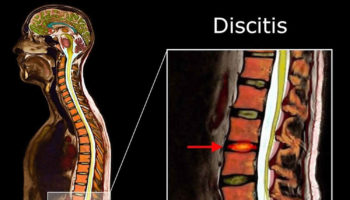
What is discitis Discitis is an inflammation or infection of the intervertebral disc or intervertebral disc space. Discitis can be caused by bacteria, virus, or fungus. Discitis
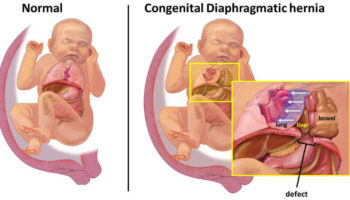
What is a diaphragmatic hernia A diaphragmatic hernia is also called congenital diaphragmatic hernia, is a birth defect in which there is an abnormal opening
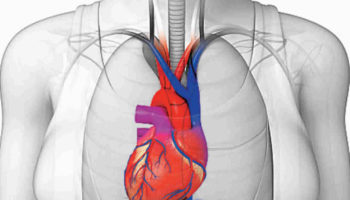
What is dextrocardia Dextrocardia is a rare condition in which the heart is located in the right side of the chest instead of the left.
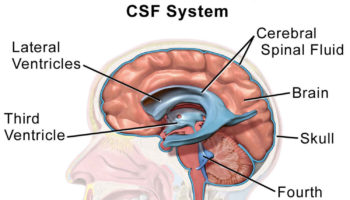
What is a CSF leak A CSF leak is an escape of the cerebrospinal fluid (CSF) that surrounds your brain and spinal cord. CSF leaks have
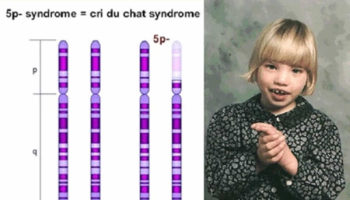
What is Cri du chat syndrome Cri du chat syndrome is a genetic disorder that result from missing a piece of chromosome number 5, also
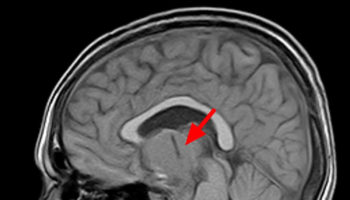
What is craniopharyngioma Craniopharyngiomas are rare benign (noncancerous) tumors that are typically found near the pituitary gland and hypothalamus, which are positioned beneath the center
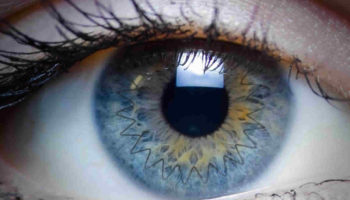
Corneal transplant surgery A corneal transplant also known as keratoplasty, is a surgical procedure that replaces a disc-shaped segment of an unhealthy cornea with a similarly
What is cryosurgery Cryosurgery is also called cryotherapy, is a medical procedure that uses intense cold produced by liquid nitrogen (or argon gas) to destroy
What is cerebral hypoxia Cerebral hypoxia or brain hypoxia refers to a condition in which there is a decrease of oxygen supply to the brain even
What is calcification Calcification is a process in which calcium builds up in body tissue, causing the tissue to harden. Calcification can be a normal