Calcific tendinitis of shoulder
Calcific tendinosis is a painful but self-limiting condition of the shoulder that is characterized by either single or multiple calcium hydroxyapatite deposits within the rotator cuff tendon or subacromial bursa 1. Rotator cuff calcific tendinosis is a common presentation of the hydroxyapatite crystal deposition disease. Typically calcific tendinosis affects middle-aged patients between the ages of 30 and 60, with a slight predilection for women (housewives and clerical workers account for most cases) 2. Radiologically evident calcification has been reported in 7.5 to 20 percent of adults with no symptoms 2 and in 6.8 percent of those with shoulder pain 2. The rotator cuff is a group of 4 muscles that holds the head of the large bone in the arm (humerus) into the socket of the scapula (called the glenoid). The shoulder joint is a ball and socket type joint where the top part of the arm bone (humerus) forms a joint with the shoulder blade (scapula).
Calcific tendinosis subsides spontaneously in the majority of cases and can be managed with conservative therapy, but some patients continue to have a painful shoulder for an extended period of time with the deposits not showing any signs of resolution. The cause of calcific tendinosis is not known, but it is generally agreed that it is not caused by trauma, and it is only rarely associated with systemic disease.
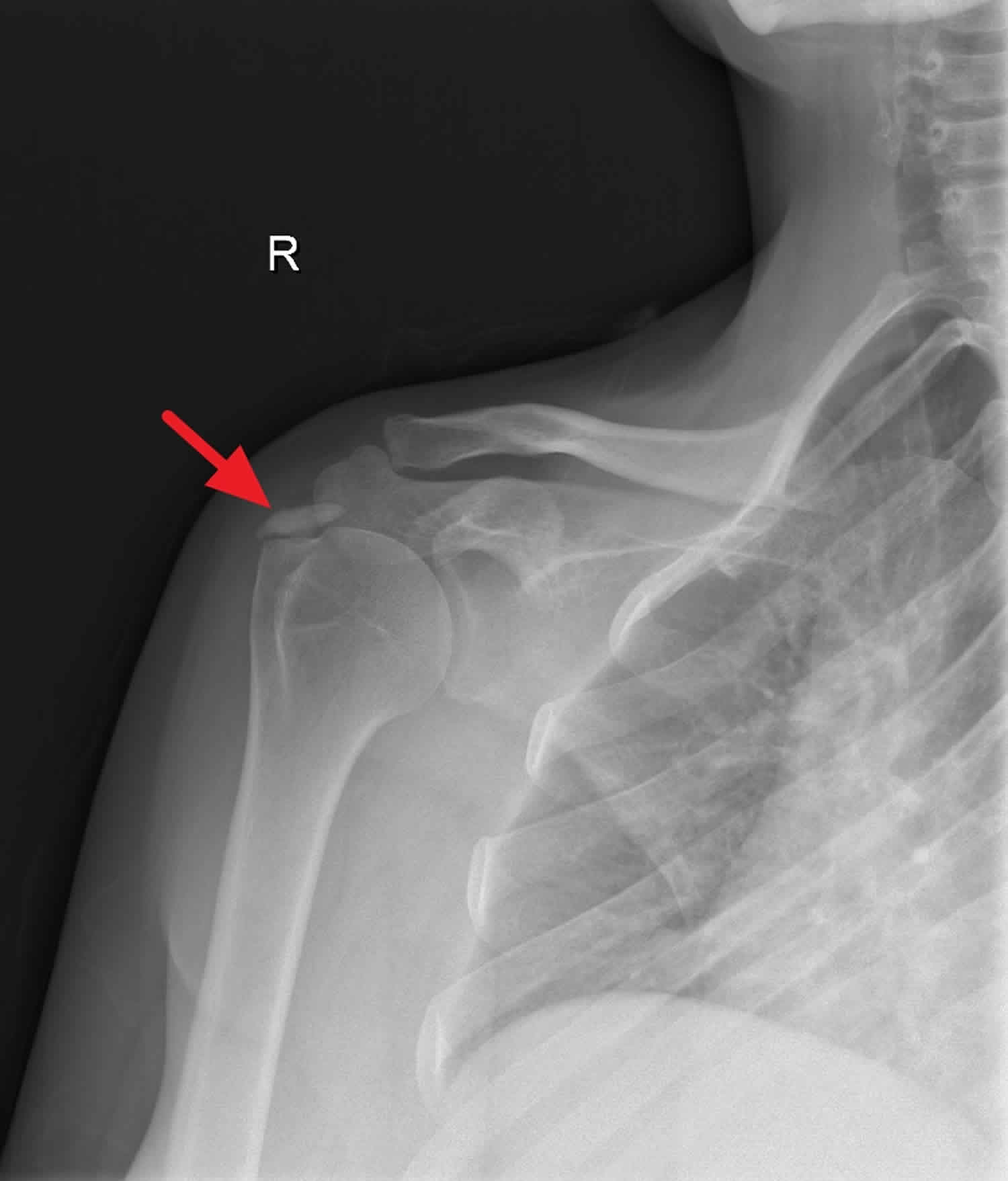
The diagnosis of calcific tendinosis is made from standard radiographs because they allow localization and assessment of the texture and morphology of the deposits. Deposits are most commonly located in the supraspinatus and infraspinatus. Less commonly, deposits are located in the teres minor and the subscapularis (3%) 3.
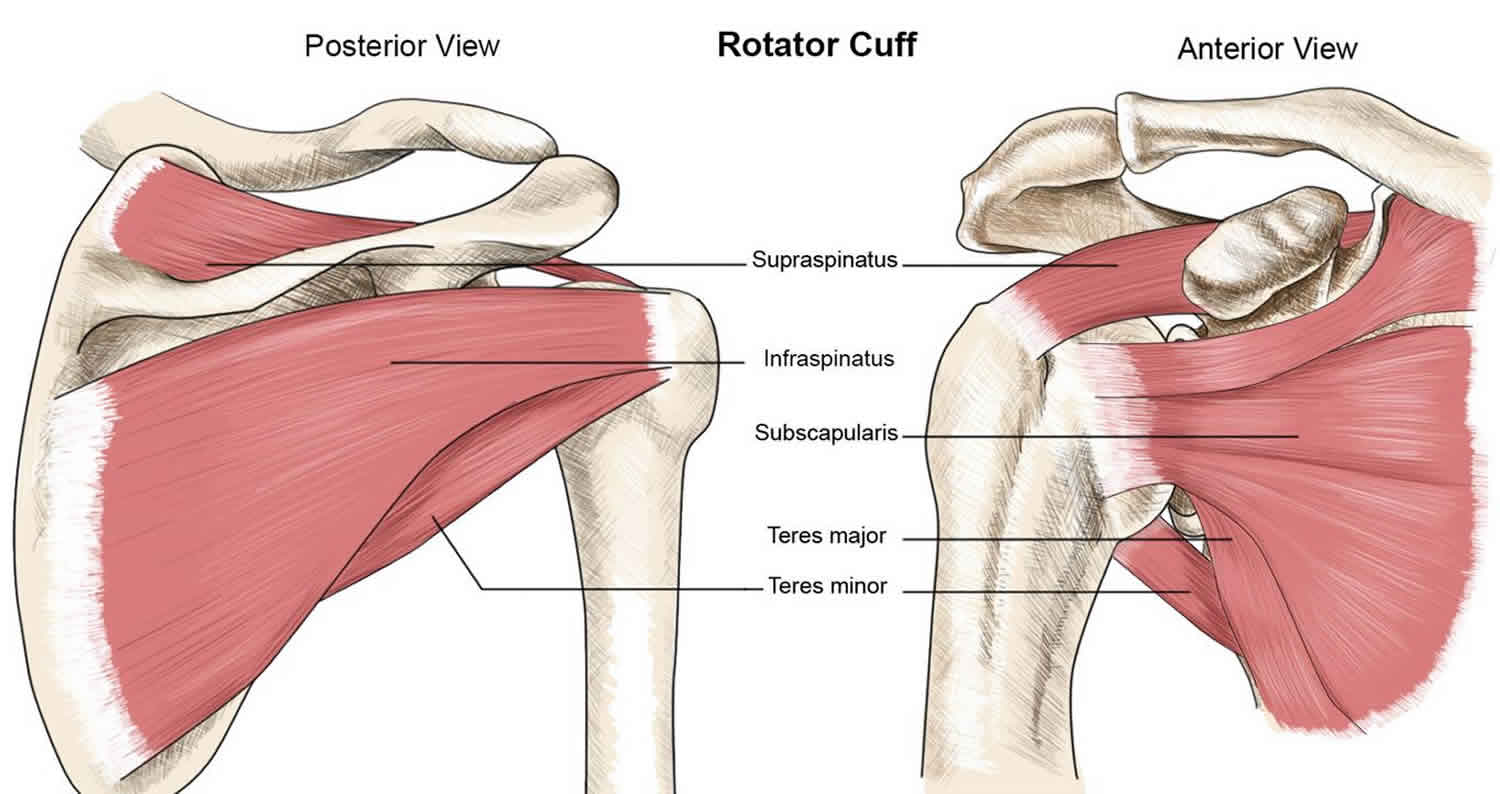
What is the rotator cuff
The rotator cuff is a group of four muscles that come together as tendons to form a “cuff” over the head of the humerus (upper arm bone). The rotator cuff is a group of muscles and their tendons that hold the shoulder joint in place by attaching the shoulder blade to the humerus (upper arm bone) and covering the head of the humerus. The rotator cuff stabilises the shoulder joint and helps move the shoulder. The 4 muscles (and their tendons) that make up the rotator cuff are:
- the supraspinatus;
- the infraspinatus;
- the subscapularis; and
- the teres minor.
The four muscles—supraspinatus, infraspinatus, subscapularis and teres minor—originate from the scapula (shoulder blade). The long head of the biceps tendon is also often included in rotator cuff pathology. The rotator cuff tendons attach to the head of the humerus in special spots referred to as the greater and lesser tuberosities.
The rotator cuff tendons cover the head of the humerus (upper arm bone), helping keep the head of the humerus in your shoulder joint and helping you to raise and rotate your arm.
There is a lubricating sac called a bursa between the rotator cuff and the bone on top of your shoulder (acromion). The bursa allows the rotator cuff tendons to glide freely when you move your arm. When the rotator cuff tendons are injured or damaged, this bursa can also become inflamed and painful.
Some of the actions of the rotator cuff are to rotate the upper arm towards the body (internal rotation) and away from the body (external rotation), and to help raise the arm (abduction).
The supraspinatus assists in elevation (abduction) of the arm; infraspinatus and teres minor in external rotation, and; subscapularis in internal rotation.
Figure 1. Shoulder joint rotator cuff muscles
Figure 2. Rotator cuff anatomy
Figure 3. Shoulder joint (lateral view)
Footnote: Oval calcific deposits superior to humeral head consistent with calcific tendinosis.
Calcific tendinosis causes
The cause of calcific tendinosis is not known, but it is generally agreed that it is not caused by trauma, and it is only rarely associated with systemic disease.
The early hypothesis was that the calcification is a consequence of age-related tendon degeneration; however, the peak incidence of calcifying tendinitis occurs at an earlier age than that of degeneration. Calcifying tendinitis, in contrast to degenerative tendinopathy, may resolve, and the tendon heals spontaneously. Calcifying tendinitis is rarely associated with tears of the rotator cuff.
The chemical composition of the calcium salts in degenerate tendons is different. The calcific deposit of calcifying tendinitis consists of poorly crystallized hydroxyapatite. Calcifying tendinitis appears to occur in viable, not necrotic, tissue, whereas dystrophic calcification appears to occur in necrotic tissue.
Uhthoff and Loehr 4 proposed that calcifying tendinitis is a disease that progresses through correlating pathologic and clinical stages, as follows:
- Formative phase: As a consequence of an unknown trigger, a portion of the tendon undergoes fibrocartilaginous transformation, and calcification occurs in the transformed tissue. The deposit enlarges; the calcific deposit resembles chalk.
- Resting phase: Once formed, the calcific deposit enters a resting period. The calcific deposit may or may not be painful. If large enough, the deposit may cause mechanical symptoms.
- Resorptive phase: After a variable period, an inflammatory reaction may ensue. Vascular tissue develops at the periphery of the deposit. Macrophages and multinuclear giant cells absorb the deposit during this phase. The calcific deposit resembles toothpaste and occasionally leaks into the subacromial bursa, which may result in very painful symptoms.
Postcalcific phase: Once the calcific deposit has been resorbed, fibroblasts reconstitute the collagen pattern of the tendon.
The correlation between increased incidence of thyroid disorders or diabetes and risk of developing cacifying tendonitis remains unclear; similarly, the associations with genetic mutations needs further study. It has been speculated that patients with theses predisposing factors may be at greater risk of developing cacifying tendonitis 3.
Calcific tendinosis symptoms
Rotator cuff calcific tendinitis is a morphologic condition. Calcific tendinosis may be discovered serendipitously by an imaging study and cause no symptoms. If and when rotator cuff calcific tendinitis is symptomatic, calcifying tendinitis may present in the following 3 ways:
- Chronic, relatively mild pain with intermittent flares, similar to shoulder impingement syndrome, is believed to indicate that the condition is in the formative phase.
- Mechanical symptoms may arise from a large calcific deposit, which may block elevation of the shoulder.
- More severe acute pain is attributed to the inflammatory response of the resorptive phase.
Pain is the most common symptom of a rotator cuff calcific tendinitis. It is typically located at the front of the shoulder, or the top of the shoulder. It is made worse by activities that require overhead work (such as brushing hair or putting items on a high shelf). The pain usually comes on gradually over a period of days to weeks. The pain may occur at night and wake people from sleep.
Other symptoms include:
- Weakness with certain shoulder movements
- Reduced range of motion at the shoulder
- Shoulder stiffness
- Catching at the shoulder
Patients with chronic or subacute symptoms may demonstrate loss of range of motion, a painful arc of motion from 70-110° of forward elevation, or impingement signs. Catching or crepitus may be noted. In the acute phase, the pain may be so severe that only little movement is allowed, and the tenderness is very marked.
Calcific tendinosis diagnosis
Rotator cuff calcific tendinitis diagnosis is made with standard radiographs of anterior–posterior (AP) views with the shoulder in internal and external rotation, outlet and axillary views of the shoulder. Plain x-rays demonstrate calcific deposits.
The calcific deposit can be characterized by its location (ie, which tendon is affected) and by its size. Symptoms usually occur if the deposit is larger than 1.5 cm, although one study found no correlation between the size of the deposit and the severity of the symptoms.
Calcific deposits have varying appearance. Two types of deposits have been recognized: a localized, homogeneous deposit with well-defined limits, which has been identified with the formative or resting phases, and a more diffuse, heterogeneous, amorphous, fluffy deposit that has a poorly defined periphery, which has been identified with acute symptoms and with the resorptive phase. However, poor correlation exists between the appearance of a calcific deposit on plain x-rays and its consistency on needling 5.
Calcific tendinosis treatment
Conservative management is always the first line of treatment. This includes non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroid injection, physiotherapy, ultrasound-guided needling and extracorporeal shock wave therapy which are aimed at promoting the natural healing process or pain relief.
Extracorporeal shock wave therapy uses sound waves that are focused to a point within the target tissue. The mechanism of action of extracorporeal shock wave therapy on calcifying tendinitis is unknown. It is probably not simply a mechanical disintegration of the calcific deposit; a tissue response is required to absorb the calcium deposit.
An assessment of minimally invasive treatments concluded that shockwave therapy is safe and effective 6. The results of one study demonstrated that positioning the shoulder in hyperextension and internal rotation during extracorporeal shock wave therapy may be a useful technique to achieve resorption of calcific deposits 7.
Kinesio taping, another rehabilitative tool, exerts an analgesic and biomechanical action on joints and muscles. A randomized controlled trrial investigated the efficacy of combined extracorporeal shock wave therapy and kinesio taping. Patients in the experimental group underwent three sessions (once a week for 3 weeks) of extracorporeal shock wave therapy with kinesio taping applied at the end of each session. Controls underwent three sessions of extracorporeal shock wave therapy only. Both groups showed significant improvement in all outcome measures, but the time course differed between the two groups. The improvement was significantly better in extracorporeal shock wave therapy+kinesio taping than extracorporeal shock wave therapy on visual analogue scale (VAS) (p=0.007), Disabilities of the Arm, Shoulder and Hand questionnaire and Subjective Shoulder Rating Questionnaire. After 12 weeks of follow-up, extracorporeal shock wave therapy+kinesio taping still showed significantly greater improvement than extracorporeal shock wave therapy on visual analog scale and Subjective Shoulder Rating Questionnaire 8.
If conservative treatment modalities fail, surgical removal of the deposits is the remaining option. Failure of nonoperative therapy has been defined as persistence of symptomatic calcific tendinitis after a minimum of 6 months of nonoperative treatment, including a minimum of 3 months of standardized nonoperative treatment 3.
Injections, needling, and lavage
Breaking up the calcific deposits by repeatedly puncturing them with a needle, aspirating the calcific material, usually with the help of repeatedly injecting and aspirating saline, is a commonly advised treatment. Some operators use 2 needles to facilitate the lavage of the subacromial space. Arthroscopic treatment is similar. The deposit can be localized by fluoroscopy or by ultrasonography.
A systemic review of literature for the efficacy of ultrasound-guided needling concluded that, due to the variation in studies and the low quality of evidence, the efficacy of ultrasound-guided needling could not be firmly established and additional high-quality studies are required 9.
In a prospective observational study, 86 patients (22 males and 64 females) with shoulder calcific tendinopathy treated with ultrasound-guided percutaneous treatment followed by a corticosteroid injection into the subacromial-subdeltoid bursa were then asked to follow a specific rehabilitation protocol (2 times/week for 5 weeks) that focused on mobility, strength, and function. All the participants had a significant decrease in the visual analog scale (VAS) and improvement in the Constant-Murley scale scores. The subjects who performed the rehabilitation exercises regularly had better results in terms of pain and functional recovery, and less associated disorders (eg, adhesive bursitis and tenosynovitis of the long head of the biceps) than those who were less compliant with the rehabilitation program 10.
Needling can be combined with lavage, in which the subacromial space is flushed with saline after the calcific deposits are broken up by repeated needling. Farin et al demonstrated excellent results with needling and lavage in 45 of 61 patients (74%) at 1-year follow-up 11. The calcification had disappeared or diminished in 74% of cases. Pfister and Gerber 12 reported that this procedure was completed successfully in 76% of 62 shoulders in their case series, and it produced significant improvement. A systematic review and meta-analysis by Zhang et al 13 concluded that ultrasound-guided percutaneous lavage has a beneficial clinical effect for calcifying tendinitis of the rotator cuff, and may offer superior pain relief and calcification clearance compared with extracorporeal shock wave therapy.
Calcific tendinosis exercises
Exercises are prescribed to maintain or regain the patient’s shoulder range of motion and all muscle strength. Physical therapy modalities are frequently employed, although their effectiveness is unproven.
The results of a study that added supervised eccentric training focused on the abductor muscles following extracorporeal shock wave therapy showed a mild improvement in maximum isometric abduction strength, but appeared to give no advantage in the short-term outcome (pain and function) compared with extracorporeal shock wave therapy alone 14.
Surgical care
An open or an arthroscopic approach may be used for surgical treatment 15. Although favorable results have been described with open removal of calcific deposits, arthroscopy has become the preferred technique to treat the chronic formative phase of calcifying tendonitis, with results similar to open surgery but with less morbidity 3.
Various arthroscopic surgical techniques are used, including complete removal of the calcium deposit (leading to a clinical amelioration) with or without closure of the residual tendon defect and needling of the tendon. A study that compared needling with complete removal of the calcium deposit and tendon repair found both techniques effective in treating pain and in improving function in chronic calcifying tendinitis recalcitrant to conservative treatment 16.
In an open procedure, the tendon is similarly incised, the deposit is curetted out, and adjacent tendon edges are debrided and, if necessary, reapproximated. Postoperatively, a sling is used for 3 days. Range-of-motion exercises are then started.
Calcific tendinosis prognosis
In general, it appears that the acute severe symptoms of calcifying tendinitis are likely to resolve spontaneously within 3 weeks. Chronic symptoms also tend to resolve over a period of months to a few years, although some have been reported to persist up to 15 years. Initially, asymptomatic shoulders with calcific deposits have been reported to become painful. This tendency for spontaneous recovery means that the effectiveness of any treatment can be established only with controlled trials.
A 2-year follow-up of 24 patients treated by arthroscopic subacromial decompression who had calcific deposits demonstrated that in 19 patients (79%), the calcific deposits became smaller, although they had not been touched 17. The postoperative clinical results of these patients were indistinguishable from those of matched patients without calcific deposits who underwent similar decompressions.
Calcification can recur following surgical treatment. Rupp et al 18 reported a 16% incidence of recurrence and Wittenberg et al 19 reported an 18% incidence.
References- Calcifying Tendonitis. https://emedicine.medscape.com/article/1267908-overview
- Calcific Tendinitis of the Shoulder. N Engl J Med. 1999 May 20;340(20):1582-4. https://www.ncbi.nlm.nih.gov/pubmed/10332023
- Merolla G, Singh S, Paladini P, Porcellini G. Calcific tendinitis of the rotator cuff: state of the art in diagnosis and treatment. J Orthop Traumatol. 2016 Mar. 17 (1):7-14.
- Uhthoff HK, Loehr JW. Calcific tendinopathy of the rotator cuff: pathogenesis, diagnosis, and management. J Am Acad Orthop Surg. 1997 Jul. 5(4):183-191.
- Izadpanah K, Jaeger M, Maier D, Südkamp NP, Ogon P. Preoperative planning of calcium deposit removal in calcifying tendinitis of the rotator cuff – possible contribution of computed tomography, ultrasound and conventional X-Ray. BMC Musculoskelet Disord. 2014 Nov 20. 15:385.
- Louwerens JK, Sierevelt IN, van Noort A, van den Bekerom MP. Evidence for minimally invasive therapies in the management of chronic calcific tendinopathy of the rotator cuff: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2014 Aug. 23 (8):1240-9.
- Tornese D, Mattei E, Bandi M, Zerbi A, Quaglia A, Melegati G. Arm position during extracorporeal shock wave therapy for calcifying tendinitis of the shoulder: a randomized study. Clin Rehabil. 2011 Aug. 25(8):731-9.
- Frassanito P, Cavalieri C, Maestri R, Felicetti G. Effectiveness of extracorporeal shock wave therapy and kinesio taping in calcific tendinopathy of the shoulder: a randomized controlled trial. Eur J Phys Rehabil Med. 2017 Nov 29.
- Vignesh KN, McDowall A, Simunovic N, Bhandari M, Choudur HN. Efficacy of ultrasound-guided percutaneous needle treatment of calcific tendinitis. AJR Am J Roentgenol. 2015 Jan. 204 (1):148-52.
- Abate M, Schiavone C, Salini V. Usefulness of rehabilitation in patients with rotator cuff calcific tendinopathy after ultrasound-guided percutaneous treatment. Med Princ Pract. 2015. 24 (1):23-9.
- Farin PU, Räsänen H, Jaroma H, Harju A. Rotator cuff calcifications: treatment with ultrasound-guided percutaneous needle aspiration and lavage. Skeletal Radiol. 1996 Aug. 25(6):551-4.
- Pfister J, Gerber H. Chronic calcifying tendinitis of the shoulder-therapy by percutaneous needle aspiration and lavage: a prospective open study of 62 shoulders. Clin Rheumatol. 1997 May. 16(3):269-74.
- Zhang T, Duan Y, Chen J, Chen X. Efficacy of ultrasound-guided percutaneous lavage for rotator cuff calcific tendinopathy: A systematic review and meta-analysis. Medicine (Baltimore). 2019 May. 98 (21):e15552.
- Carlisi E, Lisi C, Dall’angelo A, Monteleone S, Nola V, Tinelli C, et al. Focused extracorporeal shock wave therapy combined with supervised eccentric training for supraspinatus calcific tendinopathy. Eur J Phys Rehabil Med. 2018 Feb. 54 (1):41-47.
- Seyahi A, Demirhan M. Arthroscopic removal of intraosseous and intratendinous deposits in calcifying tendinitis of the rotator cuff. Arthroscopy. 2009 Jun. 25(6):590-6.
- Castagna A, DE Giorgi S, Garofalo R, Conti M, Tafuri S, Moretti B. Calcifying tendinitis of the shoulder: arthroscopic needling versus complete calcium removal and rotator cuff repair. A prospective comparative study. Joints. 2015 Oct-Dec. 3 (4):166-72.
- Tillander BM, Norlin RO. Change of calcifications after arthroscopic subacromial decompression. J Shoulder Elbow Surg. 1998 May-Jun. 7(3):213-7.
- Rupp S, Seil R, Kohn D. [Tendinosis calcarea of the rotator cuff] [German]. Orthopade. 2000 Oct. 29(10):852-67.
- Wittenberg RH, Rubenthaler F, Wölk T, et al. Surgical or conservative treatment for chronic rotator cuff calcifying tendinitis–a matched-pair analysis of 100 patients. Arch Orthop Trauma Surg. 2001. 121(1-2):56-9.