Wolfram syndrome
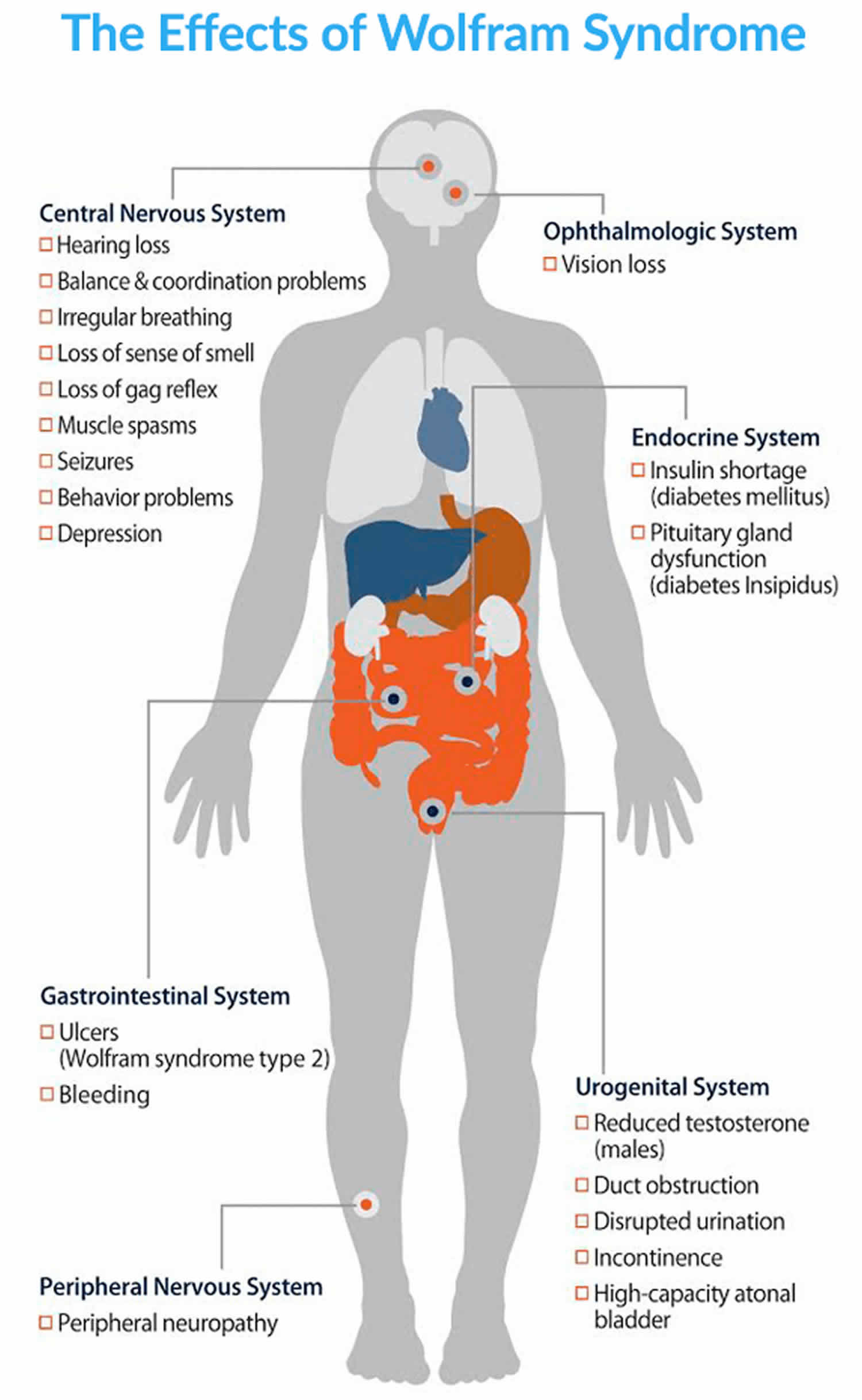
Wolfram syndrome is a rare inherited condition that is typically associated with childhood-onset insulin-dependent diabetes mellitus, progressive optic nerve atrophy and progressive neurodegeneration, especially brain stem and cerebellar atrophy 1, 2, 3, 4, 5. In addition, many people with Wolfram syndrome also develop diabetes insipidus and sensorineural hearing loss. An older name for Wolfram syndrome is “DIDMOAD“, which refers to diabetes insipidus (DI), diabetes mellitus (DM), optic nerve atrophy (OA), and deafness (D) 1. The hallmark features of Wolfram syndrome are high blood sugar levels resulting from a shortage of the hormone insulin (diabetes mellitus) and progressive vision loss due to degeneration of the optic nerves that carry information from the eyes to the brain (optic atrophy). People with Wolfram syndrome often also have pituitary gland dysfunction that results in the excretion of excessive amounts of urine (diabetes insipidus), hearing loss caused by changes in the inner ear (sensorineural deafness), urinary tract problems, reduced amounts of the sex hormone testosterone in males (hypogonadism), or neurological or psychiatric disorders 6.
Diabetes mellitus is typically the first symptom of Wolfram syndrome, usually diagnosed around age 6. Nearly everyone with Wolfram syndrome who develops diabetes mellitus requires insulin replacement therapy. Optic atrophy is often the next symptom to appear, usually around age 11. The first signs of optic atrophy are loss of color vision and side (peripheral) vision. Over time, the vision problems get worse, and people with optic atrophy are usually blind within approximately 8 years after signs of optic atrophy first begin.
In diabetes insipidus, the pituitary gland, which is located at the base of the brain, does not function normally. This abnormality disrupts the release of a hormone called vasopressin, which helps control the body’s water balance and urine production. Approximately 70 percent of people with Wolfram syndrome have diabetes insipidus. Pituitary gland dysfunction can also cause hypogonadism in males. The lack of testosterone that occurs with hypogonadism affects growth and sexual development. About 65 percent of people with Wolfram syndrome have sensorineural deafness that can range in severity from deafness beginning at birth to mild hearing loss beginning in adolescence that worsens over time. Sixty to 90 percent of people with Wolfram syndrome have a urinary tract problem. Urinary tract problems include obstruction of the ducts between the kidneys and bladder (ureters), a large bladder that cannot empty normally (high-capacity atonal bladder), disrupted urination (bladder sphincter dyssynergia), and difficulty controlling the flow of urine (incontinence).
About 60 percent of people with Wolfram syndrome develop a neurological or psychiatric disorder, most commonly problems with balance and coordination (ataxia), typically beginning in early adulthood. Other neurological problems experienced by people with Wolfram syndrome include irregular breathing caused by the brain’s inability to control breathing (central apnea), loss of the sense of smell, loss of the gag reflex, muscle spasms (myoclonus), seizures, reduced sensation in the lower extremities (peripheral neuropathy), and intellectual impairment. Psychiatric disorders associated with Wolfram syndrome include psychosis, episodes of severe depression, and impulsive and aggressive behavior.
Since diabetes mellitus and optic atrophy usually begin before the age of 16, Wolfram syndrome is typically diagnosed in childhood to adolescence. However, onset of key symptoms or the genetic confirmation can come much later in some patients. Wolfram syndrome affects males and females in equal numbers.
There are two types of Wolfram syndrome (Wolfram syndrome type 1 and Wolfram syndrome type 2) with many overlapping features. The two types are differentiated by their genetic cause. Wolfram syndrome type 1 is caused by changes (mutations) in the WFS1 gene, while Wolfram syndrome type 2 is caused by mutations in the CISD2 gene. Some people have mutations in the same gene that causes Wolfram syndrome but they do not get all the features of the syndrome, so they are said to have Wolfram syndrome type 1-related disorders. For example, this name would be used to describe someone with severe sensorineural hearing loss caused by WFS1 gene mutations but without diabetes or other features. In addition to the usual features of Wolfram syndrome, individuals with Wolfram syndrome type 2 have stomach or intestinal ulcers and excessive bleeding after an injury. The tendency to bleed excessively combined with the ulcers typically leads to abnormal bleeding in the gastrointestinal system. People with Wolfram syndrome type 2 do not develop diabetes insipidus.
Wolfram syndrome is often fatal by mid-adulthood due to complications from the many features of the condition, such as health problems related to diabetes mellitus or neurological problems.
The estimated prevalence of Wolfram syndrome type 1 is 1 in 500,000-770,000 people worldwide 7, 8. Medical experts estimate between 15,000 and 30,000 patients worldwide have Wolfram syndrome, including 114-150 in the UK 9. Only a few families from Jordan have been found to have Wolfram syndrome type 2.
Wolfram syndrome is often fatal by mid-adulthood (average lifespan 30 to 40 years) due to complications from the various health problems associated with the condition, usually from respiratory failure as a result of brain stem atrophy 10, 8, 11.
Figure 1. Wolfram syndrome
[Source 12 ]What is diabetes mellitus?
Most people (87%) affected by Wolfram syndrome develop insulin-dependent diabetes mellitus before the age of 16 1. Diabetes mellitus is the scientific name for diabetes, is a disease that occurs when your blood sugar, also called blood glucose, is too high (hyperglycemia) due to an inability to produce enough hormone called insulin and/or to respond to insulin. Over time, having too much sugar (glucose) in your blood can cause health problems, such as heart disease, nerve damage, eye problems, and kidney disease. There are two main types of diabetes mellitus: type 1 diabetes and type 2 diabetes.
Type 1 diabetes previously known as juvenile diabetes or insulin-dependent diabetes mellitus (IDDM), is an autoimmune condition characterized by high blood sugar levels (high blood glucose or hyperglycemia) that occurs when your body’s immune system attacks the insulin-producing beta cells in your pancreas (an organ behind your stomach) and destroys them. The pancreas then produces little or no insulin. When you eat, your body breaks down sugar and starches from food into glucose (sugar) to use for energy. Your pancreas makes a hormone called insulin that controls the amount of glucose (sugar) in your blood. Insulin helps glucose (sugar) produced by the digestion of carbohydrates move from your blood into your body’s cells where it can be used for energy. When you have type 1 diabetes, your body doesn’t make enough insulin or no insulin, so the glucose (sugar) cannot enter your body’s cells and you end up with too much sugar in your blood (hyperglycemia). People with type 1 diabetes depend on insulin every day of their lives to replace the insulin their body cannot produce. People with type 1 diabetes must monitor their glucose levels throughout the day to ensure they stay within their target glucose range. This can be done using a blood glucose monitor or continuous glucose monitor.
Type 2 diabetes develops when your body does not use insulin efficiently and gradually loses the ability to make enough insulin. In type 2 diabetes, there are primarily two interrelated problems at work – 1) your pancreas does not produce enough insulin and 2) your body’s cells respond poorly to insulin and take in less sugar. When you eat, your body breaks down sugar and starches from food into glucose to use for energy. Your pancreas (an organ behind your stomach) makes a hormone called insulin that controls the amount of glucose (sugar) in your blood. Insulin helps glucose (sugar) produced by the digestion of carbohydrates move from the blood into your body’s cells where it can be used for energy. When you have type 2 diabetes, your body doesn’t make enough insulin or can’t use insulin well, so you end up with too much sugar in your blood. In type 2 diabetes, the body’s cells do not respond effectively to insulin. This is known as insulin resistance, it causes glucose (sugar) to stay in your blood, leading to a higher than normal level of glucose in your blood (also known as hyperglycemia, usually above 7 mmol/L [126 mg/dL] before a meal and above 8.5 mmol/L [153 mg/dL] two hours after a meal) and not enough reaches your cells. The normal blood sugar level is between 4.0 mmol/L (72 mg/dL) and 5.5 mmol/L (99 mg/dL) when fasting (before meals), and less than 7.0 mmol/L [126 mg/dL] 2 hours after a meal. Eventually, high blood sugar levels can lead to serious health problems, like heart disease, kidney failure, blindness and disorders of the immune systems. People who have type 2 diabetes are also at greater risk of developing cardiovascular diseases such as heart attack, stroke or problems with circulation in their legs and feet (peripheral artery disease). These are the “macrovascular” complications of diabetes. “Macrovascular” means that these complications affect the larger blood vessels. This risk is especially high in people who also have high blood pressure.
If you’re diagnosed with diabetes, you’ll need to eat healthily, take regular exercise and carry out regular blood tests to ensure your blood glucose levels stay balanced.
Over time, having too much sugar (glucose) in your blood can cause health problems, such as heart disease, nerve damage, eye problems, and kidney disease. If you’re diagnosed with diabetes, you’ll need to eat healthily, take regular exercise and carry out regular blood tests to ensure your blood glucose levels stay balanced.
What is diabetes insipidus?
About 42% of people who have Wolfram syndrome also develop diabetes insipidus. Diabetes insipidus is caused by a problem with vasopressin hormone (arginine vasopressin [AVP]) or antidiuretic hormone (ADH) production in the pituitary gland (central diabetes insipidus) or decreased ability of the kidneys to concentrate urine because of resistance to antidiuretic hormone (ADH) action in the kidneys (nephrogenic diabetes insipidus) 13. Based on the site of the pathology, diabetes insipidus can be divided into central diabetes insipidus (characterized by decreased production of antidiuretic hormone [ADH] in a part of your brain called the hypothalamus and is secreted into the blood by the posterior pituitary gland) and nephrogenic diabetes insipidus (resistance to antidiuretic hormone [ADH] action in your kidneys) 13. Antidiuretic hormone (ADH) or vasopressin hormone (AVP) primarily helps your blood vessels constrict (become narrower) and helps your kidneys control the amount of water and salt in your body. This helps control blood pressure and the amount of urine that is made. Anti-diuretic hormone (ADH) most important role is to conserve the fluid volume of your body by reducing the amount of water passed out in your urine. Anti-diuretic hormone (ADH) does this by allowing water in your urine to be taken back into your body in a specific area of the kidney. Thus, more water returns to your bloodstream, urine concentration rises and water loss is reduced. Higher concentrations of anti-diuretic hormone (ADH) cause blood vessels to constrict (become narrower) and this increases blood pressure. A deficiency of body fluid (dehydration) can only be finally restored by increasing water intake.
People with Wolfram syndrome have central diabetes insipidus because the posterior pituitary gland in their head is not making enough of the antidiuretic hormone (ADH) or vasopressin hormone (AVP) 12, 14. Because of the lack of vasopressin hormone (AVP) or antidiuretic hormone (ADH) production in the pituitary gland, the low levels of anti-diuretic hormone (ADH) will cause the kidneys to excrete too much water. Urine volume will increase leading to dehydration and excessive thirst and a fall in blood pressure. Patients tend to drink enormous quantities of fluid and urinate very often. Other symptoms may be dehydration, weakness, dryness of the mouth, and sometimes constipation, which may develop rapidly if the loss of fluid is not continuously replaced. Diabetes insipidus can be treated with vasopressin hormone replacement called Desmopressin (DDAVP) tablet or nasal sprays 15, 16.
What is optic atrophy?
Optic atrophy means death of the optic nerve. The vision impairment in Wolfram syndrome is a problem in neuronal cells in the eyes transferring the electrical signal produced in the eye to the brain. It is caused by neuronal cell death and called optic atrophy. Symptoms often present as difficulty seeing in the classroom at school or everything going grey. There is currently no treatment for optic atrophy.
Wolfram syndrome causes
Mutations in the Wolfram syndrome 1 (WFS1) gene cause more than 90 percent of Wolfram syndrome type 1 cases 2. Wolfram syndrome 1 (WFS1) gene provides instructions for producing a protein called wolframin that is thought to regulate the amount of calcium in cells. A proper calcium balance is important for many different cellular functions, including cell-to-cell communication, the tensing (contraction) of muscles, and protein processing. The wolframin protein is found in many different tissues, such as the pancreas, brain, heart, bones, muscles, lung, liver, and kidneys. Within cells, wolframin is located in the membrane of a cell structure called the endoplasmic reticulum that is involved in protein production, processing, and transport. Wolframin’s function is important in the pancreas, where the protein is thought to help process a protein called proinsulin into the mature hormone insulin. This hormone helps control blood sugar levels.
WFS1 gene mutations lead to the production of a wolframin protein that has reduced or absent function. As a result, calcium levels within cells are not regulated and the endoplasmic reticulum does not work correctly. When the endoplasmic reticulum does not have enough functional wolframin, the cell triggers its own cell death (apoptosis). The death of cells in the pancreas, specifically cells that make insulin (beta cells), causes diabetes mellitus in people with Wolfram syndrome. The gradual loss of cells along the optic nerve eventually leads to blindness in affected individuals. The death of cells in other body systems likely causes the various signs and symptoms of Wolfram syndrome type 1.
A certain mutation in the CDGSH iron sulfur domain protein 2 (CISD2) gene was found to cause Wolfram syndrome type 2 2. The CISD2 gene provides instructions for making a protein that is located in the outer membrane of cell structures called mitochondria. Mitochondria are the energy-producing centers of cells. The exact function of the CISD2 protein is unknown, but it is thought to help keep mitochondria functioning normally.
The CISD2 gene mutation that causes Wolfram syndrome type 2 results in an abnormally small, nonfunctional CISD2 protein. As a result, mitochondria are not properly maintained, and they eventually break down. Since the mitochondria provide energy to cells, the loss of mitochondria results in decreased energy for cells. Cells that do not have enough energy to function will eventually die. Cells with high energy demands such as nerve cells in the brain, eye, or gastrointestinal tract are most susceptible to cell death due to reduced energy. It is unknown why people with CISD2 gene mutations have ulcers and bleeding problems in addition to the usual Wolfram syndrome features.
Some people with Wolfram syndrome do not have an identified mutation in either the WFS1 or CISD2 gene. The cause of the condition in these individuals is unknown 17.
Wolfram syndrome inheritance pattern
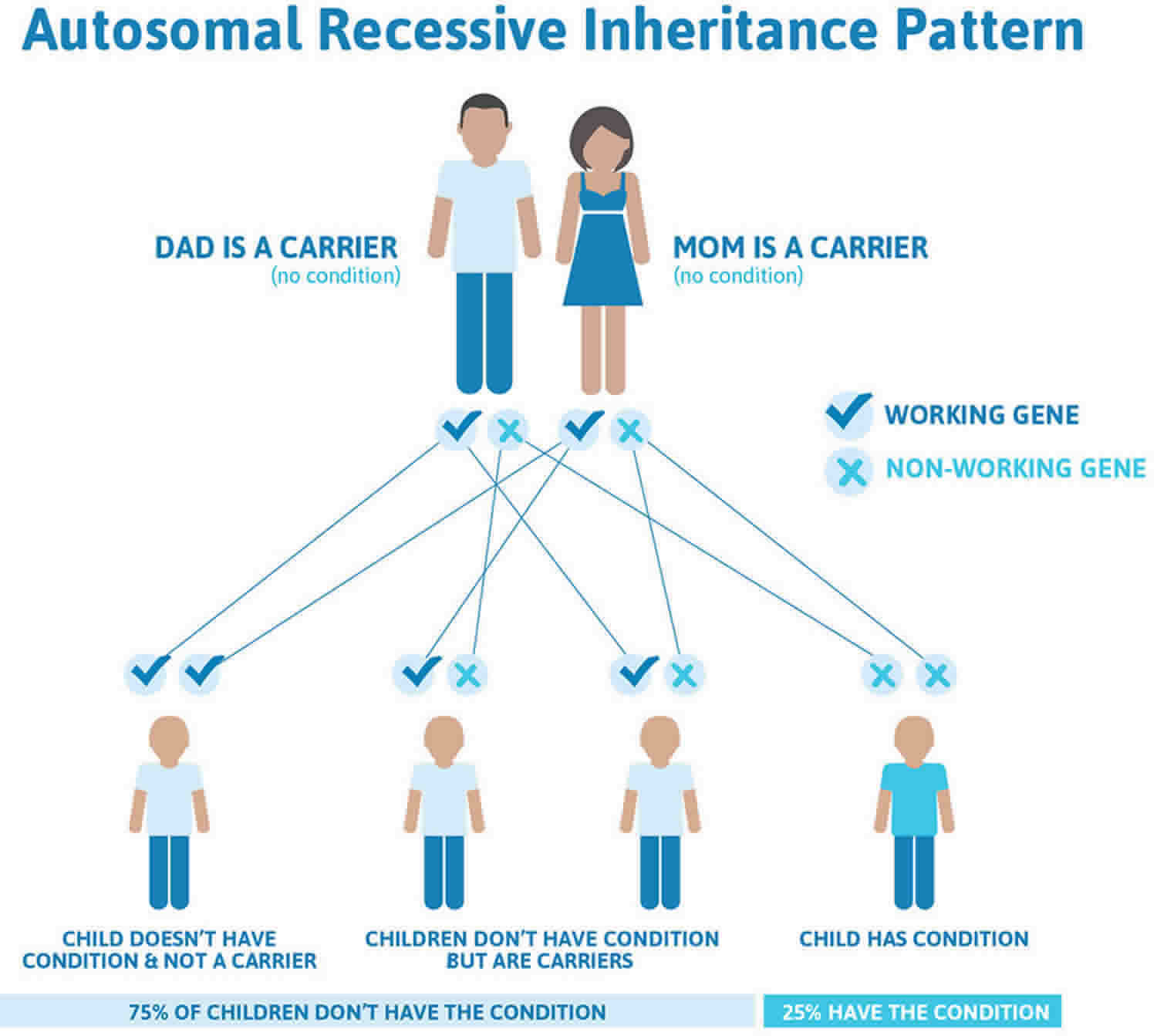
Wolfram syndrome type 1 is caused by mutations in the WFS1 gene, it is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition. Some studies have shown that people who carry one copy of a WFS1 gene mutation are at increased risk of developing individual features of Wolfram syndrome or related features, such as type 2 diabetes, hearing loss, or psychiatric illness. However, other studies have found no increased risk in these individuals.
Wolfram syndrome type 2 is caused by mutations in the CISD2 gene is also inherited in an autosomal recessive pattern.
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
Figure 2 illustrates autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 2. Wolfram syndrome autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Wolfram syndrome symptoms
The symptoms and rate of progression of Wolfram syndrome can be quite variable. The primary symptoms of Wolfram syndrome type 1 (diabetes mellitus, optic nerve atrophy, diabetes insipidus and hearing loss, which is also known by the acronym DIDMOAD ) can emerge at different ages and change at different rates. Diabetes mellitus is typically the first symptom, usually diagnosed around age 6 8. Optic nerve atrophy, marked by loss of color vision and peripheral vision, follows around age 11 8. Central diabetes insipidus is another common symptom, affecting approximately 70 % of Wolfram patients 8. Around 65 % of patients develop sensorineural deafness that can range in severity from deafness beginning at birth to mild hearing loss beginning in adolescence that worsens over time 8, 11. Urinary tract problems are another major clinical challenge for Wolfram syndrome patients affecting 60 to 90 % of this population 2. These problems include obstruction of the ureters between the kidneys and bladder, high-capacity atonal bladder, disrupted urination, bladder sphincter dyssynergia, and difficulty controlling urine flow 8. More than 60 % of patients with Wolfram syndrome develop neurological symptoms, most commonly presenting as problems with balance and coordination (ataxia) beginning in early adulthood. Brain stem atrophy is also a prominent feature that often results in death secondary to central apnea 8, 18, 19. About 65% of affected people will develop all four of these symptoms, while others will only have some of the associated health problems 20. If some of these symptoms never appear at all, such as sensorineural hearing loss without diabetes or other features, the patient would have a “WFS1-related disorder” or “Wolfram-like” but not Wolfram syndrome 9 1. Dr. Urano at Washington University and Dr. Hattersley at the University of Exeter have identified several dominant de novo Wolfram syndrome 1 (WFS1) variants associated with a genetic syndrome of neonatal/infancy-onset diabetes, congenital sensorineural deafness, and congenital cataracts, these patients would have a “WFS1-related disorder” or “Wolfram-like” but not Wolfram syndrome 9 1.
Other signs and symptoms of Wolfram syndrome type 1 may include:
- Urinary tract abnormalities
- Ataxia (problems with coordination and balance)
- Loss of sense of smell
- Loss of gag reflex
- Myoclonus (muscle spasms)
- Decreased sensation in some parts of the body (peripheral neuropathy)
- Seizures
- Depression
- Impulsive and/or aggressive behavior
- Psychosis
- Gastrointestinal problems
- Intellectual disability
- Irregular breathing due to lack of brain’s inability to control breathing (central apnea) and central respiratory failure
- Hypogonadism in males (reduced amounts of the sex hormone testosterone)
In addition to the signs and symptoms found in Wolfram syndrome type 1, people with Wolfram syndrome type 2 may also have stomach and/or intestinal ulcers; and a tendency to bleed excessively after injuries 21.
Most of those affected by Wolfram syndrome develop insulin-dependent diabetes mellitus before the age of 16 (87%). The starches and sugars (carbohydrates) in the foods we eat are normally processed by the digestive system into glucose that circulates in the blood as one energy source for body functions. A hormone produced by the pancreas (insulin) allows muscle and fat cells to take up glucose. In diabetes mellitus, the pancreas does not make enough insulin so the cells cannot take up glucose normally and the blood sugar gets too high. As a result, the patient needs daily injections of insulin to control the blood sugar. Symptoms of diabetes may include frequent urination, excessive thirst, increased appetite, weight loss, and blurred vision.
In addition, it is thought that almost all of those affected by Wolfram syndrome have primary optic atrophy (OA) and subsequent vision impairment before the age of 16 (80%). The optic nerve conducts visual information to the brain for processing. Loss of the nerve fibers and/or their insulation (myelin) results in color blindness and reduced vision typically beginning in childhood and progressing with age, though some progress quickly and others slowly.
Some people who have Wolfram syndrome also develop diabetes insipidus (42%). This is not related to diabetes or insulin. The only thing it has in common with diabetes are the symptoms of excessive thirst and urination. This condition results in excretion of large quantities of very watery-appearing urine and excessive thirst. Patients tend to drink enormous quantities of fluid and urinate very often. Other symptoms may be dehydration, weakness, dryness of the mouth, and sometimes constipation that may develop rapidly if the loss of fluid is not continuously replaced.
Hearing loss is the fourth major symptom of Wolfram syndrome and occurs in approximately 48% of patients. This symptom may occur at any time, and may be partial or complete. The hearing loss is due to a loss of sound perception transmitted by nerves (sensorineural). Symptoms may include loss of sound intensity or pitch, or loss of the ability to hear high tones.
Some of the following additional symptoms may develop:
- Urinary tract abnormalities (33%) – this is most often a problem with the bladder not emptying properly, so that the person needs to empty often. This symptom may be confused or complicated by diabetes insipidus, so both need to be checked if a person with Wolfram syndrome is having frequent urination.
- Neurological symptoms such as poor smell, poor balance, an awkward way of walking (ataxia) and central sleep apnea can occur. In addition, imaging of the brain reveals that people with Wolfram syndrome have smaller brainstem and cerebellum volumes and smaller optic nerves than those without Wolfram syndrome. These differences may increase over time.
- Psychiatric and behavioral problems such as depression, anxiety and fatigue can occur in patients with Wolfram syndrome (26%). These symptoms may be related to the changes in the nervous system from Wolfram syndrome itself or to the psychological and quality of life burden caused by the effects of the disease.
- Disordered sleep may be a problem and can be due to central sleep apnea or to frequent waking to urinate.
Other problems that may occur:
- Lowered production of testosterone (hypogonadism) in males (6%)
- Gastrointestinal disorders (5%) – including constipation, trouble swallowing, choking, diarrhea.
- Bilateral clouding of the lens of the eyes (cataracts) (1%)
- Temperature regulation (e.g. overheating).
Wolfram syndrome diagnosis
Wolfram syndrome is difficult to diagnose. In many instances, people with this disorder and their doctors may be unaware that the various symptoms and complaints are related and indicate a specific disorder. Initially, the focus may be on one symptom, typically diabetes mellitus, and its treatment. Later, the presence of other symptoms may become apparent. Wolfram syndrome should be considered in anyone with diabetes mellitus and optic nerve atrophy; anyone with low frequency sensorineural hearing loss; anyone with either diabetes mellitus or optic atrophy in addition to hearing loss or diabetes insipidus or bladder dysfunction or loss of sense of smell or a family member with Wolfram syndrome.
Molecular genetic testing for mutations in the WFS1 and WFS2 genes is available to confirm the diagnosis.
Table 1. Recommended evaluations following initial diagnosis in individuals with Wolfram syndrome
| System/Concern | Evaluation | Comment | |
|---|---|---|---|
| Diabetes mellitus | By diabetologist | ||
| Optic atrophy | Ophthalmologic evaluation | Assess extraocular movement, best corrected visual acuity, visual evoked potentials. Perform color vision testing, visual field testing, optical coherence tomography, fundus exam. | |
| Optometry &/or low-vision clinic | Assess for low-vision aids. | ||
| Sensorineural hearing impairment | Audiologic exam Evaluation by speech-language therapist | Incl: Auditory brain stem responses to confirm pathology & provide baseline Evoked otoacoustic emissions to identify type of hearing impairment Audiogram Speech discrimination tests Assessment for hearing aids; children w/profound infancy-onset deafness may require cochlear implant. | |
| Neurologic dysfunction | Neurologic exam include brain MRI (if not performed previously) | Evaluate for: Motor system: coordination, balance, ataxia Sensory system: peripheral neuropathy Cranial nerves: anosmia, ability to taste, dysarthria, swallowing/choking difficulties, apneic episodes Autonomic system: hypotensive episodes, abnormal temperature regulation &/or sweating episodes Consider speech-language therapy, occupational therapy, physical therapy assessments. | |
| Respiratory function | Polysomnography | Central apnea can occur secondary to brain stem atrophy. Sleep disturbance is common & multicausal. | |
| Psychiatric | Neuropsychiatric evaluation | Consider anxiety, depression eval. Although reported, psychoses are rare. | |
| Neurogenic bladder | History of: urgency, frequency, difficulty voiding, urinary incontinence, recurrent infections | Refer to urologist. Consider urodynamic evaluation, imaging of urinary tract & kidneys for dilated ureters, & assessment of renal function. | |
| Bowel dysfunction | History of: constipation, urgency, accidents | ||
| Other endocrine findings | Diabetes insipidus | Assess concentrating ability of urine. | Paired early morning urine & fasting plasma osmolarity & sodium concentrations after nocturnal & morning euglycemia |
| Hypogonadism | Evaluate for absent or delayed puberty &/or infertility | Refer for assessment for primary gonadal failure &/or hypogonadotropic hypogonadism. | |
| Hypothyroidism | Thyroid function tests | May be non-autoimmune | |
| Growth restriction | Plot height, weight, & head circumference on standard growth charts. | To identify growth failure &/or provide baseline | |
| Genetic counseling | By medical genetics health care professionals 1 | To inform affected persons & families re nature, mode of inheritance, & implications of Wolfram spectrum disorder | |
| Family support & resources | Contact with patient advocacy organization Assess need for social work involvement for caregiver support. Assess need for help coordinating multidisciplinary care. Assess need for community resources & support/advocacy organizations (e.g., Parent to Parent). | ||
1 Medical geneticist, certified genetic counselor, certified advanced genetic nurse
[Source 22 ]Wolfram syndrome treatment
Treatment of Wolfram syndrome is symptomatic and supportive. It requires a multidisciplinary effort to manage the various aspects of this condition. When diabetes mellitus is present, the patient will need insulin treatment. Diabetes insipidus can be difficult to diagnose and may need to be treated with intranasal or oral vasopressin. Treatment of diabetes insipidus in Wolfram may be very complicated as the person may also have diabetes mellitus and bladder dysfunction. Patients with hearing loss may benefit from hearing aids or cochlear implants as well as accommodations for hearing loss. All patients should be followed closely by an eye doctor (ophthalmologist) and may need glasses or other accommodations for low vision such as large print reading materials, high contrast visuals at school or work, allowances for colorblindness, etc. Occupational therapy may be helpful in some cases. Regular evaluation of the bladder is important to detect poor bladder emptying. Psychological evaluation and care is important for many, particularly with school performance issues. Treatment of constipation, diarrhea, and trouble swallowing may be needed. Sleep should be monitored and sleep apnea considered. Patients may have trouble tolerating high or low temperatures and may need accommodations for air conditioning or heating.
Genetic counseling is recommended for Wolfram syndrome patients and their families.
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Table 2. Treatment of individuals with Wolfram syndrome
| Manifestation/Concern | Treatment | Considerations/Other | |
|---|---|---|---|
| Diabetes mellitus | Routine practice for insulin-dependent diabetes mellitus |
| |
| Optic atrophy | Correction of refractive error | ||
| Low-vision services |
| ||
| Sensorineural hearing impairment | Treatment of sensorineural hearing loss depends on degree of hearing impairment. 2 | ||
| Activities of daily living | Vision impairment support | Communication training (e.g., Braille), walking aids | |
| Occupational therapist |
| ||
| Dysphagia | Speech-language therapist |
| |
| Dentist/dental hygienist | Attention to oral hygiene & dental care | ||
| Dysarthria | Speech-language pathologist | Help maintain vocal control, improve speech, teach breathing techniques, & assist communication in general. | |
| Central apnea | Respiratory team | Options incl overnight noninvasive ventilatory support. | |
| Psychiatric | Per standard treatment by psychiatric professional (psychiatrist, psychologist, neuropsychologist) as needed | Pharmacologic & non-pharmacologic therapies available. | |
| Neurogenic bladder | Anticholinergic drugs Clean intermittent self-catheterization or indwelling catheter Treatment of recurrent urinary tract infections |
| |
| Bowel dysfunction | Dietary management | In conjunction with bladder dysfunction | |
| Other endocrine findings | Diabetes insipidus | Per standard treatment | Care with arginine vasopressin replacement to avoid hyper-/hyponatremia |
| Hypogonadism | Hormone replacement therapy | ||
| Hypothyroidism | Thyroid hormone replacement | ||
| Growth restriction | Evaluate for growth hormone supplementation according to national guidelines for growth hormone therapy. | ||
| Transition of care to adult service providers | Assess understanding of illness, capacity for independent life skills |
| |
| Family/Community |
| Consider support with adaptive sports, higher education, & employment opportunities. | |
Table 3. Recommended surveillance for individuals with Wolfram syndrome
| System/Concern | Evaluation | Frequency | |
|---|---|---|---|
| Diabetes mellitus | Glycemic control | Every 3 months | |
| Complications of diabetes mellitus | Nephropathy | Annual screening starting at age 12 years | |
| Retinopathy | In those w/duration of diabetes ≥5 years: annual screening | ||
| Neuropathy | Annual screening for parathethesias | ||
| Dyslipidemia screen | Annually | ||
| Hypertension | At least annually | ||
| Optic atrophy |
| Annually | |
| Sensorineural hearing impairment | Audiogram incl assessment of speech discrimination | Every 1-2 years | |
| Neurologic | Neurologic exam incl assessment of cerebellar ataxia as well as memory, personality changes | ||
| Activities of daily living & mobility | Physical medicine, occupational therapy/physical therapy assessment of mobility, self-help skills | Per treating clinicians | |
| Dysphagia | For those without this concern previously: obtain history of swallowing/choking episodes & refer to speech-language therapist as needed. | Annually | |
| For those known to have this concern | Per treating speech-language therapist | ||
| Dysarthria | For those without this concern previously: obtain history of speech difficulties & refer to speech-language therapist as needed. | Annually | |
| For those known to have this concern | Per treating speech-language therapist | ||
| Development in young children | Monitor educational needs. | Annually in childhood | |
| Cognitive decline / Intellectual disability | Per treating clinician | As clinically indicated | |
| Psychiatric/Behavioral | Assess for symptoms of depression, suicidal behavior, & changes in personal appearance & social behavior | Per treating clinician | |
| Neurogenic bladder |
| Annually | |
| Other endocrine findings | Diabetes insipidus | Assess concentrating ability of urine. | Per treating clinician |
| Hypogonadism | Monitor for signs of onset of puberty. | ||
| Hypothyroidism | Monitor linear growth in children using standard growth charts. | ||
| Growth restriction | |||
| Family/Community |
| ||
Wolfram syndrome prognosis
The long-term outlook (prognosis) for people with Wolfram syndrome varies depending on the signs and symptoms present in each person. All the features that give Wolfram syndrome the acronym DIDMOAD (diabetes insipidus, diabetes mellitus, optic atrophy, and deafness) are observed in 65% of people, while others only have some of the associated health problems. Most affected people develop diabetes mellitus and optic atrophy before age 15 years. Diabetes mellitus is typically the first manifestation, usually diagnosed between the ages of 6-8, with optic nerve
atrophy following between the ages of 10-12 9. Hearing loss is present in 64% of affected people by age 20 years and up to 72% will eventually develop diabetes insipidus. Wolfram syndrome may also be associated with a variety of other symptoms that can affect almost every part of the body 23.
Diabetes mellitus can be controlled with insulin injections while vision problems usually, but not always, get worse. Often a patient will be registered blind within eight years of diagnosis.
About three quarters of patients get diabetes insipidus and two thirds become deaf in their teenage years. About two thirds experience kidney problems in their twenties and a similar proportion get neurological complications in their thirties. However, there appears to be a subgroup of patients who run a milder course and don’t have these additional complications.
Wolfram syndrome is often fatal by mid-adulthood (average lifespan 30 to 40 years) due to complications from the various health problems associated with the condition, usually from respiratory failure as a result of brain stem atrophy 10, 8, 11.
References- Wolfram Syndrome. https://rarediseases.org/rare-diseases/wolfram-syndrome
- Urano F. Wolfram Syndrome: Diagnosis, Management, and Treatment. Curr Diab Rep. 2016 Jan;16(1):6. doi: 10.1007/s11892-015-0702-6
- Wolfram DJ, Wagener HP. Diabetes mellitus and simple optic atrophy among siblings: report of four cases. Mayo Clin Proc. 1938;1:715–8.
- https://bpb-us-w2.wpmucdn.com/sites.wustl.edu/dist/5/2473/files/2020/03/wolfram-syndrome-q-a-2014.pdf
- https://bpb-us-w2.wpmucdn.com/sites.wustl.edu/dist/5/2473/files/2020/03/common-manifestations-wolfram-syndrome.pdf
- Wolfram Syndrome. https://ghr.nlm.nih.gov/condition/wolfram-syndrome
- Kinsley BT, Swift M, Dumont RH, et al. Morbidity and mortality in the Wolfram syndrome. Diabetes Care. 1995;18(12):1566–70. doi: 10.2337/diacare.18.12.1566
- Barrett TG, Bundey SE, Macleod AF. Neurodegeneration and diabetes: UK nationwide study of Wolfram (DIDMOAD) syndrome. Lancet. 1995;346(8988):1458–63. doi: 10.1016/S0140-6736(95)92473-6
- https://wolframsyndrome.co.uk/wp-content/uploads/2023/04/Wolfram-Syndrome-Different-variants.pdf
- de Heredia ML, Clèries R, Nunes V. Genotypic classification of patients with Wolfram syndrome: insights into the natural history of the disease and correlation with phenotype. Genet Med. 2013 Jul;15(7):497-506. July 2013; 15(7):497-506
- Barrett TG, Bundey SE. Wolfram (DIDMOAD) syndrome. J Med Genet. 1997;34(10):838–41. doi: 10.1136/jmg.34.10.838
- What is Wolfram Syndrome? https://wolframsyndrome.co.uk/what-is-ws/
- Hui C, Khan M, Khan Suheb MZ, et al. Diabetes Insipidus. [Updated 2023 Jan 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470458
- Bischoff AN, Reiersen AM, Buttlaire A, Al-Lozi A, Doty T, Marshall BA, Hershey T; Washington University Wolfram Syndrome Research Group. Selective cognitive and psychiatric manifestations in Wolfram Syndrome. Orphanet J Rare Dis. 2015 May 30;10:66. doi: 10.1186/s13023-015-0282-1
- Desmopressin. https://medlineplus.gov/druginfo/meds/a608010.html
- Desmopressin Nasal. https://medlineplus.gov/druginfo/meds/a682876.html
- De Franco E, Flanagan SE, Yagi T, Abreu D, Mahadevan J, Johnson MB, Jones G, Acosta F, Mulaudzi M, Lek N, Oh V, Petz O, Caswell R, Ellard S, Urano F, Hattersley AT. Dominant ER Stress-Inducing WFS1 Mutations Underlie a Genetic Syndrome of Neonatal/Infancy-Onset Diabetes, Congenital Sensorineural Deafness, and Congenital Cataracts. Diabetes. 2017 Jul;66(7):2044-2053. doi: 10.2337/db16-1296
- Hershey T, Lugar HM, Shimony JS, et al. Early brain vulnerability in wolfram syndrome. PLoS One. 2012;7(7):e40604. doi: 10.1371/journal.pone.0040604
- Zmyslowska A, Malkowski B, Fendler W, et al. Central nervous system PET-CT imaging reveals regional impairments in pediatric patients with Wolfram syndrome. PLoS One. 2014;9(12):e115605. doi: 10.1371/journal.pone.0115605
- Wolfram syndrome. https://rarediseases.org/rare-diseases/wolfram-syndrome
- Wolfram syndrome. https://ghr.nlm.nih.gov/condition/wolfram-syndrome
- Barrett T, Tranebjærg L, Gupta R, et al. WFS1 Spectrum Disorder. 2009 Feb 24 [Updated 2022 Dec 1]. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK4144
- Tranebjærg L, Barrett T, Rendtorff ND. WFS1-Related Disorders. 2009 Feb 24 [Updated 2013 Dec 19]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK4144