Condensing osteitis
Condensing osteitis is a condition that results in increased bone density at the base of a tooth’s root. Condensing osteitis is a localized form of reactive osteitis and bone sclerosis that surrounds the apices of teeth most often occurs as a response to chronic inflammation in the dental pulp (pulpitis) or pulpal necrosis, the interior part of a tooth. Condensing osteitis occurs in children and young adults, usually in the premolar and molar areas of the mandible 1. The adjacent tooth usually has a thickened periodontal ligament or periapical inflammatory lesion (eg, granuloma, cyst, or abscess).
The most common radiopaque lesion in the jaws is condensing osteitis, which occurs in 4–8% of the general population 2. For example, Williams and Brooks 3 report a condensing osteitis prevalence of 4.5% and Marmary and Kutiner 4 report a condensing osteitis prevalence of 6.7% in radiographically examined patients. In the Williams and Brooks’ study 3, 1585 full-mouth periapical radiographs were obtained from adults to evaluate the presence of idiopathic osteosclerosis or condensing osteitis lesions. One hundred eighty-seven lesions were identified. After a follow-up period of 2–28 years, 180 (96%) lesions remained; of these, 155 were unchanged in size, 18 lesions were smaller, and seven lesions were larger. In a Taiwanese study 5, the authors have indicated that most teeth associated with condensing osteitis showed previous endodontic problems in which the root canal therapy performed on these condensing osteitis teeth was inadequate. It has also been reported that condensing osteitis lesions will subside or decrease in size, after adequate root canal therapy and obturation 6. However, a condensing osteitis lesion will not subside if the condensing osteitis lesions are the result of inadequate root canal treatment. In the Eliasson study 6, the researchers found condensing osteitis lesions regressed entirely from 36 of 49 roots. Furthermore, no condensing osteitis showed any reduction in bone mass. That report showed that most cases of condensing osteitis were associated with teeth with inadequate root canal therapy. Based on previous literature results, it appears that condensing osteitis can be successfully treated by appropriate endodontic procedures and that healing can include total regression of the sclerotic bone 5, the researchers found that the condensing osteitis prevalence among their patients was 5.7%.
On radiographs, the typical feature of condensing osteitis consists of a uniform dense nonexpansile radiopaque mass that is adjacent to the apex of the tooth and has well-defined margins and a vague transition to the surrounding bone that occurs in combination with the apical loss of lamina dura and widening of the periodontal ligament space. Unlike condensing osteitis, idiopathic sclerosis is often unrelated to pathologic lesions of the dental pulp and it is neither an inflammatory nor neoplastic process. Condensing osteitis is commonly identified in the mandible and is most frequently associated with the mandibular first molar and female patients 7. Other common sites of condensing osteitis can also occur in edentulous areas, with teeth that received root canal, and in carious, inflamed, or necrotic pulps 8.
In a study 5, the authors showed that the molar area, especially the first molar, is the most frequent tooth to develop condensing osteitis (with a female predominance). This result is in agreement with a previous report that indicated condensing osteitis lesions were exclusively in the mandible and most commonly localized adjacent to the first mandibular molar 4. This observation can be partly explained by the fact that caries, traumatic occlusion stress, and pulpal infections are more frequently encountered in molar teeth than in premolar and anterior teeth. In addition, when panoramic radiographs were examined and assessed, the superimposition of the anterior mandible will limit the interpretation in the anterior mandible.
Other previous studies have also reported that condensing osteitis lesions predominantly occur in female patients. For example, Geist and Katz 9 and McDonnell 10 report that the female to male ratio of condensing osteitis is 1.5:1 and 2:1, respectively. Avramidou et al 11 determined that female patients were more likely to have radiopaque lesions than men. The high incidence of condensing osteitis in females may be explained by some of the female-specific hormones that affect bone growth 12. Estrogen, for example, has an important role in the growth and maturation of bone, and in the regulation of bone turnover in adult bone. During bone growth, estrogen is needed for proper closure of the epiphyseal growth plates in females and males. It has been reported that skeletal estrogen deficiency in the young can increase osteoclast formation and enhance bone resorption, and menopause estrogen deficiency can induce cancellous and cortical bone loss 12. Therefore, a future study with a larger sample population and longitudinal follow-up is necessary to clarify the association between female hormones and condensing osteitis.
While condensing osteitis may not cause any symptoms, it’s important for your dentist to monitor the condition and advise you on your treatment options.
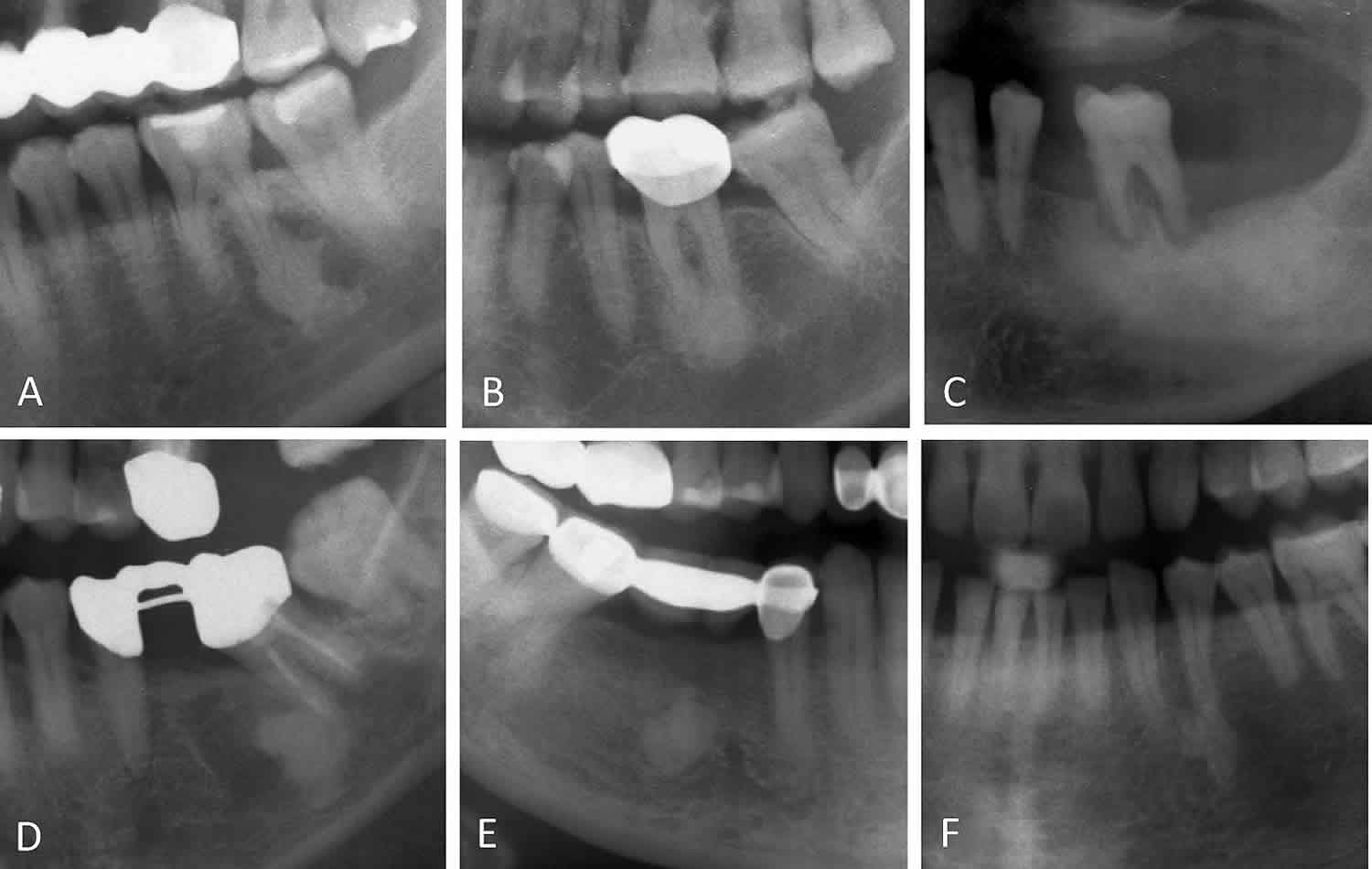
Figure 1. Condensing osteitis
Footnote: Condensing osteitis is associated with teeth with (A) a large restoration, (B) a crown, (C) periodontal disease, (D) root canal therapy, and (E) an extracted area. (F) A radiopaque lesion in the apical area and the associated intact tooth is classified as idiopathic osteosclerosis.
[Source 5 ]Figure 2. Condensing osteitis mandible
Footnote: Coronal CT image shows a poorly marginated nonexpansile sclerotic lesion (arrows), a finding indicative of condensing osteitis. The lesion is associated with a carious lesion (arrowhead).
[Source 1 ]Condensing osteitis causes
When you have an infected tooth or a dead nerve in a tooth from decay or trauma, the inflammation can sometimes cause bone growth in the jawbone. It’s important to note that this response is not severe and doesn’t destroy the bone. However, the affected area will develop more bone density and smaller bone marrow spaces. Often, patients won’t experience any pain or symptoms.
Typically, condensing osteitis affects the lower back teeth. According to a study published in Brazilian Oral Research, the condition usually appears in patients between the ages of 30 and 70.
Condensing osteitis deposits usually include histologically normal bone marrow replaced by fibrous connective tissue, and are occasionally accompanied by inflammatory cell infiltration, de novo bone formation, and the presence of bone sequestrum 5 Because of the inclusion of dense trabeculae within a reduced and limited area of bone marrow, condensing osteitis often resemble compact bone. The condensing osteitis bone tissue can contain osteoblasts, whereas the bone marrow contains lymphocytic infiltration. Condensing osteitis is characterized by dominant osteoblast activity that results in bone apposition. In this situation, mild periapical infection-stimulated bone apposition is frequently observed in patients with a very high level of tissue resistance.
Condensing osteitis symptoms
Condensing osteitis is an asymptomatic, uniformly radiopaque foci of dense bone; its manifestation is often the complication of dental infection 5.
Condensing osteitis diagnosis
Because a patient with condensing osteitis may not experience or report any pain, dental professionals usually make the diagnosis by spotting the condition on a routine X-ray and evaluating the associated tooth for problems with the pulp. The bone growth will appear as an opaque area under the root of the tooth on a dental X-ray. In contrast, severe destruction of bone will appear transparent on an X-ray and will often be associated with pain and swelling.
By using diagnostic X-ray equipment, dentists can make this assessment without conducting a biopsy of the bony area. Especially considering that the condition may not cause any symptoms, it’s important to see your dentist for regular exams and X-rays so they can diagnose any potential dental issues as soon as possible.
Condensing osteitis differential diagnosis
For many radiologists, radiopaque jaw lesions are terra incognita—Latin for “unknown land.”
The first question to be answered is whether a lesion is lytic, sclerotic, or mixed or if it has ground-glass attenuation 1. The term ground-glass appearance refers to lesions with mostly relatively homogeneous, intermediate attenuation between that of normal cortical bone and soft tissue, an appearance that is analogous to the obturating surfaces of glass stoppers used in laboratory glassware 1.
The second question is whether the transition zone between clearly normal and clearly abnormal bone is narrow or wide. Although it is usually used to help differentiate benign, slow-growing lesions (those with a narrow transition zone) from more aggressive lesions (those with a wide transition zone), the transition zone may also be used to differentiate lesions with otherwise similar appearances, such as ossifying fibromas and fibrous dysplasia.
The third question is whether the lesion is related to a tooth (ie, if is intimately associated with a single tooth and in a tooth-bearing area of the jaw). Tooth-related lesions commonly surround a component (eg, the crown or apex) of the tooth and are usually, but not always, odontogenic in origin. A tooth-related lesion may also arise or persist at the site of a congenitally absent or extracted tooth. Lesions that are clearly not tooth-related usually indicate a lesion of osseous origin. Large nonodontogenic lesions may abut adjacent teeth, and it may be difficult to determine whether they are tooth related or not.
Teeth arise from an embryologic structure known as the tooth bud. The constituent cells of the tooth bud arise from the ectoderm of the first branchial arch and ectomesenchyme from the neural crest and organize into the three important generative components of the tooth anlage: the enamel organ, dental papilla, and dental follicle. The enamel organ arises from the branchial ectoderm and endomes the developing dental papilla. Ameloblasts develop within the enamel organ and elaborate the enamel that will cover the crown of the tooth. The dental papilla is of ectomesenchymal origin; odontoblasts that arise in dental papilla produce dentin, the dominant “hard” component of the tooth. Other mesenchymal cells in the dental papilla form the neurovascular structures of the dental pulp. The third component is the dental follicle, which also arises from ectomesenchymal precursors. The dental follicle surrounds the tooth bud and generates cementoblasts, which form dental cementum; osteoblasts, which form the alveolar bone; and fibroblasts, which form the periodontal ligaments that connect the cementum-covered dental apices (roots) to the adjacent alveolar bone.
Tooth-associated lesions may be characterized as periapical (around the apex of the tooth), interapical (between apices of two adjacent teeth), or pericoronal (around the crown of the tooth). Pericoronal lesions may arise from the ectoderm-derived components of the enamel organ (ameloblasts). Periapical lesions commonly arise from areas of endodontal or periodontal inflammatory disease or the ectomesoderm-derived components of the dental papilla (odontoblasts) or follicle (cementoblasts, fibroblasts, and osteoblasts) 13.
- Mandibular idiopathic osteosclerosis. Idiopathic osteosclerosis is a focal solitary sclerotic lesion that arises in the late 1st or early 2nd decade of life. Its cause is unknown. It is asymptomatic, is not associated with inflammation, and may remain static or demonstrate slow growth that usually stops when the patient reaches skeletal maturity. In 90% of patients it occurs in the mandible, usually near the first molar or second molar or premolar. At imaging, idiopathic osteosclerosis has sharp margins and is small and round or oval, sclerotic, periapical, and tooth related, occasionally with peripheral spiculation. In 20% of patients, it is not related to a tooth. Idiopathic ostersclerosis is not expansile and has no low-attenuation rim 14. Some patients may have multiple lesions.
- Osteomas. Osteomas are benign tumors composed of mature compact or cancellous bone 1. Osteomas most commonly arise in the craniofacial bones. The most common location in the jaw is the posterior mandibular body or condyle. Multiple osteomas may be associated with Gardner syndrome 15. At imaging, osteomas appear as a non–tooth-related circumscribed sclerotic mass. Bone expansion may be present.
- Cementoblastoma. Cementoblastoma, a rare benign periapical lesion, represents less than 1% of all odontogenic tumors 1. More than 75% of cementoblastomas occur in the mandible; of those, 90% develop in the molar or premolar region. Cementoblastomas are most common in children and young adults, with 50% occurring before age 20 and 75% occurring before age 30. Although most cementoblastomas are associated with an erupted permanent tooth, they may occur near an impacted or unerupted tooth. At imaging, cementoblastomas appear as a periapical, sclerotic, sharply marginated lesion with a low-attenuation halo. They directly fuse to the root of the tooth. Some cementoblastomas may fuse to more than one tooth root or invade the root canal and pulp chamber 16. Management of cementoblastomas typically involves complete removal of the associated tooth to reduce the likelihood of recurrence 17.
- Cemento-osseous dysplasia. Cemento-osseous dysplasia represents a hamartomatous process that is usually associated with tooth apices. Its clinical forms vary, and the associated terminology may be confusing. Periapical cemento-osseous dysplasia typically arises in the anterior mandible and involves one or only a few teeth. Another limited form that occurs in the posterior jaw and typically involves molar teeth is called focal cemento-osseous dysplasia. Florid cemento-osseous dysplasia typically involves two or more jaw quadrants 18. Cemento-osseous dysplasia has a strong gender and racial predisposition, with most lesions occurring in black women and women of Asian descent who are in the 4th or 5th decade of life. Only the focal variant is more commonly reported in white women. Cemento-osseous dysplasia usually produces no symptoms, but it may cause a dull ache. Florid cemento-osseous dysplasia may be complicated by osteomyelitis and drainage of necrotic bone debris into the oral cavity or to the skin surface through osteocutaneous sinus tracts. At imaging, lesions are initially lytic, with a mixed lytic and sclerotic appearance seen later, often with a central area of calcification. Early (lytic) lesions may be confused with periapical inflammatory lesions, such as cyst, granuloma, and abscess. However, in contradistinction to these inflammatory lesions, cemento-osseous dysplasia is typically associated with a vital, nonrestored tooth and an intact lamina dura and periodontal ligament, and a central area of calcification may be seen 19. Late cemento-osseous dysplasia lesions are periapical, sclerotic, and sharply marginated. A low-attenuation halo may be seen, but unlike cementoblastomas, cemento-osseous dysplasia lesions do not fuse directly to the tooth root. Cemento-osseous dysplasia may occur in the tooth-bearing jaw after dental extraction, and when multiple lesions are present, adjacent periapical lesions may coalesce. Cemento-osseous dysplasia lesions may be expansile when associated with bone cysts or osteomyelitis. The florid variant may involve the entire mandible 20.
- Odontomas. Odontomas are the most common odontogenic tumor. The result of a developmental anomaly (hamartoma), they may obstruct tooth eruption and are most commonly seen in children. Approximately one-half of all odontomas are associated with an impacted tooth, although they may develop before or after tooth eruption. At imaging, odontomas are usually pericoronal, sharply marginated, and sclerotic, with a low-attenuation halo. They may be expansile or appear purely lucent early in their evolution. Odontomas are classified as simple, compound, or complex. Simple odontomas appear as supernumerary teeth. Compound odontomas consist of multiple small toothlike structures called denticles and most commonly arise in the anterior maxilla. Complex odontomas appear as an amorphous hyperattenuating conglomerate mass of enamel and dentin, most commonly in the molar regions the jaws. A complex odontoma may be confused with an osteoma; the low-attenuation halo that surrounds odontoma may help differentiate these lesions 21. Occasionally, odontoma is associated with dentigerous or calcifying odontogenic cysts 18.
NOTE: An abnormal result with pulp testing strongly suggests condensing osteitis and tends to rule out osteosclerosis and cementoblastoma.
Condensing osteitis treatment
After evaluating your affected tooth, your dental professional will be able to advise you on the best treatment plan. They may simply choose to monitor the increased bone density if it does not appear to be urgent or concerning. However, you will likely need treatment for the dental infection that caused the inflammatory response in the jawbone.
Treating an infected tooth often requires a root canal procedure. Root canal treatment is very common, predictable and designed to be painless. You may be able to receive the treatment at your dentist’s office, or your dentist may refer you to a specialized doctor called an endodontist. After the procedure, your dentist will work with you to determine how to best restore the tooth so it can be healthy for the rest of your life.
While you may not be able to control your body’s response to an infection in a tooth, maintaining a good oral care routine will help you avoid dental infections and decay from the outset. Remember to brush your teeth twice daily, floss once a day and see your dentist for regular checkups, including X-rays, so they can identify and treat any potential issues affecting your dental health.
References- Radiopaque Jaw Lesions: An Approach to the Differential Diagnosis. Joel K. Curé, Surjith Vattoth, and Ritu Shah. RadioGraphics 2012 32:7, 1909-1925 https://pubs.rsna.org/doi/full/10.1148/rg.327125003
- R. Eversole, L. Su, S. ElMofty. Benign fibro-osseous lesions of the craniofacial complex. A review. Head Neck Pathol, 2 (2008), pp. 177-202
- T.P. Williams, S.L. Brooks. A longitudinal study of idiopathic osteosclerosis and condensing osteitis. Dentomaxillofac Radiol, 27 (1998), pp. 275-278
- Y. Marmary, G. Kutiner. A radiographic survey of periapical jawbone lesions. Oral Surg Oral Med Oral Pathol, 61 (1986), pp. 405-408
- Frequency and distribution of mandibular condensing osteitis lesions in a Taiwanese population. Journal of Dental Sciences Volume 10, Issue 3, September 2015, Pages 291-295 https://doi.org/10.1016/j.jds.2014.10.002
- S. Eliasson, C. Halvarsson, C. Ljungheimer. Periapical condensing osteitis and endodontic treatment. Oral Surg Oral Med Oral Pathol, 57 (1984), pp. 195-199
- R. Monahan. Periapical and localized radiopacities. Dent Clin North Am, 38 (1994), pp. 113-136
- T.L. Green, R.E. Walton, J.M. Clark, D. Maixner. Histologic examination of condensing osteitis in cadaver specimens. J Endod, 39 (2013), pp. 977-979
- J.R. Geist, J.O. Katz. The frequency and distribution of idiopathic osteosclerosis. Oral Surg Oral Med Oral Pathol, 69 (1990), pp. 388-393
- D. McDonnell. Dense bone island. A review of 107 patients. Oral Surg Oral Med Oral Pathol, 76 (1993), pp. 124-128
- F.M. Avramidou, E. Markou, T. Lambrianidis. Cross-sectional study of the radiographic appearance of radiopaque lesions of the jawbones in a sample of Greek dental patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 106 (2008), pp. e38-43
- T. Thomas, B. Burguera, L.J. Melton 3rd, et al. Role of serum leptin, insulin, and estrogen levels as potential mediators of the relationship between fat mass and bone mineral density in men versus women. Bone, 29 (2001), pp. 114-120
- Morgan PR. Odontogenic tumors: a review. Periodontol 2000 2011;57(1):160–176.
- MacDonald-Jankowski DS. Idiopathic osteosclerosis in the jaws of Britons and of the Hong Kong Chinese: radiology and systematic review. Dentomaxillofac Radiol 1999;28(6):357–363.
- Fonseca LC, Kodama NK, Nunes FC et al.. Radiographic assessment of Gardner’s syndrome. Dentomaxillofac Radiol 2007;36(2):121–124.
- Kaneda T, Minami M, Kurabayashi T. Benign odontogenic tumors of the mandible and maxilla. Neuroimaging Clin N Am 2003;13(3):495–507.
- Zaitoun H, Kujan O, Sloan P. An unusual recurrent cementoblastoma associated with a developing lower second molar tooth: a case report. J Oral Maxillofac Surg 2007;65(10):2080–2082.
- Slootweg PJ. Lesions of the jaws. Histopathology 2009;54(4):401–418.
- Resnick CM, Novelline RA. Cemento-osseous dysplasia, a radiological mimic of periapical dental abscess. Emerg Radiol 2008;15(6):367–374.
- Summerlin DJ, Tomich CE. Focal cemento-osseous dysplasia: a clinicopathologic study of 221 cases. Oral Surg Oral Med Oral Pathol 1994;78(5):611–620.
- Theodorou SJ, Theodorou DJ, Sartoris DJ. Imaging characteristics of neoplasms and other lesions of the jawbones: part 1—odontogenic tumors and tumorlike lesions. Clin Imaging 2007;31(2):114–119.