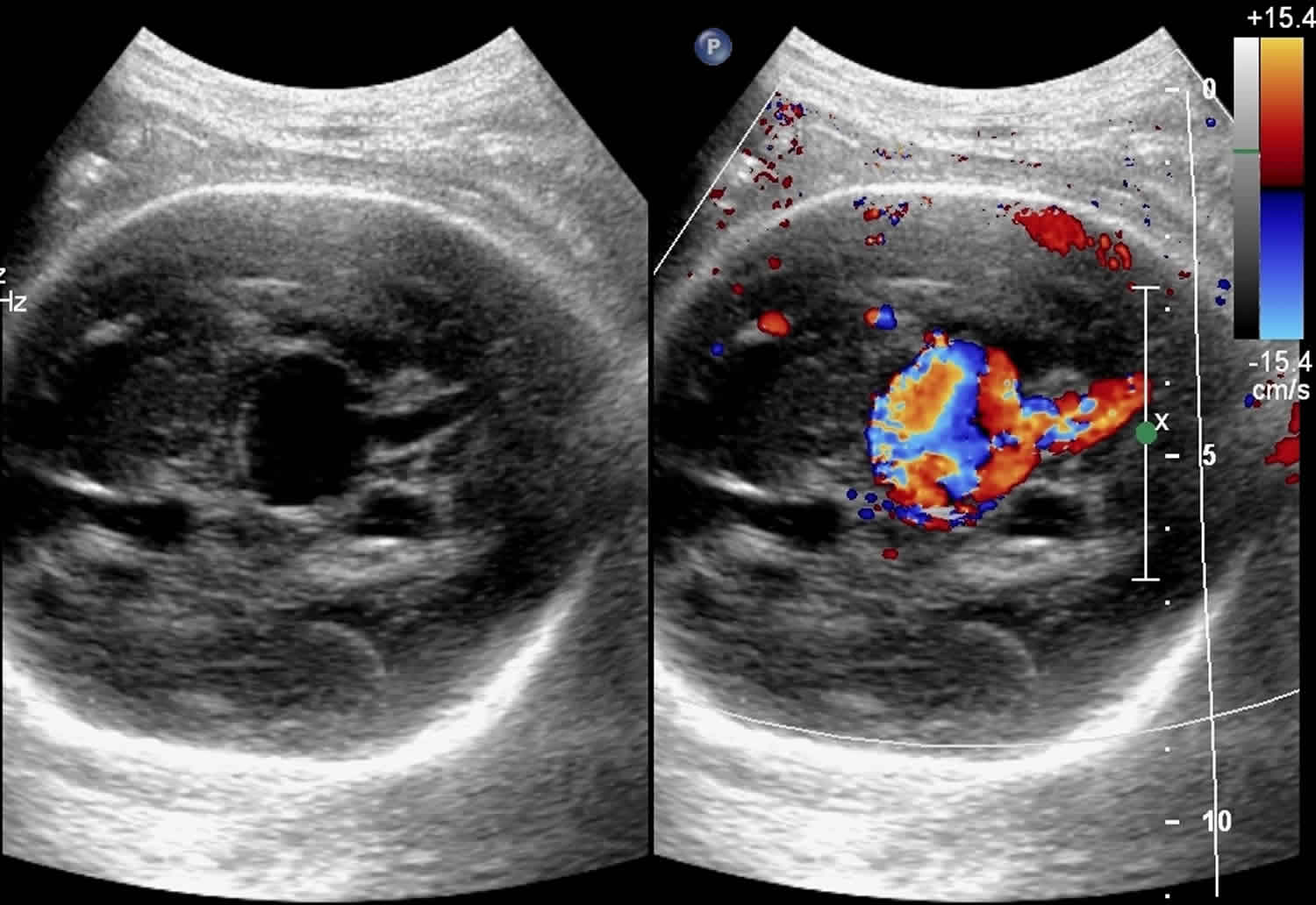
Figure 3. Vein of Galen malformation ultrasound
Footnote: A 22 year old primigravida with 8 months of amenorrhea was referred for antenatal ultrasound examination. This was her first fetal ultrasound. The fetus corresponded to 31 weeks gestational age by fetal biometry. Antenatal ultrasound of shows a supratentorial, midline, anechoic, cystic tubular structure which shows evidence of color uptake and drainage into straight sinus giving the classic appearance of “comet tail” or “keyhole” sign. Feeding vessels are seen from the circle of Willis mainly from the right internal carotid artery and right posterior communicating artery. Venous drainage is via the straight sinus and then by the transverse and sigmoid sinus and internal jugular veins, mainly through right side. The neck vessels, right internal carotid artery and internal jugular vein are dilated. Superior vena cava is also dilated. High velocity, low resistance flow is noted in the circle of Willis and the aneurysm with high volume venous flow through the draining sinuses and right internal jugular vein. The findings are diagnostic of vein of Galen aneurysmal malformation. There was no evidence of fetal cardiomegaly. No evidence of fetal skin edema, pericardial effusion, pleural effusion or ascites to suggest hydrops fetalis which is the most severe complication of this condition.
[Source 5 ]What causes vein of Galen malformation
A vein of Galen malformation develops in a fetus in the first trimester of pregnancy for reasons that are not clear, but it is likely to be genetic in origin. Regardless of the cause, familial transmission or inheritance does not happen. Vein of Galen malformation sometimes, but not always, occurs with vascular anomalies that affect other parts of the body. They generally are not inherited.
Vein of Galen malformation can sometimes be seen on an ultrasound later in the pregnancy, but it’s more commonly diagnosed in a newborn or young child.
Vein of Galen malformation symptoms
Symptoms of a vein of Galen malformation usually begin shortly after birth or during early childhood.
Common symptoms may include:
- heart failure, often within the first day or two of life
- hydrocephalus, or an enlarged head
- unusually prominent veins on the face and scalp
- developmental delays
- persistent headache
- in very rare cases, a bleed in the brain
Vein of Galen malformation diagnosis
A vein of Galen malformation can sometimes be seen on a fetal ultrasound. Ultrasound in the prenatal period often demonstrates the first view of vein of Galen malformation (see Figure 3). Vein of Galen malformation may also be suspected in a newborn with respiratory distress or signs of heart failure and whose echocardiogram does not show any structural heart abnormality. It may also be suspected in an older baby or child who shows the symptoms of a vein of Galen malformation.
Abnormalities in other organs systems (heart, kidney, liver and lung) are often clues that lead to the diagnosis as well but cerebral angiography is the mainstay of diagnosis and classification.
A definite diagnosis can be made with imaging tests:
- A cranial ultrasound is a noninvasive imaging test that allows a neurosurgeon to see the location of an abnormality in the brain.
- Computerized tomography (CT) and magnetic resonance imaging (MRI) scans, which are also noninvasive procedures, can produce detailed images of the brain. CT scans use X-rays and MRI scans use magnetic fields and radio-frequency waves to create images of the brain, but they cannot by themselves see the details of a vein of Galen’s structure, which are best seen on an angiogram.
- A catheter angiogram (also known as cerebral angiography or cerebral arteriography) is a minimally invasive procedure that can provide a detailed image of blood flow in the brain. To perform an angiogram, a specialist called an interventional radiologist inserts a catheter into a blood vessel and feeds it gently toward the location of the suspected arteriovenous malformation. A special dye called a contrast agent is released through the catheter and makes its way to the malformation. The path of the contrast agent, when viewed on an x-ray, produces a detailed image of the malformation’s structure.
An angiogram may be performed along with a CT or MRI scan for greater detail. CT angiography combines the minimally invasive catheter angiogram with the noninvasive CT scan to provide detailed pictures of the malformation. A magnetic resonance angiogram (MRA) is an MRI combined with an angiogram, which allows the radiologist and neurosurgeon to examine the blood vessels as well as the structures of the brain. CT angiograms and magnetic resonance angiograms provide excellent diagnostic views of a vein of Galen malformation.
Vein of Galen malformation treatment
The goal of treating a vein of Galen malformation is to eliminate or decrease as much of the blood flow through the vein of Galen malformation
as possible, while maximizing the blood supply to the brain. Treatment for a vein of Galen malformation depends on the severity of the condition. Some of the treatments may be:
- Anti-seizure medications to manage convulsions
- A shunt to manage hydrocephalus (see vein of Galen malformation surgery)
- Cardiac management of congestive heart failure
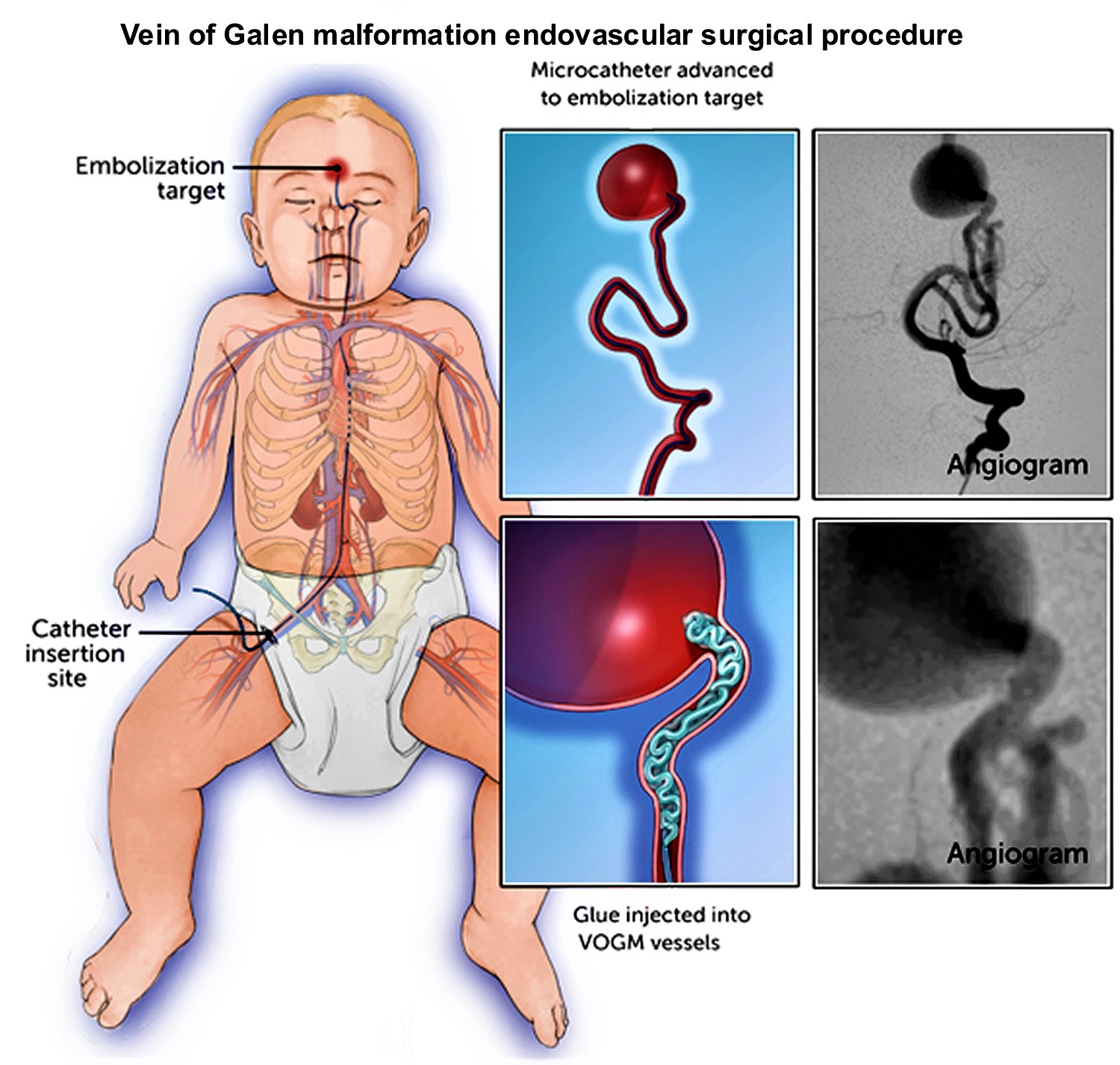
The most common treatment is endovascular embolization, a minimally invasive procedure, is available to treat vein of Galen malformation itself, greatly improving the prognosis. For this procedure, the neurosurgeon inserts a catheter (a thin, flexible tube) into an artery in the child’s groin through a tiny incision. The surgeon guides the catheter up into the brain and injects a special material (such as a type of glue or soft metal coils) into the blood vessels of the vein of Galen malformation to close off the blood flow.
Most children have no pain or other symptoms with embolization, and most are able to leave the hospital within a few days. Some children will need to spend several days in the ICU for observation.
Figure 4. Vein of Galen malformation endovascular surgical procedure
Vein of Galen malformation surgery
In a procedure called endovascular embolization, a neurosurgeon inserts a catheter through an artery or vein in the groin and guides it up the circulatory system to the site of the vein of Galen malformation, where it delivers a kind of liquid material (known as “glue”) and/or specially designed platinum wires (“coils”) that occlude the abnormal connections between arteries and veins and strop abnormal blood flow to the malformed vessel, thus restoring normal circulation. This relatively new technique is a challenging procedure to perform on infants and small children, and it should be performed by a highly trained, experienced expert in cerebrovascular surgery.
In rare cases, a neurosurgeon may also place a shunt in the head to drain away blocked or excess cerebrospinal fluid (CSF) to relieve hydrocephalus. The shunt redirects CSF (cerebrospinal fluid) into the abdomen, where it is reabsorbed into the body. The majority of individuals with vein of Galen malformations do not require this type of treatment for their hydrocephalus. It is preferred to treat the malformation first in the hopes of avoiding any need for a shunt.
Vein of Galen malformation prognosis
Prior to endovascular intervention, vein of Galen malformation prognosis was dismal, with 100% mortality without treatment and 90% mortality following surgical attempts 6.
Ideally, embolization is deferred until 6 months of age for choroidal vein of Galen aneurysmal malformations and later for mural types, to allow the cavernous sinus to mature. If cardiac failure is refractory to medical management, embolization may be performed sooner.
Both venous and arterial embolization is possible, depending on the number of feeders, and controversy persists in regards to the optimal approach. Options include 6:
- Arterial feeder and fistula occlusion
- Transtorcular or transvenous embolization of the dilated vein
- Complete or incomplete occlusion
Both coils and acrylic glue can be used 6.
Radiosurgery has been tried but is limited to patients who are not candidates for other treatment modalities 6.
Hydrocephalus is typically not shunted, as this may exacerbate cerebral ischemia by altering cerebral hemodynamics and due to the increased risk of intraventricular hemorrhage.
The prognosis is determined mainly by the presence or absence of heart failure. Thus choroidal types and those presenting in the neonatal period do poorly.
Vein of Galen malformation life expectancy
Babies with prenatally diagnosed vein of Galen malformation have unexpectedly poor outcomes in the presence of cardiac or cerebral anomalies, while those with strictly isolated vein of Galen malformation tend to have more favorable outcomes. Of 21 cases of prenatally diagnosed vein of Galen malformation, 4 (19.0%) cases were isolated and 17 (81.0%) were associated with other anomalies. There were nine terminations (42.9%) and six neonatal deaths (28.6%) 7.
References- Purdy, I. B, Halnon, N., Singh, N., & Milisavljevic, V. (2010). Vein of Galen arteriovenous malformation with PAPVR and use of serial B-type natriuretic peptide levels in the management: a case report and review of the literature. Cases Journal, 3(1). doi:http://dx.doi.org/10.1186/1757-1626-3-43 Retrieved from https://escholarship.org/uc/item/1354m67b
- Vein of Galen Malformation (VOGM). http://www.childrenshospital.org/conditions-and-treatments/conditions/v/vein-of-galen
- Sasidharan C, Anoop P, Vijayakumar M, Jayakrishnan M, Reetha G, Sindhu T: Spectrum of clinical presentations of vein of galen aneurysm. Indian Journal of Pediatrics 2004, 71:459-463.
- Entezami M, Albig M, Knoll U et-al. Ultrasound Diagnosis of Fetal Anomalies. Thieme. (2003) ISBN:1588902129.
- Vein of Galen aneurysmal malformation.. https://radiopaedia.org/cases/vein-of-galen-aneurysmal-malformation-2
- Vein of Galen Aneurysmal Malformation: Diagnosis and Treatment of 13 Children with Extended Clinical Follow-up Blaise V. Jones, William S. Ball, Thomas A. Tomsick, Justin Millard, Kerry R. Crone American Journal of Neuroradiology Nov 2002, 23 (10) 1717-1724.
- Deloison B, Chalouhi GE, Sonigo P, Zerah M, Millischer AE, Dumez Y, et al. Hidden mortality of prenatally diagnosed vein of Galen aneurysmal malformation: retrospective study and review of the literature. Ultrasound Obstet Gynecol. 2012 Dec. 40 (6):652-8.