What is androgenic alopecia
Androgenetic alopecia is a common form of hair loss in both men and women. In men, androgenic alopecia is also known as male-pattern baldness. Androgenetic alopecia in women is referred to as ‘female pattern hair loss’ or male-pattern baldness. Pattern or androgenetic alopecia is a genetically predetermined disorder due to excessive response to androgens which affects up to 50% of males and females 1. Androgenetic alopecia is the most common type of hair loss, affecting approximately 50% of men over the age of 50 and around 50% of women over the age of 65. Androgenetic alopecia is characterized by progressive loss of terminal hair of the scalp any time after puberty, in a characteristic distribution in both males and females. Hair is lost in a well-defined pattern, beginning above both temples. Over time, the hairline recedes to form a characteristic “M” shape. Hair also thins at the crown (near the top of the head), often progressing to partial or complete baldness. Unlike other areas of the body, hairs on the scalp to grow in tufts of 3–4. In androgenetic alopecia, the tufts progressively lose hairs. Eventually, when all the hairs in the tuft are gone, bald scalp appears between the hairs.
The pattern of hair loss in women differs from male-pattern baldness. In women, the hair becomes thinner all over the head, and the hairline does not recede. Androgenetic alopecia in women rarely leads to total baldness 2.
Androgenetic alopecia is a frequent cause of hair loss in both men and women. This form of hair loss affects an estimated 50 million men and 30 million women in the United States. Androgenetic alopecia can start as early as a person’s teens and risk increases with age; more than 50 percent of men over age 50 have some degree of hair loss. In women, hair loss is most likely after menopause.
White patients are most affected followed by Asians and African Americans, then Native Americans and Eskimos. The incidence approximates the age in Caucasian males, with 50% affected by 50 years old and up to 80% affected by 70 years old. In females, the disorder is quite common, with an increase in incidence after menopause 3.
Androgenetic alopecia in men has been associated with several other medical conditions including coronary heart disease and enlargement of the prostate. Additionally, prostate cancer, disorders of insulin resistance (such as diabetes and obesity), and high blood pressure (hypertension) have been related to androgenetic alopecia. In women, androgenetic alopecia is associated with an increased risk of polycystic ovary syndrome (PCOS). PCOS is characterized by a hormonal imbalance that can lead to irregular menstruation, acne, excess hair elsewhere on the body (hirsutism), and weight gain.
Multiple studies demonstrate a strong relationship between pattern baldness, especially early onset or vertex loss of hair, with cardiovascular disease including hypertension, myocardial infarction, insulin resistance, death from diabetes or heart disease, abnormal lipids, obesity, and infertility.
The data is mixed regarding the androgenetic alopecia relationship with benign prostate hypertrophy. However, there is some data suggesting a two-fold risk of prostate cancer and a higher incidence of death from the prostate cancer. There is also a modest increase in the risk of colon cancer and urolithiasis in patients with androgenetic alopecia.
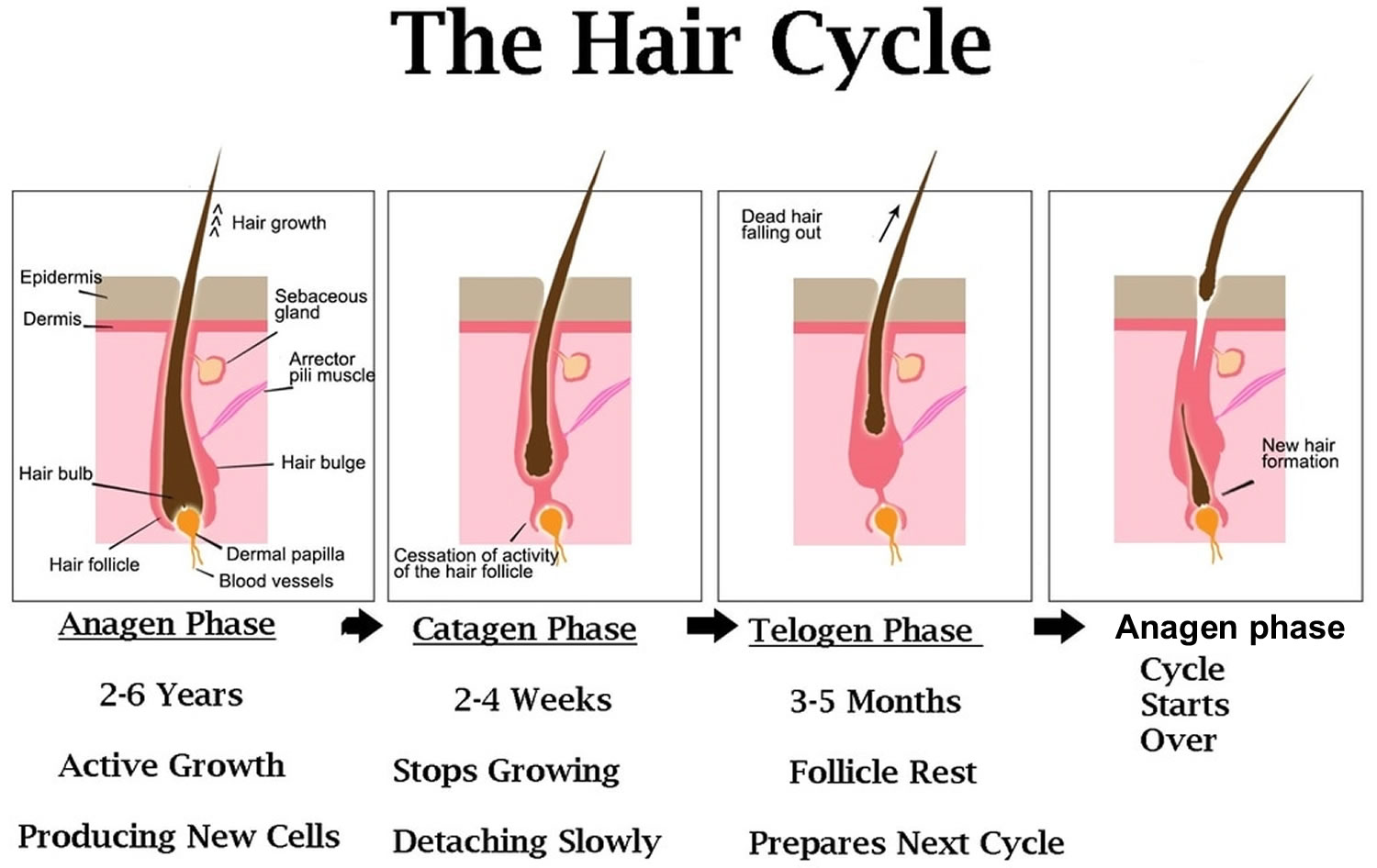
Normal hair growth cycle
The scalp contains, on average, 100,000 hairs 4. You lose up to 100 hairs from your scalp every day. That’s normal, and in most people, those hairs grow back. A hair shaft grows within a hair follicle at a rate of about 1 – 1.5 cm per month. It is due to cell division within the hair bulb at the base of the hair follicle. The cells produce the three layers of the hair shaft (medulla, cortex, cuticle), which are mainly made of the protein keratin (which is also the main structure of skin and nails). Hair growth follows a cycle and the hair growth cycle is divided into three phases: anagen (active growing stage, about 90 % of hairs), catagen (degeneration stage, less than 10% of hairs) and telogen (resting stage, 5% to 10% of hairs). Hair is shed during the telogen phase. When telogen hairs are shed, new anagen hairs grow to replace them, beginning a new cycle 5, 6. These phases are not synchronized, and any hair may be at a particular phase at random. Hair length depends on the duration of anagen. Short hairs (eyelashes, eyebrows, hair on arms and legs) have a short anagen phase of around one month. Anagen lasts up to 6 years or longer in scalp hair. In addition to the ratio of anagen hair to telogen hair, the diameter of the hair follicles determines scalp coverage. Vellus hairs have a hair-shaft diameter of less than 0.03 mm, whereas terminal hairs have a diameter greater than 0.06 mm. The optimal hairs for scalp-hair growth and scalp coverage are anagen and terminal hairs.
Timespan of the hair growth cycle
- The anagen phase constitutes about 90% (1000 days or more) of the growth cycle. Anagen hairs are anchored deeply into the subcutaneous fat and cannot be pulled out easily.
- The catagen phase (10 days) and telogen phase (100 days) constitute only 10% of the hair growth cycle.
- During the catagen and telogen phase of the hair growth cycle, as hairs are at the shedding and rest-from-growth period, no bald spots are shown as hairs are randomly distributed over the scalp.
Anagen (active growing stage, about 90 % of hairs) stage
Your hair grows around 1 – 1.5 cm per month, faster in summer than in winter.
- The anagen stage is the growing period of a hair follicle.
- This stage typically lasts about 3 to 5 years. Asian hair can last 5-7 years
- Full length hair can be upto 100 cm long
Catagen (degeneration stage, less than 10% of hairs) stage
At the end of the anagen phase, your hair enters the catagen phase.
The catagen stage is the intermediate period of hair growth.
- Hair follicles prepare themselves for the resting phase.
- It lasts around 1-2 weeks.
- During this phase, the deeper portions of the hair follicles start to collapse.
Telogen (resting stage, 5% to 10% of hairs) stage
During the telogen phase each hair is released and falls out
- The telogen stage is the resting and shedding period of the hair cycle.
- The follicle remains inactive for 3 to 4 months.
- At the end of this period, older hairs that have finished their life will fall out and newer hairs will begin to grow.
- As compared with anagen hair, telogen hair is located higher in the skin and can be pulled out relatively easily. Normally, the scalp loses approximately 100 telogen hairs per day.
Hair loss, hair thinning and problems with hairgrowth occur when the growth cycle is interrupted/disrupted. This can be triggered by conditions such as nutritional and medical situations, illness or stress. For instance 6 weeks after intensive dieting or stress you can experience hair loss. This occurs because the growing stage (Anagen) is cut short and hairs enter the falling (Telogen) stage at the same time.
Figure 1. Hair growth cycle
Is androgenetic alopecia permanent?
The hair follicles affected by androgenetic alopecia are permanently damaged. There are treatments which can help to delay the process, but hairs that have been lost will not grow back.
Androgenetic alopecia male
Androgenetic alopecia male or male pattern hair loss is the most common type of thinning of the hair and balding that occurs in adult males.
Male pattern hair loss occurs in men who are genetically predisposed to be more sensitive to the effects of dihydrotestosterone (DHT). Researchers now believe that the condition can be inherited from either side of the family. DHT (dihydrotestosterone) is found in several tissues in the body including the prostate gland and skin. 5-alpha reductase is an enzyme that regulates the production of dihydrotestosterone (DHT). An enzyme is a protein that acts as a catalyst to speed up a chemical reaction. 5-alpha reductase can be inhibited by specially synthesized drugs.
- Male pattern hair loss is due to a combination of hormones (androgens) and a genetic predisposition.
- Male pattern hair loss is also called androgenetic alopecia.
- It is characterised by a receding hairline and hair loss on the top and front of the head.
- A similar type of hair loss in women, female pattern hair loss, results in thinning hair on the mid-frontal area of the scalp and is generally less severe than occurs in males.
Male pattern hair loss affects nearly all men at some point in their lives. It affects different populations at different rates, probably because of genetics. Up to half of male Caucasians will experience some degree of hair loss by age 50, and possibly as many as 80% by the age of 70 years, while other population groups such as Japanese and Chinese men are far less affected.
Male pattern hair loss can have a negative psychological impact. Studies have shown that hair loss can be associated with low self-esteem, depression, introversion, and feelings of unattractiveness. This is reinforced by attitudes in Western society, which place great value on youthful appearance and attractiveness. Some studies have shown that based on appearance alone, men with hair loss are seen as less attractive, less assertive, less likeable, and less successful than men without hair loss.
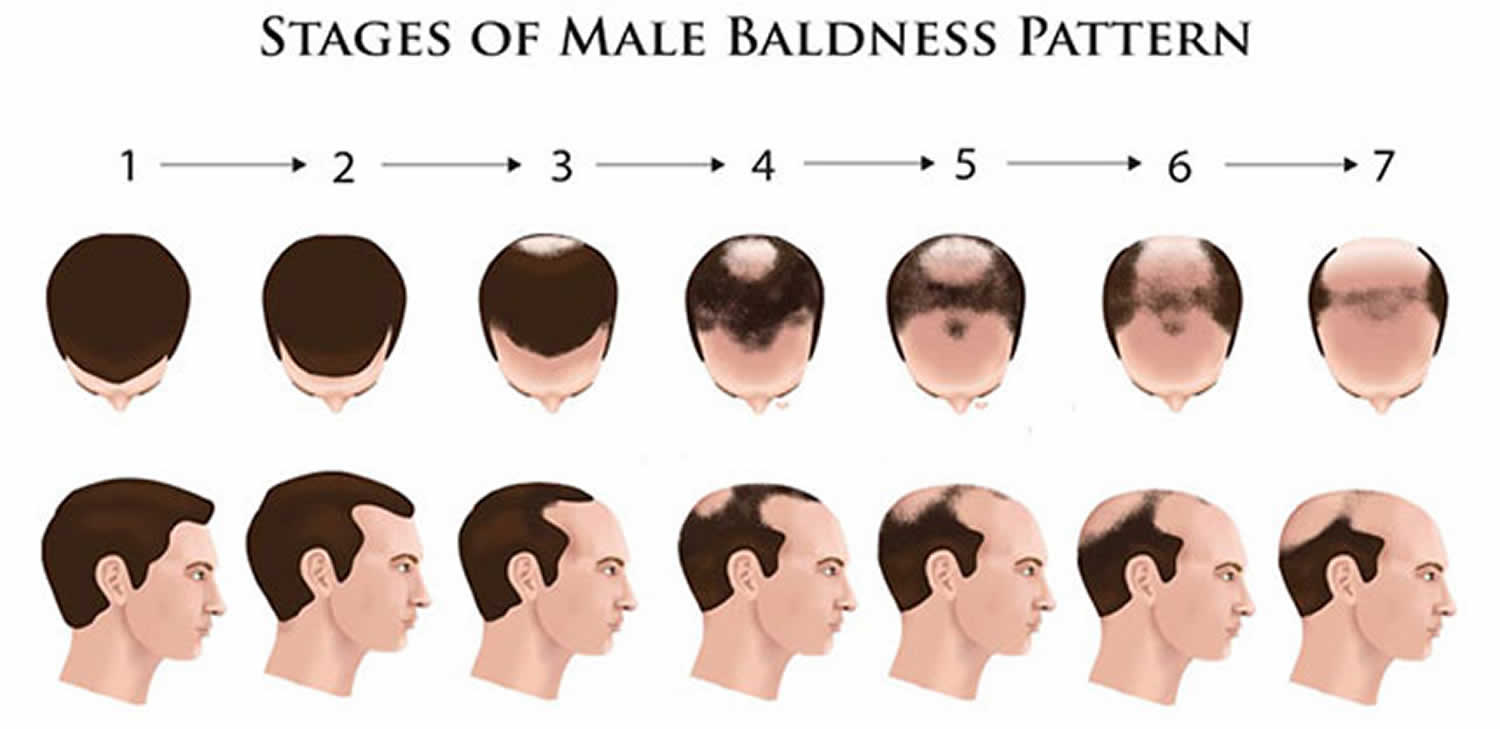
The severity of hair loss can be classified in several ways. Sinclair systems are shown below.
Figure 2. Androgenetic alopecia male
What causes androgenetic alopecia male?
Male pattern hair loss is an inherited condition, caused by a genetically determined sensitivity to the effects of dihydrotestosterone (DHT) in some areas of the scalp. DHT (dihydrotestosterone) is believed to shorten the growth, or anagen, phase of the hair cycle, from a usual duration of 3–6 years to just weeks or months. This occurs together with miniaturisation of the follicles and progressively produces fewer and finer hairs. The production of DHT is regulated by an enzyme called 5-alpha reductase.
Androgenetic alopecia male occurs in men who are genetically predisposed to be more sensitive to the effects of DHT. Researchers now believe that the condition can be inherited from either side of the family.
Several genes are involved, accounting for differing age of onset, progression, pattern and severity of hair loss in family members. The susceptibility genes are inherited from both mother and father. At this time, genetic testing for prediction of balding is unreliable.
A few women present with male pattern hair loss because they have excessive levels of androgens as well as genetic predisposition. These women also tend to suffer from acne, irregular menses and excessive facial and body hair. These symptoms are characteristic of polycystic ovarian syndrome (PCOS) although the majority of women with PCOS do not experience hair loss. Less often, congenital adrenal hyperplasia may be responsible. Females that are losing their hair with age are more likely to present with female pattern hair loss, in which hormone tests are normal.
Is androgenetic alopecia male hereditary?
Yes. It is believed male pattern hair loss can be inherited from either or both parents.
Can androgenetic alopecia male be cured?
No, there is no cure. However, it tends to progress very slowly, from several years to decades. An earlier age of onset may lead to quicker progression.
Androgenetic alopecia male signs and symptoms
Androgenetic alopecia male affects nearly all men at some point in their lives. It affects different populations at different rates, probably because of genetics. Up to half of male Caucasians will experience some degree of hair loss by age 50, and possibly as many as 80% by the age of 70 years, while other population groups such as Japanese and Chinese men are far less affected.
The severity of hair loss can be classified in several ways (see Figure 14 above).
Androgenetic alopecia male diagnosis
Your doctor will usually diagnose androgenetic alopecia by examining the pattern of hair loss on the scalp. They may also perform blood tests to measure hormone levels, serum ferritin and thyroid function.
Androgenetic alopecia male treatment
It is important to seek reliable information and advice from authoritative sources as there are many bogus treatments that are expensive and do not work.
Treatment is based on patient preference. Current treatment options include:
- Hair replacement / transplantation
- Cosmetics
- Micropigmentation (tattoo) to resemble shaven scalp
- Hairpieces
- Minoxidil solution
- Finasteride tablets (type II 5-alpha-reductase inhibitor)
- Dutasteride.
Minoxidil and oral finasteride are the only treatments currently approved by the U.S. Food and Drug Administration for the treatment of androgenetic alopecia. Both of these drugs stimulate hair regrowth in some men, but are more effective in preventing progression of hair loss. Although there are a number of other treatments listed in various texts, there is not good evidence to support their use 7.
Topical minoxidil (2% or 5% solution) is approved for the treatment of androgenetic alopecia in men 8. Minoxidil comes as a solution or foam – the easiest way to measure the correct amount is to use a large tangerine-sized blob of the foam. Hair regrowth is more robust at the vertex than in the frontal area, and will take six to 12 months to improve 9. The response to treatment should be assessed at six months – if beneficial treatment needs to be continued to maintain efficacy. Up to 40% of patients may benefit. Treatment should continue indefinitely because hair loss reoccurs when treatment is discontinued. Adverse effects include irritant and contact dermatitis.
Finasteride (Propecia), 1 mg per day orally, although a single dose of 5 mg per week is probably as effective and much cheaper for the patient and is approved to treat androgenetic alopecia in men for whom topical minoxidil has been ineffective. Adverse effects of finasteride include decreased libido, erectile dysfunction, and gynecomastia (increase in the amount of breast gland tissue in men) 10. There is some evidence that dutasteride 2.5 mg oral once daily may be more effective than finasteride.
There is some evidence that ketoconazole shampoo may also be of benefit, perhaps because it is effective in seborrheic dermatitis and dandruff.
Low-level laser therapy is of unproven benefit in pattern balding; one device has been approved by the FDA for marketing. Platelet-rich plasma injections are also under investigation. Further studies are required to determine the magnitude of the benefit if any.
Wigs and hair pieces
Some affected individuals find wigs, toupees and even hair extensions very helpful in disguising hair loss. There are two types of postiche (false hairpiece) available to individuals; these can be either synthetic or made from real hair. Synthetic wigs and hairpieces, such as a toupee, usually last about 6 to 9 months, are easy to wash and maintain, but can be susceptible to heat damage and may be hot to wear. Real hair wigs or hairpieces can look more natural, can be styled with low heat and are cooler to wear.
Skin camouflage
Spray preparations containing small pigmented fibres are available from the internet and may help to disguise the condition in some individuals. These preparations however, may wash away if the hair gets wet i.e. rain, swimming, perspiration, and they only tend to last between brushing/shampooing.
Surgical treatments
Surgical treatment includes (i) hair transplantation, a procedure where hair follicles are taken from the back and sides of the scalp and transplanted onto the bald areas; and (ii) scalp reduction, where a section of the bald area is removed and the hair-bearing scalp stretched to cover the gap. Tissue expanders may be used to stretch the skin.
Androgenetic alopecia female
Androgenetic alopecia women or female pattern hair loss is a distinctive form of hair loss that occurs in women with androgenetic alopecia; however, the role of androgens in this type of hair loss remains uncertain 11. Androgenetic alopecia female is often familial or inherited 12. Many women are affected by androgenetic alopecia female. Female-pattern hair loss can develop any time after the onset of puberty 11. Androgenetic alopecia female can affect women in any age group, but it occurs more commonly after menopause. The hair loss process is not constant and usually occurs in fits and bursts. It is not uncommon to have accelerated phases of hair loss for 3–6 months, followed by periods of stability lasting 6–18 months. Without medication, it tends to progress in severity over the next few decades of life. Around 40% of women by age 50 show signs of hair loss and less than 45% of women reach the age of 80 with a full head of hair 13. Unlike other areas of the body, hairs on the scalp grow in tufts of 3–4. In androgenetic alopecia, the tufts progressively lose hairs. Eventually, when all the hairs in the tuft are gone, bald scalp appears between the hairs.
In androgenetic alopecia female, there is diffuse thinning of hair on the scalp due to increased hair shedding or a reduction in hair volume, or both. It is normal to lose up to 50-100 hairs a day. Another condition called chronic telogen effluvium also presents with increased hair shedding and is often confused with androgenetic alopecia female. It is important to differentiate between these conditions as management for both conditions differ.
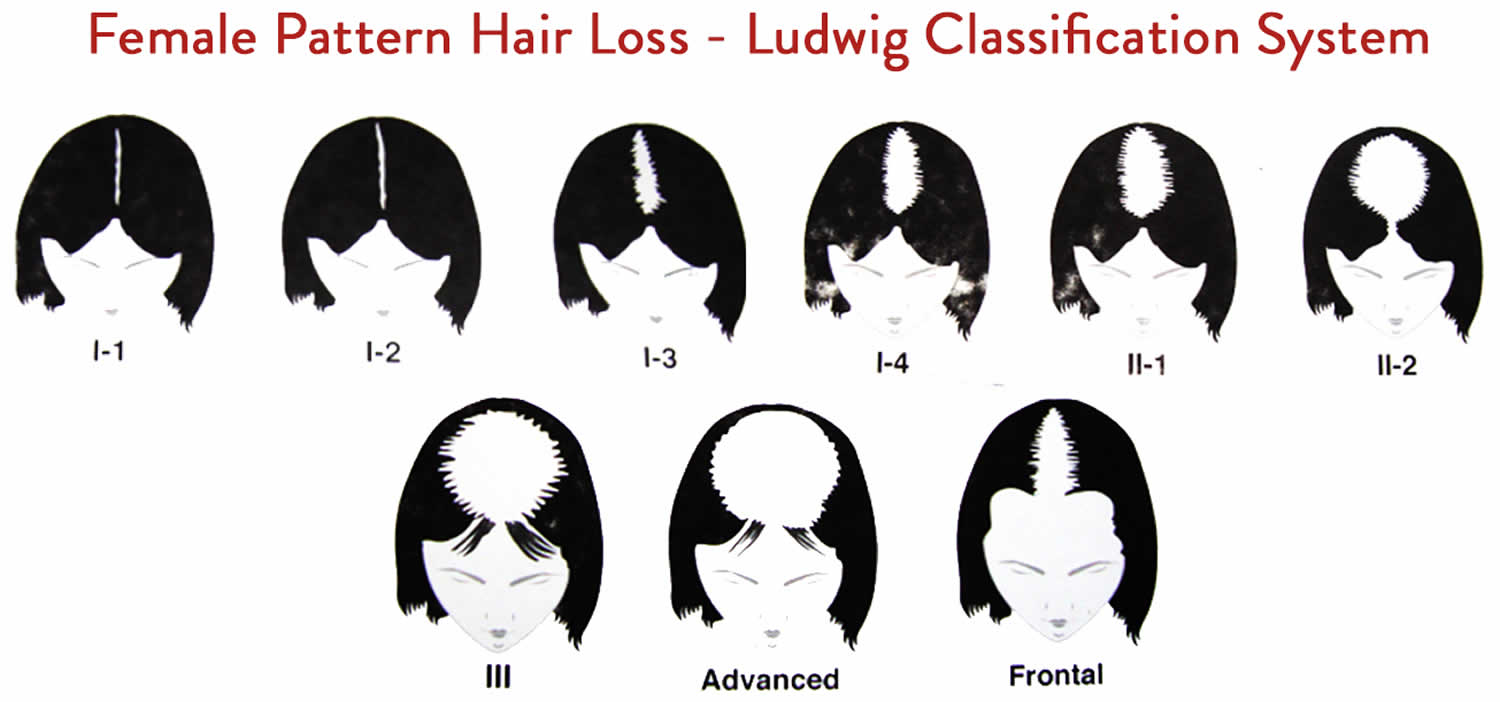
Increased hair shedding is a feature to androgenetic alopecia female. Female pattern baldness affects the central portion of the scalp, sparing the frontal hairline, and is characterized by a wider midline part on the crown than on the occipital scalp (Figure 4). In some women, hair thinning over the side area of the scalp also occurs. The severity of hair loss is staged according to the Ludwig classification (Figure 3), in which increasing stages (I to III) correspond to increasing widths of the midline part 14. Women can use the hair shedding guide below to define whether hair shedding is normal or excessive. If hair thinning is more evident in the frontal portion of the scalp, the part may resemble a fir tree in what is known as a “Christmas tree pattern” behind the frontal hair line (Figure 5). This pattern is referred to as “frontal accentuation” 11.
Androgenetic alopecia women presents quite differently from the more easily recognizable male pattern baldness, which usually begins with a receding frontal hairline that progresses to a bald patch on top of the head. It is very uncommon for women to bald following the male pattern unless there is excessive production of androgens in the body. Male patterns of hair loss may be associated with hyperandrogenism, but the majority of women with female-pattern hair loss have normal serum androgen levels 15. One study 16 showed a prevalence of biochemical hyperandrogenemia of 38.5% among women with moderate-to-severe alopecia; approximately one quarter of these women had no other signs of hyperandrogenemia, such as hirsutism or menstrual disturbances.
The hair loss associated with female pattern baldness, although permanent, requires no treatment if you are comfortable with your appearance.
There is no known prevention for hair loss; shampooing and other hair products have no adverse effects other than harsh products or practices that may damage the hair shaft, causing breakage.
Many studies have shown that hair loss is not merely a cosmetic issue, but it also causes significant psychological distress. Compared to unaffected women, those affected have a more negative body image and are less able to cope with daily functioning. Hair loss can be associated with low self-esteem, depression, introversion, and feelings of unattractiveness. It is especially hard to live in a society that places great value on youthful appearance and attractiveness.
Baseline photographs (typically of the midline part) should be taken and used on subsequent visits for comparison. To assess hair shedding, women should choose which of the six photographs of hair bundles best represents how much hair they shed on an average day.
Doctors can use the hair shedding scale to score hair loss at each patient visit to assess response to treatment. It can also be used in clinical trials to assess new treatments for excess hair shedding.
Therapies for androgenetic alopecia women include topical minoxidil (2% & 5%), antiandrogen medication and hair transplantation in selected patients. Six months to 1 year of treatment may be required before there is considerable improvement.
Figure 3. Androgenetic alopecia women
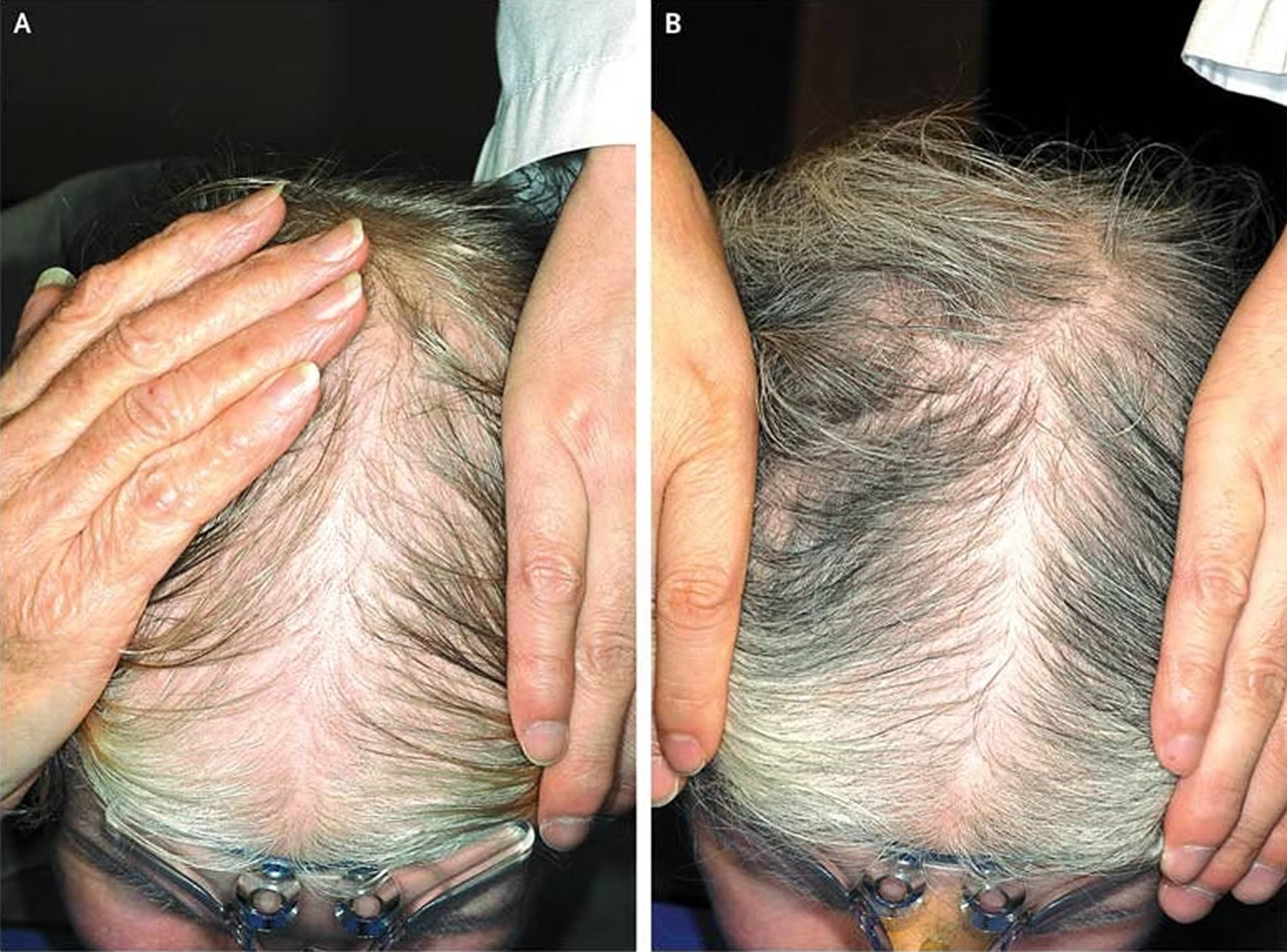
Figure 4. Female pattern hair loss
Figure 5. Female pattern hair loss with frontal accentuation (Christmas tree pattern)
Footnote: Panel A shows hair loss before topical 5% Minoxidil treatment, and Panel B shows regrowth after 6 months of treatment.
Can androgenetic alopecia female be cured?
No, there is no cure for androgenetic alopecia female. However, it tends to progress very slowly, from several years to decades. An earlier age of onset may lead to quicker progression.
Is androgenetic alopecia female inherited?
Yes. It is believed that it can be inherited from either or both parents.
How long does it take for female pattern hair loss to progress?
Androgenetic alopecia female can affect women in any age group, but it occurs more commonly after menopause. The hair loss process is not constant and usually occurs in fits and bursts. It is not uncommon to have accelerated phases of hair loss for 3–6 months, followed by periods of stability lasting 6–18 months. Without medication, it tends to progress in severity over the next few decades of life.
Androgenetic alopecia female causes
Female pattern baldness is caused by a combination of genetic and hormonal factors. The hairs produced by the affected follicles become progressively smaller in diameter, shorter in length and lighter in colour until eventually the follicles shrink completely and stop producing hair. The mode of inheritance is polygenic, indicating that there are many genes that contribute to female pattern baldness and these genes could be inherited from either parent or both. Genetic testing to assess the risk of balding is currently not recommended, as it is unreliable.
Female pattern hair loss can be associated with conditions in which androgen (a group of hormones) levels are elevated such as polycystic ovarian syndrome (PCOS). Acne, increased facial hair, irregular periods and infertility are all signs of PCOS.
Currently, it is not clear if androgens (male sex hormones) play a role in female pattern baldness, although androgens have a clear role in male pattern baldness. The majority of women with female pattern hair loss have normal levels of androgens in their bloodstream. Due to this uncertain relationship, the term androgenetic alopecia female is preferred to ‘female androgenetic alopecia’.
The role of estrogen is uncertain. Androgenetic alopecia female is more common after the menopause suggesting estrogens may be stimulatory for hair growth. But laboratory experiments have also suggested estrogens may suppress hair growth.
Androgenetic alopecia female diagnosis
Blood tests include female and male sex hormone levels as well as thyroid function, as part of the diagnostic workup.
The majority of women affected by androgenetic alopecia female do not have underlying hormonal abnormalities. However, a few women with androgenetic alopecia female are found to have excessive levels of androgens. These women also tend to suffer from acne, irregular menses and excessive facial and body hair. These symptoms are characteristic of the polycystic ovarian syndrome (PCOS) although the majority of women with PCOS do not experience hair loss. Less often, congenital adrenal hyperplasia may be responsible.
Androgenetic alopecia female treatment
It is important to seek reliable information and advice from authoritative sources as there are many bogus treatments that are expensive and do not work.
Treatments are available for androgenetic alopecia female although there is no cure. It is important to manage expectations when seeking treatment, as the aim is to slow or stop the progression of hair loss rather than to promote hair regrowth. However, some women do experience hair regrowth with treatment. Results are variable, and it is not possible to predict who may or may not benefit from treatment.
A Cochrane systematic review published in 2012 concluded that minoxidil solution was effective for androgenetic alopecia female. Minoxidil is available as 2% and 5% solutions; the stronger preparation is more likely to irritate and may cause undesirable hair growth unintentionally on areas other than the scalp.
Hormonal treatment, i.e. oral medications that block the effects of androgens (e.g. spironolactone, cyproterone, finasteride and flutamide) is also often tried.
A combination of low dose oral minoxidil (0.25 mg daily) and spironolactone (25 mg daily) has been shown to significantly improve hair growth, reduce shedding and improve hair density.
Once started, treatment needs to continue for at least six months before the benefits can be assessed, and it is important not to stop treatment without discussing it with your doctor first. Long term treatment is usually necessary to sustain the benefits.
Cosmetic camouflages include colored hair sprays to cover thinning areas on the scalp, hair bulking fiber powder, and hair wigs. Hair transplantation for androgenetic alopecia female is becoming more popular although not everyone is suitable for this procedure.
Low-level laser therapy is of unproven benefit in pattern balding, but one device has been approved by the FDA for marketing. Platelet-rich plasma injections are also under investigation. Further studies are required to determine the magnitude of the benefit if any.
Topical and oral medications
- Applying 2% or 5% minoxidil solution to the scalp every day may help to slow down the progression and partially restore hair in some women. Only the 2% strength is licensed for women; the 5% minoxidil solution can be used under the advice of a medical doctor and is expensive. Minoxidil solution should be applied to the affected scalp (not the hair) using a dropper or pump spray device and should be spread over the affected area lightly, it does not need to be massaged in. Minoxidil can cause skin reactions such as dryness, redness, scaling and/or itchiness at the site of application and should not be applied if there are cuts or open wounds. Minoxidil solution should only be applied to the scalp. Any spillage to the forehead or cheeks should be cleansed to avoid increased hair growth in these areas. Minoxidil should not be used in pregnant or nursing women. Minoxidil should be used for at least 6 months before any benefit may be noted. Any benefit will only be maintained for as long as the treatment is used. Minoxidil solution may cause an initial hair fall in the first 2-8 weeks of treatment, and this usually subsides when the new hairs start to grow.
- Antiandrogen agents such as spironolactone, cyproterone acetate, flutamide and cimetidine can block the action of dihydrotestosterone (DHT) on the scalp, which may lead to some improvement in hair loss. These treatments are not licensed for use in androgenetic alopecia female. Spironolactone and cyproterone acetate should be avoided in pregnancy since they can cause feminization of a male fetus; both should be avoided during breast feeding. Flutamide carries a risk of damaging the liver.
It is important to note that all of these topical and oral treatments only work for as long as the treatment is continued.
Minoxidil solution
Topical 2% minoxidil solution is approved by the Food and Drug Administration (FDA) for women with thinning hair due to female-pattern hair loss. In a double-blind, placebo-controlled trial, 2% minoxidil used twice daily resulted in minimal hair regrowth in 50% of women and moderate hair regrowth in 13% of women after 32 weeks of treatment, as compared with rates of 33% and 6%, respectively, in the placebo group 17. Efficacy can be assessed definitively after 6 to 12 months of treatment. Side effects of topical minoxidil therapy include contact dermatitis (attributed in many cases to irritation from propylene glycol in the solution) and symmetric facial hypertrichosis manifested as fine hairs on the cheeks or forehead in up to 7% of women. Hypertrichosis disappears within 4 months after discontinuation of the drug. Minoxidil should not be used in pregnant or nursing women.
The use of 5% minoxidil may be considered in women who do not have a response to the 2% formulation or who want more aggressive management 18. A double-blind, randomized trial comparing a 5% minoxidil solution with a 2% minoxidil solution used twice daily in women with mild-to-moderate female-pattern hair loss showed no significant difference between the two solutions with respect to investigator assessments of efficacy, but it showed significantly greater patient satisfaction with the 5% preparation 18. However, the incidences of hypertrichosis (excessive hair growth) and contact dermatitis were higher with the 5% solution than with the 2% solution. A new 5% minoxidil foam formulation that contains no propylene glycol appears to be much less likely to cause contact dermatitis than topical minoxidil solution. Although they are prescribed by many dermatologists in practice, neither the 5% minoxidil solution nor the foam preparation is FDA-approved for use in women 4.
Antiandrogen therapies
Antiandrogen agents (including the androgen-receptor blockers spironolactone, cyproterone acetate, and flutamide and the 5α-reductase inhibitor finasteride) and oral contraceptives are not commonly used to treat female-pattern hair loss in North America, but they are used more commonly in Europe 4. None of these agents are FDA-approved for female-pattern hair loss. Cyproterone acetate is not approved in the United States, and neither flutamide nor finasteride is approved for any indication in women, although finasteride is approved for the treatment of hair loss in men.
In an open-label study of cyproterone acetate (50 to 100 mg daily for 10 days of the menstrual cycle) or spironolactone (200 mg daily) in women with female-pattern hair loss, more than 80% of women had either hair regrowth or stabilization of hair loss, but this study was uncontrolled 19. In a randomized trial comparing topical 2% minoxidil solution plus an oral contraceptive with cyproterone acetate (52 mg per day) plus an oral contraceptive in women with female-pattern hair loss, the latter combination resulted in greater hair density in women with hyperandrogenism, whereas in women without hyperandrogenism, minoxidil had a greater effect 20. If antiandrogen agents are used in women of reproductive age, an oral contraceptive should be prescribed concomitantly, since these agents are known teratogens. Teratogens are substances that may produce birth defects in the human embryo or fetus after the pregnant woman is exposed.
In two small, uncontrolled studies, finasteride (Propecia) at a minimum dose of 2.5 mg per day appeared to have a benefit for women with female-pattern hair loss 21, 22. However, in a double-blind, controlled trial23 involving postmenopausal women with female-pattern hair loss, treatment with finasteride at a dose of 1 mg per day was not significantly better than placebo. Like the antiandrogens, finasteride is a known teratogen, and its use is not recommended in women of reproductive age.
Wigs and hair pieces
Some affected individuals find wigs, toupees and even hair extensions can be very helpful in disguising androgenetic alopecia female. There are two types of postiche (false hairpiece) available to individuals; these can be either synthetic or made from real hair. Synthetic wigs and hairpieces, usually last about 6 to 9 months, are easy to wash and maintain, but can be susceptible to heat damage and may be hot to wear. Real hair wigs or hairpieces can look more natural, can be styled with low heat and are cooler to wear.
Skin camouflage
Spray preparations containing small pigmented fibers are available from the internet and may help to disguise the condition in some individuals. These preparations however, may wash away if the hair gets wet (i.e. rain, swimming, perspiration), and they only tend to last between brushing/shampooing.
Surgical hair transplantation
Surgical hair transplantation is a procedure where hair follicles are taken from the back and sides of the scalp and transplanted onto the bald areas. Surgical hair transplantation is increasingly used to treat many women with female-pattern hair loss 23. Clinical experience indicates that when the newer technique of follicular-unit transplantation is performed by an experienced surgeon, a natural result is possible 4. However, data on long-term outcomes are lacking, and rates of graft failure, although considered to be very low, remain uncertain. Costs vary, but they may range from $4,000 to $15,000 per session, depending on the size of the area treated and the surgeon. One or two sessions are usually sufficient for a cosmetically acceptable result. Hair density in the donor (occipital) area must be sufficient to yield the required number of grafts with no visible scarring. Complications, which are rare, include infection, permanent scalp dysthesias, and arteriovenous malformations (which occur in less than 1% of patients). Many surgeons use minoxidil therapy in patients who have undergone hair transplantation, although this strategy has also not been rigorously studied 24.
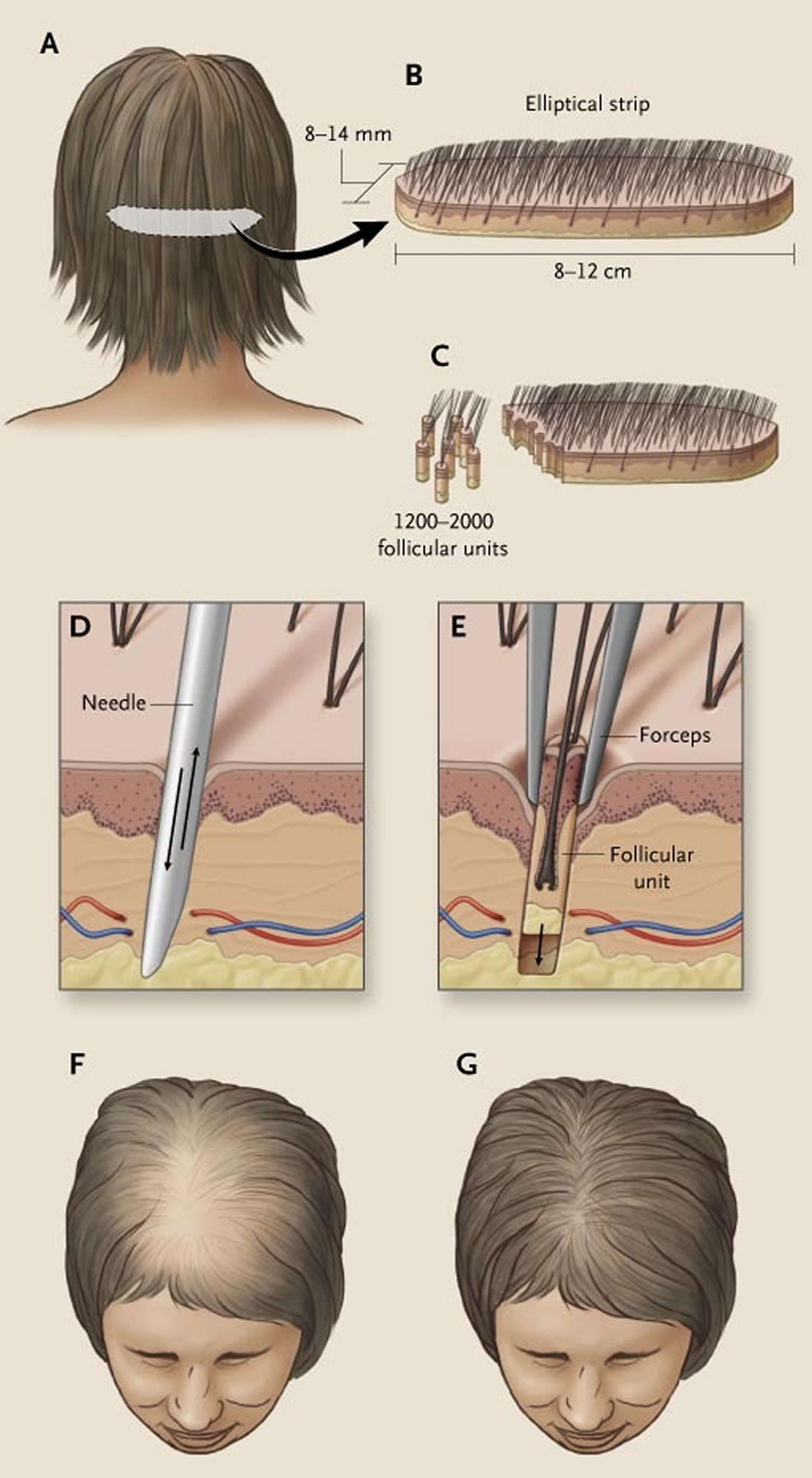
Figure 5. Hair transplantation with grafts obtained from an elliptical strip from the back of the scalp
Footnote: An elliptical strip averaging in size from 8 to 14 mm wide and 8 to 12 cm long is excised from the occipital portion of the scalp (Panels A and B). This strip is subdivided into 1200 to 2000 follicular units of two to three hairs each (Panel C). Slits are made with a tiny spear or needle (Panel D). The needle is then removed, and follicular units are planted in these slits (Panel E). With appropriate placement and orientation of follicular units, it is possible to increase hair density from Ludwig stage II (Panel F) to Ludwig stage I (Panel G) in a patient with female-pattern hair loss.
What causes androgenic alopecia?
A variety of genetic and environmental factors likely play a role in causing androgenetic alopecia. Although researchers are studying risk factors that may contribute to this condition, most of these factors remain unknown. Researchers have determined that androgenic alopecia is related to hormones called androgens, particularly an androgen called dihydrotestosterone (DHT) 25, 26. Androgens are important for normal male sexual development before birth and during puberty. Androgens also have other important functions in both males and females, such as regulating hair growth and sex drive.
Hair growth begins under the skin in structures called follicles. Each strand of hair normally grows for 2 to 6 years, goes into a resting phase for several months, and then falls out. The cycle starts over when the follicle begins growing a new hair. Increased levels of androgens in hair follicles can lead to a shorter cycle of hair growth and the growth of shorter and thinner strands of hair. Additionally, there is a delay in the growth of new hair to replace strands that are shed.
Androgenic alopecia is a polygenic disorder with variable penetrance, and both maternal and paternal genes are involved. There is a familial predisposition to androgenetic alopecia with sons at a five to six time higher relative risk if their fathers were balding.
Androgenic alopecia also requires androgen to occur. It develops only after puberty. Males castrated before puberty and those with androgen insensitivity syndrome do not have pattern baldness. It is clear that both hormone metabolism and androgen receptor play a key role in pattern alopecia.
Although researchers suspect that several genes play a role in androgenetic alopecia, variations in only one gene, AR, have been confirmed in scientific studies. The AR gene provides instructions for making a protein called an androgen receptor. Androgen receptors allow the body to respond appropriately to dihydrotestosterone and other androgens. Studies suggest that variations in the AR gene lead to increased activity of androgen receptors in hair follicles. It remains unclear, however, how these genetic changes increase the risk of hair loss in men and women with androgenetic alopecia.
Researchers continue to investigate the connection between androgenetic alopecia and other medical conditions, such as coronary heart disease and prostate cancer in men and polycystic ovary syndrome (PCOS) in women. They believe that some of these disorders may be associated with elevated androgen levels, which may help explain why they tend to occur with androgen-related hair loss. Other hormonal, environmental, and genetic factors that have not been identified also may be involved.
There are two major isoforms of the 5 alpha-reductase enzyme. The 5 alpha-reductase converts testosterone to DHT (dihydrotestosterone), which has a much greater affinity for the androgen receptor. Type 2 5 alpha-reductase enzyme plays a greater role in androgenetic alopecia.
Type 1 5 alpha-reductase enzymes are in sebaceous glands, keratinocytes, and sweat glands. Type 2 5 alpha-reductase enzymes are in the outer root sheath of hair follicles, epididymis, vas deferens, seminal vesicles, and prostate.
The normal hair growth cycle consists of four phases: anagen (growth), catagen (involution), telogen (resting), and exogen (shedding of hair). Eighty percent to 90% of hair is in the anagen phase which lasts 2 to 6 years and determines the hair length; less than 5% are in catagen, and the rest are in telogen. Shedding of 100 hairs a day (exogen) is normal.
Activation of the androgen receptor shortens the anagen or growth phase in the normal hair growth cycle. In androgenetic alopecia, excessive activation leads to follicular miniaturization through a progressively shorter anagen phase, resulting in thinner and shorter hair follicles which in the end may not even penetrate through the epidermis. Pathological specimens will show a decreased 5:0 ratio of anagen to telogen hair where the norm is 12:1.
Androgenetic alopecia patients have higher production of dihydrotestosterone, and higher levels of 5 alpha-reductase and androgen receptors in balding scalp.
Androgenic alopecia inheritance pattern
The inheritance pattern of androgenetic alopecia is unclear because many genetic and environmental factors are likely to be involved. This condition tends to cluster in families, however, and having a close relative with patterned hair loss appears to be a risk factor for developing the condition.
Androgenic alopecia symptoms
In men, early androgenetic alopecia is defined as occurring before 30 years old and is seen as the male phenotypic equivalent to a polycystic ovarian syndrome.
In women, pattern baldness is often unmasked by telogen effluvium, which occurs 1 to 6 months after a stressor causes a larger portion of the hair to shift from the anagen phase to the telogen phase, leading to an increasing number of hair follicles in the exogen phase.
In both males and females, it is not known how far pattern baldness will progress.
In addition to male-pattern baldness, androgenetic alopecia in men has been associated with several other medical conditions including coronary heart disease and enlargement of the prostate. Additionally, prostate cancer, disorders of insulin resistance (such as diabetes and obesity), and high blood pressure (hypertension) have been related to androgenetic alopecia in men. In women, androgenetic alopecia is associated with an increased risk of polycystic ovary syndrome (PCOS), which is characterized by a hormonal imbalance that can lead to irregular menstruation, acne, excess body hair (hirsutism), and weight gain.
Androgenetic alopecia is gradual in onset and occurs after puberty. In men, it begins as bitemporal thinning of frontal scalp first then involves the vertex. In women, it is noted as thinning of hair between the frontal and the vertex of the scalp without affecting the frontal hairline and usually demonstrated as a wider part or a visible scalp.
Androgenic alopecia diagnosis
Androgenetic alopecia is usually diagnosed clinically with a history of gradual onset, occurring after puberty, and often but not necessarily, a family history of baldness. A biopsy is usually not necessary unless the diagnosis is unclear. Dermoscopy shows miniaturized hair and brown perihilar casts which can help differentiate from diffuse alopecia areata that mimics male pattern baldness as diffuse alopecia areata will have tapered fractures such as exclamation point hairs 27.
A thorough review of systems, past medical history, and the patient’s medication list is important to ensure other causes are not present for hair loss or other reasons for the unmasking of the androgenetic alopecia. Thyroid studies, CBC, screening for iron deficiency with iron, total iron binding capacity, and ferritin may be warranted. Screen for syphilis if suspected. A quick psychiatric screen for depressive symptoms and other psychiatric disorders may also be warranted in all hair loss patients visiting a dermatologist.
Androgenic alopecia treatment
There are two FDA approved drugs for androgenetic alopecia: topical minoxidil and finasteride, both of which require at least a 4- to 6-month trial before noticing improvement and must be used indefinitely to maintain a response. As such, medication adherence often can be poor. Furthermore, initiation of the drug may cause an initial shedding phase. They work better together 28.
Topical minoxidil is available over-the-counter and in various strengths, up to 5% solution. Higher strengths are more effective. Minoxidil does not alter the natural history of hair loss, but rather it can thicken / increase the density of remaining hair. Minoxidil comes as a solution or foam – the easiest way to measure the correct amount is to use a large tangerine-sized blob of the foam. The most common adverse effects are pruritus (itch) and local irritation with resulting flaking. The latter is usually due to propylene glycol or alcohol in the formulation of the drug. Minoxidil is a potassium channel blocker and widens blood vessels which hypothetically allow more oxygen, blood, and nutrients to follicles and promote the anagen phase. The response to treatment should be assessed at six months – if beneficial treatment needs to be continued to maintain efficacy. Up to 40% of patients may benefit.
Finasteride is a 5 alpha-reductase type 2 inhibitor and not an anti-androgen 29. Finasteride gives some benefit to approximately two-thirds of male patients. As opposed to Minoxidil, finasteride is used to try and slow the rate of hair loss. It is prescribed at 1 mg daily, although a single dose of 5 mg per week is probably as effective and much cheaper for the patient and is more effective at increasing hair regrowth at the vertex than the frontal area of the scalp. The efficacy of finasteride is unclear in female androgenetic alopecia and contraindicated for women with reproductive potential (Category X) as it can cause a male fetus to develop ambiguous genitalia. Adverse effects include sexual dysfunction, which usually reduces with time; increased risk of high-grade prostate cancer because PSA is masked and detected later; and case reports of persistent diminished libido and erectile dysfunction.
Other drugs used in androgenetic alopecia are not FDA-approved. Dutasteride is three times more potent on type II 5 alpha-reductase enzyme, 100 times more potent on type 1 enzyme, and often used on patients who failed finasteride. The adverse effect profile is similar to finasteride.
In women, oral antiandrogens such as spironolactone are often used. Spironolactone is a very weak partial agonist to the androgen receptor, blocking the much more potent DHT and free testosterone from interacting with the androgen receptor, thus physiologically behaving like a direct antagonist. It also inhibits androgen synthesis and enhances conversion of testosterone to estradiol. Cyproterone acetate may be used internationally but is not available in the United States. Anti-androgens are more effective if there are other signs of virilization.
Hair transplant is effective and cosmetically satisfactory to the patient. However, patients need to have a sufficient number of donor plugs (greater than 40 follicular units/cm2) to cover the bald area. New techniques have made hair transplant more cosmetically pleasing and natural looking.
Red light or laser at 660 nm also has demonstrated efficacy for hair loss and is available OTC for androgenetic alopecia.
Other proposed treatments include saw palmetto extract (Serenoa Repens); prostaglandin analogs like latanoprost and bimatoprost, which may be cost prohibitive; and multiple growth factors, which are a theoretical reason why platelet-rich plasma and adipose-derived stem cells may be used as adjunctive to treatments listed.
Wigs
- Can be considered for patients with moderate to severe androgenetic alopecia.
- Patients can be referred (normally to local dermatology departments) for the provision of wigs, which are of sufficient quality to normally make for a good cosmetic appearance.
Surgery
- Can be performed in both male and female patients, although the outcomes appear better for men
- Patients need to have sufficient donor hair – the best site is from the neck region of the scalp
- Outcomes are variable, and depend to a large extent on the skill / experience of the surgeon
- Treatments are very expensive and patients need to give considerable thought before having such a procedure performed
- Ho CH, Zito PM. Androgenetic Alopecia. [Updated 2019 May 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430924
- Sasaki GH. Review of Human Hair Follicle Biology: Dynamics of Niches and Stem Cell Regulation for Possible Therapeutic Hair Stimulation for Plastic Surgeons. Aesthetic Plast Surg. 2019 Feb;43(1):253-266.
- He H, Xie B, Xie L. Male pattern baldness and incidence of prostate cancer: A systematic review and meta-analysis. Medicine (Baltimore). 2018 Jul;97(28):e11379
- Hair Loss in Women. N Engl J Med 2007; 357:1620-1630. https://www.nejm.org/doi/full/10.1056/nejmcp072110
- Meephansan J, Thummakriengkrai J, Ponnikorn S, Yingmema W, Deenonpoe R, Suchonwanit P. Efficacy of topical tofacitinib in promoting hair growth in non-scarring alopecia: possible mechanism via VEGF induction. Arch Dermatol Res. 2017;309(9):729–738. doi:10.1007/s00403-017-1777-5
- Rojhirunsakool, S., & Suchonwanit, P. (2017). Parietal scalp is another affected area in female pattern hair loss: an analysis of hair density and hair diameter. Clinical, cosmetic and investigational dermatology, 11, 7–12. https://doi.org/10.2147/CCID.S153768
- Banka N, Bunagan MJ, Shapiro J. Pattern hair loss in men: diagnosis and medical treatment. Dermatol Clin. 2013;31(1):129–140.
- Jimenez-Cauhe J, Saceda-Corralo D, Rodrigues-Barata R, Hermosa-Gelbard A, Moreno-Arrones OM, Fernandez-Nieto D, Vaño-Galvan S. Effectiveness and safety of low-dose oral minoxidil in male androgenetic alopecia. J Am Acad Dermatol. 2019 May 2. pii: S0190-9622(19)30685-1. doi: 10.1016/j.jaad.2019.04.054. [Epub ahead of print]
- Price VH. Treatment of hair loss. N Engl J Med. 1999;341(13):964–973.
- Rittmaster RS. Finasteride. N Engl J Med. 1994;330(2):120–125.
- Olsen EA. Female pattern hair loss. J Am Acad Dermatol. 2001 Sep;45(3 Suppl):S70-80. doi: 10.1067/mjd.2001.117426
- Birch MP, Lalla SC, Messenger AG. Female pattern hair loss. Clin Exp Dermatol. 2002 Jul;27(5):383-88. doi: 10.1046/j.1365-2230.2002.01085.x
- Birch MP, Messenger JF, Messenger AG. Hair density, hair diameter and the prevalence of female pattern hair loss. Br J Dermatol. 2001 Feb;144(2):297-304. doi: 10.1046/j.1365-2133.2001.04018.x
- Ludwig E. Androgenetic alopecia. Arch Dermatol. 1977 Jan;113(1):109. doi: 10.1001/archderm.1977.01640010111023
- Kasick JM, Bergfeld WF, Steck WD, Gupta MK. Adrenal androgenic female-pattern alopecia: sex hormones and the balding woman. Cleve Clin Q. 1983 Summer;50(2):111-22. doi: 10.3949/ccjm.50.2.111
- Futterweit W, Dunaif A, Yeh HC, Kingsley P. The prevalence of hyperandrogenism in 109 consecutive female patients with diffuse alopecia. J Am Acad Dermatol. 1988 Nov;19(5 Pt 1):831-6. doi: 10.1016/s0190-9622(88)70241-8
- DeVillez RL, Jacobs JP, Szpunar CA, Warner ML. Androgenetic Alopecia in the Female: Treatment With 2% Topical Minoxidil Solution. Arch Dermatol. 1994;130(3):303–307. doi:10.1001/archderm.1994.01690030035005
- Lucky AW, Piacquadio DJ, Ditre CM, Dunlap F, Kantor I, Pandya AG, Savin RC, Tharp MD. A randomized, placebo-controlled trial of 5% and 2% topical minoxidil solutions in the treatment of female pattern hair loss. J Am Acad Dermatol. 2004 Apr;50(4):541-53. doi: 10.1016/j.jaad.2003.06.014
- Sinclair R, Wewerinke M, Jolley D. Treatment of female pattern hair loss with oral antiandrogens. Br J Dermatol. 2005 Mar;152(3):466-73. doi: 10.1111/j.1365-2133.2005.06218.x
- Vexiau P, Chaspoux C, Boudou P, Fiet J, Jouanique C, Hardy N, Reygagne P. Effects of minoxidil 2% vs. cyproterone acetate treatment on female androgenetic alopecia: a controlled, 12-month randomized trial. Br J Dermatol. 2002 Jun;146(6):992-9. doi: 10.1046/j.1365-2133.2002.04798.x
- Trüeb RM; Swiss Trichology Study Group. Finasteride treatment of patterned hair loss in normoandrogenic postmenopausal women. Dermatology. 2004;209(3):202-7. doi: 10.1159/000079890
- Iorizzo M, Vincenzi C, Voudouris S, Piraccini BM, Tosti A. Finasteride treatment of female pattern hair loss. Arch Dermatol. 2006 Mar;142(3):298-302. doi: 10.1001/archderm.142.3.298
- Unger WP, Unger RH. Hair transplanting: an important but often forgotten treatment for female pattern hair loss. J Am Acad Dermatol. 2003 Nov;49(5):853-60. doi: 10.1016/s0190-9622(03)01568-8
- Avram MR, Cole JP, Gandelman M, Haber R, Knudsen R, Leavitt MT, Leonard RT Jr, Puig CJ, Rose PT, Vogel JE, Ziering CL; Roundtable Consensus Meeting of The 9th Annual Meeting of The International Society of Hair Restoration Surgery. The potential role of minoxidil in the hair transplantation setting. Dermatol Surg. 2002 Oct;28(10):894-900; discussion 900. doi: 10.1046/j.1524-4725.2002.02068.x
- Chan L, Cook DK. Female pattern hair loss. Aust J Gen Pract. 2018 Jul;47(7):459-464.
- Tanaka Y, Aso T, Ono J, Hosoi R, Kaneko T. Androgenetic Alopecia Treatment in Asian Men. J Clin Aesthet Dermatol. 2018 Jul;11(7):32-35.
- Bienenfeld A, Azarchi S, Lo Sicco K, Marchbein S, Shapiro J, Nagler AR. Androgens in women: Androgen-mediated skin disease and patient evaluation. J. Am. Acad. Dermatol. 2019 Jun;80(6):1497-1506.
- Nast A, Gaskins M, Eisert L, Werner RN, Borradori L, Marinovic B, Paul C, Dressler C. Prioritizing topics in guideline development: results of a two-phase online survey of dermatologist members of the EADV. J Eur Acad Dermatol Venereol. 2019 Jan;33(1):227-233.
- Zito PM, Syed K. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Dec 19, 2018. Finasteride.