What is bleeding time
Bleeding time is a clinical laboratory test to assess platelet function and your body’s ability to form a blood clot. Bleeding time lab test involves making a standardized incision in a superficial area of the skin and monitoring the time needed for bleeding to stop (ie, bleeding site turns “glassy”) 1. Bleeding normally stops within 1-9 minutes but may be longer in children (1-13 minutes) and tends to take slightly longer in females than in males.
A bleeding time evaluation is most helpful in a patient with clinical bleeding whose platelet count and results of coagulation studies (PT/INR, aPTT) are normal. In this setting, the bleeding time will help recognize dysfunctional platelets.
At the current time, bleeding time has been largely discredited and, in part, replaced by other testing. The historical indications for bleeding time lab test were the pre-operative assessment of patients taking aspirin or NSAIDs and screening for von-Willebrand disease. Unfortunately, it is insensitive and lacks reproducibility 2. Platelet function assay (i.e PFA 100) has largely replaced bleeding time. Despite standardization of methods, the sensitivity and specificity of the bleeding time for platelet-mediated coagulopathy is low.
Many hospitals and health systems have removed the test without any demonstrated harm. In most cases, a thorough history and physical is the only workup needed for the pre-operative assessment of bleeding risk. When the clinical effectiveness of platelet aggregation is desired, a modern platelet function assay can provide the necessary information. This is being increasingly utilized in intracranial hemorrhage on various antiplatelet agents prior to pooled platelet transfusion.
Hemostasis is a sequence of events that leads to bleeding cessation via the formation of a fibrin-platelet hemostatic plug. It involves the triad of an injured vascular wall, platelets, and coagulation cascade. Once platelets are exposed to endothelial cells and collagen in the injured vascular wall, von Willebrand factor (vWF) is released, and platelets become activated and adhere to collagen through von Willebrand factor. Injured cells release tissue factor, which activates factor VII (extrinsic pathway), and the exposure of thrombogenic subendothelial collagen activates factor XII (intrinsic pathway).
Platelets play a major role in hemostasis, starting with adherence to the injured wall through von Willebrand factor, which adheres to subendothelial collagen. Platelets then adhere to von Willebrand factor via glycoprotein Ib. After adherence occurs, platelet activation takes place, whereby they change in shape with degranulation and thromboxane A2 synthesis. Soon thereafter, platelet aggregation occurs, whereby additional platelets are recruited from the bloodstream and aggregate via adenosine diphosphate and thromboxane A2 and bind to each other by binding to fibrinogen using GP IIb-IIIa, thus forming a fibrin-platelet plug.
The bleeding time reflects this process, and, if the platelets do not function properly in any of these steps, the bleeding time will prolong.
Bleeding time lab test
Bleeding time lab test is performed via two primary methods based on the length and location of the incision.
Ivy method
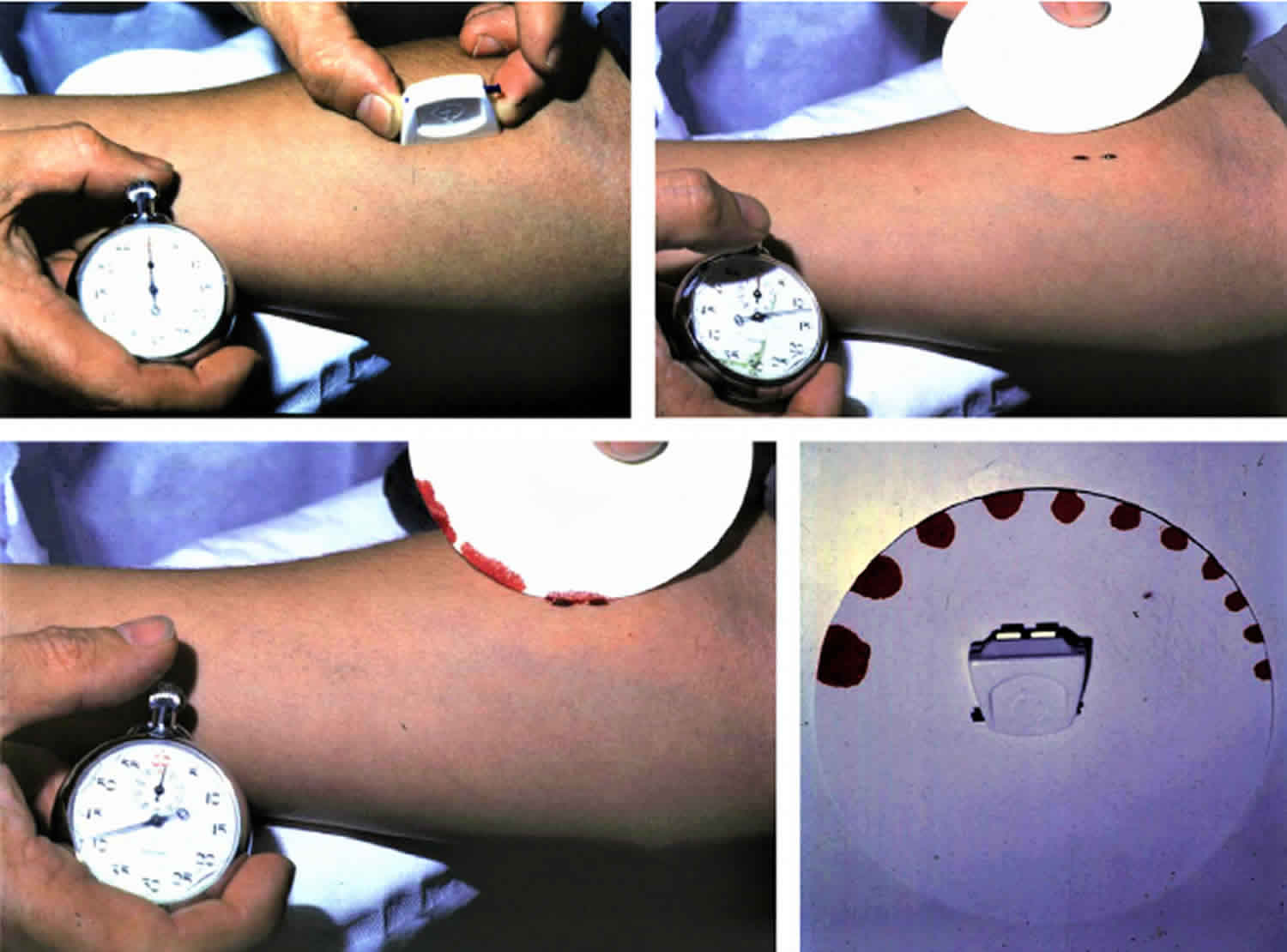
The IVY method is the most commonly used method.
A blood pressure cuff is applied to the arm and inflated to 40 mm Hg. The patient’s forearm is then cleaned with alcohol, and an incision is made with a sterile blade or scalpel, 1 mm deep and 10 mm long. Since the test is directed to capillary vessels, the area should have no large vessels.
Immediately, a stopwatch starts recording time. Then, every 30 seconds, a filter paper is applied gently over the wound. Whenever the paper absorbs blood, it means that the bleeding is active and has not stopped. This is repeated every 30 seconds until the bleeding stops completely (ie, no more blood is being absorbed by the filter). After the bleeding stops, the blood pressure cuff should be deflated. The bleeding time is defined as the time from the incision until all bleeding has stopped.
Although the Ivy method is more invasive, it is preferable, since its results are more reproducible but has an increased scarring risk.
Duke method
The Duke method is similar to the Ivy method; however, no blood pressure cuff is needed. In addition, it is less invasive, since it involves making a puncture wound that is 3 mm deep after the area is cleaned with alcohol. Areas with no large vessels are preferred, such as earlobe. Then, with a filter paper, the wound is swabbed every 30 seconds until no more blood is absorbed.
The Duke method is less accurate and carries a higher hematoma rate.
Either method carries the risks of infection and bleeding. In addition, the discomfort is not insignificant. Different normal ranges exist for each method further confounding the interpretation of results by lay clinicians.
Bleeding time normal value
General interpretations of bleeding time are as follows 3:
- 1-9 minutes: Normal
- Normal bleeding time:
- Duke method – Less than 3 minutes
- IVY method – Less than 8 minutes
- Prolonged bleeding times greater than 5 minutes in the Duke method and 10 minutes in the IVY method are concerning for coagulopathy. Abnormalities would require further evaluation with a focus on the coagulation pathway of interest.
- Normal bleeding time:
- 9-15 minutes: Platelet dysfunction
- More than 15 minutes: Critical; test must be discontinued and pressure should be applied
A bleeding time evaluation is used to measure the primary phase of hemostasis, which involves platelet adherence to injured capillaries and then platelet activation and aggregation. The bleeding time can be abnormal when the platelet count is low or the platelets are dysfunctional. Causes of abnormal bleeding time can be hereditary or acquired.
Hereditary causes of abnormal bleeding time are as follows:
- von Willebrand disease. Von Willebrand disease is an inherited deficiency in the quantity or function of the platelet aggregation protein Von Willebrand factor. Rather than bleeding time, modern workup includes complete blood count, factor VIII levels, ristocetin cofactor activity, and GP-Ib binding assay 4
- Glanzmann thrombasthenia (GP IIb/IIIa deficiency). Glanzmann’s thrombasthenia is an autosomal recessive inherited defect in the fibrinogen binding receptor glycoprotein IIb/IIIa.
- Bernard-Soulier syndrome (deficient GP1bIX-X). Bernard-Soulier Syndrome is a rare autosomal recessive genetic defect in glycoprotein Ib causing giant platelets with perceived thrombocytopenia. Platelet transfusion is the treatment of choice.
- Connective-tissue diseases (Ehlers-Danlos syndrome, Wiskott-Aldrich syndrome, Chédiak-Higashi syndrome, hereditary hemorrhagic telangiectasia [HHT])
Acquired causes of abnormal bleeding time are as follows:
- Thrombocytopenia. Decreased platelet count impairs primary hemostasis. Sepsis, drug reactions, hematologic malignancies, autoimmune conditions, and vitamin deficiencies are among the non-inherited causes. Spontaneous bleeding is not generally a problem seen until counts fall beneath 30,000.
- Medications (aspirin, nonsteroidal anti-inflammatory drugs [NSAIDs], antibiotics [penicillin, cephalosporins], anticoagulants [eg, heparin, streptokinase], tricyclic antidepressants, antipsychotics, theophylline)
- Vitamin C deficiency
- Alcohol intoxication
- Uremia
- Liver failure
- Leukemias
- Myelodysplastic syndrome
- Amyloidosis
- Disseminated Intravascular Coagulation (DIC). DIC is a symptom of other severe disease processes like sepsis, burns, trauma, pregnancy, and malignancy. The coagulopathy is consumptive from the formation of blood clots throughout the peripheral vasculature. Thrombocytopenia with low fibrinogen and a high INR are the classic laboratory abnormalities.
- Russeau AP, Manna B. Bleeding Time. [Updated 2019 Jan 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537233
- Kruse-Jarres R, Singleton TC, Leissinger CA. Identification and basic management of bleeding disorders in adults. J Am Board Fam Med. 2014 Jul-Aug;27(4):549-64.
- Bleeding Time. https://emedicine.medscape.com/article/2085022-overview
- Diagnosis, Evaluation and Management of von Willebrand Disease. NIH Publication #08-5832. National Heart, Lung and Blood Institute, 2007