Bare lymphocyte syndrome
Bare lymphocyte syndrome is an inherited disorder of the immune system also called primary immunodeficiency disorder. Your body’s immune system is responsible for fighting infections and anything it sees as foreign invaders to the body. In bare lymphocyte syndrome, the body has a shortage of immune proteins called major histocompatibility complex (MHC) class 1 (Bare lymphocyte syndrome type 1) and 2 (Bare lymphocyte syndrome type 2) proteins. MHC proteins attack bacteria or viruses that enter the body. Children inherit the BLS gene from their parents. Both parents must carry the genetic mutation for bare lymphocyte syndrome, but may not have symptoms of the disease.
Bare lymphocyte syndrome is a rare disease. Since bare lymphocyte syndrome symptoms are much the same as symptoms of other childhood illnesses, doctors don’t know how many people have the disease.
Bare lymphocyte syndrome symptoms
Depending on how severe the disease is, children may have symptoms before one year of age or not until later in childhood.
Bare lymphocyte syndrome symptoms may be longer-lasting and more severe than those of other childhood diseases.
Some symptoms of bare lymphocyte syndrome are:
- Respiratory infections that keep coming back, including sinus and lung infections.
- Skin infections that don’t respond well to treatment.
- Chronic diarrhea.
Bare lymphocyte syndrome complications
Children with primary immune deficiencies like bare lymphocyte syndrome are:
- More prone than others to getting infections.
- Slower to clear infections from their bodies.
- At risk for recurrent, severe lung infections that can cause permanent damage to other organs such as the lungs and liver. This, in turn, causes severe health problems into adulthood.
Bare lymphocyte syndrome diagnosis
Doctors diagnose bare lymphocyte syndrome through blood tests. Testing for certain immune markers in the blood lets doctors see how well the immune system is functioning.
Your child may also need a chest x-ray to see whether bare lymphocyte syndrome has caused damage to the lungs.
Bare lymphocyte syndrome treatment
The goals of bare lymphocyte syndrome treatment are to:
- Control the symptoms of this disease.
- Avoid infections.
- Improve your child’s quality of life.
Children with bare lymphocyte syndrome may need aggressive treatment for any infections they have. If your child doesn’t have any infections, your doctor might prescribe antibiotics to prevent them.
Your child needs to avoid live vaccines and may need intravenous immunoglobulin (IVIg) therapy.
If bare lymphocyte syndrome is causing severe health problems such as lung failure, your child may benefit from a:
- Bone marrow transplant
- Cord blood transplant
- Or even a lung transplant
Bare lymphocyte syndrome type 1
Bare lymphocyte syndrome type 1 also called HLA class 1 deficiency, is an inherited disorder of the immune system (primary immunodeficiency). Immunodeficiencies are conditions in which the immune system is not able to protect the body effectively from foreign invaders such as bacteria or viruses. Starting in childhood, most people with bare lymphocyte syndrome type 1 develop recurrent bacterial infections in the lungs and airways (respiratory tract). These recurrent infections can lead to a condition called bronchiectasis, which damages the passages leading from the windpipe to the lungs (bronchi) and can cause breathing problems.
Many people with bare lymphocyte syndrome type 1 also have open sores (ulcers) on their skin, usually on the face, arms, and legs. These ulcers typically develop in adolescence or young adulthood. Some people with bare lymphocyte syndrome type 1 have no symptoms of the condition.
People with bare lymphocyte syndrome type 1 have a shortage of specialized immune proteins called major histocompatibility complex (MHC) class 1 proteins on cells, including infection-fighting white blood cells (lymphocytes), which is where the condition got its name.
Bare lymphocyte syndrome type 1 is a rare disorder with an unknown prevalence. About 30 affected individuals have been described in the medical literature 1. Bare lymphocyte syndrome type 1 is likely underdiagnosed, because doctors may not investigate the underlying cause of respiratory tract infections.
Bare lymphocyte syndrome type 1 causes
Bare lymphocyte syndrome type 1 is usually caused by mutations in the TAP1 or TAP2 gene. Each of these genes provides instructions for making a protein that plays a role in helping the immune system recognize and fight infections. In particular, the TAP1 and TAP2 proteins aid the function of MHC class 1 proteins.
The TAP1 and TAP2 proteins attach (bind) together to form a protein complex called transporter associated with antigen processing (TAP) complex. This complex, which is found in the membrane of a cell structure called the endoplasmic reticulum, moves (transports) protein fragments (peptides) from foreign invaders into the endoplasmic reticulum. There, the peptides are attached to MHC class 1 proteins. The peptide-bound MHC class 1 proteins are then moved to the surface of the cell so that specialized immune system cells can interact with them. When these immune system cells recognize the peptides as harmful, they launch an immune response to get rid of the foreign invaders.
Mutations in the TAP1 or TAP2 gene prevent formation of the TAP complex, which impairs the transport of peptides into the endoplasmic reticulum. Because there are no peptides for MHC class 1 proteins to bind, they are broken down, which results in a shortage of MHC class 1 proteins on the surface of cells. A lack of these proteins impairs the body’s immune response to bacteria, leading to recurrent bacterial infections. Researchers are unsure why people with bare lymphocyte syndrome I do not also get viral infections, but they suspect that other immune processes are able to recognize and fight viruses. It is also not clear how TAP1 and TAP2 gene mutations are involved in the development of skin ulcers.
Mutations in another gene involved in the attachment of peptides to MHC class I proteins very rarely cause bare lymphocyte syndrome type 1.
Bare lymphocyte syndrome type 1 inheritance pattern
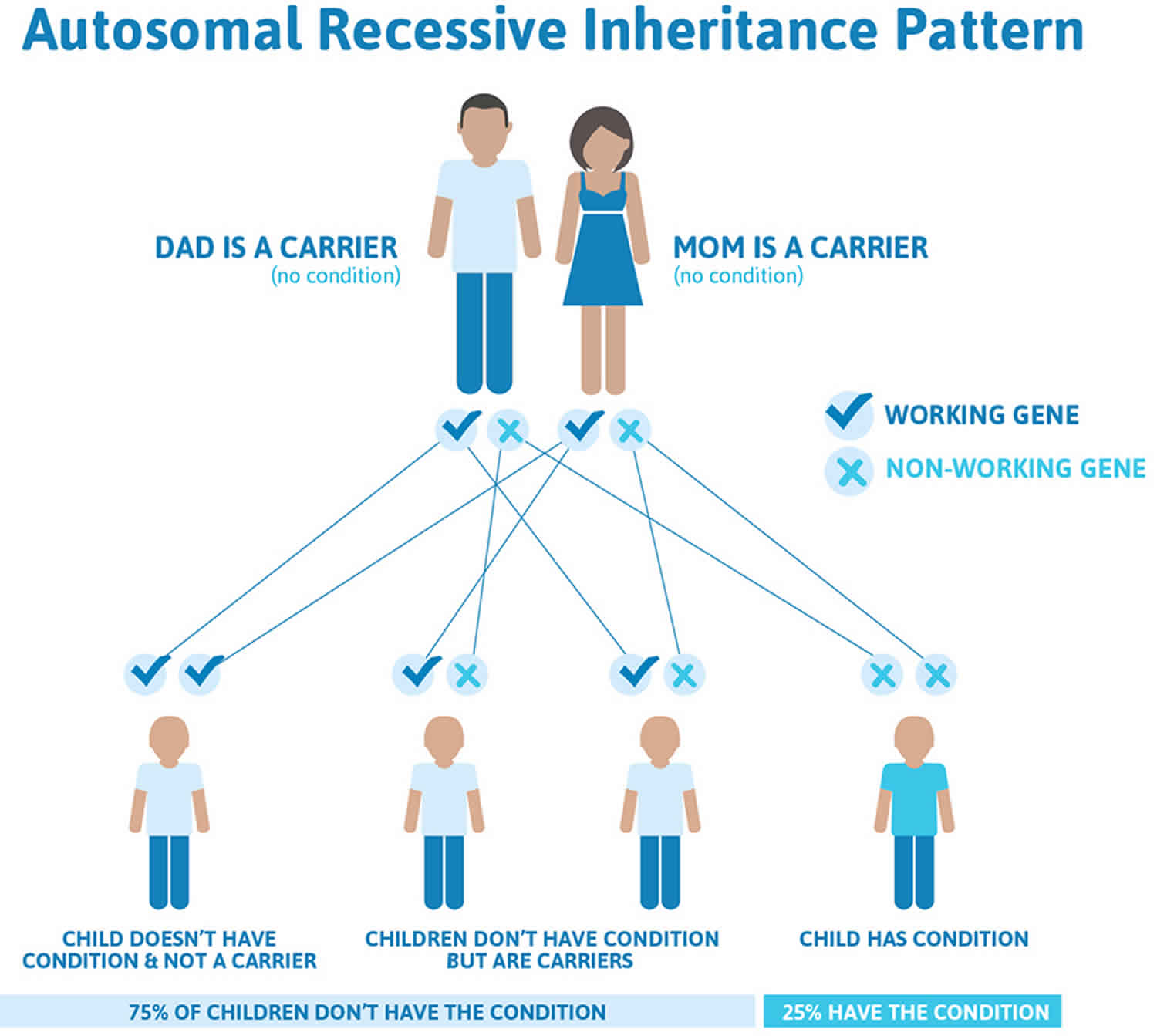
Bare lymphocyte syndrome type 1 is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
Figure 1 illustrates autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 1. Bare lymphocyte syndrome type 1 autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Bare lymphocyte syndrome type 1 symptoms
Bare lymphocyte syndrome type 1 symptoms include:
- chronic otitis media
- ectopia lentis
- Respiratory airways:
- bronchitis
- bronchiolitis
- bronchial obstruction
- unilateral bronchiectasis
- bilateral bronchiectasis
- bacterial infections of the respiratory tract
- chronic sinusitis
- pansinusitis
- emphysema
- nasal polyposis
- Skin, nails and hair:
- pigmentary abnormalities
- localized cutaneous necrobiosis lipoidica
- deep skin ulcers
Bare lymphocyte syndrome type 2
Bare lymphocyte syndrome type 2 also called MHC class 2 deficiency, is an inherited disorder of the immune system categorized as a form of severe combined immunodeficiency (SCID). People with bare lymphocyte syndrome type 2 lack virtually all immune protection from bacteria, viruses, and fungi. They are prone to repeated and persistent infections that can be very serious or life-threatening. These infections are often caused by “opportunistic” organisms that ordinarily do not cause illness in people with a normal immune system. Because bare lymphocyte syndrome type 2 is the most common and best studied form of a group of related conditions, it is often referred to as simply bare lymphocyte syndrome (BLS).
In people with bare lymphocyte syndrome type 2, infection-fighting white blood cells (lymphocytes) are missing specialized proteins on their surface called major histocompatibility complex (MHC) class 2 proteins, which is where the condition got its name. The deficiency of MHC class 2 molecules affects the cellular and humoral immune response by impairing the development of CD4+ T helper (Th) cells and T helper (Th) cell-dependent antibody production by B cells.
Bare lymphocyte syndrome type 2 is typically diagnosed in the first year of life. Most affected infants have persistent respiratory, gastrointestinal, and urinary tracts infections. Because of the infections, affected infants have difficulty absorbing nutrients (malabsorption), and they grow more slowly than their peers. Eventually, the persistent infections lead to organ failure. Without treatment, individuals with bare lymphocyte syndrome type 2 usually do not survive past early childhood. Hematopoietic stem cell transplantation (HSCT) is the only curative therapy available for treating these patients 2.
Bare lymphocyte syndrome type 2 is a rare condition. At least 100 cases have been reported in the medical literature 3. While bare lymphocyte syndrome type 2 has been found in several populations throughout the world, it appears to be especially prevalent in the Mediterranean region and North Africa.
Bare lymphocyte syndrome type 2 causes
Bare lymphocyte syndrome type 2 is caused by mutations in the CIITA, RFX5, RFXANK, or RFXAP gene. Each of these genes provides instructions for making a protein that plays a role in controlling the activity (transcription) of genes called MHC class 2 genes. Transcription is the first step in the production of proteins, and the CIITA, RFX5, RFXANK, and RFXAP proteins are critical for the production of MHC class II proteins from these genes.
The RFX5, RFXANK, and RFXAP proteins come together to form the regulatory factor X (RFX) complex, which attaches (binds) to specific regions of DNA involved in the regulation of MHC class 2 gene activity. The CIITA protein interacts with the RFX complex and brings together other proteins that turn on gene transcription, leading to the production of MHC class 2 proteins.
MHC class 2 proteins play an important role in the body’s immune response to foreign invaders, such as bacteria, viruses, and fungi. To help the body recognize and fight infections, MHC class 2 proteins on lymphocytes bind to fragments of proteins (peptides) from foreign invaders so that other specialized immune system cells can interact with them. When these immune system cells recognize the peptides as harmful, they trigger the lymphocytes to launch immune responses to get rid of the foreign invaders.
Mutations in the CIITA, RFX5, RFXANK, or RFXAP gene prevent transcription of MHC class 2 genes, which leads to an absence of MHC class 2 proteins on the surface of certain lymphocytes. Lack of these proteins on lymphocytes impairs the body’s immune response to bacteria, viruses, and fungi, leading to persistent infections in individuals with Bare lymphocyte syndrome type 2 syndrome.
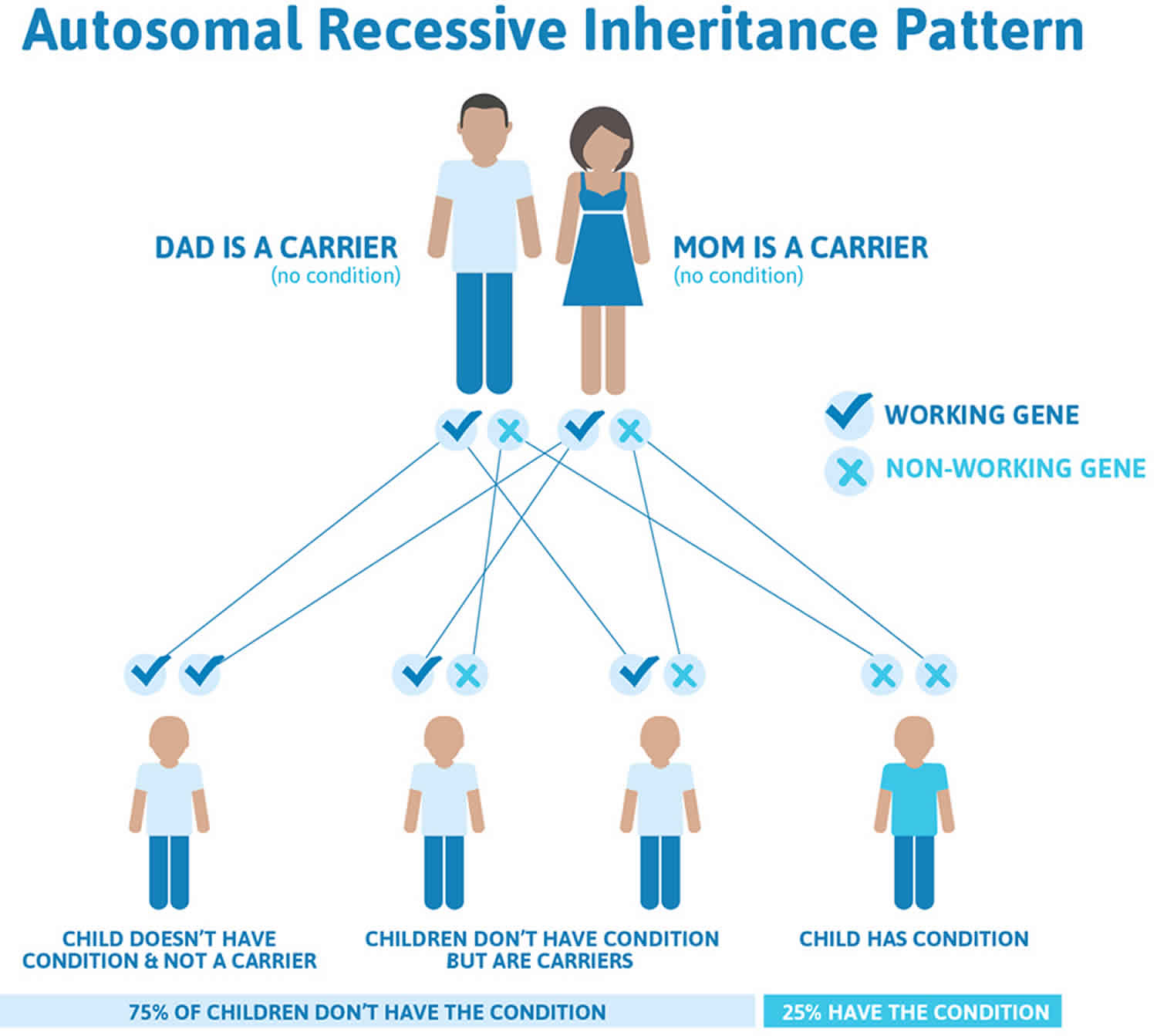
Bare lymphocyte syndrome type 2 inheritance pattern
Bare lymphocyte syndrome type 2 is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
Figures 1 and 2 illustrate autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 2. Bare lymphocyte syndrome type 2 autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Bare lymphocyte syndrome type 2 symptoms
The clinical hallmarks of severe combined immunodeficiency (SCID) are repetitive and frequent bacterial, viral, and fungal infections that persist despite standard medical treatment.
Bare lymphocyte syndrome type 2 symptoms include 4:
- 100% of people have these symptoms: reduced MHC 2 surface expression
- 80%-99% of people have these symptoms:
- Lack of T cell function
- Recurrent gastrointestinal infections
- Recurrent respiratory infections
- 30%-79% of people have these symptoms:
- Chronic hepatitis due to cryptosporidium infection
- Chronic mucocutaneous candidiasis
- Decreased circulating beta-2-microglobulin level
- Decreased proportion of CD4-positive helper T cells
- Failure to thrive
- Protracted diarrhea
- Recurrent candida infections
- Recurrent herpes
- Recurrent protozoan infections
- Recurrent Staphylococcus aureus infections
- Rhinitis
- Sclerosing cholangitis
- Sinus inflammation
- 5%-29% of people have these symptoms:
- Abnormal CD4:CD8 ratio
- Acute otitis media
- Autoimmune hemolytic anemia
- Autoimmune thrombocytopenia
- Decreased lymphocyte proliferation in response to mitogen
- Neutropenia in presence of anti-neutropil antibodies
- Pancytopenia
- Panhypogammaglobulinemia
- Skin rash
- 1%-4% of people have these symptoms:
- Abnormal facial shape
- Difficulty articulating speech (dysarthria)
- Inability to coordinate movements when walking (gait ataxia)
Other symptoms:
- Agammaglobulinemia
- Cholangitis (bile duct inflammation)
- Chronic lymphocytic meningitis
- Colitis
- Cutaneous anergy
- Encephalitis (brain inflammation)
- Intestinal malabsorption
- Neutropenia (low blood neutrophil count)
- Recurrent bacterial infections
- Recurrent fungal infections
- Recurrent lower respiratory tract infections (recurrent chest infections)
- Recurrent upper respiratory tract infections (recurrent colds)
- Recurrent urinary tract infections
- Recurrent viral infections
- Villous atrophy
- Viral hepatitis
- Bare lymphocyte syndrome type 1. https://ghr.nlm.nih.gov/condition/bare-lymphocyte-syndrome-type-i
- Aluri J, Gupta M, Dalvi A, et al. Clinical, Immunological, and Molecular Findings in Five Patients with Major Histocompatibility Complex Class II Deficiency from India. Front Immunol. 2018;9:188. Published 2018 Feb 16. doi:10.3389/fimmu.2018.00188 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5829618
- Bare lymphocyte syndrome type 2. https://ghr.nlm.nih.gov/condition/bare-lymphocyte-syndrome-type-ii
- Bare lymphocyte syndrome 2. https://rarediseases.info.nih.gov/diseases/824/bare-lymphocyte-syndrome-2