Adenoiditis
Adenoiditis occurs when there is inflammation of the adenoid tissue resulting from infection, allergies, or irritation from stomach acid 1. Adenoiditis rarely occurs on its own and is more often involved in a more extensive disease process such as adenotonsillitis, tonsillitis, pharyngitis, rhinosinusitis, etc. Continual irritation may lead to adenoid enlargement (hypertrophy) which is responsible for many of the complications of adenoid disease. Large or swollen adenoids may cause symptoms such as a sore throat, trouble breathing, ear problems, or sleep problems.
Adenoiditis is often indistinguishable from bacterial sinusitis. Estimates are that children have six to eight viral upper respiratory tract infections (URTIs) per year. Five to thirteen percent of these viral URTIs result in bacterial sinusitis which may have adenoiditis as a component of the illness 2.
Adenoiditis can be classified as acute or chronic:
- Acute adenoiditis often occurs after a viral upper respiratory tract infection (URTI). Bacterial agents proliferate and infect the adenoids and surrounding tissue resulting in inflammation and increased production of exudates. Symptoms include rhinorrhea, post-nasal drip, nasal obstruction, snoring, fever, and halitosis.
- Chronic adenoiditis shows many of the same symptoms of acute adenoiditis but on a persistent basis lasting 90 days and is often caused by polymicrobial infections and biofilm formation 3.
Another cause of adenoiditis may also be environmental allergens or caustic irritation from stomach acid in the presence of gastroesophageal reflux disease (GERD) 4.
Any form of chronic inflammation may lead to the proliferation of lymphoid tissue and subsequent adenoid hypertrophy. This hypertrophy can lead to nasal airway obstruction and obstruction of the Eustachian tubes which in turn leads to other problems such as obstructive sleep apnea (OSA) and acute otitis media 5.
Swollen adenoids may be treated at home like any sore throat. If there is an infection caused by bacteria, such as strep throat, the doctor may give your child antibiotics.
Patients with recurrent adenoiditis or the complications of adenoid hypertrophy should obtain a referral to an ear, nose, and throat specialist (otolaryngologist) for further evaluation and treatment. Other disciplines that may need to be involved in the care of the patient include sleep medicine, allergy specialists, and gastroenterology depending on the individual’s needs.
If your child gets infections often or has trouble breathing, your doctor might suggest taking out the adenoids. Surgery to remove the adenoids is called adenoidectomy.
Removal of the adenoid (adenoidectomy) is a surgical procedure. It is performed by an ears, nose, and throat surgeon (otolaryngologist) in the operating room under general anesthesia. In this day and age, general anesthesia is very safe and your child will be carefully monitored during the procedure. Although the adenoid is in the back of the nose, it is removed through the mouth and there are no visible scars following surgery. Unlike the tonsils, your surgeon cannot completely remove all adenoid tissue in the back of the nose (although today’s instruments allow us to do a pretty good job). It is therefore possible for the adenoid to “grow back” and cause symptoms again. However, it is quite rare for a child to need to have the adenoid removed a second time.
How can you care for your child at home?
- If your child’s doctor prescribed antibiotics for your child, give them as directed. Do not stop using them just because your child feels better. Your child needs to take the full course of antibiotics.
- Give your child acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) for pain. Read and follow all instructions on the label. Do not give aspirin to anyone younger than 18. It has been linked to Reye syndrome, a serious illness.
- Be careful when giving your child over-the-counter cold or flu medicines and Tylenol at the same time. Many of these medicines have acetaminophen, which is Tylenol. Read the labels to make sure that you are not giving your child more than the recommended dose. Too much acetaminophen (Tylenol) can be harmful.
- Have your child drink plenty of fluids. Fluids may help soothe a sore throat. Your child can drink warm or cool liquids (whichever feels better). These include tea, soup, and juice.
- Make sure your child gets lots of rest.
- Place a humidifier by your child’s bed or close to your child. This may make it easier for your child to breathe. Follow the directions for cleaning the machine.
What are adenoids?
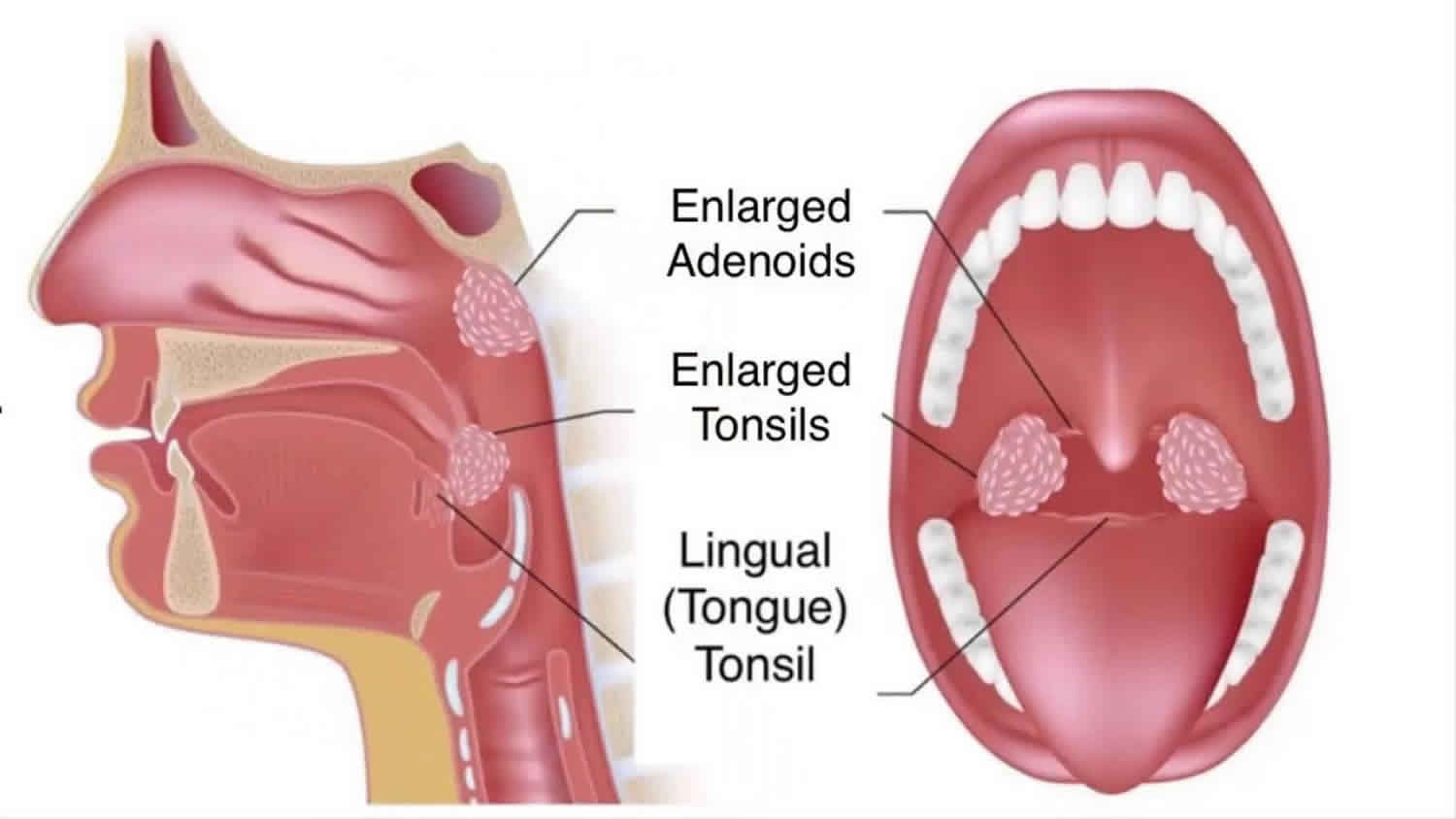
Adenoids are a grouping of lymphoid tissue at the back of the nose and throat (on the posterior wall of the nasopharynx behind the soft palate). Adenoids are made of the same tissue that forms the tonsils. Adenoid tissue is a single patch of tissue that contain lymphocytes, white blood cells that help to fight off infections from viruses or bacteria. The tonsils, two small glands on either side of the back of your throat, also contain lymphocytes. Adenoids are higher in the back of your throat than your tonsils and usually can’t be seen. Adenoids help your body fight infection.
The adenoids, along with the palatine tonsils, lingual tonsils, and tubal tonsils of Gerlach make up what is known as Waldeyer’s ring 1. Together, these tissues function as an essential part of the human immune system. Antigens, introduced through the oral and nasal cavities, come into contact with the immune cells of Waldeyer’s ring. These cells can then produce immunologic memory of the antigens and fight them by producing IgA antibodies.
The adenoids are present at birth and enlarge throughout childhood. Some children are born with large adenoids. They usually shrink as the child gets older. Adenoid tissue and tonsils continue to grow until a child is about eight years old. In most individuals, the adenoids will regress in size during puberty and may be nearly absent by adulthood. For this reason, adenoiditis is commonly a problem of childhood and adolescence 1.
Adenoid size grading is on a scale of zero to four:
- Grade 0 = Absent
- Grade 1+ = Less than 25% obstruction of the nasopharynx
- Grade 2+ = 25-50% obstruction of the nasopharynx
- Grade 3+ = 50-75% obstruction of the nasopharynx
- Grade4+ = Greater than75% obstruction of the nasopharynx
The adenoids receive their blood supply from the ascending pharyngeal artery, maxillary artery, and facial artery. Venous drainage occurs through the pharyngeal veins. Nervous innervation is through the vagus nerve and glossopharyngeal nerve.
Adenoiditis causes
Many agents and pathogens can cause inflammation of the adenoid tissue or adenoiditis. A viral upper respiratory tract infection (URTI) often precedes acute adenoiditis. In this vulnerable state, bacterial pathogens can infect the tissues and proliferate.
The most common bacterial pathogens cultured from adenoid specimens are 5:
- Haemophilus influenzae, Streptococcus pneumoniae, Streptococcus pyogenes and Staphylococcus aureus. Chronic adenoiditis is more often a polymicrobial infection and may include anaerobic pathogens and biofilm development 3.
- Allergies are believed to play a role in adenoiditis and subsequent adenoid hypertrophy. Allergens inhaled through the nose come in contact with the adenoid tissue. The tissues will proliferate in order to create a response to allergens and produce IgA 6.
- Chronic irritation from stomach acid in the setting of gastroesophageal reflux disease (GERD) may also play a role in adenoiditis and adenoid hypertrophy 4.
Adenoiditis symptoms
Symptoms of swollen adenoids
These symptoms are often associated with swollen adenoids:
- difficulty breathing through the nose
- breathing through the mouth
- talking as if the nostrils are pinched
- noisy breathing
- snoring
- stopped breathing for a few seconds during sleep (obstructive sleep apnea)
- frequent “sinus” symptoms
- ongoing middle ear infections or middle ear fluid in a school-aged child
Adenoid tissue typically regresses around puberty. Therefore, the typical patient with adenoiditis is a prepubescent child with a recent history URTI. The patient may also have a history of acute otitis media, obstructive sleep apnea, or GERD. Enlarged tonsils and adenoid tissue can cause symptoms such as a stuffy nose, sore throat, and a scratchy voice. Children with chronically enlarged adenoid tissue may also have frequent ear infections, sinusitis, hearing problems, and upper respiratory infections. These conditions can also lead to a breathing disorder called obstructive sleep apnea, which causes snoring and gasping for breath during sleep and sleepiness, and occasional hyperactivity during the day.
If enlarged adenoids are suspected, the doctor may ask about and then check your child’s ears, nose, and throat, and feel the neck along the jaw. To get a really close look, the doctor might order X-rays or look into the nasal passage with a tiny telescope. For a suspected infection, the doctor may prescribe different types of medicine like pills or liquids. Nasal steroids (a liquid that is sprayed into the nose) might also be prescribed to help reduce swelling in the adenoids.
Physical findings include purulent rhinorrhea, post-nasal drip, nasal obstruction, snoring, fever, mouth breathing, and halitosis. Indirect mirror exam may allow the practitioner to observe enlarged adenoids with exudates. A flexible nasolaryngoscope exam can allow for direct observation of the adenoids but is often not tolerated by children and requires advanced training to use.
Long-standing adenoiditis with subsequent adenoid hypertrophy can lead to the development of what is known as adenoid facies or long face syndrome. Enlarged adenoids block the nasopharynx and result in obligate mouth breathing, which can lead to craniofacial abnormalities including a high-arched palate and retrognathic mandible 7.
Adenoiditis complications
If adenoiditis is left untreated, the patient may develop a chronic low-level infection of the adenoids which in some cases can lead to the development of a biofilm. The adenoids may then serve as a nidus of infection for other closely related structures and lead to rhinosinusitis, pharyngitis, tonsillitis, and acute otitis media 8.
Adenoid hypertrophy
Adenoid hypertrophy is responsible for some of the more common complications related to disease of the adenoids. As they enlarge the tissues can create a significant obstacle to the flow of air through the nasopharynx. This enlargement can cause mouth breathing, snoring, and obstructive sleep apnea (OSA). Obstructive sleep apnea can be a life-threatening disease if left untreated. Removing the adenoids can increase the flow of air through the nasopharynx, decreasing obstructive episodes and leading to better continuous positive airway pressure (CPAP) compliance.
Enlarged adenoids may also obstruct the opening of the Eustachian tubes in the nasopharynx. Without proper function of the Eustachian tube, negative pressure can build in the middle ear. This negative pressure can lead to the formation of an effusion which can cause conductive hearing loss and serve as a breeding ground for bacteria.
Long-standing adenoiditis with subsequent adenoid hypertrophy can lead to the development of what is known as adenoid facies or long-face syndrome. Enlarged adenoids can block the nasopharynx and result in obligate mouth breathing, which can lead to craniofacial abnormalities including a high-arched palate and retrognathic mandible 7.
Adenoiditis diagnosis
The diagnosis of acute adenoiditis is made clinically based on the findings of:
- Fever
- Purulent rhinorrhea
- Post-nasal drip
- Halitosis
- Nasal obstruction
- Throat pain
Visual inspection of the adenoids may be attempted using a laryngeal mirror or flexible nasolaryngoscope.
Laboratory testing
If it presents in the context of pharyngitis, your doctor may want to perform a rapid strep test. The purpose of doing so is two-fold. First, this will give a definitive diagnosis of the patient’s condition and help guide antibiotic therapy. Second, the doctor’s office will have a record of positive and negative strep tests which will play an important role when deciding whether an adenoidectomy, plus or minus tonsillectomy, is indicated.
In cases of persistent infection despite antibiotic therapy, your doctor may choose to perform throat cultures to help identify the causative agent and guide therapy as direct cultures of adenoids may be difficult in the office setting.
If the adenoiditis is believed to be the result of seasonal or environmental allergies, allergy skin testing may be useful in directing therapy.
Radiology testing
Sinus x-rays or sinus CT’s may be obtained to look for a source of infection in the sinuses. Lateral neck X-rays are an effective way to evaluate specifically for adenoid hypertrophy. In a patient with adenoid hypertrophy who snores a sleep study can be ordered to rule out obstructive sleep apnea.
Adenoiditis treatment
Adenoiditis is often seen clinically as a component of rhinosinusitis or pharyngitis. Due to this fact, doctors often use clinical management guidelines for rhinosinusitis and pharyngitis when approaching the treatment of adenoiditis 1.
Medical management
Watch and wait
If the clinician believes the cause of adenoiditis is by the common cold or other common viral infection they should refrain from using antibiotics. Typically, uncomplicated upper respiratory viral infections will resolve within 5-7 days 2.
Antibiotic treatment
If symptoms continue or clinical presentation is suggestive of bacterial etiology, such as a high fever or purulent discharge from the nose or throat, the first line management is antibiotics covering the most common pathogens. Amoxicillin is a commonly used first due to its good coverage and tolerability. Alternatively, cefdinir or cefuroxime may be first-line treatment. If the patient has a penicillin allergy, alternatives include clarithromycin or azithromycin. Effective antibiotic treatment should yield an improvement of symptoms in 48-72 hours. Sources suggest that treatment duration should be ten days. If the condition fails to improve after a course of amoxicillin or other first-line agents, amoxicillin-clavulanate should be prescribed to eliminate potential beta-lactamase producing organisms 2.
Allergy treatment
If the adenoiditis is believed to be secondary to environmental allergies, the patient can be given a trial of nasal steroid sprays, oral steroids, oral antihistamines, or some combination thereof to see if this produces any relief in symptoms. The patient may also receive formal allergy testing followed by immune-modulating therapy to provide relief.
Reflux treatment
If the adenoiditis is believed to be secondary to GERD treatment of this condition using lifestyle and diet modification with or without the use of H2 blockers or proton-pump inhibitors may provide sufficient relief of symptoms 4.
Surgical management
AdenoidectomyIn the absence of symptomatic improvement after treatment with amoxicillin-clavulanate or if the patient has multiple episodes of adenoiditis requiring antibiotic treatment, referral to an otolaryngologist is warranted for further evaluation and potential surgical intervention. Depending on the individual circumstances, surgical procedures may include adenoidectomy with or without tonsillectomy or functional endoscopic sinus surgery. If the patient meets the Paradise criteria for tonsillectomy, most otolaryngologists will remove the adenoids at the same time to remove another possible source of recurrent infections 9.
What happens during adenoids surgery
Surgery, no matter how common or simple the procedure, can be frightening for both kids and parents. You can help prepare your child for surgery by talking about what to expect. During the adenoidectomy:
- Your child will receive general anesthesia. This means the surgery will be performed in an operating room so that an anesthesiologist can monitor your child.
- Your child will be asleep for about 20 minutes.
- The surgeon can get to the tonsils and/or the adenoids through your child’s open mouth — there’s no need to cut through skin.
- The surgeon removes the adenoids and then controls any bleeding.
Your child will wake up in the recovery area. In most cases, a child can go home the same day as the procedure. Some children may need to stay overnight for observation.
The typical recovery after an adenoidectomy often involves several days of moderate pain and discomfort, which may include sore throat, runny nose, and bad breath.
In less than a week after surgery, everything should return to normal and the problems caused by the adenoids should be gone. There are no stitches to worry about, and the adenoid area will heal naturally.
When is adenoids surgery necessary?
There are actually quite a number of reasons that your doctor may recommend removal of your child’s adenoids. If swollen or infected adenoids keep bothering your child and are not controlled by medication, the doctor may recommend surgically removing them with an adenoidectomy. This may be recommended if your child has one or more of the following:
- difficulty breathing
- obstructive sleep apnea
- repeated infections
- frequent sinus infections
- ear infections, middle ear fluid, and hearing loss requiring a second or third set of ear tubes
Today, the most common reason that children have their adenoid removed is to help them breathe and sleep better. In some children, the adenoid becomes too big. This may happen for a variety of reasons, but we usually don’t know why it happens to a particular child. If the adenoid becomes too large it can partially block a child’s breathing during sleep. In severe cases, the adenoid can completely block the back of the nose! This will usually result in loud snoring and sometimes causes a child’s sleep to be very restless or fragmented resulting in poor concentration during the daytime, behavior changes, and sometime persistent bedwetting. This is known as sleep apnea. Removing the adenoid (and sometimes the tonsils too) makes this breathing much better. Sometimes just the adenoid needs to be removed and sometimes both the tonsils and adenoids need to come out to solve this problem.
Another common reason that children have their adenoid removed is because of frequent ear infections. The adenoid is located next to the opening of the Eustachian tube [yoo-STAY-shun] in the back of the nose. Normal Eustachian tube function is responsible for keeping our ears healthy. When the tube is blocked or inflamed, middle ear infections or middle ear fluid can result. A large or constantly infected adenoid can lead to poor Eustachian tube function. When this kind of adenoid is removed, ear infections and fluid are less likely to occur.
A less common reason to remove the adenoid is for recurrent nasal infections. Some children have recurrent nasal infections characterized by thick, green or yellow drainage that is present more or less all the time. Sometimes this drainage will improve with antibiotics, but often returns when the antibiotics are stopped. Left untreated for a long period of time this can even lead to chronic inflammation of the sinuses. Removal of the adenoid will often help manage this problem, although it will not prevent the common cold or every illness that causes nasal drainage.
Having your child’s adenoids removed is especially important if repeated infections lead to sinus and ear infections. Badly swollen adenoids can interfere with the ability of the middle ear space to stay ventilated. This can sometimes lead to infections or middle ear fluid causing a temporary hearing loss. So kids whose infected adenoids cause frequent earaches and fluid buildup might also need an adenoidectomy at the time of their ear tube surgery.
And although adenoids can be taken out without the tonsils, if your child is having tonsil problems, they may be removed at the same time. A tonsillectomy with an adenoidectomy is a common pediatric operation.
What can I expect after adenoids surgery?
The procedure itself usually takes 20 to 30 minutes. Your doctor will talk to you as soon as the surgery is over.
Your child will wake up in the recovery room after surgery. This may take 45 minutes to an hour. When your child is awake, he or she will be taken to the Short Stay post operative area to complete the recovery. You can be with your child once he or she has been transferred to this area.
Children usually go home the same day after surgery, but in some cases your doctor may recommend keeping your child in the hospital overnight (e.g., your child is under age 4 and had his or her tonsils removed). If your child does stay overnight, one parent is required to stay overnight too.
An upset stomach and vomiting (throwing up) are common for the first 24 hours after surgery.
If just the adenoid is removed (not the tonsils too) your child’s throat will be mildly sore for a day or two after surgery. Most children are able to eat and drink normally within a few hours after surgery, even if their throat hurts a little. It is very important that your child drink plenty of fluids after surgery. If your child complains of neck pain, throat pain, or difficulty swallowing you can give your child plain Tylenol® (acetaminophen) or Children’s Motrin® (ibuprofen). Prescription pain medications are not necessary.
Antibiotics are no longer routinely prescribed following adenoid surgery.
Your child may have a fever for 3-4 days after surgery. This is normal and is not cause for alarm.
Neck soreness, bad breath, and snoring are also common after surgery. These symptoms will also go away during the first 3 weeks after surgery.
How should I take care of my child after adenoids surgery?
It is important to encourage your child to drink plenty of liquids. Keeping the throat moist decreases discomfort and prevents dehydration (a dangerous condition in which the body does not have enough water). There are no specific dietary restrictions after adenoidectomy. In other words, your child can eat whatever you would normally feed him or her.
In most cases, your child may return to his or her regular activities within 1 or 2 days after surgery. There is no need to restrict normal activity after your child feels back to normal. Vigorous exercise (such as swimming and running) should be avoided for 1 week after surgery.
What else do I need to know?
Upset stomach and vomiting are common during the first 24 to 48 hours after surgery. If vomiting continues for more than 1 or 2 days after surgery, call our office.
Signs of dehydration include sunken eyes, dry and sticky lips, no urine for over 8 hours, and no tears. If your child has these signs you should call our office.
Streaks of blood seen if your child sneezes or blows the nose are common during the first few hours and should be no cause for alarm.
Severe bleeding is rare after adenoidectomy. If your child coughs up, throws up, or spits out bright red blood or blood clots you should bring him or her to the emergency room at Children’s Hospital immediately. Although rare, this type of bleeding can occur up to 2 weeks after surgery.
Will my child’s immune system be weaker if the adenoid is removed?
The adenoid is only a very small part of your immune system. It turns out that your immune system has many different ways of learning to recognize germs. Children who have their adenoid and even the tonsils removed do not, on average, have any more illnesses than children who “keep” their adenoid. In fact, some children will get fewer illnesses, like recurrent nasal infections, after their adenoid is taken out.
Adenoiditis prognosis
The medical treatment available for treating adenoiditis should be capable of treating most cases successfully. For those with recurrent disease, an adenoidectomy surgery provides a definitive solution by removing all the adenoid tissues.
References- Bowers I, Shermetaro C. Adenoiditis. [Updated 2019 Jun 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536931
- American Academy of Pediatrics. Subcommittee on Management of Sinusitis and Committee on Quality Improvement. Clinical practice guideline: management of sinusitis. Pediatrics. 2001 Sep;108(3):798-808.
- Zuliani G, Carron M, Gurrola J, Coleman C, Haupert M, Berk R, Coticchia J. Identification of adenoid biofilms in chronic rhinosinusitis. Int. J. Pediatr. Otorhinolaryngol. 2006 Sep;70(9):1613-7.
- Niu X, Wu ZH, Xiao XY, Chen X. The relationship between adenoid hypertrophy and gastroesophageal reflux disease: A meta-analysis. Medicine (Baltimore). 2018 Oct;97(41):e12540.
- Shin KS, Cho SH, Kim KR, Tae K, Lee SH, Park CW, Jeong JH. The role of adenoids in pediatric rhinosinusitis. Int. J. Pediatr. Otorhinolaryngol. 2008 Nov;72(11):1643-50.
- Cho KS, Kim SH, Hong SL, Lee J, Mun SJ, Roh YE, Kim YM, Kim HY. Local Atopy in Childhood Adenotonsillar Hypertrophy. Am J Rhinol Allergy. 2018 May;32(3):160-166.
- Koca CF, Erdem T, Bayındır T. The effect of adenoid hypertrophy on maxillofacial development: an objective photographic analysis. J Otolaryngol Head Neck Surg. 2016 Sep 20;45(1):48.
- Marzouk H, Aynehchi B, Thakkar P, Abramowitz T, Goldsmith A. The utility of nasopharyngeal culture in the management of chronic adenoiditis. Int. J. Pediatr. Otorhinolaryngol. 2012 Oct;76(10):1413-5.
- Šumilo D, Nichols L, Ryan R, Marshall T. Incidence of indications for tonsillectomy and frequency of evidence-based surgery: a 12-year retrospective cohort study of primary care electronic records. Br J Gen Pract. 2019 Jan;69(678):e33-e41