What is abruptio placentae
Abruptio placentae also called placental abruption, is when the placenta prematurely separates from the inner wall of the uterus before the baby is born. Abruptio placentae is an uncommon yet serious complication of pregnancy that happens when the placenta separates from your uterus before your baby is born (usually after the 20th week of gestation and before the 3rd stage of labor). The majority of placental abruptions occur before 37-weeks gestation 1. Placental abruption often happens suddenly. Left untreated, it endangers both the mother and the baby. The placenta is a temporary organ that develops in your uterus during pregnancy. The placenta connects the fetus (unborn baby) via the baby’s umbilical cord to the mother’s uterus (Figure 1). The placenta attaches to the wall of your uterus and supplies your baby with nutrients, blood, and oxygen. The placenta also helps your baby get rid of waste products from your baby’s blood. The placenta attaches to the wall of your uterus, and your arises from it. The placenta is usually attached to the top, side, front or back of the uterus. In rare cases, the placenta might attach in the lower area of the uterus. When this happens, it’s called a low-lying placenta (placenta previa).
Abruptio placentae (placental abruption) occurs when the placenta prematurely partly or completely separates from the inner wall of the uterus before delivery 2. This can decrease or block the baby’s supply of oxygen and nutrients and cause heavy bleeding in the mother. Placental abruption can be life-threatening to your baby and sometimes to you. Placental abruption is most likely to occur in the last trimester of pregnancy, especially in the last few weeks before birth, but it can happen any time after 20 weeks of pregnancy up until delivery.
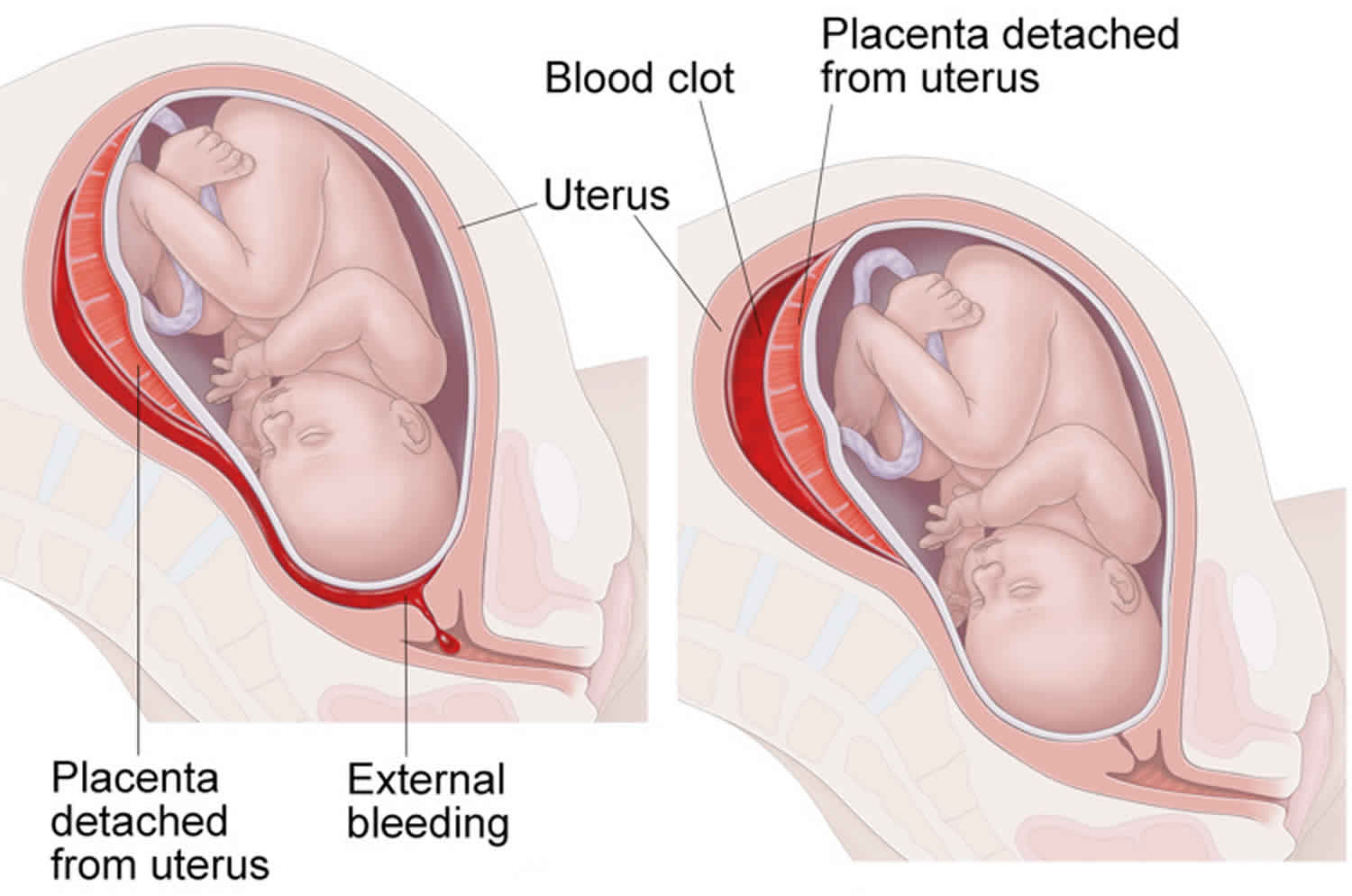
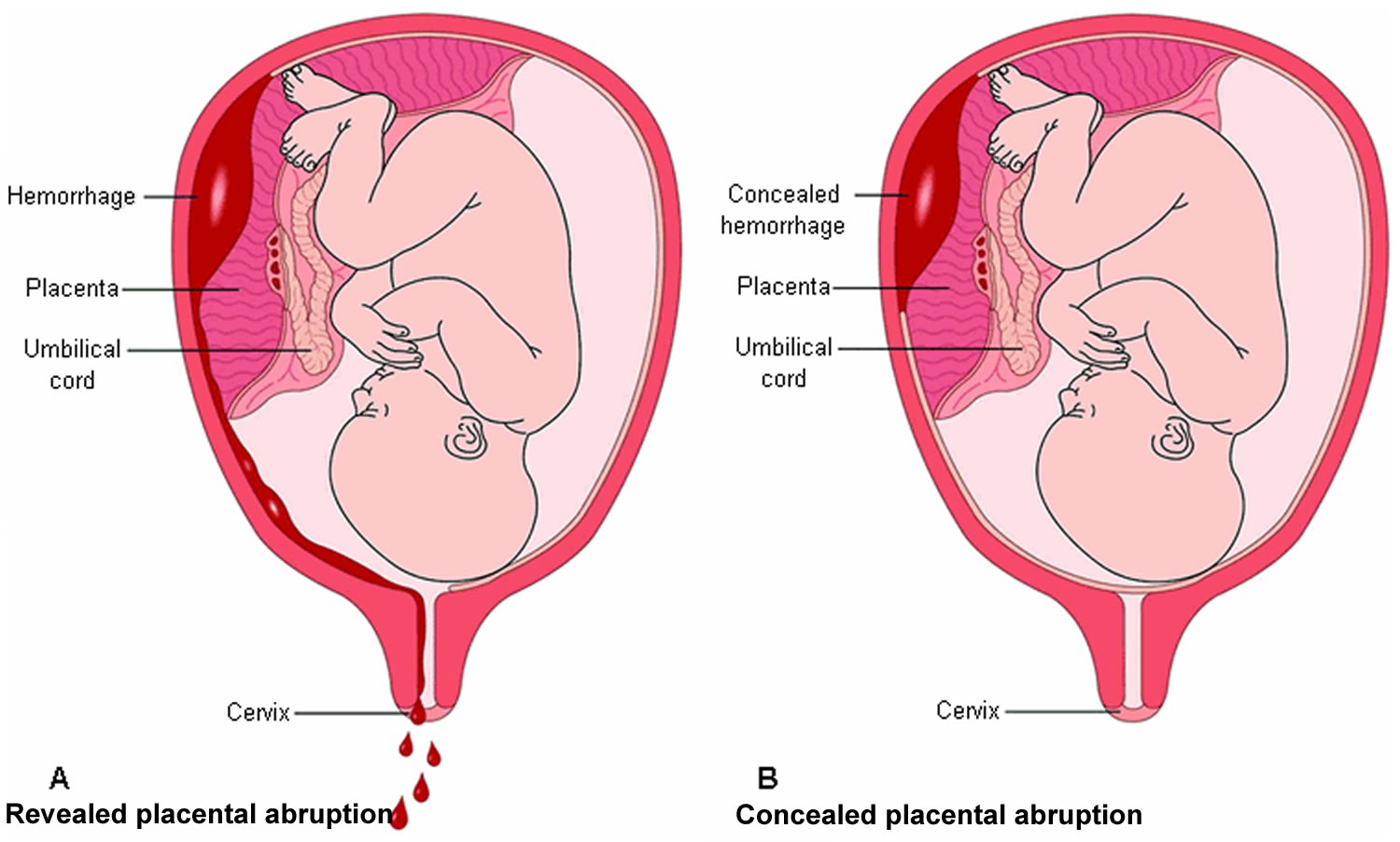
The most common placental abruption symptoms are vaginal bleeding associated with abdominal pain and painful contractions in the second half of pregnancy. The amount of bleeding depends on how much of the placenta has detached and the types of placental abruption (see Figure 2 below). Abruptio placentae (placental abruption) may be revealed, when blood escapes through the vagina, or concealed, when the bleeding occurs behind the placenta, with no evidence of bleeding from the vagina 2. Placental abruption may be partial, affecting only part of the placenta, or total, involving the entire placenta. Sometimes the blood that collects when the placenta detaches stays between the placenta and uterine wall, so you may not have bleeding from your vagina.
- If the separation is slight, you may have only light bleeding. You may also have cramps or feel tender in your belly.
- If the separation is moderate, you may have heavier bleeding. Cramps and belly pain will be more severe.
- If more than half the placenta detaches, you may have belly pain and heavy bleeding. You may also have contractions. The baby may move more or less than normal.
If you have any of these symptoms during your pregnancy, see your doctor right away.
Vaginal bleeding can vary and is not an indication of how much the placenta has separated. In some instances, there could be no visible bleeding because the blood is trapped between the placenta and the uterine wall. Pain can range from mild cramping to strong contractions and often begins suddenly.
These symptoms can resemble other pregnancy conditions. Always consult with your healthcare provider for a diagnosis.
Abruptio placentae diagnosis is made clinically. Some ultrasound features may be helpful. Other tests are, for the most part, unreliable.
Abruptio placentae management and outcome depend on the gestational age, the degree of separation, and the maternal and fetal status.
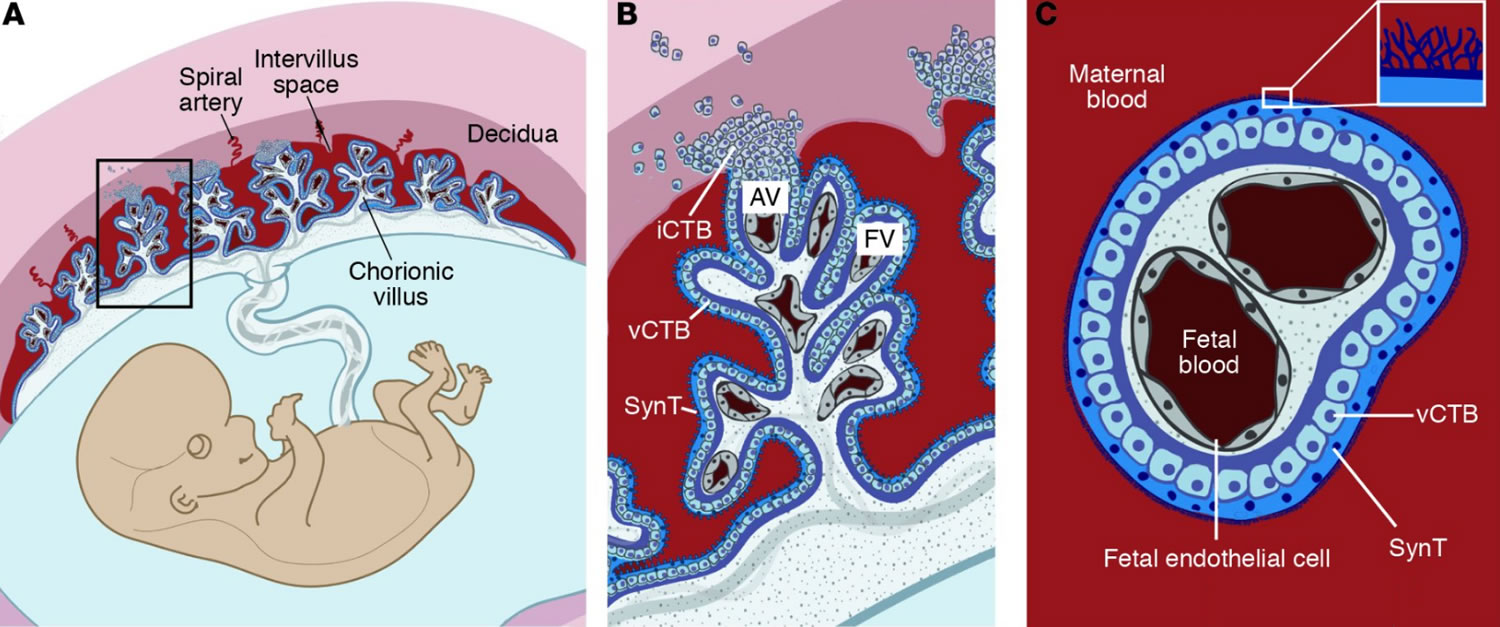
Figure 1. The placenta
Footnotes: Maternal (red portions) and fetal (blue cells and gray vessels) structures make up the placenta. The inset B shows trophoblast cells (invasive cytotrophoblasts or iCTB) re-forming and advancing into the uterine lining. In humans, decidual spiral arterioles perfuse the chorionic villi that line the intervillous space. (B) In floating villi (FV), a continuous layer of multinucleated syncytiotrophoblasts (SynT) interfaces with maternal blood. Beneath lies a progenitor population of mononuclear villous cytotrophoblast (vCTB). At the uterine wall, invasive cytotrophoblasts (iCTBs) differentiate along the invasive pathway to form anchoring villi (AV). A subset of invasive cytotrophoblasts (iCTBs) breaches spiral arterioles and differentiates into an endovascular subtype that replaces the resident maternal endothelium (not shown). (C) The cross-sectional anatomy of a floating villus shows that the apical surfaces of syncytiotrophoblasts (SynT) are covered with branched microvilli that maximize their surface areas for gas and nutrient/waste exchange. The blood vessels that ramify through the villous stroma carry embryonic/fetal blood.
[Source 3 ]Figure 2. Abruptio placentae
Footnotes: Types of placental abruption. (A) Revealed placental abruption, where blood tracks between the membranes, and escapes through the vagina and cervix. (B) Concealed placental abruption where blood collects behind the placenta, with no evidence of vaginal bleeding.
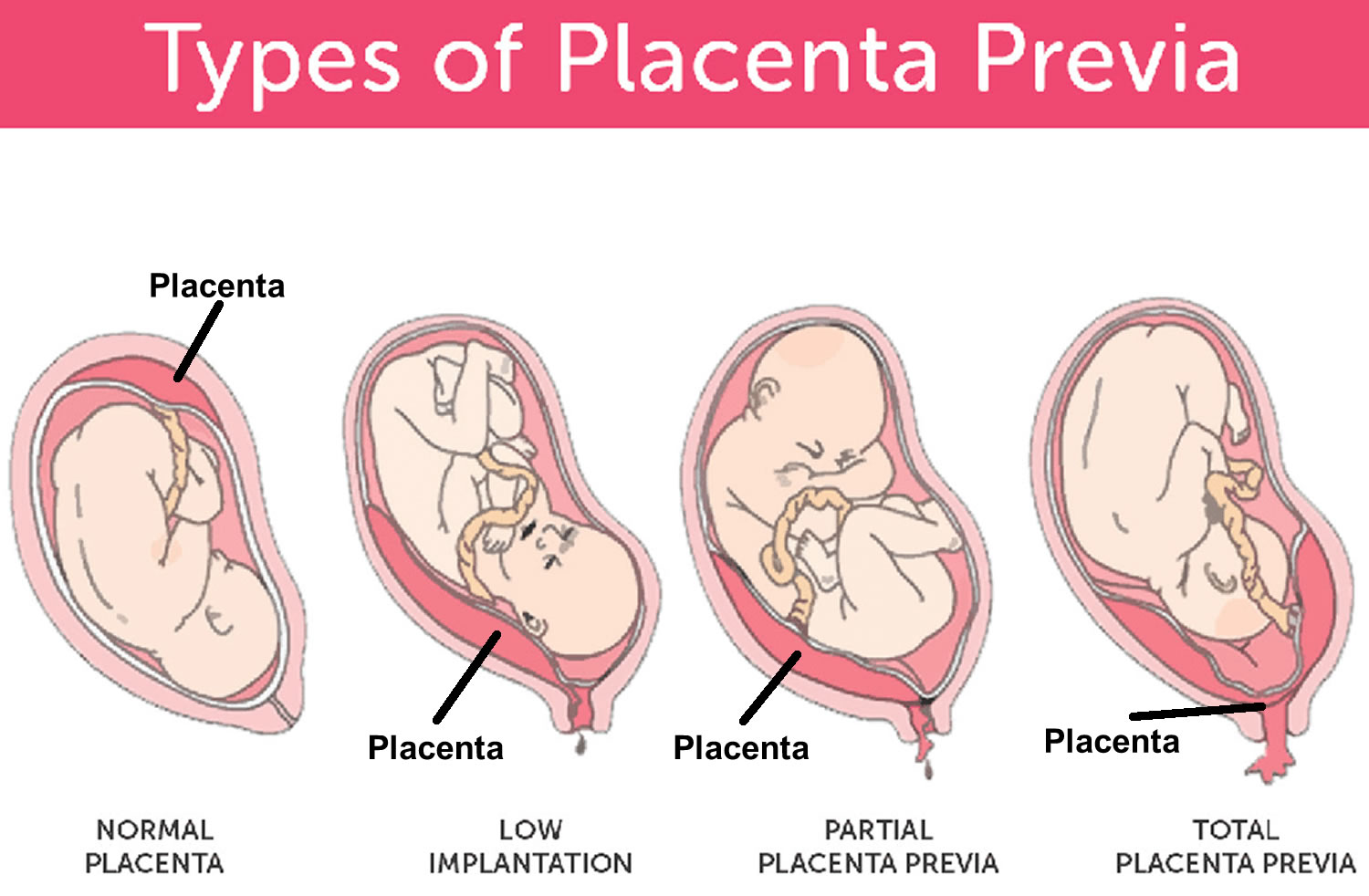
[Source 2 ]What is the difference between placental abruption and placenta previa?
In placenta previa, the placenta is covering all or part of the mother’s cervix — the outlet for the uterus (Figure 3). Placenta previa is also called low-lying placenta. Think of it as an obstacle that’s blocking the exit from the uterus. Even though the placenta is in a complicated position, it’s still attached to the uterus. Placenta previa can cause severe bleeding during pregnancy and delivery.
If you have placenta previa, you might bleed throughout your pregnancy and during your delivery. Your doctor will recommend avoiding activities that might cause contractions, including having sex, douching, using tampons, or engaging in activities that can increase your risk of bleeding, such as running, squatting, and jumping.
You’ll need a C-section to deliver your baby if the placenta previa doesn’t resolve.
On the other hand, when the placenta prematurely detaches from the uterus, this is known as placental abruption or abruptio placenta. Both abruptio placenta and placenta previa can cause vaginal bleeding during pregnancy and labor.
Figure 3. Placenta previa
Do you always bleed during a placental abruption?
Most of the time, you will see some blood during a placental abruption. In the event of a concealed placental abruption, the blood will be behind the placenta. In that case, there will be no bleeding. In other cases, the placental abruption develops slowly, which can cause occasional, light bleeding.
Talk to your doctor about any vaginal bleeding you experience during your pregnancy.
What does placental abruption feel like?
You may experience sudden or sharp pain, cramping, or tenderness in your lower pelvic region or back during a placental abruption. You could also feel your baby move less. You should discuss these symptoms with your doctor immediately.
What are the first signs of a placental abruption?
The most common symptom of a placental abruption is vaginal bleeding, although you will not always bleed. You may also have sudden, ongoing pain in your abdomen or back.
How common is a placental abruption?
Worldwide, placental abruption occurs in about one pregnancy in every 100. In about half of cases, placental abruption is mild and can be managed by ongoing close monitoring of the mother and baby. About 25 per cent of cases are moderate, while the remaining 25 per cent threaten the life of both baby and mother.
Abruptio placentae is usually seen in the third trimester, but it can happen any time after 20 weeks of pregnancy up until delivery.
Can I have another placental abruption?
You have about a 15% chance of having another abruption in a future pregnancy. With two prior abruptions, this chance increases to about 25%. If you have had a previous abruption, please let your healthcare provider know.
Can sex cause a placental abruption?
Sexual intercourse is not a direct cause of placental abruption. In most cases, it’s perfectly safe to have sex during pregnancy. Activities with a high risk of falling or abdominal trauma should be avoided during pregnancy.
Can sneezing cause a placental abruption?
Sneezing is a normal thing your body does and is not a cause for placental abruption. It cannot harm your baby in any way. If you have any concerns about frequent and forceful sneezing or coughing, reach out to your healthcare provider for guidance.
Can smoking cause a placental abruption?
Smoking can increase your risk of many complications during pregnancy, including placental abruption. Ask your healthcare provider about ways to quit smoking.
Abruptio placentae types
Types of placental abruption are:
- A partial placental abruption occurs when the placenta does not completely detach from the uterine wall.
- A complete or total placental abruption occurs when the placenta completely detaches from the uterine wall. There is usually more vaginal bleeding associated with this type of abruption.
- Revealed placental abruptions have moderate to severe vaginal bleeding that you can see.
- Concealed placental abruptions have little or no visible vaginal bleeding. Blood is trapped between the placenta and uterine wall.
The clinical implications of a placental abruption vary based on the extent of the separation and the location of the separation. Placental abruption can be complete or partial and marginal or central. The classification of placental abruption is based on the following clinical findings 1:
Class 0: Asymptomatic
- Discovery of a blood clot on the maternal side of a delivered placenta
- Diagnosis is made retrospectively
Class 1: Mild
- No sign of vaginal bleeding or a small amount of vaginal bleeding.
- Slight uterine tenderness
- Maternal blood pressure and heart rate
- No signs of fetal distress
Class 2: Moderate
- No sign of vaginal bleeding to a moderate amount of vaginal bleeding
- Significant uterine tenderness with tetanic contractions
- Change in vital signs: maternal tachycardia, orthostatic changes in blood pressure.
- Evidence of fetal distress
- Clotting profile alteration: hypofibrinogenemia
Class 3: Severe
- No sign of vaginal bleeding to heavy vaginal bleeding
- Tetanic uterus/ board-like consistency on palpation
- Maternal shock
- Clotting profile alteration: hypofibrinogenemia and coagulopathy
- Fetal death
Classification of 0 or 1 is usually associated with a partial, marginal separation; whereas, classification of 2 or 3 is associated with complete or central separation.
Abruptio placentae symptoms
Each person can have different symptoms of placental abruption. However, the most common placental abruption symptoms are vaginal bleeding with cramping or painful contractions during the third trimester of pregnancy, but it can happen any time after 20 weeks of pregnancy up until delivery. The amount of bleeding depends on how much of the placenta has detached. Sometimes the blood that collects when the placenta detaches stays between the placenta and uterine wall, so you may not have bleeding from your vagina.
- If the separation is slight, you may have only light vaginal bleeding. You may also have cramps or feel tender in your belly.
- If the separation is moderate, you may have heavier vaginal bleeding. Cramps and belly pain will be more severe.
- If more than half the placenta detaches, you may have belly pain and heavy vaginal bleeding. You may also have contractions. The baby may move more or less than normal.
Placental abruption symptoms or signs can also include:
- Continuous abdominal pain.
- Continuous lower back pain or backache.
- Uterine contractions that are longer and more intense than average labor contractions.
- Uterine tenderness or rigidity. Tender and hard uterus.
- Painful abdomen when touched.
- Decreased fetal movement.
- Abnormal fetal heart rhythm (sign of fetal distress).
If you have any of these symptoms or signs during your pregnancy, seek emergency care right away!
Abdominal pain and back pain often begin suddenly. The amount of vaginal bleeding can vary greatly, and doesn’t necessarily indicate how much of the placenta has separated from the uterus. It’s possible for the blood to become trapped inside the uterus, so even with a severe placental abruption, there might be no visible bleeding.
In some cases, placental abruption develops slowly (chronic abruption), which can cause light, intermittent vaginal bleeding. Your baby might not grow as quickly as expected, and you might have low amniotic fluid or other complications.
Signs of a placental abruption
See your doctor immediately if you have any of these signs that can indicate placental abruption:
- Vaginal bleeding or spotting, or if your water breaks and the fluid is bloody. In most cases of placental abruption, you’ll have some vaginal bleeding, ranging from a small amount to an obvious and sudden gush. Sometimes, though, the blood stays in the uterus behind the placenta, so you might not see any bleeding at all.
- Cramping, uterine tenderness, abdominal pain, or back pain.
- Frequent contractions or a contraction that doesn’t end. In close to a quarter of cases, an abruption will cause the woman to go into labor prematurely.
- Your baby isn’t moving as much as before.
Call your local emergency services number if you are bleeding heavily or have any signs of shock such as if you feel weak, faint, pale, sweaty, or disoriented, or your heart is pounding.
Complications of abruptio placenta
Placental abruption can cause life-threatening problems for both mother and baby.
Complications from a placental abruption include:
For your baby:
- Premature birth. Premature birth also called preterm birth is when a baby is born too early, before 37 weeks of pregnancy have been completed. Babies born too early (especially before 32 weeks) have higher rates of death and disability. Babies who survive may have:
- Breathing problems
- Feeding difficulties
- Cerebral palsy
- Developmental delay
- Vision problems
- Hearing problems
- Low birth weight.
- Growth problems.
- Brain injury from lack of oxygen.
- Stillbirth. A stillbirth is when a baby dies in the womb during the last 20 weeks of pregnancy. A miscarriage is a fetal loss in the first half of pregnancy.
For the mother:
- Blood loss.
- Blood clotting issues.
- Blood transfusion.
- Hemorrhage.
- Kidney failure.
With placental abruption, the mother is at risk for hemorrhage and the need for blood transfusions, hysterectomy, bleeding disorders specifically disseminated intravascular coagulopathy (DIC), renal failure or other organs failure resulting from blood loss and Sheehan syndrome or postpartum pituitary gland necrosis. With the availability of blood replacement, maternal death is rare but continues to be higher than the overall maternal mortality rate.
Causes of abruptio placenta
The exact cause of placental abruption is often unknown. It is thought that an abnormal blood supply in the uterus or placenta may play a role, but the cause of the suspected abnormality isn’t clear. However, these factors raise a woman’s risk for abruptio placentae:
- History of placental abruption in previous pregnancy
- Long-term (chronic) high blood pressure (hypertension)
- Presence of preeclampsia. Preeclampsia is high blood pressure and signs of liver or kidney damage that occur in women after the 20th week of pregnancy. While rare, preeclampsia also may occur in a woman after delivering her baby, most often within 48 hours. This is called postpartum preeclampsia.
- Sudden high blood pressure in pregnant women who had normal blood pressure in the past
- Heart disease
- Abdominal trauma
- Smoking
- Alcohol or cocaine use
- Fibroids in the uterus
- An injury to the mother (such as a car crash or fall in which the abdomen was hit)
- Early rupture of membranes, which causes leaking amniotic fluid before the end of pregnancy
- Infection inside of the uterus during pregnancy (chorioamnionitis)
- Being older than 40 – older mothers are at increased risk of a range of pregnancy complications, including placental abruption.
In many countries, the rate of placental abruption has been increasing, even with improved obstetrical care and monitoring techniques. This suggests a multifactorial cause that is not well understood 4.
Abruptio placentae risk factors
You are at higher risk for placental abruptions if you have any of the following:
- Trauma or injury to your uterus (like a car accident, fall or blow to the stomach).
- Previous placental abruption (recurrence rate 19-25%) 5
- Multiple fetuses – carrying twins, triplets, quads or more increases the risk of placental abruption compared to carrying a single fetus.
- Multiparity (having two or more number of children) – the risk increases the more pregnancies a woman has had.
- High blood pressure (hypertension), gestational diabetes or preeclampsia — up to 50% of cases. High blood pressure increases the risk of abnormal bleeding between the placenta and the wall of the uterus. In nearly half of placenta abruption cases (44%), the pregnant mother is hypertensive. One of the most common causes of hypertension during pregnancy is a condition known as pre-eclampsia.
- If you smoke or have a history of drug use (cocaine or amphetamine use).
- Short umbilical cord.
- Maternal age 35 or greater. Pregnant women who are younger than 20 years or older than 35 years are at greater risk
- Uterine fibroids.
- Excessive amniotic fluid (polyhydramnious) – more fluid than normal increases the risk of bleeding between the placenta and the uterus wall.
- Thrombophilia (a blood clotting disorder).
- Premature rupture of membranes (the water breaks before your baby is full term).
- Rapid loss of the amniotic fluid.
- Chorioamnionitis (infection of the placenta tissues and amniotic fluid).
- Amniocentesis – a prenatal test that involves a needle inserted through the mother’s abdomen and into the uterus to withdraw amniotic fluid. Very rarely, the needle puncture causes bleeding.
- Amnioreduction – the prenatal condition of too much amniotic fluid is called polyhydramnious. Amnioreduction is a procedure to remove excess amniotic fluid using a needle inserted through the mother’s abdomen into the uterus. This procedure uncommonly causes bleeding.
- External cephalic version – the doctor uses ultrasound imaging and external massage on the mother’s abdomen to try to turn the baby from a head-up position (breech) to a head-down position in readiness for childbirth. This procedure can occasionally (rarely) dislodge the placenta.
Pathophysiology of abruptio placenta
Placental abruption occurs when the maternal blood vessels tear away from the placenta (rupture of a spiral artery with hemorrhage into the decidua basalis leading to separation of the placenta) and bleeding occurs between the uterine lining and the maternal side of the placenta 1. The small vessel disease seen in abruptio placentae may also result in placental infarction. As the blood accumulates, it pushes the uterine wall and placenta apart. The placenta is the fetus’ source of oxygen and nutrients as well as the way the fetus excretes waste products. Diffusion to and from the maternal circulatory system is essential to maintaining these life-sustaining functions of the placenta. When accumulating blood causes separation of the placenta from the maternal vascular network, these vital functions of the placenta are interrupted. If the fetus does not receive enough oxygen and nutrients, it dies 6.
Abruptio placentae prevention
You cannot prevent placental abruption, but you can control the risk factors for abruptio placentae by:
- Keeping your blood pressure at a healthy level.
- Keeping your diabetes and heart disease under control.
- Not using tobacco, alcohol, cocaine or other illicit drugs.
- Taking health and safety precautions like wearing a seat belt when in a motor vehicle.
- Reporting any abdominal trauma — from an auto accident, fall or other injury — to your healthcare provider or seek immediate medical help.
- Talking to your healthcare provider about any vaginal bleeding.
- Following your doctor’s recommendations about ways to lower your risk if you had an abruptio placenta in a past pregnancy.
If you’ve had a placental abruption, and you’re planning another pregnancy, talk to your health care provider before you conceive to see if there are ways to reduce the risk of another abruption.
Abruptio placentae diagnosis
Placental abruption is diagnosed through an exam and monitoring. If your health care provider suspects placental abruption, he or she will do a physical exam to check for uterine tenderness or rigidity. You may be admitted to the hospital depending on the severity of the abruption or you may be able to rest at home. Your healthcare provider will:
- Ask how much bleeding has occurred.
- Ask where you feel pain and how intense the pain is.
- Ask when symptoms started.
- Monitor your blood pressure.
- Monitor the baby’s heart rate and movement.
- Monitor your contractions.
- Use ultrasound to locate the bleeding and to check your baby. During an ultrasound, high-frequency sound waves create an image of your uterus on a monitor. It’s not always possible to see a placental abruption on an ultrasound, however.
- Recommend blood or urine tests.
Sometimes, the diagnosis of placental abruption can’t be confirmed until childbirth, when the placenta is delivered with an attached blood clot that appears old rather than fresh. The placenta is usually sent to a laboratory for further diagnostic testing.
There are typically three grades of placental abruption a healthcare provider will diagnose:
- Grade 1 placental abruption: Small amount of bleeding, some uterine contractions, and no signs of fetal or maternal stress.
- Grade 2 placental abruption: Mild to moderate amount of bleeding, some uterine contractions, and signs of fetal stress.
- Grade 3 placental abruption: Moderate to severe bleeding or concealed bleeding, uterine contractions that do not relax, abdominal pain, low maternal blood pressure, and fetal death.
It is important to discuss any symptoms or changes in symptoms with your healthcare provider.
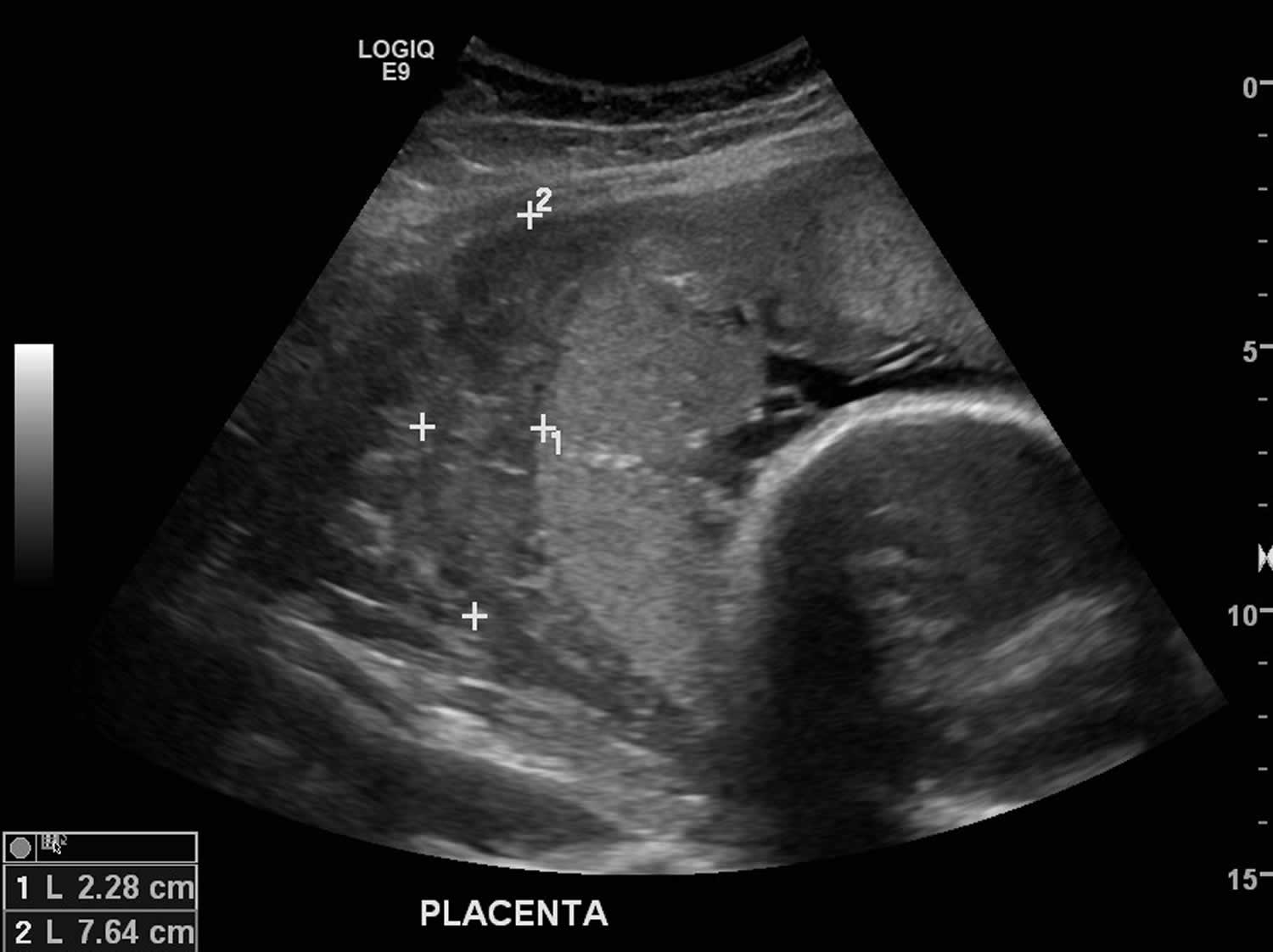
Abruptio placenta ultrasound
Ultrasound is almost always the first (and usually the only) imaging modality used to evaluate placental abruption, but an index of suspicion should be maintained for the diagnosis since ultrasound is relatively insensitive for the diagnosis of placental abruption 7. This is partly because a retroplacental hematoma may be identified only in 2-25% of all abruptions 8. Given the low sensitivity for detecting placental abruption on ultrasound, if there is a high clinical suspicion, then it is likely prudent to treat based on the clinical suspicion 7.
The sonographic signs of placental abruption include 8:
- retroplacental hematoma (often poorly echogenic)
- intraplacental anechoic areas
- separation and rounding of the placental edge
- thickening of the placenta: often to over 5.5 cm
- thickening of the retroplacental myometrium: usually should be 1-2 cm unless there is a focal myometrial contraction
- disruption in retroplacental circulation
- intra-amniotic echoes due to intra-amniotic hemorrhage
- blood in the fetal stomach
- intermembranous clot in twins
The echogenicity of hematomas depends upon their age. Acute hematomas imaged at the time of symptoms tend to be hyperechoic or isoechoic compared to the adjacent placenta. As the hematoma is commonly isoechoic to the placenta, it may be mistaken for focal thickening of the placenta. A ‘normal’ ultrasound does not exclude a placental abruption-particularly as the blood may have escaped through the vagina in the case of external hemorrhage
In other cases, the retroplacental hematoma may be hypoechoic or of heterogeneous echogenicity.
Figure 4. Abruptio placenta ultrasound
Footnotes: 25 year old female with 30 week gestation and antepartum hemorrhage for investigation. Ultrasound showed a crescent of avascular, low echogenicity between the placenta and uterine wall consistent with placental abruption. Ultrasound scan also showed an otherwise live fetus, with normal growth parameters, liquor volume and Doppler parameters.
[Source 9 ]Management for abruptio placenta
Once the placenta has separated from the uterus, it cannot be reconnected or repaired. A healthcare provider will recommend treatment based on:
- The severity of the abruptio placenta.
- How long your pregnancy is/gestational age of your unborn baby.
- Signs of distress from your unborn baby.
- Amount of blood you’ve lost.
Generally, the severity of the placental abruption and gestational age of your baby are the two most important factors 10:
- If your baby is not close to full term
- If it’s too soon for your baby to be born and your abruption is mild, you will be closely monitored until you reach 34 weeks of pregnancy. If your baby’s heart rate is normal and you’re not bleeding, your healthcare provider may allow you to go home to rest. They may give you medication to help with your baby’s lung development and to protect the baby’s brain, in case early delivery becomes necessary.
- If your abruption is severe and the health of you or your baby are at risk, immediate delivery may be necessary.
- If your baby is near full term
- If your abruption is mild and the baby’s heart rate is stable, a closely monitored vaginal delivery is possible. This is generally determined around 34 weeks of pregnancy.
- If the abruption gets worse or you or your baby are in danger at any time, the baby will be delivered via emergency Cesarean section (C-section).
For severe bleeding, you might need a blood transfusion.
Women classified with a class 1 or mild placental abruption and no signs of maternal or fetal distress and pregnancy less than 37 weeks gestation may be managed conservatively. These patients are usually admitted to the obstetrical unit for close monitoring of maternal and fetus status. Intravenous access and blood work for type and cross-match is part of the plan of care. The maternal-fetal dyad will continue to be monitored until there is a change in condition or until fetal maturity is reached.
If the collected data results in class 2 (moderate) or class 3 (severe) classification and the fetus is viable and alive, delivery is necessary. Because of the hypertonic contractions, a vaginal birth may occur rapidly. Given the potential for coagulopathy, vaginal birth presents less risk to the mother. However, if there are signs of fetal distress an emergency cesarean birth is necessary to protect the fetus. During the surgical procedure, careful management of fluids and circulatory volume is important. Post-operatively the patient needs to be monitored for postpartum hemorrhage and alterations in the clotting profile. A neonatal team needs to be present in the delivery room to receive and manage the infant.
Abruptio placentae prognosis
Placental abruption is a life-threatening condition for both the mother and the fetus. Abruptio placentae prognosis can vary depending on the severity of your symptoms and how far along you are in your pregnancy. If the bleeding continues, both maternal and fetal lives are at stake. You can expect to be monitored closely and often. Watch for any changes in symptoms and discuss them with your healthcare provider immediately.
Partial placenta separation is associated with low mortality compared to full separation; however in both cases, without an emergent cesarean section, fetal demise may occur. Fetal mortality rates of 1-40% have been reported, but this also depends on the age of the fetus and the extent of separation. Today, in the US, about 1 to 5% of maternal deaths are linked to placental abruption 1. Besides the hemorrhage, the other morbidity is related to blood transfusions, the prematurity of the fetus, hysterectomy, and cesarean section (which will make the need for future cesarean sections more likely). Recurrence rates of 3-10% are reported 11.
The two factors that affect survival rate are gestational age at birth and the severity of the abruption. Early detection, close monitoring, and quick treatment can help reduce complications.
See your healthcare provider immediately if are bleeding, cramping or experiencing pelvic pain during your pregnancy, especially in the third trimester.
References- Schmidt P, Skelly CL, Raines DA. Placental Abruption. [Updated 2021 Jul 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482335
- Oyelese Y, Ananth CV. Placental abruption. Obstet Gynecol. 2006 Oct;108(4):1005-16. doi: 10.1097/01.AOG.0000239439.04364.9a
- The placenta: transcriptional, epigenetic, and physiological integration during development. J Clin Invest. 2010;120(4):1016-1025. https://doi.org/10.1172/JCI41211
- Miller C, Grynspan D, Gaudet L, Ferretti E, Lawrence S, Moretti F, Lafreniere A, McGee A, Lattuca S, Black A. Maternal and neonatal characteristics of a Canadian urban cohort receiving treatment for opioid use disorder during pregnancy. J Dev Orig Health Dis. 2019 Feb;10(1):132-137. doi: 10.1017/S2040174418000478
- TIKKANEN, M. (2010), Etiology, clinical manifestations, and prediction of placental abruption. Acta Obstetricia et Gynecologica Scandinavica, 89: 732-740. https://doi.org/10.3109/00016341003686081
- Plowman RS, Javidan-Nejad C, Raptis CA, Katz DS, Mellnick VM, Bhalla S, Cornejo P, Menias CO. Imaging of Pregnancy-related Vascular Complications. Radiographics. 2017 Jul-Aug;37(4):1270-1289. doi: 10.1148/rg.2017160128
- Glantz, C. and Purnell, L. (2002), Clinical Utility of Sonography in the Diagnosis and Treatment of Placental Abruption. Journal of Ultrasound in Medicine, 21: 837-840. https://doi.org/10.7863/jum.2002.21.8.837
- Radswiki, T., Jones, J. Placental abruption. Reference article, Radiopaedia.org. https://doi.org/10.53347/rID-12479
- Dixon, A. Placental abruption. Case study, Radiopaedia.org. https://doi.org/10.53347/rID-14281
- Society for Maternal-Fetal Medicine (SMFM). Electronic address: [email protected], Gyamfi-Bannerman C. Society for Maternal-Fetal Medicine (SMFM) Consult Series #44: Management of bleeding in the late preterm period. Am J Obstet Gynecol. 2018 Jan;218(1):B2-B8. doi: 10.1016/j.ajog.2017.10.019
- Martinelli KG, Garcia ÉM, Santos Neto ETD, Gama SGND. Advanced maternal age and its association with placenta praevia and placental abruption: a meta-analysis. Cad Saude Publica. 2018 Feb 19;34(2):e00206116. doi: 10.1590/0102-311X00206116