Vestibular papillomatosis
Vestibular papillomatosis also known as vestibular papillae are normal anatomical structure of the vulva, which are very small painless, asymptomatic filiform or soft, frond-like projections on the vestibular epithelium or the inner aspect of the labia minora 1. Vestibular papillomatosis or vestibular papillae have a smooth surface and similar color to the adjacent mucosa 2. Although common, vestibular papillomatosis may be unfamiliar to clinicians and may be misdiagnosed as condyloma acuminata (also known as anogenital warts caused by human papillomavirus [HPV]) 3.
Vestibular papillomatosis is considered a normal flexibility in topography and morphology of the vulvar epithelium 4. Prevalence reported in various studies has ranged between 1–33% 5. In past, papillary projections of the inner labia have been overdiagnosed as caused by HPV (human papillomavirus) infection. Careful identification of clinical parameters of vestibular papillomatosis—clusters of pink, soft, uniformly arranged tubular papillae on inner labia, hymen, or periurethral area with round tips, separate bases, and lack of circumscribed whitening on 5% acetic acid application—is diagnostic 6. On the other hand, genital warts or condyloma acuminata are skin-colored or pigmented, randomly arranged, firm, acuminate papules—individual papillary projections fuse at the base—with prominent whitening on 5% acetic acid application 6. The fact that vestibular papillomatosis is distinct from genital warts has also been well-established by polymerase chain reaction (PCR) and in-situ hybridization studies 4.
Vestibular papillomatosis is asymptomatic in majority of affected females, however, vulvar pruritus, pain, burning, and dyspareunia may accompany in some patients 7. Coexisting, vulvar vestibulitis syndrome has also been reported, which is defined as severe pain on vestibular touch or vaginal entry and tenderness located within the vulvar vestibule 8. The feeling of irritation and burning can persist for hours or days following sexual activity, engendering a sense of hopelessness and depression in the patient 8.
A female with vestibular papillomatosis may be referred to a dermatologist for treatment of suspected genital warts. Therefore, it is imperative that clinicians are familiar with this condition in order to avoid unnecessary treatment.
Vestibular papillae key points 9:
- Vestibular papillomatosis is a normal anatomic variation of vulvar mucosa
- Careful identification of clinical appearance – smooth, soft, uniform-sized, small, monomorphic papules on inner labia and vestibule – is diagnostic of vestibular papillomatosis, further aided by acetowhitening test
- It can be an added source of anxiety for a patient with coexisting pain, burning sensation, and vulvar vestibulitis syndrome
- A firm understanding about this condition spares the patient from any unnecessary investigation and treatment.
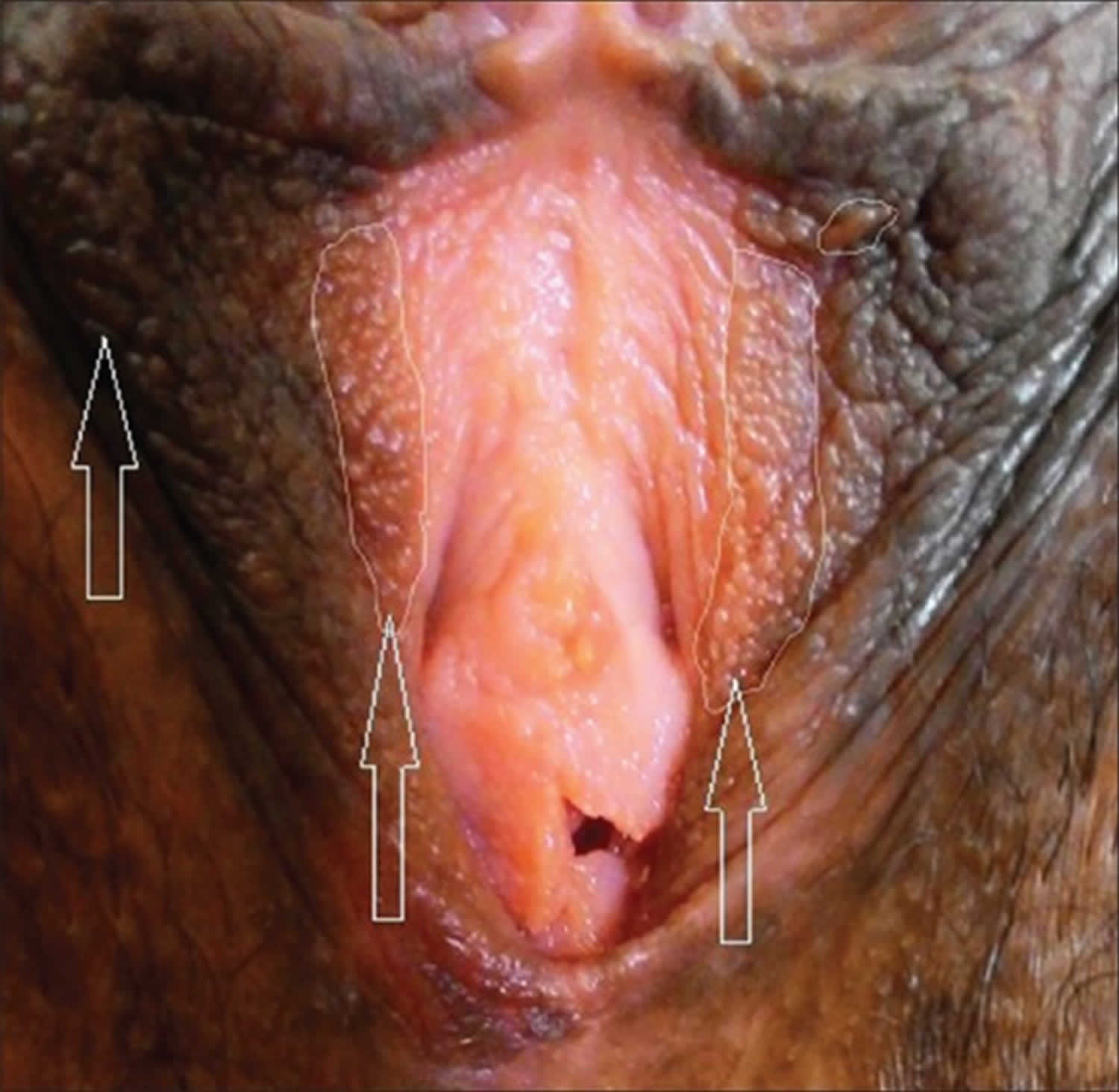
Figure 1. Vestibular papillomatosis
Footnote: Uniformly arranged, monomorphic, symmetric papillae on inner labia and vestibule (arrows and encircled area).
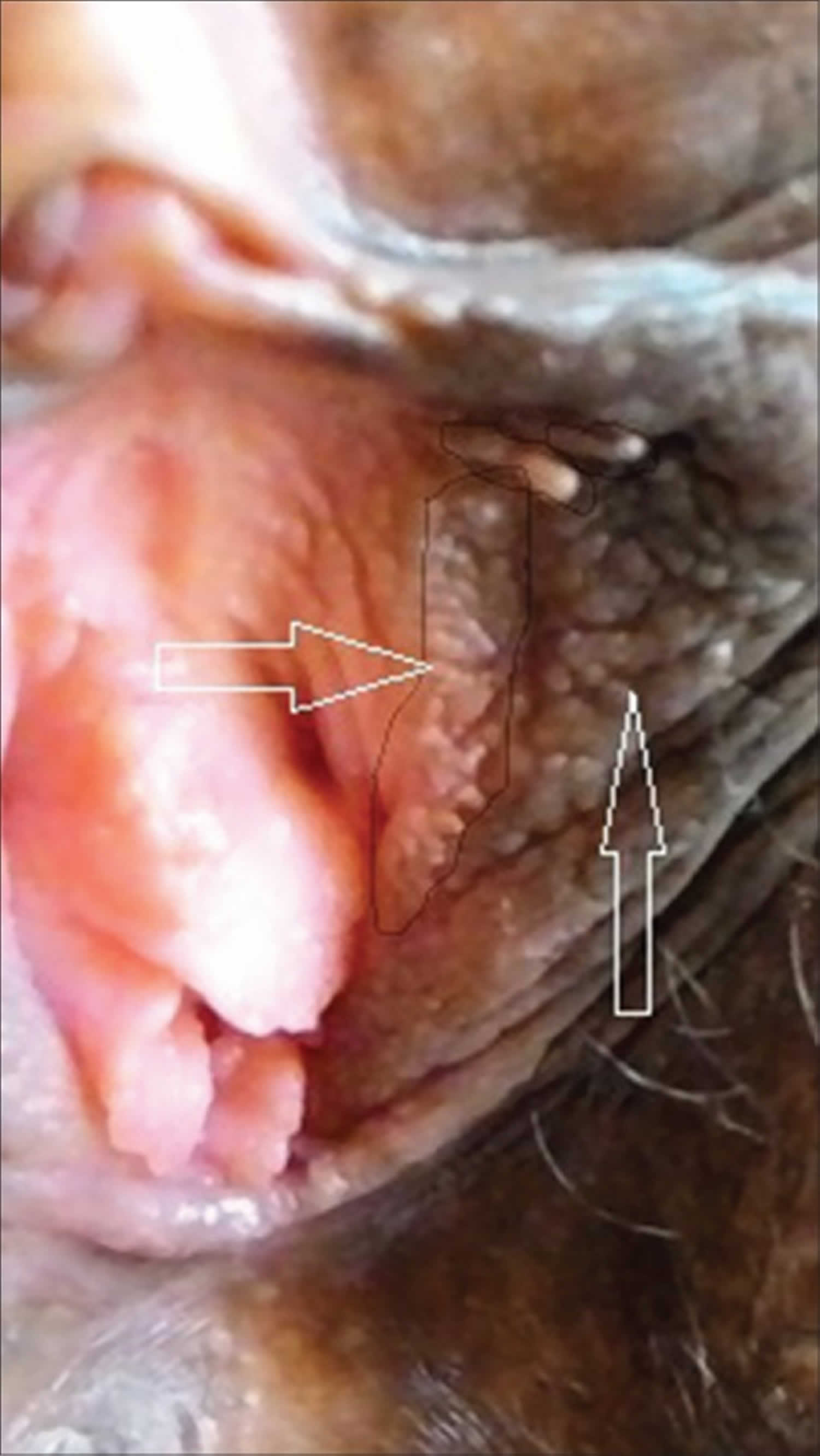
[Source 4 ]Figure 2. Vestibular papillomatosis
Footnote: Vestibular micropapillae with separate bases and symmetric arrangement on inner labia (arrows and encircled area).
[Source 4 ]Vestibular papillomatosis causes
Vestibular papillomatosis also known as vestibular papillae are normal anatomical structure of the vulva, which are very small painless, asymptomatic filiform or soft, frond-like projections on the vestibular epithelium or the inner aspect of the labia minora 1.
Vestibular papillomatosis symptoms
Vestibular papillomatosis also known as vestibular papillae are normal anatomical structure of the vulva, which are very small painless, asymptomatic filiform or soft, frond-like projections on the vestibular epithelium or the inner aspect of the labia minora 1. Vestibular papillomatosis or vestibular papillae have a smooth surface and similar color to the adjacent mucosa 2.
Vestibular papillomatosis is asymptomatic in majority of affected females, however, vulvar pruritus, pain, burning, and dyspareunia may accompany in some patients 7. Coexisting, vulvar vestibulitis syndrome has also been reported, which is defined as severe pain on vestibular touch or vaginal entry and tenderness located within the vulvar vestibule 8. The feeling of irritation and burning can persist for hours or days following sexual activity, engendering a sense of hopelessness and depression in the patient 8.
Vestibular papillomatosis diagnosis
Vestibular papillomatosis are usually diagnosed clinically. Lack of circumscribed whitening on 5% acetic acid application—is diagnostic 6.
Biopsy is sometimes necessary to confirm the diagnosis or exclude viral wart or to diagnose an associated cancer.
Vestibular papillomatosis differential diagnosis
Vestibular papillomatosis are often confused and misdiagnosed with anogenital warts (condyloma acuminata), which are soft growths on the skin and mucous membranes of the anogenital area that is caused by human papillomavirus (HPV). Anogenital warts may be found on the penis, vulva, urethra, vagina, cervix, and around and in the anus. Anogenital warts are spread through sexual contact. Anogenital warts are also called genital warts, venereal warts and squamous cell papilloma.
As anogenital warts are sexually acquired during close skin contact, they are most commonly observed in young adults between the ages of 15 and 30 years. They are highly contagious, and occur in equal numbers in unvaccinated males and females. However, they are rare in people that have been vaccinated against HPV in childhood before beginning sexual activity.
An anogenital wart is a flesh colored papule a few millimeters in diameter. Warts may join together to form plaques up to several centimeters across.
Anogenital warts may occur in the following sites:
- Vulva
- Vagina
- Cervix
- Urethra
- Penis
- Scrotum
- Anus.
Warts due to the same types of HPV can also arise on the lips or within the oral mucosa.
Table 1. Clinical differential diagnosis with vestibular papillae and genital warts (condyloma accuminata)
| Clinical features | Vestibular papillomatosis | Genital warts (condyloma accuminata) |
| Distribution | Symmetric or linear | Irregular |
| Palpation | Soft | Hard |
| Color | Pink, same as adjacent mucosa | Pink, white, and red lesions often associated |
| Base | Bases of individual projections remain separate | Superficial projections coalesce in a common base |
| Acetic acid test | No circumscribed whitening | Whitening in most cases |
Visible genital warts and subclinical HPV infection nearly always arise from direct skin to skin contact.
- Sexual contact. This is the most common way amongst adults.
- Transmission is more likely from visible warts than from subclinical HPV infection.
- Oral sex. HPV appears to prefer the genital area to the mouth however.
- Vertical (mother to baby) transmission through the birth canal.
- Auto (self) inoculation from one site to another.
- Fomites (i.e., from objects like bath towels). It remains very controversial whether warts can spread this way.
Often, warts will appear three to six months after infection but they may appear months or even years later.
Transmission of warts to a new sexual partner can be reduced but not completely prevented by using condoms. Condoms do not prevent all genital skin-to-skin contact, but they also protect against other sexually transmitted diseases (STDs).
Successful treatment of the warts decreases the chance of passing on the infection.
Genital warts are usually diagnosed clinically.
Biopsy is sometimes necessary to confirm the diagnosis or viral wart or to diagnose an associated cancer.
In some circumstances, researchers and clinicians may wish to confirm the presence or absence of HPV. One commercially available qualitative test for HPV is the COBAS 4800 Human Papillomavirus (HrHPV) Test, which evaluates 14 high-risk (HR oncogenic) HPV types. A negative test excludes high-risk infection.
Genital warts treatment
The primary goal of genital wart treatment is to eliminate warts that cause physical or psychological symptoms such as:
- Pain
- Bleeding
- Itch
- Embarrassment.
Options include:
- No treatment
- Self-applied treatments at home
- Treatment at a doctor’s surgery or medical clinic.
The underlying viral infection may persist after the visible warts have cleared. Warts sometimes re-emerge years later because the immune system has weakened.
Self-applied treatments
To be successful the patient must identify and reach the warts, and follow the application instructions carefully. Available treatments include:
- Podophyllotoxin solution or cream
- Imiquimod cream
- Sinecatechins ointment.
Treatment at the clinic
In-clinic treatments include:
- Cryotherapy
- Podophyllin resin
- Trichloroacetic acid applications
- Electrosurgery
- Curettage and scissor or scalpel excision
- Laser ablation
- 5% fluorouracil cream.
Experimental therapies for genital warts include:
- Interferon
- 5-fluorouracil/epinephrine-gel implant
- Cidofovir.
Vestibular papillomatosis treatment
Vestibular papillomatosis or vestibular papillae are normal anatomical structure of the vulva, therefore no treatment is required. However, a female with vestibular papillomatosis may be referred to a dermatologist for treatment of suspected genital warts.
References- Bunker CB, Neill SM. The genital, perianal and umbilical regions. In: Burns DA, Breathnach SM, Cox NH, Griffiths CEM, editors. Rook’s textbook of dermatology, 7th ed, vol. 4. Oxford: Blackwell Publishing; 2004. pp. 53-68.
- Woodruff JD, Friedrich EG Jr. The vestibule. Clin Obstet Gynecol 1985;28:134-41.
- Moyal-Barracco M, Leibowitch M, Orth G. Vestibular papillae of the vulva. Lack of evidence for human papillomavirus etiology. Arch Dermatol 1990;126:1594-8.
- Kakkar S, Sharma PK. Benign vulvar vestibular papillomatosis: An underreported condition in Indian dermatological literature. Indian Dermatol Online J. 2017;8(1):63–65. doi:10.4103/2229-5178.198777 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5297281
- Wollina U, Verma S. Vulvar vestibular papillomatosis. Indian J Dermatol Venereol Leprol. 2010;76:270–2.
- Moyal-Barraco M, Leibowitch M, Orth G. Vestibular papillae of the vulva: Lack evidence for human papillomavirus etiology. Arch Dermatol. 1990;126:1594–8.
- Sarifakioglu E, Erdal E, Gunduz C. Vestibular papillomatosis: Case report and literature review. Acta Dermatol Venereol. 2006;86:177–8.
- Origoni M, Rossi M, Ferrari D, Lillo F, Ferrari AG. Human papillomavirus with co-existing vulvar vestibulitis syndrome and vestibular papillomatosis. Int J Gynaecol Obstet. 1999;64:259–63.
- Kakkar S, Sharma PK. Monomorphic Papillae on Inner Labia and Vulvar Vestibule. Indian J Dermatol. 2016;61(4):460–461. doi:10.4103/0019-5154.185736 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4966415