Wilson’s disease
Wilson’s disease is an inherited genetic disorder associated with abnormal copper metabolism that results in excess storage of copper, primarily in the liver, brain and eyes. The excess copper damages the liver and nervous system. Your body needs a small amount of copper from food to stay healthy; however, too much copper is poisonous. Normally, the liver filters extra copper and releases it into bile. Bile is a fluid made by the liver that carries toxins and wastes out of the body through the gastrointestinal tract. In Wilson’s disease, the liver does not filter copper correctly and copper builds up in the liver, brain, eyes, and other organs. Over time, high copper levels can cause life-threatening organ damage.
Wilson disease is caused by an inherited autosomal recessive mutation, or change, in the ATP7B gene, which means that to develop the disease you must inherit one copy of the defective gene from each parent. If you receive only one abnormal gene, you won’t become ill yourself, but you’re a carrier and can pass the gene to your children.
Wilson’s disease is named after an American neurologist, Alexander Kinnear Wilson, who originally described the disease while working in England in the early part of the 1900’s 1.
Copper is an essential mineral that is absorbed into the body through the diet. It is incorporated into enzymes that play a role in the regulation of iron metabolism, formation of connective tissue, energy production at the cellular level, the production of melanin (skin pigmentation), immune system and the function of the nervous system and brain 2.
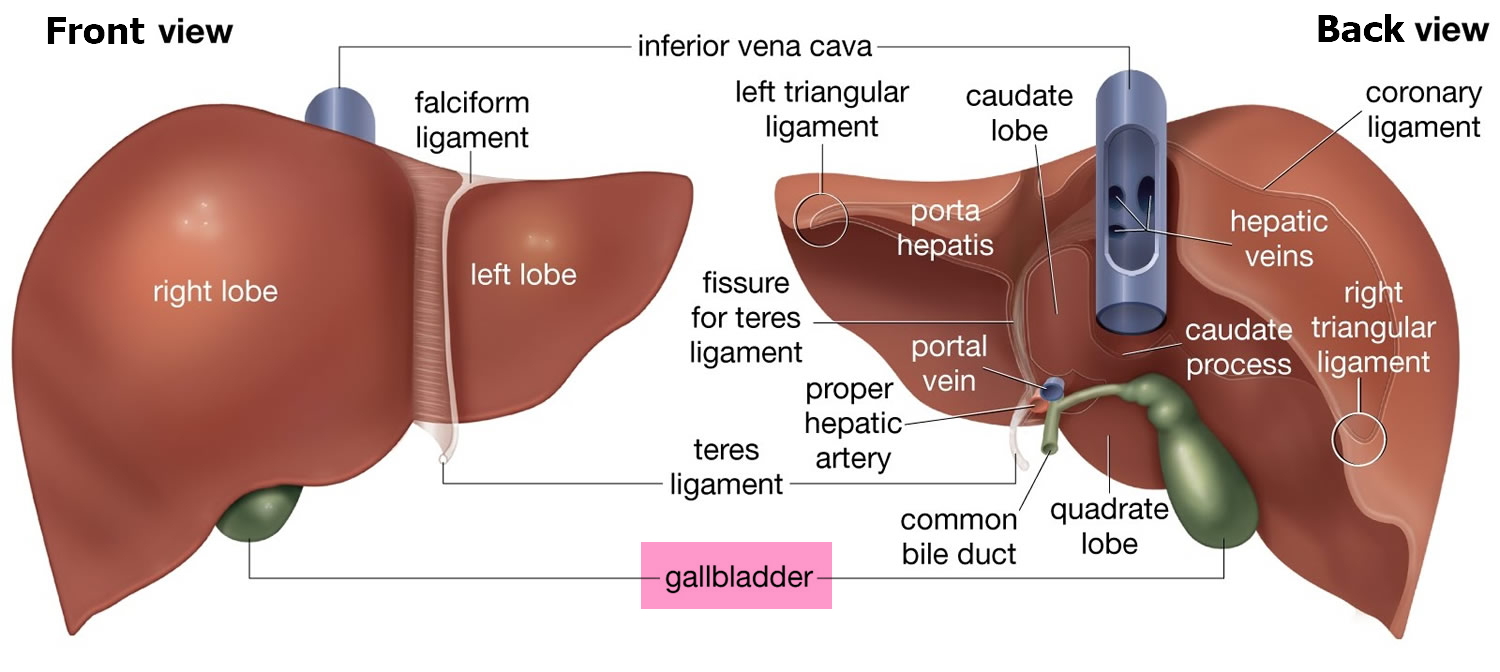
Copper is absorbed in the intestines, bound to a carrier protein, and transported to the liver. The liver stores some of the copper and binds most of the rest to a protein called apoceruloplasmin to produce the enzyme ceruloplasmin (also known as “cuproenzymes” which is a cofactor for several enzymes that play a role in iron metabolism). About 95% of the copper in the blood is bound to ceruloplasmin, and most of the rest is bound to other proteins, such as albumin 3. Only a small amount is normally present in the blood in a free (unbound) state. Excess copper is normally excreted into the bile and removed from the body in the stool. Some copper is also eliminated by the kidneys into the urine. Only small amounts of copper are typically stored in the body, and the average adult has a total body content of 50–120 mg copper 2. Total fecal losses of copper of biliary origin and nonabsorbed dietary copper are about 1 mg/day 4, 2. Copper levels in the body are homeostatically maintained by copper absorption from the intestine and copper release by the liver into bile to provide protection from copper deficiency and toxicity 5.
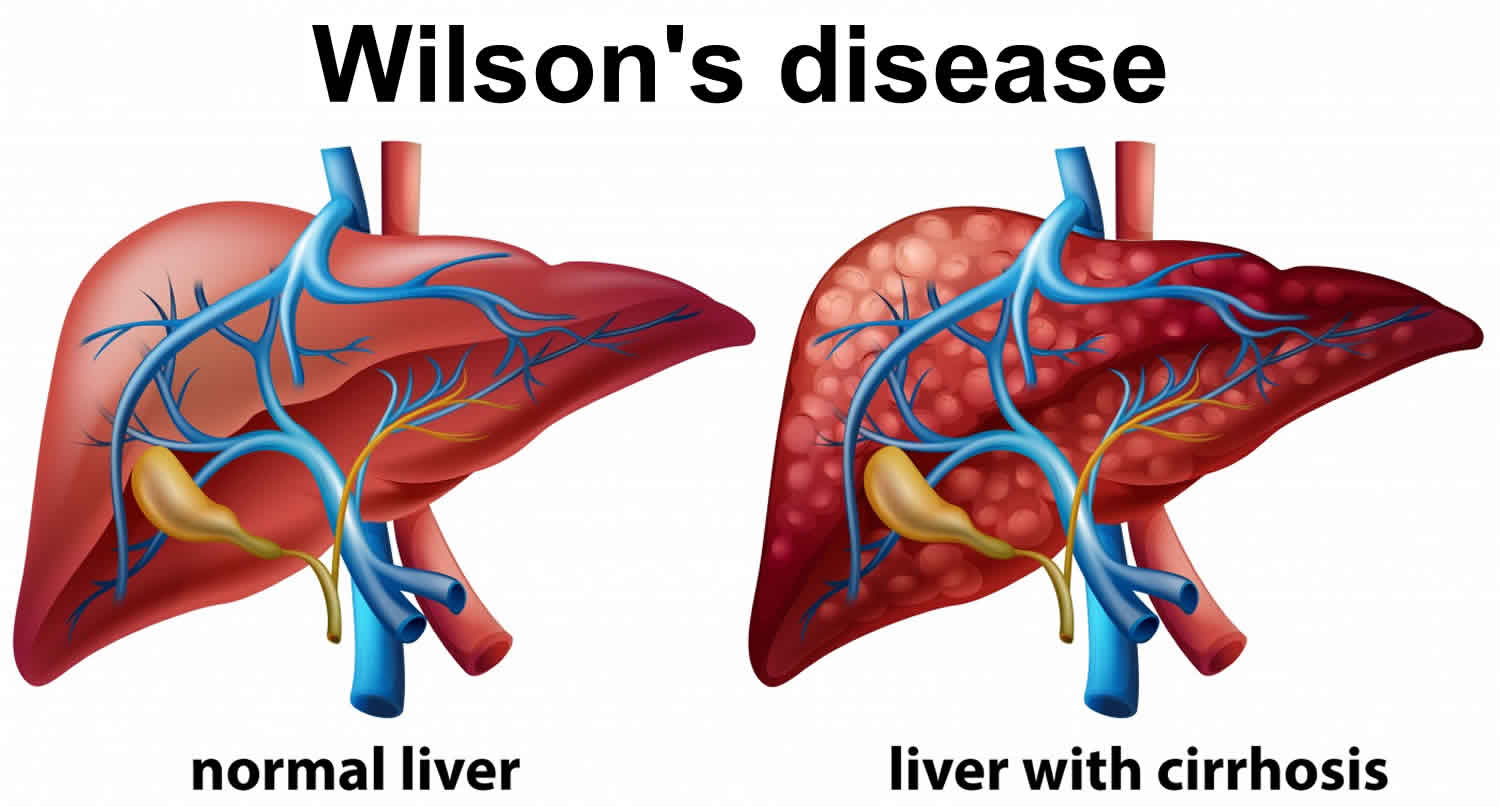
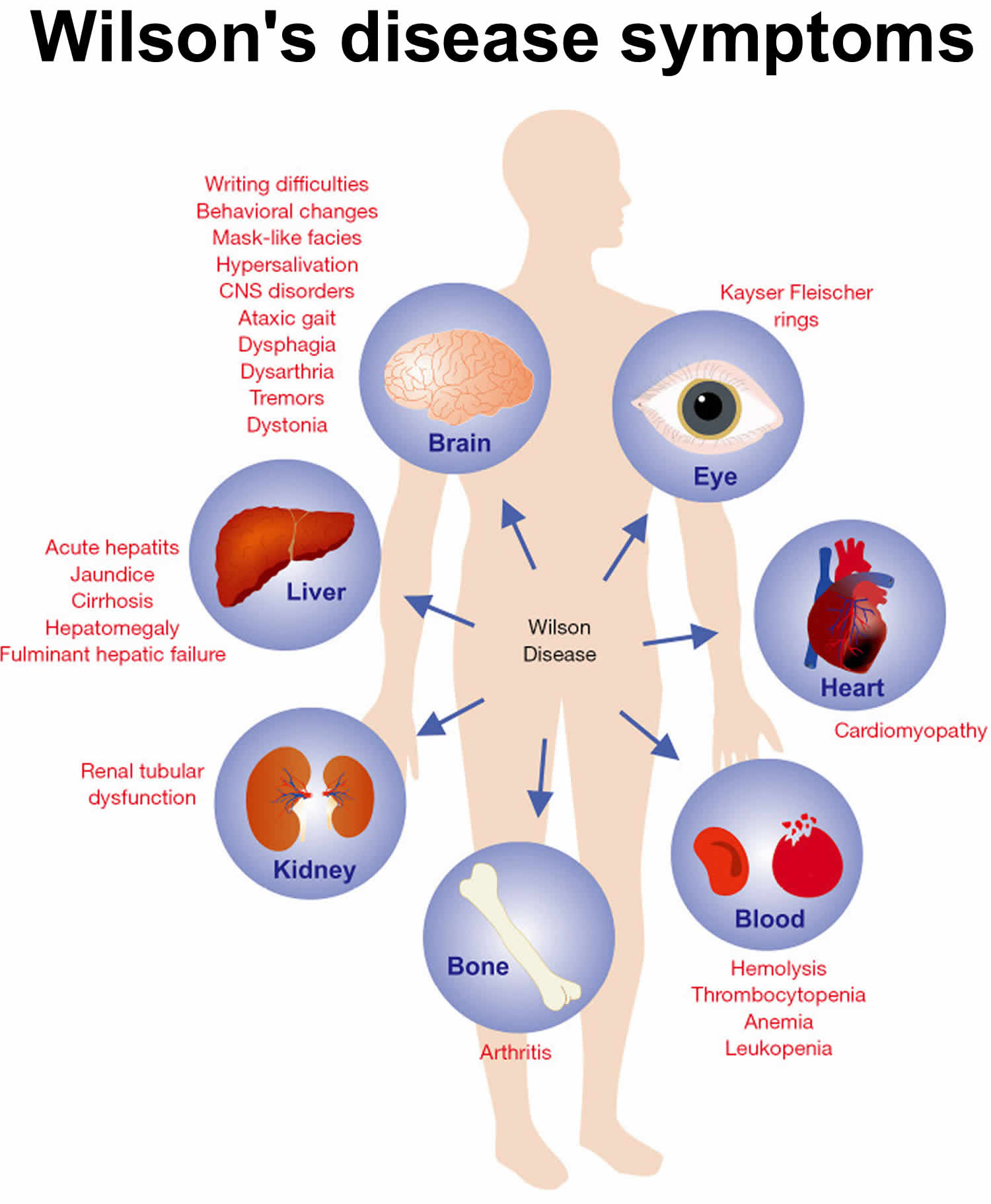
Copper accumulates in the liver and brain, and in other organs, due to greater ingestion than excretion of copper in Wilson’s disease. Excess copper is at first stored in the liver, whose damage presents as hepatitis, liver failure, or chronic cirrhosis 6. With increased levels of circulating non-ceruloplasmin-bound copper (free copper), copper is deposited in other organs. The next most sensitive organ is the brain, in which copper accumulates as non-ceruloplasmin-bound copper (free copper), which can cross the blood-brain barrier 7, 8. Increased copper levels have also been observed in other organs, including the kidneys, eyes, heart, bones, and other organs, resulting in a range of clinical manifestations 9.
The signs and symptoms of Wilson’s disease usually first appear between the ages of 5 and 35, but they most often begin during the teenage years. However, new cases have been reported in people ages 3 to 72 10. About 1 in 30,000 people in the United States have Wilson disease and as many as 1 in 90 are estimated to be carriers. Both males and females are affected equally. There are currently about 40 known normal variants of the ATP7B gene and over 260 different mutations of the ATP7B gene that have been associated with Wilson disease. Only a few of these mutations are common, however, with their prevalence varying with ethnicity throughout the world. Those affected may have two copies of the same genetic mutation or two different mutations.
The features of Wilson’s disease include a combination of liver disease and neurological and psychiatric problems. Liver disease is typically the initial feature of Wilson disease in affected children and young adults; individuals diagnosed at an older age usually do not have symptoms of liver problems, although they may have very mild liver disease. The signs and symptoms of liver disease include yellowing of the skin or whites of the eyes (jaundice), fatigue, loss of appetite, and abdominal swelling.
Deposits of copper in the liver can lead to acute, chronic, and progressive hepatitis and cirrhosis and cause signs and symptoms such as:
- Yellowing of the skin and whites of the eyes (jaundice)
- Fatigue
- Abdominal pain
- Nausea
- Fluid accumulation in the abdomen (ascites)
People whose brain is affected may have a range of physical symptoms, including:
- Muscle contractions that persist and cause limb twitching and repetitive movements (dystonia)
- Stiff face muscles
- Tremors
- Abnormal eye movements
- Altered gait
- Difficulty walking, speaking, and swallowing
They may also experience behavioral changes such as depression, paranoia, impulsiveness, obsessive behavior, aggression, and a shortened attention span.
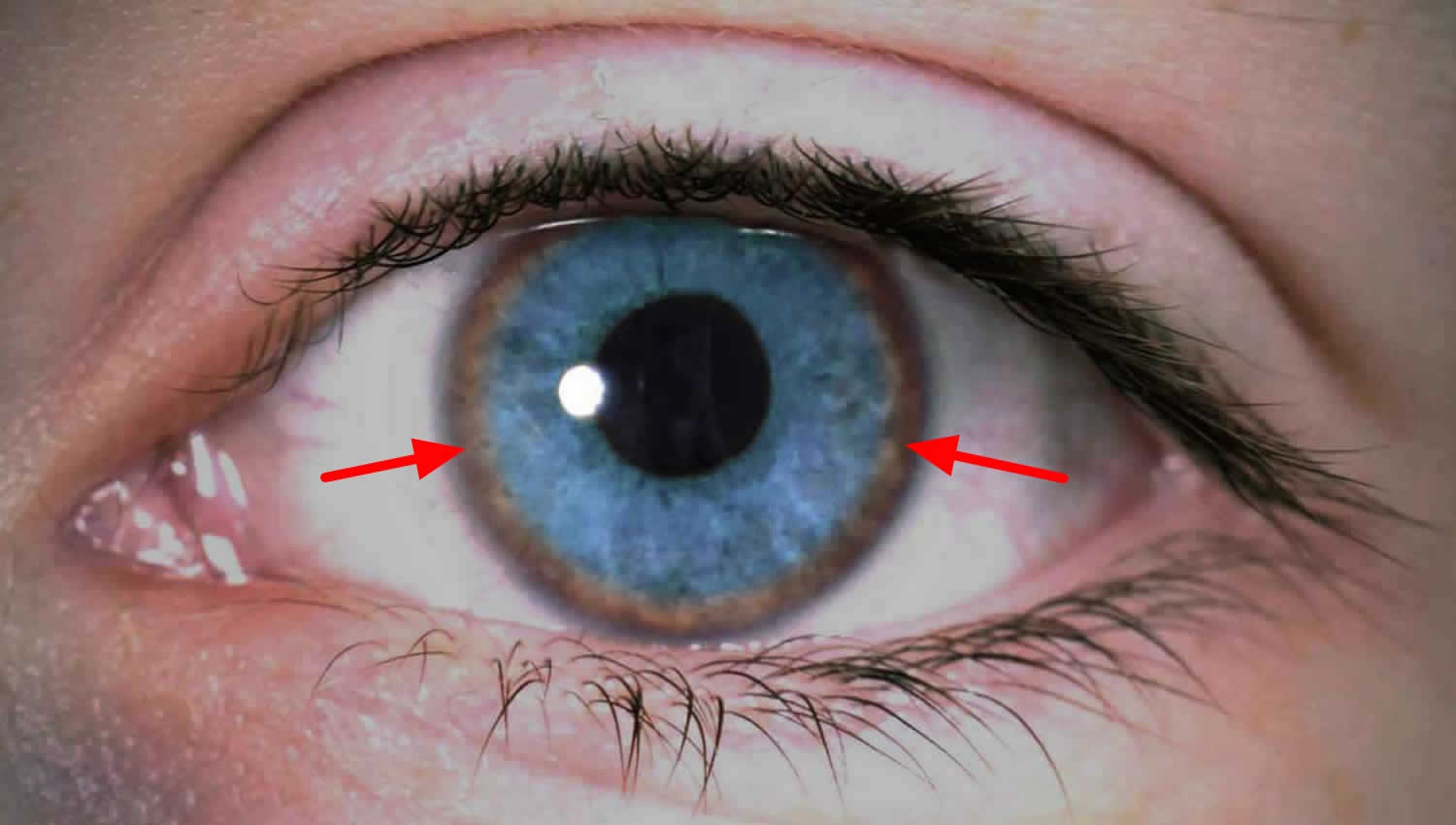
About 50% of those with liver disease and 90% of those with brain involvement will have Kayser-Fleischer rings, deposits of copper in a ring around the cornea that can be seen with an eye exam called a slit lamp examination.
Some with Wilson disease may also experience anemia, easy bruising, joint pain, and/or kidney dysfunction.
Left untreated, Wilson disease tends to become progressively worse and is eventually fatal. With early detection and treatment, most of those affected can live relatively normal lives. Liver and neurologic damage that occurs prior to treatment may improve, but it is often permanent.
Nervous system or psychiatric problems are often the initial features in individuals diagnosed in adulthood and commonly occur in young adults with Wilson disease. Signs and symptoms of these problems can include clumsiness, tremors, difficulty walking, speech problems, impaired thinking ability, depression, anxiety, and mood swings.
In many individuals with Wilson disease, copper deposits in the front surface of the eye (the cornea) form a green-to-brownish ring, called the Kayser-Fleischer ring, that surrounds the colored part of the eye (see Figures 5 and 6 below). Abnormalities in eye movements, such as a restricted ability to gaze upwards, may also occur.
When diagnosed early, Wilson’s disease is treatable, and many people with the disorder live normal lives.
Symptoms, complications, and response to treatment will vary from person to person, even within families who have the same genetic mutations.
In those with symptomatic Wilson disease, the goals of treatment are to decrease excess copper stores, prevent their recurrence, preserve liver, neurological, and kidney function, and minimize complications associated with the condition and associated with the medications used to treat it.
People who are asymptomatic but have been diagnosed as having Wilson disease, such as siblings of affected people, will usually be treated to decrease any excess copper that is present and to prevent its buildup. Those who are carriers of Wilson disease should receive genetic counseling but do not usually require any treatment.
Most people with Wilson disease are treated first with one of two chelating agents, D-penicillamine or trientine (triethylene tetramine dihydochloride), to increase urinary excretion of copper and decrease copper stores. Trientine is preferred because of fewer side effects. D-penicillamine can be used during pregnancy and does not pose any risk to the fetus 11. People with Wilson disease who are treated with chelating agents must be monitored for side effects as the medications can decrease red and white blood cells and platelets and can cause nausea, fever, and skin conditions. Some people must take these medications long-term; others can switch to zinc therapy once copper stores have normalized. High doses of zinc inhibit the absorption of copper.
Those affected are put on a low copper diet. Copper dietary restriction and treatment must be continued throughout a person’s life. Treatments may be changed but should never be discontinued. Untreated Wilson disease is eventually fatal, and organ damage is usually permanent. In some severe cases, liver transplantation may be necessary.
Antioxidants such as vitamin E may be recommended to help prevent liver and other tissue damage.
Figure 1. Kayser-Fleischer ring (the right eye showing a heavily pigmented red brown Kayser-Fleischer ring)
[Source 12 ]Figure 2. Wilson’s disease symptoms
Footnote: In Wilson disease the symptoms are highly variable and can affect liver, brain, kidney, eyes, heart, bone, blood system, and many other organs or tissues.
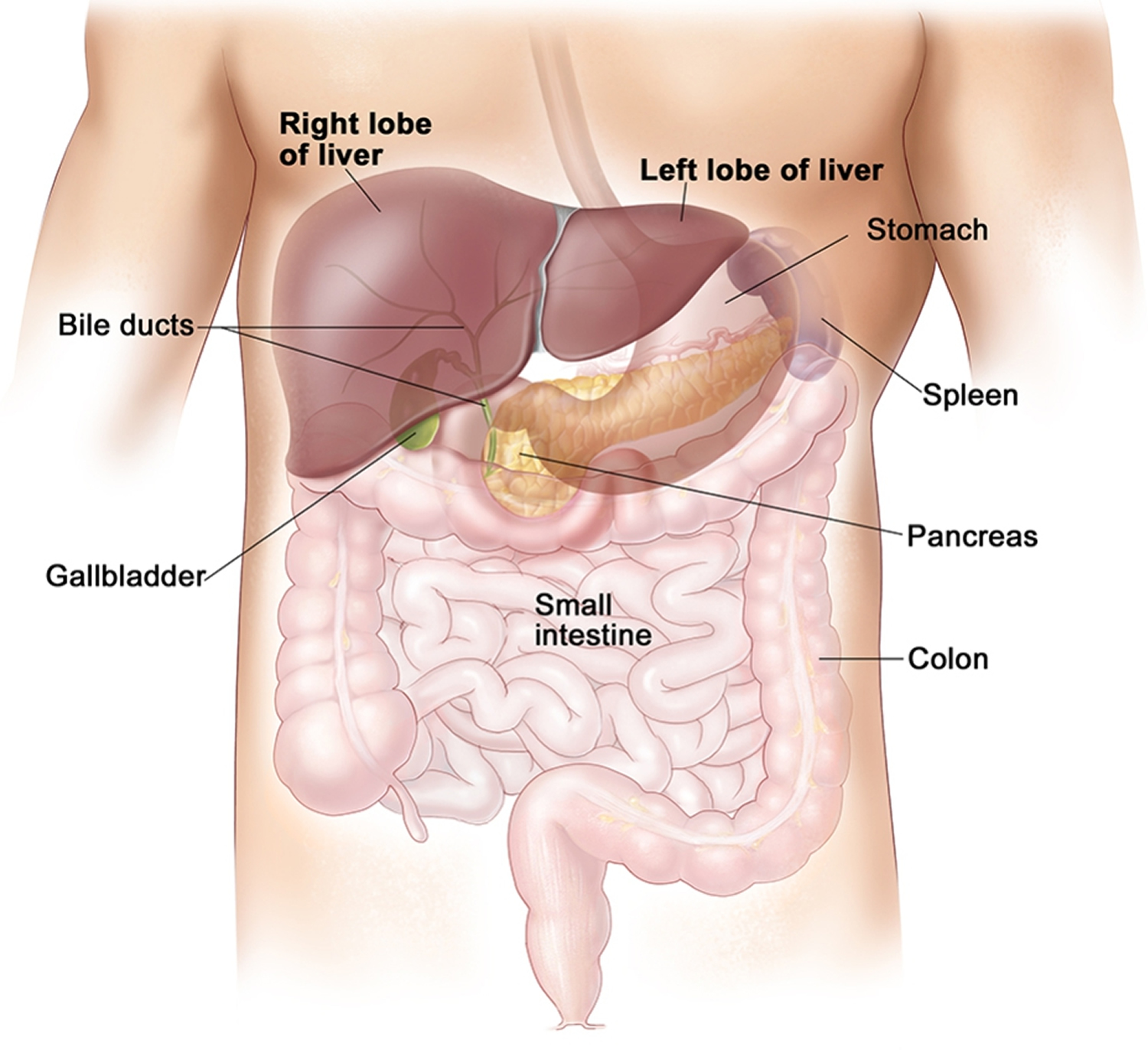
[Source 13 ]What is the liver?
The liver is the body’s largest internal organ. The liver is called the body’s metabolic factory because of the important role it plays in metabolism—the way cells change food into energy after food is digested and absorbed into the blood.
Amazingly versatile, your liver performs over 500 functions. Its digestive function is to produce bile, a green alkaline liquid that is stored in the gallbladder and secreted into the duodenum. Bile salts emulsify fats in the small intestine; that is, they break up fatty nutrients into tiny particles, just as dish detergent breaks up a pool of fat drippings in a roasting pan. These smaller particles are more accessible to digestive enzymes from the pancreas. The liver also performs many metabolic functions and you cannot live without your liver:
- Picks up glucose from nutrient-rich blood returning from the alimentary canal and stores this carbohydrate as glycogen for subsequent use by the body.
- Processes fats and amino acids and stores certain vitamins.
- Detoxifies many poisons and drugs in the blood.
- Makes the blood proteins.
- It breaks down and stores many of the nutrients absorbed from the intestine that your body needs to function. Some nutrients must be changed (metabolized) in the liver before they can be used for energy or to build and repair body tissues.
- It makes most of the clotting factors that keep you from bleeding too much when you are cut or injured.
- It secretes bile into the intestines to help absorb nutrients (especially fats).
- It breaks down alcohol, drugs, and toxic wastes in the blood, which then pass from the body through urine and stool.
Almost all of these functions are carried out by a type of cell called a hepatocyte or simply a liver cell.
The liver carries on many important metabolic activities. The liver plays a key role in carbohydrate metabolism by helping maintain concentration of blood glucose within the normal range. Liver cells responding to the hormone insulin lower the blood glucose level by polymerizing glucose to glycogen. Liver cells responding to the hormone glucagon raise the blood glucose level by breaking down glycogen to glucose or by converting noncarbohydrates into glucose.
The liver’s effects on lipid metabolism include oxidizing (breaking down) fatty acids at an especially high rate; synthesizing lipoproteins, phospholipids, and cholesterol; and converting excess portions of carbohydrate molecules into fat molecules. The blood transports fats synthesized in the liver to adipose tissue for storage.
Other liver functions concern protein metabolism. They include deaminating amino acids; forming urea; synthesizing plasma proteins such as clotting factors; and converting certain amino acids into other amino acids.
The liver also stores many substances, including glycogen, iron, and vitamins A, D, and B12. In addition, macrophages in the liver help destroy damaged red blood cells and phagocytize foreign antigens. The liver also removes toxic substances such as alcohol and certain drugs from blood (detoxification).
A healthy liver is necessary for survival. The liver can regenerate most of its own cells when they become damaged. However, if injury to the liver is too severe or long lasting, regeneration is incomplete and the liver creates scar tissue.
Figure 3. Location of the human liver
Figure 4. Liver anatomy
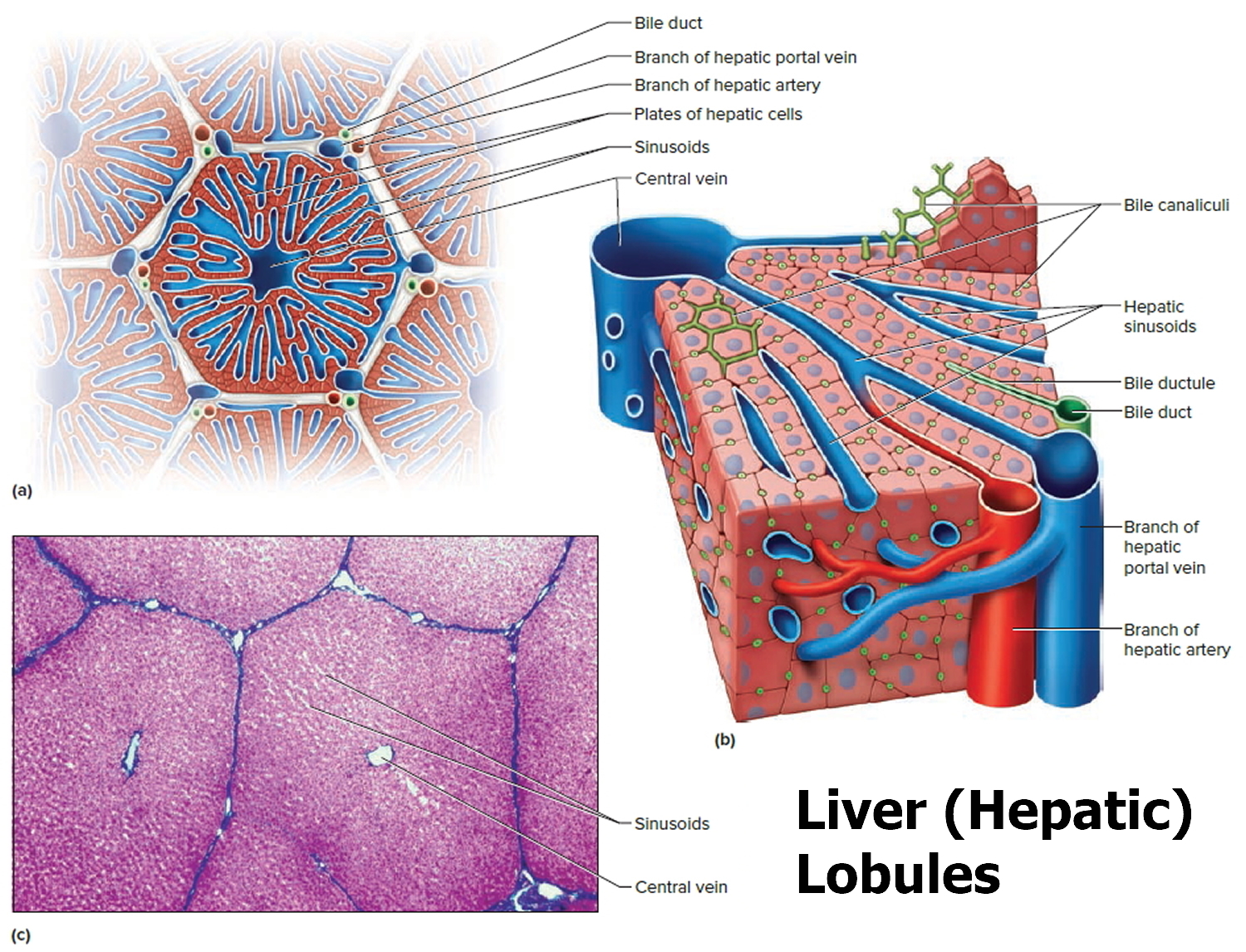
Figure 5. Liver lobule
Note: (a) Cross section of a hepatic lobule. (b) Enlarged longitudinal section of a hepatic lobule. (c) Light micrograph of hepatic lobules in cross section.
Is Wilson disease curable?
No. A abnormal gene cannot be corrected – it is present for life. Wilson’s disease a genetic disease that is inherited as an autosomal recessive trait. Wilson disease is caused by mutations in the ATP7B gene on chromosome 13, which codes for a membrane-bound copper transporting ATPase found mostly in the liver 14. ATP7B gene provides instructions for making a protein called copper-transporting ATPase 2, which plays a role in the transport of copper from the liver to other parts of the body. Copper is necessary for many cellular functions, but it is toxic when present in excessive amounts. The copper-transporting ATPase 2 protein is particularly important for the elimination of excess copper from the body. Mutations in the ATP7B gene prevent the transport protein from functioning properly. With a shortage of functional protein, excess copper is not removed from the body. As a result, copper accumulates to toxic levels that can damage tissues and organs, particularly the liver and brain.
The ATP7B mutations that cause Wilson disease are inherited, meaning they are passed from parent to child. These mutations are autosomal recessive , meaning that a person must inherit two ATP7B genes with mutations, one from each parent, to have Wilson disease. People who have one ATP7B gene without a mutation and one ATP7B gene with a mutation do not have Wilson disease, but they are carriers of the disease.
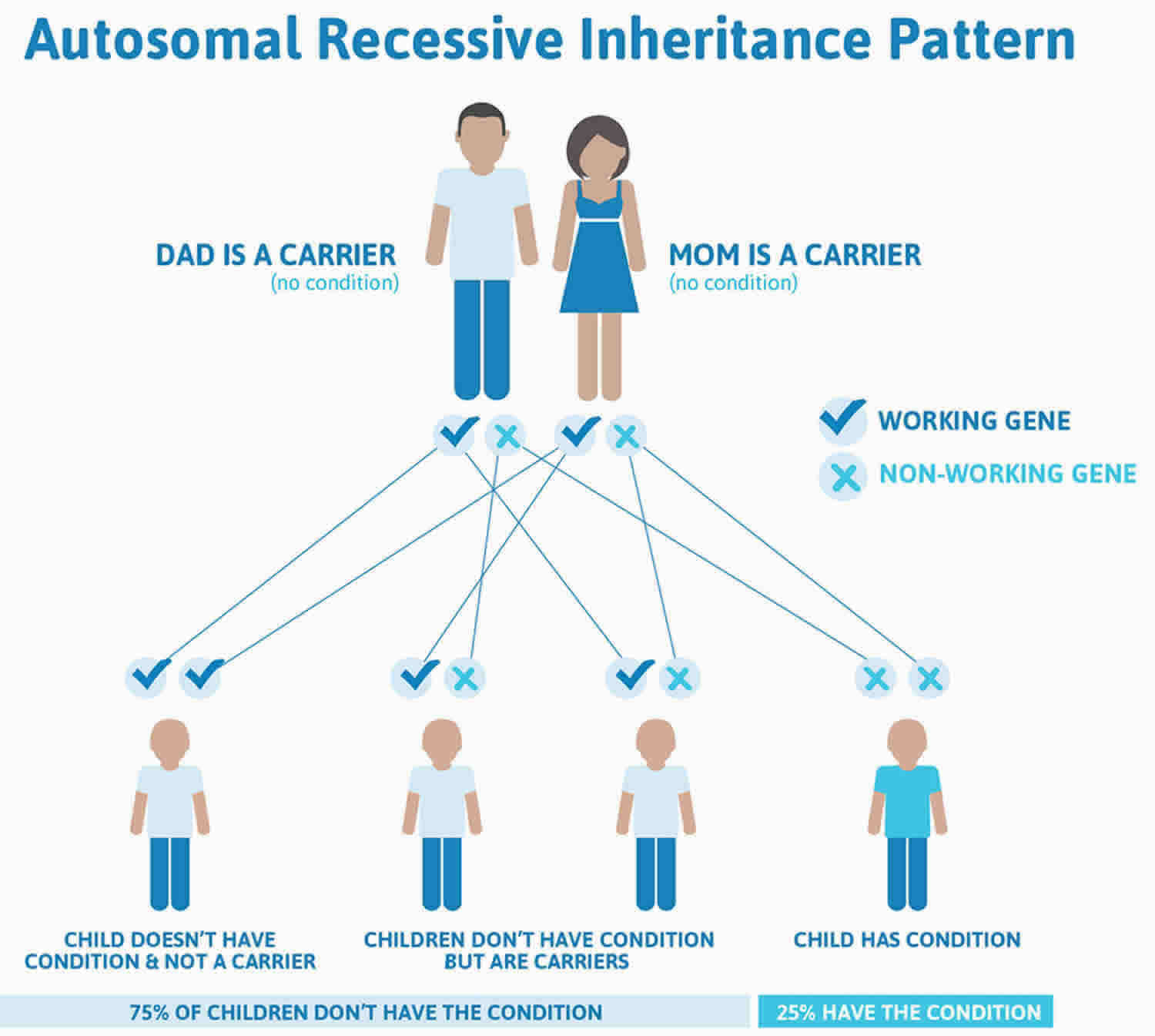
People can inherent Wilson disease if both parents are carriers who don’t have the disease. Figure 2 below shows the chance of inheriting Wilson disease from parents who are carriers.
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
How common is Wilson disease?
Experts are still studying how common Wilson disease is. Older studies suggested that about 1 in 30,000 people have Wilson disease 15. These studies were conducted before researchers discovered the gene mutations that cause Wilson disease.
Newer studies of people’s genes suggest that Wilson disease may be more common. A study in the United Kingdom found that about 1 in 7,000 people have gene mutations that cause Wilson disease 16.
Experts aren’t sure why gene studies suggest that Wilson disease is more common than previously thought. One reason might be that some people with Wilson disease are not diagnosed. Another reason might be that some people have gene mutations for Wilson disease but don’t develop the disease 17.
Who is more likely to have Wilson disease?
People have a higher chance of having Wilson disease if they have a family history of Wilson disease, especially if a first-degree relative, a parent, sibling, or child, has the disease.
People who have Wilson disease typically develop symptoms when they are between ages 5 and 40 18. However, some people develop symptoms at younger or older ages. Doctors have found the first symptoms of Wilson disease in infants as young as 9 months and in adults older than 70 years 15, 19.
How or where is the brain affected by copper accumulation?
Generally, the brain is affected symmetrically with excess copper deposition, although symptoms can be worse on one side of the body than another. This may have to do with factors of asymmetric neurologic development, such as being right or left-handed. The copper is often seen most prominently in the basal ganglia, the area deep within the brain that coordinates movements. The face of the giant panda sign refers to a characteristic appearance of the basal ganglia in advanced Wilson’s disease. This is a description of the appearance of the basal ganglia wherein one can get an impressionists image of the face of a giant panda.
Can Wilson’s disease result in permanent brain damage leading to memory loss?
Even though Wilson’s disease is primarily classified and considered as a “movement disorder,” cognitive decline is very common. The analogy is with Parkinson disease, where some patients develop “subcortical dementia.” The subject of dementia/cognitive decline in Wilson’s disease has not been studied that well but some papers about this have been published. Basically, what is going on is the disruption of projections of the basal ganglia to the prefrontal cortex. This may be reversible if Wilson disease is treated and the patient responds to the treatment.
My doctor says I have high copper in my blood (serum copper). Could I have Wilson disease?
High serum copper is not an indication of Wilson disease (see diagnosis below). Since most Wilson patients have a low ceruloplasmin they actually have a lower than normal serum copper. Ceruloplasmin is the protein that binds with copper to remove it from the body. It is the unbound (to ceruloplasmin) copper that is free to roam around the body and accumulate in organs causing Wilson disease damage.
An elevated serum copper is more often due to an elevation of the level of serum ceruloplasmin since it contains ~90% of the circulating copper bound to it. Elevations of ceruloplasmin can occur with inflammation, in response to estrogen therapy and in pregnancy. Note: The exception to this is when there is severe liver injury (acute liver failure) caused by Wilson disease. This causes very large amounts of copper to be released into circulation and causes markedly elevated serum copper. When this occurs, patients are very ill and usually have jaundice (yellow eyes and skin color) and very abnormal lab results with respect to liver function and blood coagulation.
Are copper IUDs safe for Wilson’s disease patients?
The IUD is plastic with copper wound around it. Experts would not advise it in women with Wilson’s disease. There are progesterone containing IUDs, one of which was just released, that are good for five years instead of one to two years.
It is not uncommon for symptomatic women with Wilson’s disease to suffer irregular periods and multiple miscarriages. These are due to malfunction of the liver causing hormonal changes which are reversible with successful treatment of the underlying disorder.
With what medication should the Wilson’s disease patient begin treatment?
There are now new options for the medical treatment of patients with Wilson’s disease. Penicillamine is no longer the “treatment of choice,” as there is a growing experience with safer and effective alternatives. Trientine may be the best first choice amongst currently approved drugs as initial therapy for symptomatic patients requiring chelation therapy, and may be even more effective when used in combination with zinc treatment. Zinc is an effective medication for maintenance therapy. Further studies are needed to determine the best therapy for pregnant patients with Wilson’s disease, and whether combination therapy using trientine and zinc will be the next “treatment of choice” for all symptomatic patients with liver or neurologic disease.
What happens if too much copper is removed through chelation?
When too much copper is removed, then there can be reductions in blood counts and inhibition of wound healing, amongst other possible effects. This is the reason that blood counts should be periodically monitored. The amount of copper can be gauged by reviewing the patterns of the 24- hour urine copper excretion as well as looking for the “non-ceruloplasmin” copper in the blood– this being done by a simultaneous measure of ceruloplasmin and serum copper. When these values are too low, excluding the possibility of non-compliance which can alter the interpretation of the urine copper excretion, then the dosages must be adjusted.
Can Zinc and Trientine be used in combination?
The combination of zinc and trientine can be used for the first four months of therapy in patients with significant liver or neurologic disease. How often you check lab values depends on the extent of Wilson’s disease, the range can be from weekly checks of urine copper and zinc to every three months after initiating treatment. Subsequently, the urine copper and zinc could be checked every six months for two years, then annually with more frequent checks if compliance is in doubt. Urine copper levels should be in the range expected for treatment with trientine alone, in other words 1-2 mg /24 hours initially and then reducing to 0.5-1.0 mg after several months of treatment.
Doctors look at the trend in urine values over time as much as the absolute numbers at any one time to gauge compliance and treatment effectiveness at reducing copper. You also can monitor the non-ceruloplasmin copper. This frequently falls to less than 10 micrograms/dl on the combination therapy. Monitoring for compliance: The urine zinc should be over 2.0 mg with adequate compliance with zinc treatment. Compliance with trientine is gauged by an initial increase in urine copper when the medicine is first started followed by a drop in urine copper values over time.
Monitoring for over treatment: Be concerned if the urine copper is less than 35, consider in the presence of anemia or decreased white blood count. On combination therapy, the urine copper may be higher than 35 in the presence of copper deficiency, so watch for unexplained anemia or decreased white blood count.
Monitoring for toxicity: Watch for gastric side effects from zinc such as nausea. Watch for proteinuria, bone marrow suppression and autoimmune disease with trientine.
Summary
Monitoring patients taking the combination of trientine and zinc is most like monitoring those taking trientine alone. The main difference is an increase in urine zinc should be seen to demonstrate compliance with zinc treatment.
How long should Zinc and Trientine be used in combination?
In our experience, the combination of zinc and trientine is not necessary beyond the initial four to six month period of removing free copper stores. Zinc maintenance therapy works well for most people thereafter. Obviously, treatment programs and decisions need to be individualized. Nevertheless, experts are not aware of compelling data to suggest that there is any need for taking the combination of zinc and trientine long term for the majority of people.
Will Galzin dissolve and remove the already accumulated copper in the brain or is it only effective controlling the further accumulation of copper?
With zinc acetate (Galzin) treatment there is a negative copper balance. More copper goes out than in, so in time all extra stores of copper, even in the brain, are removed. Proof of this is the loss of Kayser-Fleischer rings in treated patients with time on zinc. However, if there has been damage done to the brain cells by copper, this may [or may not] be reversible.
Are there any problems with zinc collecting in the body over time?
The zinc levels in the body increase slightly initially but zinc does not accumulate over time. Experts know this from repeat measurements including repeat liver biopsies which were used to measure liver copper and zinc to answer this very question. In short, the main concern with long-term treatment with zinc (as well as a concern with all other forms of treatment of Wilson’s Disease) would be the potential for over treatment which may lead to copper deficiency. Fortunately, this is relatively unusual but doctors monitor 24-hour urine copper and zinc levels to avert this from happening on at least an annual basis. If copper levels get too low, zinc doses can be reduced before the symptoms of copper deficiency, primarily manifested as anemia, ensue. The best approach is keep taking your zinc and check your urine copper and zinc at least once a year.
How long does Galzin last?
Galzin capsules should last indefinitely, so long as they do not physically fall apart. Zinc itself is an element, so it does not deteriorate over time.
How can I reduce the possible nausea and indigestion when taking zinc?
Experts suggest that you take a small piece of lunch meat (turkey, bologna, ham, etc.) with your first morning dose of zinc. This should help settle your stomach. Do not take any carbohydrate (bread, etc.) with the dose–this is very important! The nausea usually abates as treatment persists. Occasionally, someone finds that nausea to persist, but lunchmeat generally helps.
Does zinc cause ulcers?
Zinc does not cause ulcers, but ulcers are common problems. Patients experiencing abdominal pain and nausea should consult with their gastroenterologist.
What does high urine zinc mean?
High urine zinc proves the patient is taking his or her zinc conscientiously.
Is Wilson’s disease treatment safe for the unborn baby?
Review of the literature and experts experience indicate that women successfully treated with either penicillamine, trientine or zinc uninterruptedly, have excellent chances for carrying through uncomplicated pregnancies and for delivering normal babies. However, precautions are indicated in women with dilated veins in the stomach or esophagus, which may rupture and bleed because of the increased abdominal pressure caused by the enlarging uterus. There is no report of an untoward reaction to a baby nursed while the mother continued on an anti-copper regimen.
What are some of the other symptoms of Wilson disease?
- Hepatic: Asymptomatic hepatomegaly; isolated splenomegaly; Persistent elevated aspartate aminotransferase (AST), alanine aminotransferase (ALT); fatty liver; acute hepatitis; resembling autoimmune hepatitis; cirrhosis (compensated or decompensated); fulminant hepatic failure
- Neurological: Movement disorders (tremor, involuntary movements); drooling, dysarthria; rigid dystonia; pseudobulbar palsy; seizures; migraine headaches; insomnia
- Psychiatric: Depression; neuroses; personality changes; psychosis
- Other symptoms: Renal abnormalities: amino-aciduria and nephrolithiasis; skeletal abnormalities: premature osteoporosis and arthritis; cardiomyopathy, dysrhythmias; pancreatitis; hypoparathyroidism; menstrual irregularities: infertility, repeated miscarriages.
Will Tizanidine help control or reduce dystonia?
Medications doctors commonly use to control the symptoms of dystonia are Klonipin and Artane. Tizanidine may be reasonable to try as well. Obviously, an examining physician must decide what is best to try for each patient’s individual condition. Doctors also use zinc acetate or at times trientine in preference to penicillamine due to the risk of making neurologic disease worse on penicillamine. Physical therapy is also quite important for your treatment plan.
Should Wilson’s disease patients use weight-gaining supplements to help maintain their weight?
Metabolic enhancers like pro-kinetic are dangerous for people with liver disease, they can cause liver failure even in healthy people. Many dietary supplements like Ensure, etc., also contain copper supplements. If you are trying to gain weight and have been on appropriate therapy, drinking one can of Vanilla Boost Plus per day should not give you too much copper. You also can make your own high calorie drinks by mixing protein supplements with a milk shake.
What copper levels in drinking water are potentially hazardous for Wilson’s disease patients?
If the water copper level is over 0.1 ppm (parts per million) (which is 0.1 mg/L), experts recommend you drink water from an alternative source. While 0.1 ppm isn’t particularly hazardous, it indicates that significant copper is coming from somewhere, and at certain times or under certain circumstances the level might be quite a bit higher.
Should Wilson’s patients receive Hepatitis A or Hepatitis B vaccine?
Yes. Since Wilson’s disease often affects the liver, many Wilson’s disease patients cannot afford additional injury to the liver. Hepatitis A or Hepatitis B vaccine is as safe for Wilson’s disease patients as it is for others.
What percentage of Wilson’s disease patients need liver transplants?
Only about 5% of patients with Wilson’s disease need transplants. Two thirds are those presenting with liver failure. The remainder are those discovered with severe liver disease that doesn’t respond well to medical therapy, those who stop therapy and deteriorate, or those that experience severe complications of cirrhosis such as frequent gastrointestinal bleeding from varices due to portal hypertension or low oxygenation due to hepatopulmonary syndrome.
Do patients taking penicillamine have a difficult time in general healing from surgery?
For all surgical procedures, it is recommended that the dosage of penicillamine be temporarily reduced to 250-500 mg per day until wound healing is achieved. Similarly, the dosage should be reduced during the last trimester pregnancy and until wound healing after childbirth is achieved. No such dosage reduction is needed for zinc treatment.
What level of liver recovery can I expect with treatment?
The course of liver disease in Wilson’s disease stands in contrast to other forms of cirrhosis for many people. The chronic liver injury in Wilson’s disease is caused by excess free copper, and the liver disease often stabilizes or even improves once the excess copper is treated with zinc acetate maintenance therapy. While some people do progress to need liver transplantation, others may actually see long-term improvement in their liver function over time. It is important to be attentive to issues such as immunizations for viral hepatitis, avoiding excess alcohol consumption, and treating complications of portal hypertension in order to give the liver its best chance to mend.
What genetic testing is currently available for Wilson disease?
The sequence analysis of ATP7B gene (Wilson disease gene) to identify the mutations is clinically available as a test. Although this is the most updated and thorough test, please be aware that some alterations such as large deletion or duplication may not be detected with this method. It is important that the biochemical testing must be performed prior to genetic tests.
Wilson disease complications
People who have Wilson disease that is not treated or diagnosed early can have serious complications, such as:
- Cirrhosis—scarring of the liver. As liver cells try to make repairs to damage done by excess copper, scar tissue forms in the liver, making it more difficult for the liver to function.
- Kidney damage—as liver function decreases, the kidneys may be damaged. Wilson’s disease can damage the kidneys, leading to problems such as kidney stones and an abnormal number of amino acids excreted in the urine.
- Persistent nervous system problems when nervous system symptoms do not resolve. Tremors, involuntary muscle movements, clumsy gait and speech difficulties usually improve with treatment for Wilson’s disease. However, some people have persistent neurological difficulty despite treatment.
- Psychological problems. These might include personality changes, depression, irritability, bipolar disorder or psychosis.
- Liver cancer—hepatocellular carcinoma is a type of liver cancer that can occur in people with cirrhosis
- Liver failure—a condition in which the liver stops working properly. This can occur suddenly (acute liver failure), or it can develop slowly over years. A liver transplant might be a treatment option.
- Blood problems. These might include destruction of red blood cells (hemolysis) leading to anemia and jaundice.
- Death, if left untreated
Other complications may include:
- Anemia (hemolytic anemia is rare)
- Fatty liver
- Hepatitis
- Increased number of bone fractures
- Increased number of infections
- Injury caused by falls
- Jaundice
- Joint contractures or other deformity
- Loss of ability to care for self
- Loss of ability to function at work and home
- Loss of ability to interact with other people
- Loss of muscle mass (muscle atrophy)
- Psychological complications
- Side effects of penicillamine and other medicines used to treat the disorder
- Spleen problems
Liver failure and damage to the central nervous system (brain, spinal cord) are the most common and dangerous effects of the disorder. If Wilson disease is not caught and treated early, it can be fatal.
Wilson’s disease life expectancy
The oldest newly diagnosed Wilson’s disease patient is over 70 years old.
The chronic liver injury in Wilson’s disease is caused by excess free copper, and the liver disease often stabilizes or even improves once the excess copper is treated with zinc acetate maintenance therapy. While some people do progress to need liver transplantation, others may actually see long-term improvement in their liver function over time. It is important to be attentive to issues such as immunizations for viral hepatitis, avoiding excess alcohol consumption, and treating complications of portal hypertension in order to give the liver its best chance to mend.
Wilson’s disease prognosis
The prognosis of untreated Wilson disease patients is poor with a median life expectancy of 40 years 13. The natural history of Wilson’s disease without treatment is usually progression of either or both liver disease and neurologic disease, and eventually death 20. Today with all of the available therapeutic regimens, a normal life expectancy of patients with Wilson disease is achievable 21. In addition clinical, neurological, and hematological symptoms improve during treatment to a significant extent 21. Exceptions are those indicating impaired liver function due to cirrhosis and complications of portal hypertension 22. Most challenging are neurologic disorders, which are only partial reversed and in rare cases may even deteriorate which may be due to inefficient access of present therapies to brain copper and iron or due to the mutated neuronal ATP7B 13.
Various scoring systems have been put forward for Wilson disease prognostication. Some of these incorporate levels of AST, bilirubin, and prothrombin time, etc. on presentation 23. Patients with a prognostic score of 7 or more should be referred for a liver transplant. Patients with this score are generally dead within 8 weeks without treatment. After liver transplant, the prognosis is good. A survival rate of 87% at 15 years has been reported 24.
Wilson’s disease causes
Wilson disease is caused by mutations in the ATP7B gene on the long arm of chromosome 13 at position 14.3 (13q14), which codes for a membrane-bound copper transporting ATPase found mostly in the liver 25, 26, 27. In Wilson disease almost 800 different mutations of the ATP7B gene are known 28, 29, 30. ATP7B gene provides instructions for making a protein called copper-transporting ATPase 2, which plays a role in the transport of copper from the liver to other parts of the body 31. Copper is necessary for many cellular functions, but it is toxic when present in excessive amounts. The copper-transporting ATPase 2 protein is particularly important for getting rid of excess copper from the body 32. Mutations in the ATP7B gene prevent the transport protein from functioning properly. With a shortage of functional protein, excess copper is not removed from the body. As a result, copper accumulates to toxic levels that can damage tissues and organs, particularly the liver and brain.
Normally, the liver releases extra copper into bile. Bile carries the copper, along with other toxins and waste products, out of the body through the digestive tract. In Wilson disease, the liver releases less copper into bile, and extra copper stays in the body.
Research indicates that a normal variation in the PRNP gene may modify the course of Wilson disease. The PRNP gene provides instructions for making prion protein, which is active in the brain and other tissues and appears to be involved in transporting copper. Studies have focused on the effects of a PRNP gene variation that affects position 129 of the prion protein. At this position, people can have either the protein building block (amino acid) methionine or the amino acid valine. Among people who have mutations in the ATP7B gene, it appears that having methionine instead of valine at position 129 of the prion protein is associated with delayed onset of symptoms and an increased occurrence of neurological symptoms, particularly tremors. Larger studies are needed, however, before the effects of this PRNP gene variation on Wilson disease can be established.
Wilson disease inheritance pattern
Wilson disease is inherited in an autosomal recessive pattern, meaning that a person must inherit two ATP7B genes with mutations, one from each parent, to have Wilson disease. The parents of an individual with Wilson disease (an autosomal recessive condition) each carry one copy of the mutated ATP7B gene, but they typically do not show signs and symptoms of the condition and do not have Wilson disease, but they are carriers of the disease.
People can inherent Wilson disease if both parents are carriers who don’t have the disease. The mutations that cause Wilson disease are autosomal recessive, meaning that a person must inherit two ATP7B genes with mutations to have Wilson disease. The chart below shows the chance of inheriting Wilson disease from parents who are carriers.
Autosomal recessive genetic disorders occur when an individual inherits the same abnormal gene for the same trait from each parent. If an individual receives one normal gene and one gene for the disease, the person will be a carrier for the disease, but usually will not show symptoms. The risk for two carrier parents to both pass the altered gene and, therefore, have an affected child is 25% with each pregnancy. The risk of having a child who is a carrier like the parents is 50% with each pregnancy. The chance for a child to receive normal genes from both parents and be genetically normal for that particular trait is 25%. The risk is the same for males and females.
Men and women develop Wilson disease at equal rates.
A person’s risk of being a carrier or having Wilson disease increases when his or her family has a known history of Wilson disease. Some people may not know about a family history of the condition because the mutation is often passed to a child by a parent who is a carrier. A person’s chances of having Wilson disease increase if a health care provider has diagnosed one or both parents with the condition.
Genetic counseling may help you understand the risks of passing Wilson’s disease on to any children you have.
- To find a medical professional who specializes in genetics, you can ask your doctor for a referral or you can search for one yourself. Online directories are provided by the American College of Medical Genetics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) and the National Society of Genetic Counselors (https://www.findageneticcounselor.com/).
Figure 6. Wilson’s disease autosomal recessive inheritance pattern
How can Wilson’s disease be prevented?
A person cannot prevent Wilson disease; however, people with a family history of Wilson disease, especially those with an affected sibling or parent, should talk with a health care provider about testing. A health care provider may be able to diagnose Wilson disease before symptoms appear. Early diagnosis and treatment of Wilson disease can reduce or even prevent organ damage.
People with a family history of the disease may also benefit from genetic testing that can identify one or more gene mutations. A health care provider may refer a person with a family history of Wilson disease to a geneticist—a doctor who specializes in genetic diseases.
Genetic counseling may help you understand the risks of passing Wilson’s disease on to any children you have.
- To find a medical professional who specializes in genetics, you can ask your doctor for a referral or you can search for one yourself. Online directories are provided by the American College of Medical Genetics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) and the National Society of Genetic Counselors (https://www.findageneticcounselor.com/).
Wilson’s disease symptoms
The signs and symptoms of Wilson disease vary, depending on what organs of the body are affected. Wilson disease is present at birth; however, the signs and symptoms of the disease do not appear until the copper builds up in the liver, the brain, or other organs.
When people have signs and symptoms, they usually affect the liver, the central nervous system, or both. The central nervous system includes the brain, the spinal cord, and nerves throughout the body. Sometimes a person does not have symptoms and a health care provider discovers the disease during a routine physical exam or blood test, or during an illness. Children can have Wilson disease for several years before any signs and symptoms occur.
People with Wilson disease may have:
- liver-related signs and symptoms
- central nervous system-related signs and symptoms
- mental health-related signs and symptoms
- other signs and symptoms
People with Wilson disease may develop signs and symptoms of chronic, or long lasting, liver disease:
- weakness
- fatigue, or feeling tired
- loss of appetite
- nausea
- vomiting
- weight loss
- pain and bloating from fluid accumulating in the abdomen
- edema—swelling, usually in the legs, feet, or ankles and less often in the hands or face
- itching
- spiderlike blood vessels, called spider angiomas, near the surface of the skin
- muscle cramps
- jaundice, a condition that causes the skin and whites of the eyes to turn yellow
Some people with Wilson disease may not develop signs or symptoms of liver disease until they develop acute liver failure—a condition that develops suddenly.
Central nervous system-related symptoms usually appear in people after the liver has retained a lot of copper; however, signs and symptoms of liver disease may not be present. Central nervous system-related symptoms occur most often in adults and sometimes occur in children 10. Signs and symptoms include
- tremors or uncontrolled movements
- muscle stiffness
- problems with speech, swallowing, or physical coordination
A health care provider may refer people with these symptoms to a neurologist—a doctor who specializes in nervous system diseases.
Some people will have mental health-related signs and symptoms when copper builds up in the central nervous system. Signs and symptoms may include
- personality changes
- depression
- feeling anxious, or nervous, about most things
- psychosis—when a person loses contact with reality
Wilson’s disease eyes
Kayser-Fleischer rings result from a buildup of copper in the eyes and are the most unique sign of Wilson disease. During an eye exam, a health care provider will see a rusty-brown ring around the edge of the iris and in the rim of the cornea. The iris is the colored part of the eye surrounding the pupil. The cornea is the transparent outer membrane or layer that covers the eye.
People with Wilson disease who show signs of nervous system damage usually have Kayser-Fleischer rings. Approximately 95% of Wilson disease patients presenting with neurological signs will have a Kayser-Fleischer ring. However, Kayser-Fleischer rings are present in only 40 to 66 percent of people with signs of liver damage alone 10. Copper chelation therapy may cause fading and even disappearance of the corneal copper over time.
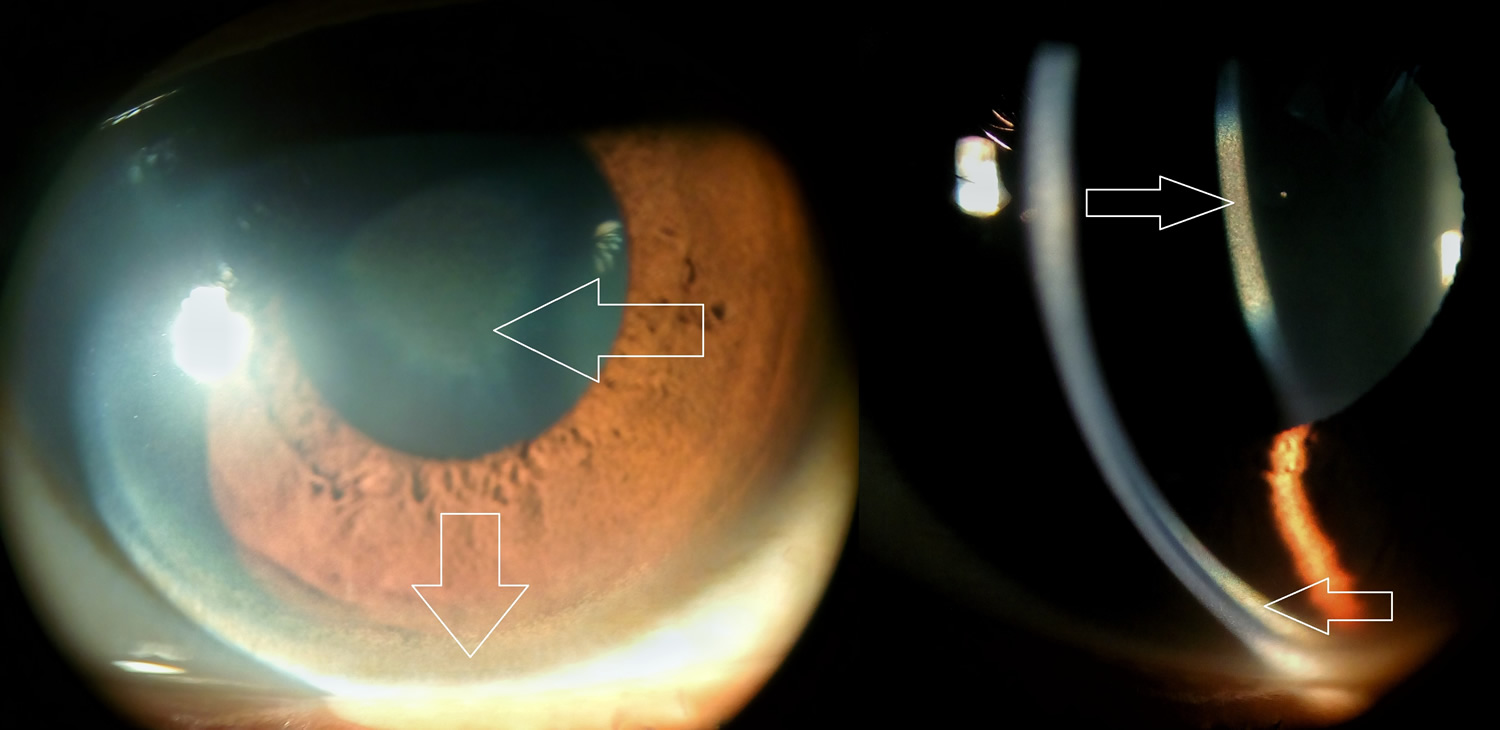
Figure 5. Wilson’s disease eyes
Footnote: Kayser Fleischer Ring (big down arrow) due to copper deposition in peripheral Descemet membrane and Sunflower cataract (big left arrow) in a 40 year old male suffering from Wilson’s Disease.
[Source 33]Figure 6. Kayser-Fleischer ring
Other signs and symptoms
Other signs and symptoms of Wilson disease may include
- anemia, a condition in which red blood cells are fewer or smaller than normal, which prevents the body’s cells from getting enough oxygen
- arthritis, a condition in which a person has pain and swelling in one or more joints
- high levels of amino acids, protein, uric acid, and carbohydrates in urine
- low platelet or white blood cell count
- osteoporosis, a condition in which the bones become less dense and more likely to fracture
Wilson’s disease diagnosis
Diagnosing Wilson’s disease can be challenging because its signs and symptoms are often hard to tell from those of other liver diseases, such as hepatitis. Also, symptoms can evolve over time. Behavioral changes that come on gradually can be especially hard to link to Wilson’s.
Doctors may use several tests and exams to diagnose Wilson disease. Tests and procedures used to diagnose Wilson’s disease include:
- medical and family history
- physical exam
- blood tests
- urine tests
- liver biopsy
- imaging tests
Doctors typically see the same symptoms of Wilson disease in other conditions, and the symptoms of Wilson disease do not occur together often, making the disease difficult to diagnose.
Medical and Family History
A health care provider may take a medical and family history to help diagnose Wilson disease.
Physical Exam
A physical exam may help diagnose Wilson disease. During a physical exam, a health care provider usually:
- examines a patient’s body
- uses a stethoscope to listen to sounds related to the abdomen
A health care provider will use a special light called a slit lamp to look for Kayser-Fleischer rings in the eyes.
Wilson’s disease test
Blood Tests
A nurse or technician will draw blood samples at a health care provider’s office or a commercial facility and send the samples to a lab for analysis. A health care provider may:
- Perform liver enzyme or function tests—blood tests that may indicate liver abnormalities.
- Check copper levels in the blood. Since the copper is deposited into the organs and is not circulating in the blood, most people with Wilson disease have a lower-than-normal level of copper in the blood. In cases of acute liver failure caused by Wilson disease, the level of blood copper is often higher than normal.
- Total serum copper – may be ordered to help diagnose; usually decreased.
- Free serum copper (non-ceruloplasmin-bound) – used to diagnose and monitor; usually increased.
- 24-hour urine copper – used to diagnose and monitor; usually increased.
- Hepatic copper – a liver tissue biopsy collected to help diagnose; deposits of copper may not be evenly distributed in the liver.
- Ceruloplasmin — a protein that carries copper in the bloodstream is usually ordered to help diagnose Wilson disease. Most people with Wilson disease have a lower-than-normal ceruloplasmin level. But about 5% of those affected who have neurological symptoms will have normal ceruloplasmin levels as will up to 40% of those with hepatic symptoms.
- Conduct genetic testing. A health care provider may recommend genetic testing in cases of a known family history of Wilson disease.
How to calculate serum free copper
The amount of serum free copper is the amount of copper circulating in the blood which is unbound by ceruloplasmin. This is the copper which is “free” to accumulate in the liver and other organs. Most reference labs do not automatically calculate the amount of serum free copper in a Wilson’s disease patient’s lab report. To calculate serum free copper, use the following formula:
(Total Serum Copper in μg/dl) – (Ceruloplasmin in mg/dl x 3) = Free Copper (Normal range is 5 – 15 μg/dl)
Example:
- Serum Copper of 22.2 (μg/dl) 22.2 (μg/dl)
- Ceruloplasmin of 4.7 (mg/dl) x 3 -14.1 (μg/dl)
- Free Copper =8.1(μg/dl)
OR - (Total Serum Copper in μmole/L x 63.55) – (Ceruloplasmin in mg/L x 3) = (Free Copper in μg/L ÷ 10) = Free Copper in μg/dl (Normal range is 5 – 15 μg/dl)
Example:
- Serum Copper of 6.3(μmole/L) x 63.55 400.3 (μg/L)
- Ceruloplasmin of 60 (mg/L) x 3 -180 (μg/L)
- Free Copper =220.3 (μg/L)
- Free Copper in (μg/L) ÷ 10 =20.3(μg/dl)
NOTE: There are often lab variations in the determination of ceruloplasmin and sometimes negative values are found. Some labs will not report the low serum coppers. If a patient has a very low ceruloplasmin, this formula may not be useable to determine free copper
Molecular genetic testing
This is specialized testing that is available from a limited number of reference or research laboratories. It is used to diagnose Wilson disease and identify mutation(s) and identify carriers. Some prediction of disease severity can be established based upon the mutations present, but testing cannot determine the severity, complications, or organ involvement that will be experienced by a specific individual. Severity can vary significantly, even between family members with the same mutations.
- ATP7B gene: panels of the most prevalent mutations in a region or ethnic population may be performed.
- If the mutations have been identified in a person with Wilson disease, then the family members of that person can be tested for those specific mutations.
- Gene sequencing can be performed to examine the entire gene for mutations. This is the most thorough test.
- Linkage analysis: this requires blood from parents, siblings, and an affected family member. It compares genetic information present close to the ATP7B gene.
Urine Tests
24-hour urine collection. A patient will collect urine at home in a special container provided by a health care provider’s office or a commercial facility. A health care provider sends the sample to a lab for analysis. A 24-hour urine collection will show increased copper in the urine in most patients who have symptoms due to Wilson disease.
Liver Biopsy
A liver biopsy is a procedure that involves taking a small piece of liver tissue for examination with a microscope for signs of damage or disease. The health care provider may ask the patient to stop taking certain medications temporarily before the liver biopsy. He or she may also ask the patient to fast—eat or drink nothing—for 8 hours before the procedure.
During the procedure, the patient lies on a table, right hand resting above the head. The health care provider applies a local anesthetic to the area where he or she will insert the biopsy needle. If needed, a health care provider will also give sedatives and pain medication. The health care provider uses the needle to take a small piece of liver tissue. He or she may use ultrasound, computerized tomography scans, or other imaging techniques to guide the needle. After the biopsy, the patient must lie on the right side for up to 2 hours and is monitored an additional 2 to 4 hours before being sent home.
A pathologist—a doctor who specializes in diagnosing diseases—examines the liver tissue in a lab. The test can show cirrhosis of the liver. Sometimes the liver biopsy will show copper buildup in the liver cells; however, the results can vary because the copper does not always deposit evenly into the liver. Therefore, health care providers often find it more useful to analyze a piece of liver tissue for copper content. Most patients with Wilson disease have high levels of copper in the liver tissue when compared with carriers or with people who do not have Wilson disease.
Imaging Tests
A health care provider may order imaging tests to evaluate brain abnormalities in patients who have nervous system symptoms often seen with Wilson disease, or in patients diagnosed with Wilson disease. Health care providers do not use brain imaging tests to diagnose Wilson disease, though certain findings may suggest the patient has the disease.
Magnetic resonance imaging (MRI). An MRI is a test that takes pictures of the body’s internal organs and soft tissues without using x-rays. A specially trained technician performs the procedure in an outpatient center or a hospital, and a radiologist—a doctor who specializes in medical imaging—interprets the images. The patient does not need anesthesia, though people with a fear of confined spaces may receive light sedation, taken by mouth. An MRI may include the injection of a special dye, called contrast medium. With most MRI machines, the patient will lie on a table that slides into a tunnel-shaped device that may be open ended or closed at one end. Some machines allow the patient to lie in a more open space. The technician will take a sequence of images from different angles to create a detailed picture of the brain. During sequencing, the patient will hear loud mechanical knocking and humming noises. MRI can show if other diseases or conditions are causing the patient’s neurological symptoms.
Computerized tomography (CT) scan. A CT scan uses a combination of x-rays and computer technology to create images. For a CT scan, a health care provider may give the patient a solution to drink and an injection of contrast medium. CT scans require the patient to lie on a table that slides into a tunnel-shaped device where a technician takes the x-rays. An x-ray technician performs the procedure in an outpatient center or a hospital. A radiologist interprets the images. The patient does not need anesthesia. A CT scan can show if other diseases or conditions are causing the patient’s neurological symptoms.
Wilson’s disease treatment
Your doctor will treat Wilson’s disease with a lifelong effort to reduce and control the amount of copper in your body.
Your doctor might recommend medications called chelating agents, which bind copper and then prompt your organs to release the copper into your bloodstream. The copper is then filtered by your kidneys and released into your urine.
Treatment then focuses on preventing copper from building up again. For severe liver damage, a liver transplant might be necessary.
Treatment may include
- medications
- changes in eating, diet, and nutrition
- a liver transplant
Medications
A health care provider will prescribe medications to treat Wilson disease. The medications have different actions that health care providers use during different phases of the treatment.
People with Wilson disease will take medications for the rest of their lives. Follow-up and adherence to the health care provider’s treatment plan is necessary to manage symptoms and prevent organ damage.
Chelating agents. Chelating agents are medications that remove extra copper from the body by releasing it from organs into the bloodstream. Once the copper is in the bloodstream, the kidneys then filter the copper and pass it into the urine. A health care provider usually recommends chelating agents at the beginning of treatment. A potential side effect of chelating agents is that nervous system symptoms may become worse during treatment. The two medications available for this type of treatment include
- Trientine (Syprine)—the risk for side effects and worsening nervous system symptoms appears to be lower with trientine than d-penicillamine. Researchers are still studying the side effects; however, some health care providers prefer to prescribe trientine as the first treatment of choice because it appears to be safer. Still, neurological symptoms can worsen when taking trientine.
- D-penicillamine (Cuprimine, Depen) —people taking D-penicillamine may have other reactions or side effects, such as:
- fever
- a rash
- kidney problems
- bone marrow problems
A health care provider will prescribe a lower dose of a chelating agent to women who are pregnant to reduce the risk of birth defects. A health care provider should consider future screening on any newborn whose parent has Wilson disease.
- Zinc acetate (Galzin). A health care provider will prescribe zinc for patients who do not have symptoms, or after a person has completed successful treatment using a chelating agent and symptoms begin to improve. Zinc, taken by mouth as zinc salts such as zinc sulfate, zinc gluconate or zinc acetate, blocks the digestive tract’s absorption of copper from food 34. Zinc salts induce intestinal metallothioneins, which safely bind copper in food and endogenous secretions to be sloughed off and excreted in the stools. Zinc also induces metallothioneins in liver cells (hepatocytes), lowering non-ceruloplasmin-bound copper (free copper) circulating in the blood and resulting in a gradual de-coppering of organs 35. Although most people taking zinc usually do not experience side effects, some people may experience stomach upset. A health care provider may prescribe zinc for children with Wilson disease who show no symptoms. Women may take the full dosage of zinc safely during pregnancy.
Maintenance, or long term treatment begins when symptoms improve and tests show that copper is at a safe level. Maintenance treatment typically includes taking zinc or a lower dose of a chelating agent. A health care provider closely monitors the person and reviews regular blood and urine tests to ensure maintenance treatment controls the copper level in the body.
Treatment for people with Wilson disease who have no symptoms may include a chelating agent or zinc in order to prevent symptoms from developing and stop or slow disease progression.
Changes in Eating, Diet, and Nutrition
People with Wilson disease should reduce their dietary copper intake by avoiding foods that are high in copper, such as:
- shellfish
- liver
- mushrooms
- nuts
- chocolate
Table 1. Copper content of selected foods
| Food | Micrograms (mcg) per serving |
|---|---|
| Beef, liver, pan fried (3 ounces) | 12400 |
| Oysters, eastern, wild, cooked, 3 ounces | 4850 |
| Baking chocolate, unsweetened, 1 ounce | 938 |
| Potatoes, cooked, flesh and skin, 1 medium potato | 675 |
| Mushrooms, shiitake, cooked, cut pieces, ½ cup | 650 |
| Cashew nuts, dry roasted, 1 ounce | 629 |
| Crab, Dungeness, cooked, 3 ounces | 624 |
| Sunflower seed kernels, toasted, ¼ cup | 615 |
| Turkey, giblets, simmered, 3 ounces | 588 |
| Chocolate, dark, 70%-85% cacao solids, 1 ounce | 501 |
| Tofu, raw, firm, ½ cup | 476 |
| Chickpeas, mature sees, ½ cup | 289 |
| Millet, cooked, 1 cup | 280 |
| Salmon, Atlantic, wild, cooked, 3 ounces | 273 |
| Pasta, whole wheat, cooked, 1 cup (not packed) | 263 |
| Avocado, raw, ½ cup | 219 |
| Figs, dried, ½ cup | 214 |
| Spinach, boiled, drained, ½ cup | 157 |
| Asparagus, cooked, drained, ½ cup | 149 |
| Seseame seeds, ¼ cup | 147 |
| Turkey, ground, cooked, 3 ounces | 128 |
| Cereals, Cream of Wheat, cooked with water, stove-top, 1 cup | 104 |
| Tomatoes, raw, chopped, ½ cup | 53 |
| Yogurt, Greek, plain, lowfat, 7-ounce container | 42 |
| Milk, nonfat, 1 cup | 27 |
| Apples, raw, with skin, ½ cup slices | 17 |
People should not eat these foods during the initial treatment and talk with the health care provider to discuss if they are safe to eat in moderation during maintenance treatment.
People with Wilson disease whose tap water runs through copper pipes or comes from a well should check the copper levels in the tap water. Water that sits in copper pipes may pick up copper residue, but running water lowers the level to within acceptable limits. People with Wilson disease should not use copper containers or cookware to store or prepare food or drinks.
To help ensure coordinated and safe care, people should discuss their use of complementary and alternative medical practices , including their use of vitamins and dietary supplements, with their health care provider. If the health care provider recommends taking any type of supplement or vitamin, a pharmacist can recommend types that do not contain copper.
People should talk with a health care provider about diet changes to reduce copper intake.
Liver Transplant
A liver transplant may be necessary in people when:
- cirrhosis leads to liver failure
- acute liver failure happens suddenly
- treatment is not effective
A liver transplant is an operation to remove a diseased or an injured liver and replace it with a healthy one from another person, called a donor. A successful transplant is a life-saving treatment for people with liver failure. Most transplanted livers come from donors who have died. But in some cases a liver can come from a living donor, such as a family member. In that case, the surgeon removes your diseased liver and replaces it with a portion of the donor’s liver.
Most liver transplants are successful. About 85 percent of transplanted livers are functioning after 1 year 37. Liver transplant surgery provides a cure for Wilson disease in most cases.
References- Compston A. Progressive lenticular degeneration: A familial nervous disease associated with cirrhosis of the liver, by S. A. Kinnier Wilson, (From the National Hospital, and the Laboratory of the National Hospital, Queen Square, London) Brain 1912: 34; 295–509. Brain. 2009;132:1997–2001. doi: 10.1093/brain/awp193
- Collins JF. Copper. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014:206-16.
- Hellman NE, Gitlin JD. Ceruloplasmin metabolism and function. Annu Rev Nutr. 2002;22:439-58. https://doi.org/10.1146/annurev.nutr.22.012502.114457
- Prohaska JR. Copper. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:540-53.
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington, DC: National Academies Press; 2001.
- European Association for Study of Liver EASL clinical practice guidelines: Wilson’s disease. J. Hepatol. 2012;56:671–685. doi: 10.1016/j.jhep.2011.11.007
- Litwin T., Gromadzka G., Szpak G., Jabłonka-Salach K., Bulska E., Członkowska A. Brain metal accumulation in Wilson’s disease. J. Neurol. Sci. 2013;329:55–58. doi: 10.1016/j.jns.2013.03.021
- Shribman S., Bocchetta M., Sudre C.H., Acosta-Cabronero J., Burrows M., Cook P., Thomas D.L., Gillett G.T., Tsochatzis E.A., Bandmann O., et al. Neuroimaging correlates of brain injury in Wilson’s disease: A multimodal, whole-brain MRI study. Brain. 2022;145:263–275. doi: 10.1093/brain/awab274
- Dzieżyc K., Litwin T., Członkowska A. Other organ involvement and clinical aspects of Wilson disease. Handb. Clin. Neurol. 2017;142:157–169. doi: 10.1016/b978-0-444-63625-6.00013-6
- Rosencrantz R, Schilsky M. Wilson disease: pathogenesis and clinical considerations in diagnosis and treatment. Seminars in Liver Disease. 2011;31:245–259.
- Chaudhry HS, Anilkumar AC. Wilson Disease. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441990
- Sullivan CA, Chopdar A, Shun-Shin GA. Dense Kayser-Fleischer ring in asymptomatic Wilson’s disease (hepatolenticular degeneration). British Journal of Ophthalmology 2002;86:114. https://bjo.bmj.com/content/86/1/114.1
- Stremmel W, Weiskirchen R. Therapeutic strategies in Wilson disease: pathophysiology and mode of action. Ann Transl Med. 2021 Apr;9(8):732. doi: 10.21037/atm-20-3090
- Tanzi RE, Petrukhin K, Chernov I, et al. The Wilson disease gene is a copper transporting ATPase with homology to the Menkes disease gene. Nat Genet 1993;5:344-50.
- Bandmann O, Weiss KH, Kaler SG. Wilson’s disease and other neurological copper disorders. Lancet Neurol. 2015 Jan;14(1):103-13. doi: 10.1016/S1474-4422(14)70190-5
- Coffey AJ, Durkie M, Hague S, McLay K, Emmerson J, Lo C, Klaffke S, Joyce CJ, Dhawan A, Hadzic N, Mieli-Vergani G, Kirk R, Elizabeth Allen K, Nicholl D, Wong S, Griffiths W, Smithson S, Giffin N, Taha A, Connolly S, Gillett GT, Tanner S, Bonham J, Sharrack B, Palotie A, Rattray M, Dalton A, Bandmann O. A genetic study of Wilson’s disease in the United Kingdom. Brain. 2013 May;136(Pt 5):1476-87. doi: 10.1093/brain/awt035
- Definition & Facts for Wilson Disease. https://www.niddk.nih.gov/health-information/liver-disease/wilson-disease/definition-facts
- Kanwar P, Kowdley KV. Metal storage disorders: Wilson disease and hemochromatosis. Med Clin North Am. 2014 Jan;98(1):87-102. doi: 10.1016/j.mcna.2013.09.008
- Kim JW, Kim JH, Seo JK, Ko JS, Chang JY, Yang HR, Kang KH. Genetically confirmed Wilson disease in a 9-month old boy with elevations of aminotransferases. World J Hepatol. 2013 Mar 27;5(3):156-9. doi: 10.4254/wjh.v5.i3.156
- Avan A, Członkowska A, Gaskin S, Granzotto A, Sensi SL, Hoogenraad TU. The Role of Zinc in the Treatment of Wilson’s Disease. Int J Mol Sci. 2022 Aug 18;23(16):9316. doi: 10.3390/ijms23169316
- Stremmel W, Meyerrose KW, Niederau C, et al. Wilson disease: clinical presentation, treatment and survival. Ann Intern Med 1991;115:720-6. 10.7326/0003-4819-115-9-720
- Beinhardt S, Leiss W, Stättermayer AF, et al. Long-term outcomes of patients with Wilson disease in a large Austrian cohort. Clin Gastroenterol Hepatol 2014;12:683-9. 10.1016/j.cgh.2013.09.025
- Nazer H, Ede RJ, Mowat AP, Williams R. Wilson’s disease: clinical presentation and use of prognostic index. Gut. 1986 Nov;27(11):1377-81. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1434058/pdf/gut00371-0105.pdf
- Guillaud O, Dumortier J, Sobesky R, Debray D, Wolf P, Vanlemmens C, Durand F, Calmus Y, Duvoux C, Dharancy S, Kamar N, Boudjema K, Bernard PH, Pageaux GP, Salamé E, Gugenheim J, Lachaux A, Habes D, Radenne S, Hardwigsen J, Chazouillères O, Trocello JM, Woimant F, Ichai P, Branchereau S, Soubrane O, Castaing D, Jacquemin E, Samuel D, Duclos-Vallée JC. Long term results of liver transplantation for Wilson’s disease: experience in France. J Hepatol. 2014 Mar;60(3):579-89. doi: 10.1016/j.jhep.2013.10.025
- Tanzi R.E., Petrukhin K., Chernov I., Pellequer J.L., Wasco W., Ross B., Romano D.M., Pavone L., Brzustowicz L.M. The Wilson disease gene is a copper transporting ATPase with homology to the Menkes disease gene. J. Nat. Genet. 1993;5:344–350. doi: 10.1038/ng1293-344
- Gouider-Khouja N. Wilson’s disease. Parkinsonism Relat. Disord. 2009;15:126–129. doi: 10.1016/S1353-8020(09)70798-9
- Chaudhry HS, Anilkumar AC. Wilson Disease. [Updated 2023 Jan 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441990
- Park S, Park JY, Kim GH, et al. Identification of novel ATP7B gene mutations and their functional roles in Korean patients with Wilson disease. Hum Mutat 2007;28:1108-13. 10.1002/humu.20574
- Terada K, Schilsky ML, Miura N, et al. ATP7B (WND) protein. Int J Biochem Cell Biol 1998;30:1063-7. 10.1016/S1357-2725(98)00073-9
- Parisi S, Polishchuk EV, Allocca S, et al. Characterization of the most frequent ATP7B mutation causing Wilson disease in hepatocytes from patient induced pluripotent stem cells. Sci Rep 2018;8:6247. 10.1038/s41598-018-24717-0
- Dong Q.Y., Wu Z.Y. Advance in the pathogenesis and treatment of Wilson disease. Transl. Neurodegener. 2012 doi: 10.1186/2047-9158-1-23
- Wu F, Wang J, Pu C, Qiao L, Jiang C. Wilson’s disease: a comprehensive review of the molecular mechanisms. Int J Mol Sci. 2015 Mar 20;16(3):6419-31. doi: 10.3390/ijms16036419
- Wilson’s Disease/Kayser Fleischer Ring. http://eyewiki.org/Wilson%27s_Disease/Kayser_Fleischer_Ring
- Hoogenraad T.U. Paradigm shift in treatment of Wilson’s disease: Zinc therapy now treatment of choice. Brain Dev. 2006;28:141–146. doi: 10.1016/j.braindev.2005.08.008
- Askari F.K., Greenson J., Dick R.D., Johnson V.D., Brewer G.J. Treatment of Wilson’s disease with zinc. XVIII. initial treatment of the hepatic decompensation presentation with trientine and zinc. J. Lab. Clin. Med. 2003;142:385–390. doi: 10.1016/S0022-2143(03)00157-4
- U.S. Department of Agriculture, Agricultural Research Service. FoodData Central. https://fdc.nal.usda.gov
- Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR). OPTN/SRTR 2011 annual data report. Department of Health and Human Services. Health Resources and Services Administration. Healthcare Systems Bureau, Division of Transplantation https://srtr.transplant.hrsa.gov/annual_reports/2011/