Cavernous sinus syndrome
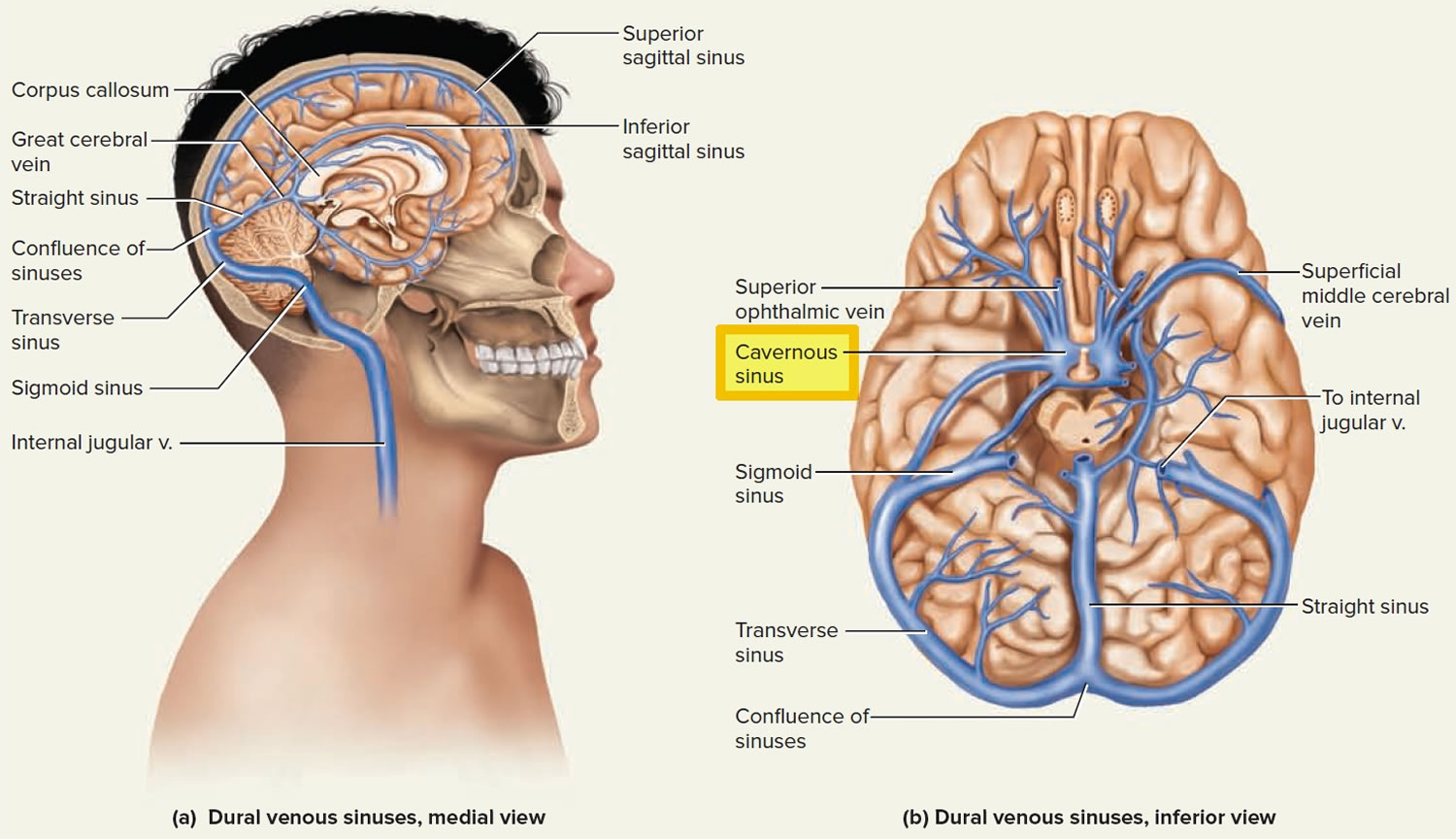
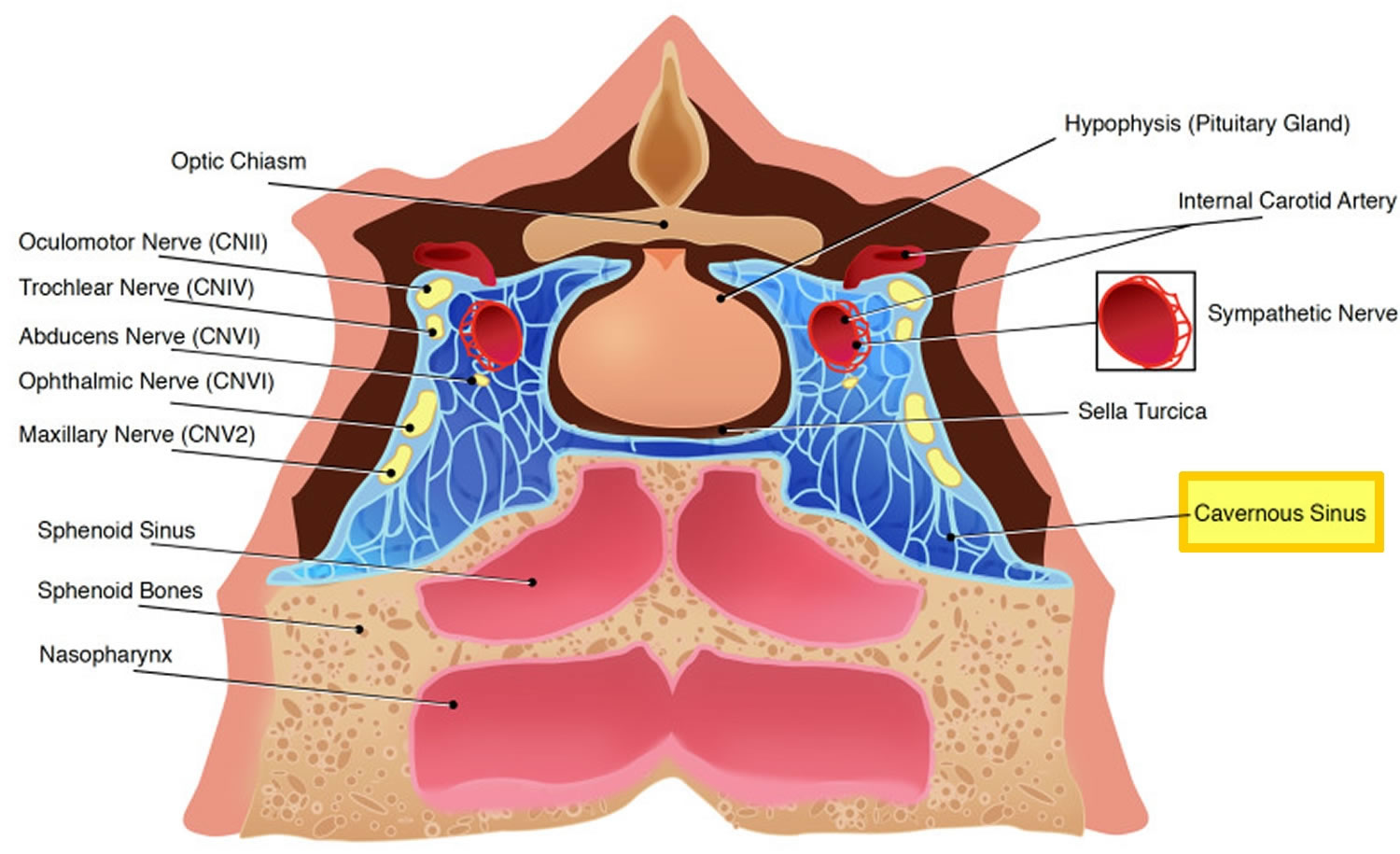
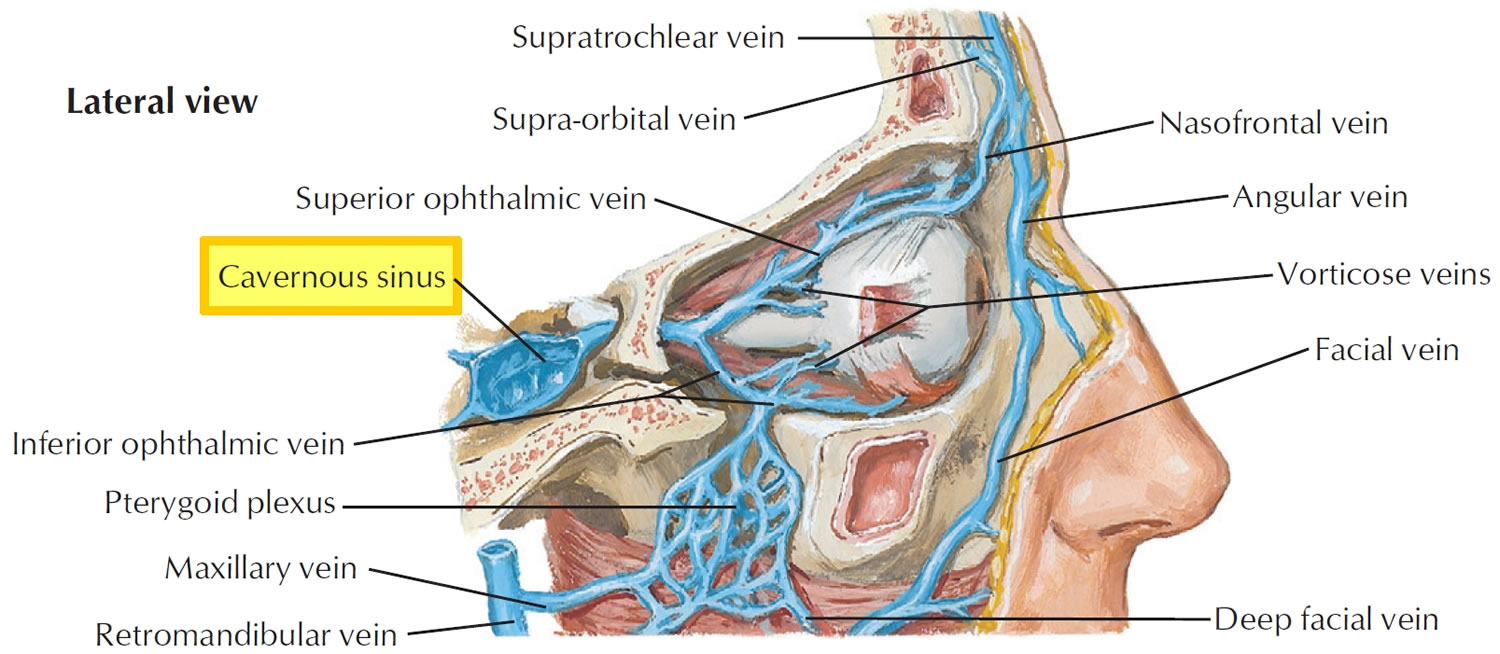
Cavernous sinus syndrome is a condition characterized by multiple cranial nerve palsies manifesting as ophthalmoplegia, chemosis, proptosis, ptosis, Horner syndrome, or trigeminal sensory loss secondary to pathologic changes in or around the cavernous sinus 1, 2. In the United States, approximately 5% of ophthalmoplegias are secondary to involvement of cranial nerves in the cavernous sinuses. This is probably true worldwide 3. The cavernous sinuses are honeycombs of blood-filled spaces on each side of the body of the sphenoid bone (Figure 1). The cavernous sinus is located on either side of the pituitary fossa and body of the sphenoid bone. The cavernous sinus spans from the apex of the orbit to the apex of the petrous temporal bone. The cavernous sinuses receive blood from the superior ophthalmic vein of the orbit and the superficial middle cerebral vein of the brain, among other sources. The cavernous sinuses drain through several outlets including the transverse sinus, internal jugular vein, and facial vein. The cavernous sinuses are clinically important because infections can pass from the face and other superficial sites into the cranial cavity by this route. Also, inflammation of a cavernous sinus can injure important structures that pass through it, including the internal carotid artery and cranial nerves III to VI (oculomotor [cranial nerve III], trochlear [cranial nerve IV], abducens nerve [cranial nerve VI] and the ophthalmic (cranial nerve V1) and maxillary (cranial nerve V2) parts of the trigeminal nerve [cranial nerve V]).
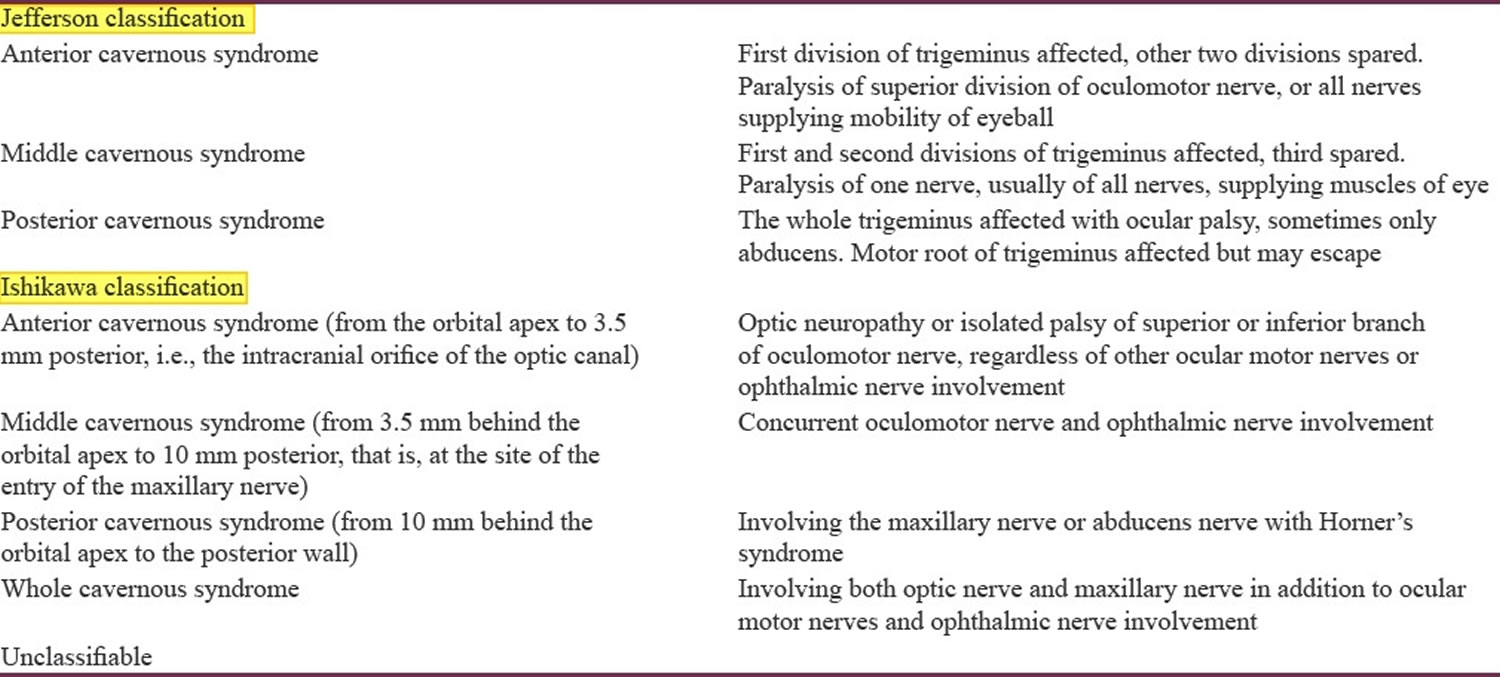
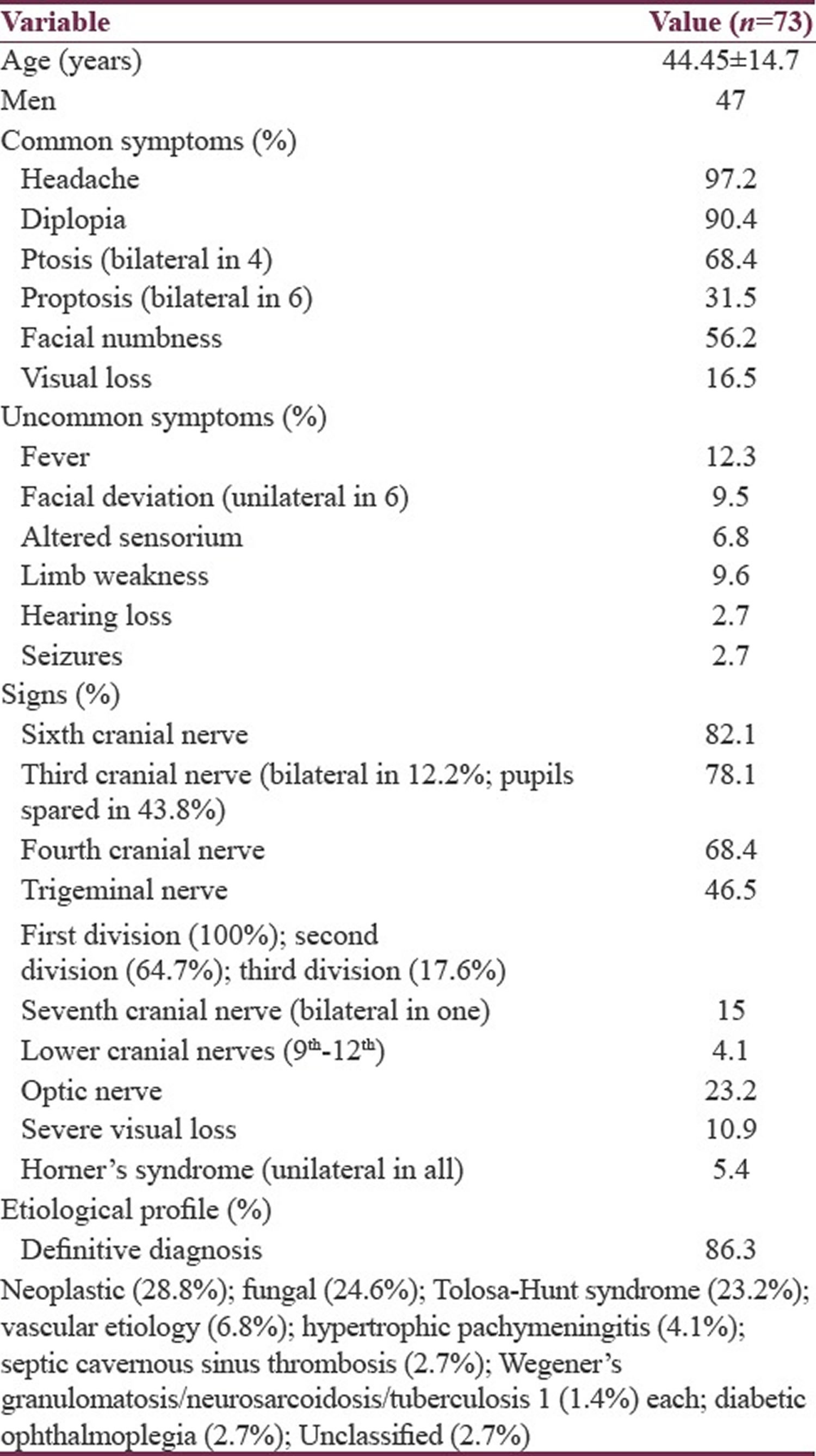
Jefferson first classified cavernous sinus syndrome in 1938 into 3 types: anterior, middle, and posterior cavernous sinus syndrome 4. Jefferson classification is based on the extent of involvement of the trigeminal nerve (cranial nerve V). In 1996, Ishikawa emphasized the lack of a clinical-anatomical correlation in Jefferson’s classification and proposed a new classification of cavernous sinus syndrome 5. Cavernous sinus syndrome was classified into 3 separated part such as the anterior, middle, posterior by Ishikawa 5. They used the optic canal and the maxillary nerve as anatomical landmarks. The Ishikawa classification in a study with 162 patients with cavernous sinus lesions was shown to be superior in identifying and classifying the localization of cavernous sinus lesions 6. However, Ishikawa classification is not superior to Jefferson based on etiology, shown by a study at a tertiary care center in Northern India with 73 consecutive cavernous sinus syndrome patients 7.
There are many causes of cavernous sinus syndrome, principally due to infectious or noninfectious inflammatory disorders, vascular, traumatic, and tumors (see Table 3 below) 8. The pathomechanism of cavernous sinus syndrome is characterized by the compression and dysfunction of the structures within the cavernous sinus. The cavernous sinus is a fixed space limited by bony structures, so any pathology within the sinus has the ability to compress internal structures, causing ophthalmoplegia and facial sensory changes. Additionally, due to the postganglionic sympathetic plexus traveling on the internal carotid artery (ICA) and cranial nerve VI (abducens nerves), damage can cause an ipsilateral loss of sympathetic tone presenting as a Horner’s syndrome (also called oculosympathetic paresis) is characterized by drooping of the upper eyelid (ptosis) on the affected side, a constricted pupil in the affected eye (miosis) resulting in unequal pupil size (anisocoria), and absent sweating (anhidrosis) on the affected side of the face. Sinking of the eye into its cavity (enophthalmos) and a bloodshot eye often occur in this disorder. The combination of cranial nerve VI (abducens nerves) palsy and ipsilateral Horner syndrome localizes the lesion to the cavernous sinus (Parkinson sign) 9.
Due to the fact that several cranial nerves including the can be wholly or partially involved in this syndrome, there is a range of clinical signs that may be elicited.
Cavernous sinus syndrome are characterized by the following signs:
- Unilateral and isolated third, fourth, or sixth cranial nerve palsy
- Variety of combination nerve palsies resulting in partial or complete ophthalmoplegia
- Painful ophthalmoplegia
- Proptosis (pulsating exophthalmos suggests a direct carotid-cavernous fistula)
- Ocular and cranial bruits
- Conjunctival congestion; arterialization of conjunctival veins
- Ocular hypertension
- Optic disc edema or pallor; retinal hemorrhages
- Anesthesia in the ophthalmic division of the trigeminal nerve (V1) and/or decreased or absent corneal reflex and possibly anesthesia in the maxillary (V2) branch
- Pupil in mid-position and nonreactive if both sympathetic and parasympathetic fibers of the third nerve are affected
The diagnosis of cavernous sinus syndrome is initially suspected on clinical grounds. However, further workup is needed to determine the underlying etiology of cavernous sinus syndrome. Due to wide array of potential causes, workup can be challenging and extensive. Imaging of the head and orbit and laboratory tests play a role in confirming the diagnosis. Patients in whom cavernous sinus lesions are suspected should undergo thin-section multiplanar imaging studies of the orbit and the sellar/parasellar region. Pre-contrast and postcontrast scans are advisable. CT scan offers better visualization of bone structures. However, MRI using T2, fluid-attenuated inversion recovery (FLAIR), pre-contrast and post-contrast T1-weighted with a fat saturated protocol images provide better detail of all soft tissues contained in the sinuses, the expected signal void of the carotid artery (image below), and its relation to the surrounding structures as well as individual nerves if the thin-section 3D are acquired.
The management of cavernous sinus syndrome depends on its underlying cause. As such, treatment is not standardized. The most common cause of cavernous sinus syndrome is tumor, but due to the variability of tumor pathology, treatment can vary. Surgery and/or radiotherapy are potential options for treatment of a tumor. Traumatic cases may self-resolve or may require orbital surgical decompression to repair severe damage and cases with significant edema. For the management of inflammatory disease, the use of systemic glucocorticoid therapy is often effective. Vascular causes such as fistulas and aneurysms are often amenable to interventional radiology procedures such as balloon or coil embolization 10. Patients with an infectious cause should receive the appropriate treatment per Infectious Diseases Society of America (IDSA) guidelines (https://www.idsociety.org/practice-guideline/practice-guidelines).
Causes such as septic cavernous sinus thrombosis that may be acutely life-threatening must be recognized and managed emergently. Intravenous antibiotics must be started immediately for the treatment of an underlying infection. Though controversial, anticoagulation is recommended. Otolaryngology should be consulted to evaluate for the need for surgical drainage of the primary infection.
Table 1. Jefferson’s and Ishikawa classification of cavernous sinus lesions
[Source 7 ]Table 2. Clinical and demographic profile of patients with cavernous sinus syndrome
[Source 7 ]Cavernous sinus anatomy
The venous drainage system of the head and face have a unique anatomy. The cavernous sinuses are honeycombs of blood-filled spaces on each side of the body of the sphenoid bone (Figure 1). The cavernous sinus is located on either side of the pituitary fossa and body of the sphenoid bone. The cavernous sinus spans from the apex of the orbit to the apex of the petrous temporal bone. The cavernous sinuses receive blood from the superior ophthalmic vein of the orbit and the superficial middle cerebral vein of the brain, among other sources (Figure 2). The cavernous sinuses are paired dural venous sinuses that communicate with one another. Unlike other dural venous sinuses, it is divided by numerous fibrous septa into a series of small caves, which is where its name is derived from. The normal lateral wall should be either straight or concave.
Cavernous sinus boundaries 11:
- roof: fold of dura mater attached to the anterior and middle clinoid processes
- anterior wall: medial end of the superior orbital fissure
- posterior wall: petrous apex
- medial wall: endosteum overlying the body of the sphenoid bone
- lateral wall: dura mater from the ridge of the roof to the floor of the middle cranial fossa
- floor: endosteum overlying the base of the greater wing of the sphenoid bone
Cavernous sinus relations 11:
- superiorly: middle cerebral artery, optic chiasm
- anteriorly: apex of the orbit
- posteriorly: cerebral peduncle
- medially: pituitary fossa, pituitary gland
- laterally: temporal lobe (medial surface), Meckel’s cave (posteroinferiorly)
- inferiorly: sphenoid sinus
Cavernous sinus contents
Cavernous sinus contents can be remembered with the mnemonic “O TOM CAT” 12. ‘O TOM’ are the first letters of components of the lateral wall of cavernous sinus considered vertically, from the top to the bottom. ‘CA’ are the first letters of the structures located within the sinus. ‘CA’ continues virtually at the level of the T of ‘O TOM’. So that the T represents the point of conjunction of the two words. See Figure 1 for further illustration.
O TOM CAT Mnemonic
- O: oculomotor nerve (CN III)
- T: trochlear nerve (CN IV)
- O: ophthalmic branch (CN V1) of trigeminal nerve
- M: maxillary branch (CN V2) of trigeminal nerve
- C: internal carotid artery
- A: abducens nerve (CN VI)
- T: trochlear nerve (CN IV)
The cavernous sinus transmits multiple cranial nerves to the superior orbital fissure and foramen rotundum. These are:
- in the lateral wall from superior to inferior
- oculomotor nerve (CN III)
- trochlear nerve (CN IV)
- trigeminal nerve (CN V)
- ophthalmic division (CN V1)
- maxillary division (CN V2): within the very inferolateral aspect of the cavernous sinus wall or even outside the sinus rather than truly within it 13
- traversing cavernous sinus
- abducens nerve (CN VI): inferolateral to the internal carotid artery
Remember two things:
- The mandibular branch (CN V3) of the trigeminal nerve is NOT associated with the cavernous sinus since it has descended vertically through the foramen ovale underneath the trigeminal ganglion (Gasser ganglion), which is anatomically posteriorly to the cavernous sinus
- The maxillary branch (CN V2) of the trigeminal nerve is external but immediately adjacent to the lateral wall of the cavernous sinus, which becomes important in the differential diagnosis of lesions of the cavernous sinus – lesions of this nerve tends to distort the sinus rather than occupy it
Cavernous sinus receives venous blood from 11:
- inferior and superior ophthalmic veins
- intercavernous sinus
- sphenoparietal sinus
- superficial middle cerebral vein
- occasionally
- central retinal vein
- a frontal tributary of the middle meningeal vein
Drainage of the cavernous sinus is via 11:
- superior petrosal sinus to the transverse sinus
- inferior petrosal sinus directly to the jugular bulb
- venous plexus on the internal carotid artery (ICA) to the clival (basilar) venous plexuses
- emissary veins passing through the
- foramen Vesalii
- foramen ovale: communicates between the cavernous sinus and pterygoid venous plexus
- foramen lacerum
- Depending on relative pressures the superior ophthalmic veins either drain to or from the cavernous sinus. Additionally, the cavernous sinuses connect to each other via the intercavernous sinuses.
Each cavernous sinus is flanked laterally by the temporal bone of the skull and inferiorly by the sphenoid bone, with close proximity to the sphenoid sinuses. The lateral wall of the cavernous sinus is primarily formed by the continuation of the meningeal layer of the dura, flowing medially up from the floor of the middle cranial fossa, over the cavernous sinus, to the clinoid processes before forming the diaphragma sella (a sheet of dura mater that forms the roof of the pituitary fossa). From here, the meningeal layer passes downwards to surround the pituitary gland, thus forming the medial wall of the cavernous sinus. In contrast, the floor of the cavernous sinus is formed by the endosteal layer of the meninges (actually just periosteum) that covers the sphenoid bone and passes medially across the midline below the pituitary gland, separated from the aforementioned meningeal layer by the intercavernous sinus 14.
The pituitary gland sits within the sella turcica which exists medial to the cavernous sinus, and the optic chiasm lies superior to the cavernous sinus on the midline in close proximity to the pituitary gland (Figure 1) 15.
The nerves in the lateral wall of the cavernous sinus are surrounded by thin connective tissue and thus, the lateral wall of the cavernous sinus has two layers; a thick meningeal layer and a much thinner translucent layer surrounding the cranial nerves 14. This thin layer is variably described as being meningeal in origin 16 or continuous with the endosteal layer 14.
The dural sinuses and the cerebral and emissary veins have no valves, which allows blood to flow in either direction (anterograde or retrograde) according to venous pressure gradients in the vascular system. This fact and the extensive direct and indirect vascular connections of the centrally located cavernous sinuses make them vulnerable to pathology at many sites 17.
Each cavernous sinus receives venous drainage from several structures within the face and eye. The superior and inferior ophthalmic veins drain anteriorly into the sinus. The superficial middle cerebral veins, deep cerebral veins (via the sphenoparietal sinus), and inferior cerebral veins drain into the cavernous sinus as well. Inferiorly, the cavernous sinus drains to the pterygoid plexus and posteriorly, it communicates with the superior and inferior petrosal sinuses. Both drainage systems ultimately converge at the internal jugular vein (Figure 2) 18.
The presence of important cranial nerves and blood vessels makes the cavernous sinus a unique site for potential pathology (Figure 1). The internal carotid artery (ICA) traverses the carotid sinuses bilaterally. Post-ganglionic, third-order sympathetic fibers (Horner syndrome) run on the internal carotid artery (ICA) and cranial nerve VI (abducens nerve) and then cranial nerve V1 (ophthalmic nerve). Cranial nerve III (oculomotor nerve), cranial nerve IV (trochlear nerve), cranial nerve V1 (ophthalmic nerve) and cranial nerve V2 (maxillary nerve) are all tethered to the lateral wall of the cavernous sinus, but cranial nerve VI (abducens nerve) lies freely inferolateral to the internal carotid artery (ICA) and medially to the other cranial nerves. Cranial nerve II (optic nerve) does not travel within the cavernous sinus, but is closely associated superomedially 15.
Figure 1. Cavernous sinus anatomy
Figure 2. Cavernous sinus drainage
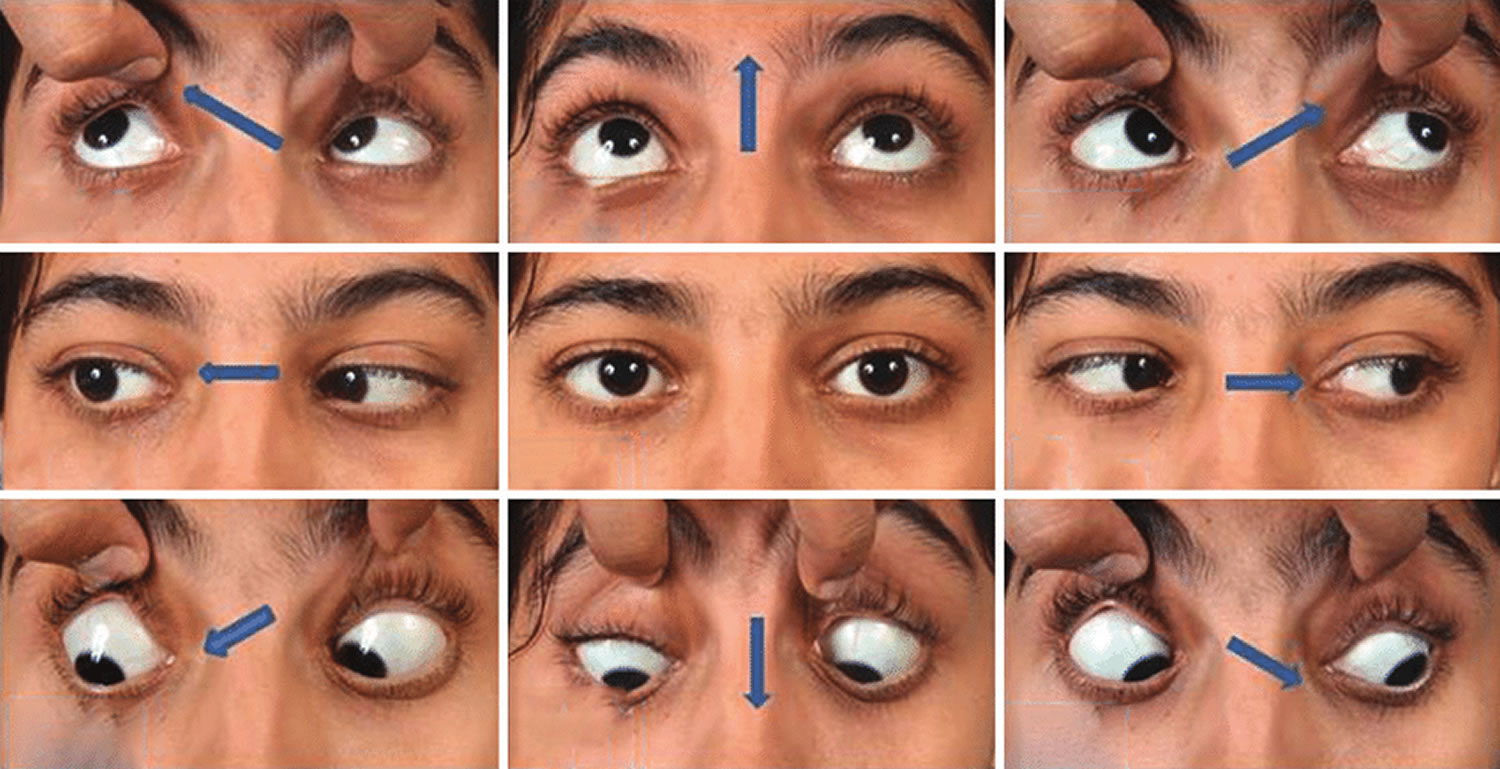
Figure 3. Cavernous sinus syndrome
Footnote: 34-year-old female presenting with right lateral rectus palsy and numbness over mandibular division of trigeminal nerve caused by meningioma. Extraocular movements in 9 cardinal positions of gaze (a-i) (the black and white arrows indicate the direction of intended movement of eyeballs). Note: Restriction of right eye in lateral gaze (two-dimensional) suggestive of the right lateral rectus palsy; contrast-enhanced magnetic resonance imaging of the brain (3J-K) was suggestive of a meningioma (3J-coronal, 3K-axial) (black and white arrows).
[Source 7 ]Cavernous sinus syndrome symptoms
The signs and symptoms frequently found in patients with cavernous sinus lesions present with multiple unilateral cranial neuropathies involving any combination of the following 19:
- Ophthalmoplegia (cranial nerves III, IV, or VI), most commonly presenting as diplopia and visual loss
- Total/partial ophthalmoplegia
- CN III (oculomotor nerve) palsy – partial or total loss of elevation, depression and adduction of ipsilateral eye
- CN IV (trochlear nerve) palsy – partial or total loss of abduction and depression of ipsilateral eye
- CN VI (abducens nerve) palsy – partial or total loss of abduction of ipsilateral eye
- Total/partial ophthalmoplegia
- Facial sensory loss (cranial nerves V1 and V2)
- CN V1 loss – partial or total loss of sensation in ophthalmic distribution
- CN V2 loss – partial or total loss of sensation in maxillary distribution
- Horner syndrome (oculosympathetic fibers presenting with classic triad of ptosis, miosis, and anhidrosis)
Pain can occur, especially with inflammatory processes.
Additional symptoms may be vascular in origin (due to increased pressure within cavernous sinus):
- Chemosis (swelling of the tissue that lines the eyelids and surface of the eye [conjunctiva])
- Proptosis (bulging eyes)
- Elevation of ocular pressure
Presence of fever, tachycardia, hypotension, rigors, nuchal rigidity, altered mental status should cause concern for cavernous sinus thrombosis.
It is important to note that cavernous sinus syndrome does not always include all these findings. Cavernous sinus syndrome may present with any combination of these symptoms, which generally are unilateral but may be bilateral with neoplastic processes. Symptoms may be acute or slowly progressive.
Cavernous sinus syndrome causes
Cavernous sinus syndrome is caused by any pathology or lesion present within the cavernous sinus that disrupts the function of other anatomical structures. The most common cause of cavernous sinus syndrome is mass effect from a primary tumor. Other common causes of cavernous sinus syndrome include trauma and self-limited inflammatory disease. Less common causes are vascular etiologies and infections 20. Lymphomas have been reported to involve the cavernous sinus, both as primary cavernous sinus lymphomas or as secondary lesions 21.
One important infectious etiology of cavernous sinus syndrome includes cavernous sinus thrombosis, which may present initially to an ophthalmologist and requires urgent management due to its life-threatening prognosis. Septic cavernous sinus thrombosis is typically seen as a complication of a facial infection, such as sinusitis or cellulitis. Due to the valveless nature of the facial veins, the sinuses are vulnerable to stagnation and poor drainage in the setting of severe infection, causing the formation of a thrombus. The thrombus can then cause damage locally or travel to the brain, causing stroke-like symptoms or encephalitis and meningitis 15. Specific causes of cavernous sinus syndrome are listed in Table 3.
Table 3. Cavernous sinus syndrome causes
| Etiology | Division | Example |
|---|---|---|
| Infection | Fungal | Mucormycosis, phycomycosis, aspergillosis |
| Viral | Herpes zoster virus opthalmicus | |
| Bacterial | Meningitis, actinomycosis, nocardiosis, mycobacterium, cavernous sinus thrombophlebitis (septic cavernous sinusitis) | |
| Tumors | Within cavernous sinus (primary tumors) | Meningeal tumors (e.g., meningioma, melanocytoma), peripheral nerve sheath tumors (e.g., schwannoma, neurofibroma, malignant peripheral nerve sheath tumor) |
| Compressive tumors | Pituitary adenomas, craniopharyngioma, neuroma, skull base tumors (e.g. chordoma, chondrosarcoma), metastatic lesions (e.g. lung cancer, breast cancer), hematolymphoid tumors (e.g. lymphoma, plasmacytoma, leukemia), nasopharyngeal carcinoma, cavernous malformation (cavernous hemangioma), neuroblastoma, histiocytoses (e.g. Langerhans cell histiocytosis, Rosai-Dorfman disease), head and neck tumors (e.g. nasopharyngeal carcinoma, adenoid cystic carcinoma, squamous cell carcinoma, juvenile angiofibroma) | |
| Vascular | Aneurysms | Cavernous segment aneurysm, intramural intracranial aneurysm, internal carotid artery aneurysm |
| Carotid-cavernous fistulas | Direct and indirect fistulas, dural arteriovenous fistula | |
| Cavernous sinus thrombosis | ||
| Trauma | Any base of skull fracture which involves the cavernous sinus, operative trauma to cavernous sinus after skull base surgery | |
| Inflammation | Sarcoidosis | |
| Tolosa–Hunt syndrome | ||
| Granulomatosis with polyangiitis (Wegener’s granulomatosis) | ||
| Congenital/developmental | Epidermoid cyst | |
| Dermoid cyst | ||
Cavernous sinus tumors
Cavernous sinus tumors are the most common cause of cavernous sinus syndrome 24. Tumors may be primary or arise as either local spread or metastases. Examples of primary tumors include schwannoma, plexiform neurofibroma, malignant peripheral nerve sheath tumor, cavernous hemangioma, meningioma, melanocystoma, chondroma and chondrosarcoma. Examples of locally spreading tumors are nasopharyngeal carcinoma, pituitary adenoma, chordoma, epidermoid and dermoid cyst. Metastatic lesions are most often from the breast, prostate, or the lung. Total resection of these lesions remains very challenging and, in many cases, impossible if the lesion is invasive 25. Other treatment solutions include radiotherapy, which often offers transient relief, particularly in nasopharyngeal cancer. Lateral extension of pituitary tumors may be treated with surgical resection and dopamine agonists in the case of prolactinoma 26.
Acute or slowly progressive ophthalmoplegia is the dominant presentation, with diplopia being the most common symptom. At times, painful diplopia is present.
Usually the patient has a preceding history of cancer. Occasionally, cavernous sinus syndrome is the first manifestation of a systemic neoplasm (leukemia, lymphoma).
Exophthalmos can be observed.
If the tumor is a pituitary macroadenoma, endocrine symptoms and/or visual field deficits may be present.
Carotid-cavernous aneurysms
Unlike intracranial aneurysms in the extradural locations, carotid-cavernous aneurysms do not involve a major risk of subarachnoid hemorrhage but often are giant (>2.5cm in diameter). Thus they produce symptoms through compression of the adjacent structures and their rupture can result in direct carotid-cavernous fistulas. These aneurysms, which are more frequent in the elderly, often present with an indolent ophthalmoplegia. Although some patients suffer minor disability and do not require treatment, endovascular coiling is often successful and is attempted in many patients 27.
Patients frequently are elderly and present with subacute or chronic ophthalmoplegia. Rarely, they may have pain similar to that of trigeminal neuralgia.
Spontaneous rupture of a carotid-cavernous aneurysm leads to an abrupt onset of a direct carotid-cavernous fistula fistula. This results in acute onset of massive exophthalmos with orbital, ocular, and conjunctival chemosis, binocular diplopia, and visual loss.
Carotid-cavernous fistulas
Carotid-cavernous fistula is an abnormal connection between the carotid artery and the sinus. There are 2 main types of carotid-cavernous fistulas. Direct fistula (type A) is characterized by a high blood flow communication between the carotid artery and cavernous sinus. It manifests with a sudden onset of pulsating exophthalmos, proptosis, chemosis, visual loss, and usually painful ophthalmoplegia. Trauma or aneurysm rupture is a common cause of a direct carotid-cavernous fistula. Dural fistula (types B–D) occurs when communication develops between the cavernous sinus and the meningeal or persistent fetal branches of the internal carotid artery, external carotid artery, or both. This type has a milder and more insidious presentation than a direct fistula, often with spontaneous resolution. Indirect fistulas are characterized by mild proptosis, chronic diplopia, drooping of the lid, a red eye, arterialization of the conjunctival vessels, and visual loss. The patient may report subjective “noises” in his or her head. Interventional radiologists can successfully treat all fistula types by endovascular occlusion techniques. Occasionally, surgical treatment with carotid ligation is necessary; this sometimes is preceded by a superficial temporal-to-middle cerebral bypass to ensure cerebral circulation after carotid ligation 26.
Cavernous sinus thrombosis
Cavernous sinus thrombosis is a blood clot in an area at the base of the brain. Cavernous sinus thrombosis is most often caused by a bacterial infection that has spread from the sinuses, teeth, ears, eyes, nose, or skin of the face. However, this is infrequent in the antibiotic era.
You are more likely to develop cavernous sinus thrombosis if you have an increased risk of blood clots.
Cavernous sinus thrombosis may occur as a complication of spreading infection from the ethmoid, sphenoid, or frontal sinuses or from midfacial, dental, or orbital infections.
Patients may present with sepsis or metastatic spread of septic emboli, most commonly occurring in the lung. This presentation may appear as acute respiratory distress syndrome (ARDS).
Retrobulbar pain, drooping of the upper eyelid, and diplopia may be the first symptoms indicating the lesion’s extension to the cavernous sinus.
Cavernous sinus inflammatory and granulomatous lesions
These may involve the cavernous sinuses or the walls of the sinus. Infection within cavernous sinus or in the adjacent structures can result in sinus thrombosis and/or development of inflammatory changes. The rare but important causes include: aspergillosis, Wegener granulomatosis, tuberculosis, and sarcoidosis. Some of these share symptoms with Tolosa-Hunt syndrome (unilateral ophthalmoplegia, cranial nerve palsies, and a dramatic response to corticosteroids), which describes a retroorbital pseudotumor encroaching the cavernous sinus 26.
Herpes zoster in its acute or chronic stage rarely causes pain, diplopia, and a droopy eyelid in addition to the typical zoster blisters. In the chronic stage, a scar from the acute lesion usually is found.
An idiopathic inflammation of the walls of the cavernous sinuses is referred to as Tolosa-Hunt syndrome.
Sarcoid or Wegener granulomatosis may also predispose to cavernous sinus syndrome.
Cavernous sinus syndrome differential diagnosis
- Infectious: Bacterial, fungal (e.g., mucormycosis, aspergillosis), viral (e.g., HSV), mycobacterial
- Inflammatory: Granulomatosis with polyangiitis (GPA), idiopathic orbital inflammatory syndrome, IgG4-related ophthalmic disease, sarcoidosis, Tolosa-Hunt syndrome
- Neoplastic: Nasopharyngeal carcinoma, lymphoma, meningioma, craniopharyngioma, pituitary adenoma, metastasis
- Vascular: Carotid-cavernous fistula, internal carotid artery aneurysm, cavernous sinus thrombosis
- Iatrogenic: Sinus/orbital/facial surgery
- Traumatic
Cavernous sinus syndrome diagnosis
The diagnosis of cavernous sinus syndrome is initially suspected on clinical grounds. However, further workup is needed to determine the underlying etiology of cavernous sinus syndrome. Due to wide array of potential causes, workup can be challenging and extensive. Imaging of the head and orbit and laboratory tests play a role in confirming the diagnosis.
The patient’s history should be clinically correlated with the physical examination findings, and the appropriate diagnostic tests should be performed accordingly, to reach a diagnosis efficiently. Blood tests, such as complete blood count (CBC) and blood cultures, can be used to assess for underlying infection. Serum studies, such as erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), angiotensin converting enzyme (ACE), and antineutrophil cytoplasmic antibodies (ANCA) are recommended to evaluate for an underlying inflammatory process.
Magnetic resonance imaging (MRI) of the brain and orbits with contrast and magnetic resonance venography (MRV) is preferred to determine the presence of a tumor, trauma, inflammation, or cavernous sinus thrombosis. Imaging with computed tomography (CT) of the brain and orbits or CT venography can be done to help adjudicate the presence of trauma or vascular process 28.
Patients in whom cavernous sinus lesions are suspected should undergo thin-section multiplanar imaging studies of the orbit and the sellar/parasellar region. Pre-contrast and postcontrast scans are advisable. CT scan offers better visualization of bone structures. However, MRI using T2, fluid-attenuated inversion recovery (FLAIR), pre-contrast and post-contrast T1-weighted with a fat saturated protocol images provide better detail of all soft tissues contained in the sinuses, the expected signal void of the carotid artery and its relation to the surrounding structures as well as individual nerves if the thin-section 3D are acquired.
Cavernous sinus syndrome treatment
The management of cavernous sinus syndrome depends on its underlying cause. As such, treatment is not standardized. The most common cause of cavernous sinus syndrome is tumor, but due to the variability of tumor pathology, treatment can vary. Surgery and/or radiotherapy are potential options for treatment of a tumor. Traumatic cases may self-resolve or may require orbital surgical decompression to repair severe damage and cases with significant edema. For the management of inflammatory disease, the use of systemic glucocorticoid therapy is often effective. Vascular causes such as fistulas and aneurysms are often amenable to interventional radiology procedures such as balloon or coil embolization 10. Patients with an infectious cause should receive the appropriate treatment per Infectious Diseases Society of America (IDSA) guidelines (https://www.idsociety.org/practice-guideline/practice-guidelines).
Causes such as septic cavernous sinus thrombosis that may be acutely life-threatening must be recognized and managed emergently. Intravenous antibiotics must be started immediately for the treatment of an underlying infection. Though controversial, anticoagulation is recommended. Otolaryngology should be consulted to evaluate for the need for surgical drainage of the primary infection.
Cavernous sinus tumors
Tumors in cavernous sinus represent a major challenge for surgical resection because of their proximity to critical neurologic structures making it difficult for complete excision or leaving a high risk of complications with surgical resection. Radiotherapy is important in providing excellent tumor control and avoiding the risk of surgery 29.
About 400 patients with cavernous sinus meningiomas treated with stereotactic radiosurgery in three large series from a dose of 12 to 14 Gy resulted in a five-year tumor control rate ranging from 94 to 98 percent 30.
Transsphenoidal surgery is the preferred treatment for most kinds of pituitary adenomas. Gamma knife surgery (GKS) is a common treatment for recurrent or residual pituitary adenomas 31.
Radiotherapy may offer transient relief, particularly in nasopharyngeal cancer.
Whole radiotherapy may offer a transient improvement of metastatic lesions.
Cavernous sinus aneurysms
Carotid-cavernous aneurysms have the lowest rates of rupture is shown for unruptured cerebral aneurysms in a Japanese cohort 32. Unruptured intracranial aneurysms treatment has been evaluated by a 2003 International Study of Unruptured Intracranial Aneurysms performing cost-effectiveness analyzes that showed treatment was ineffective or not cost-effective for large aneurysms (greater than 25 mm) and located in the cavernous carotid artery for 40-year-old patients 33. Treat cavernous sinus aneurysms by endovascular balloon occlusion.
Carotid-cavernous fistulas
The management of carotid-cavernous fistulas depends on the classification of carotid-cavernous fistulas, the onset of symptoms, and the risk of long-term neurological impairment. Most of (20% to 60%) indirect carotid-cavernous fistulas will close spontaneously 34. Direct carotid-cavernous fistulas should be closed if symptomatic and at risk of progression with attendant morbidity because these carotid-cavernous fistulas are unlikely to close spontaneously.
Access to the fistula may be intraarterial; however, the transvenous approach has become the mainstay of treatment, in some cases a combined surgical/endovascular approach can be used with surgical exposure of the superior ophthalmic vein followed by fistula embolization. Several venous approaches have been used, including the safest transfemoral approach; however, if this is not feasible, a superior orbital vein or a percutaneous trans-orbital puncture to the cavernous sinus can be used 35.
Surgery can be considered when endovascular treatment is not possible or is unsuccessful. Surgery includes placement of packing, sealing with fascia and glue, suturing or clipping the fistula. Stereotactic radiosurgery is indicated when an endovascular approach is not feasible, and surgical intervention is difficult or carries a risk of significant morbidity 36.
Supraorbital vein dissection with placement of a catheter to access the cavernous sinuses has been performed successfully.
Percutaneous trans-orbital access to the cavernous sinus followed by embolization.
Small indirect carotid-cavernous fistulas may occlude either spontaneously or following diagnostic angiography. If the clinical signs are mild, consider careful monitoring.
The management of increased intraocular pressure with topical agents, beta-blockers, acetazolamide, and intravenous corticosteroids may give some relief. If vision loss is threatened or intraocular pressure remains elevated, closure of the fistula required for favorable pressure control.
Cavernous sinus thrombosis
The management of cavernous sinus thrombosis should include antimicrobial with/without surgical drainage of the air sinuses or mastoid regions and antithrombotic therapies. High-dose antibiotic therapy should be directed against the most common pathogens, such as S. aureus and S. pneumoniae, as well as gram-negative rods and anaerobes. Patient with cavernous sinus thrombosis should be treated for 3 to 4 weeks with intravenous antibiotic(s) or somites 6 to 7 weeks on the clinical picture. Treatment should be broad-spectrum with vancomycin vs. nafcillin plus a third-generation cephalosporin plus metronidazole until a definite pathogen 37. Antifungal therapy with Amphotericin-B is required in the developing countries.
Anticoagulation in cavernous sinus thrombosis evoked by infection is controversial, but may hasten recovery. Retrospective analysis suggests that treatment with heparin may reduce mortality in carefully selected cases of septic cavernous-sinus thrombosis 38.
Drainage of any primary site of infection (eg, abscess, sinusitis) is advised.
Corticosteroids are not recommended. Steroids in the acute phase of cerebral venous thrombosis were not useful and were detrimental in patients without parenchymal cerebral lesions. These results do not support the use of steroids in cerebral venous thrombosis in the International Study on Cerebral Veins and Dural Sinus Thrombosis 39. The potential benefit of using the corticosteroid on cavernous sinus thrombosis would be decreased inflammation and vasogenic edema surrounding cranial nerves and orbital structures.
Anticoagulation also may be helpful in aseptic patients.
Miscellaneous inflammatory syndromes
Inflammatory cavernous sinus syndromes may respond to treatment of the specific systemic inflammation or vasculitis etiology.
Tolosa-Hunt syndrome responds well to a 3- to 6-month course of high-dose steroid therapy that can be tapered slowly thereafter 40. Initial high-dose glucocorticoids for two to four weeks followed by a gradual taper for at least 4 to 6 weeks up to several months. Close clinical follow-up with repeat MRI every 1 to 2 months is necessary to be sure followed by a gradual taper for at least 4 to 6 weeks up to several months. Close clinical follow-up with repeat MRI, 1 to 2 months, is necessary to be sure the glucocorticoid treatment remains effective, and no evidence of another etiology develops, as seen in a case report showing the progression of Tolosa-Hunt syndrome to a carotid-cavernous fistula 41, 42.
Radiotherapy and immunosuppressive medications like cyclosporine, azathioprine, methotrexate, mycophenolate mofetil, and infliximab have been tried in many case reports with benefits 43, 44.
Cavernous sinus syndrome prognosis
Most of the lesions affecting the cavernous sinuses are treatable.
Metastatic cancer is a frequent cause of cavernous sinus syndromes, and the prognosis depends on the specific tumor type.
Cavernous sinus septic thrombophlebitis mortality has decreased from 100% to 20% with the improvement of diagnosis and therapies.
Cavernous sinus aneurysms and carotid-cavernous fistulas can be treated successfully by endovascular techniques.
Lateral extension of pituitary tumors, a common cause of this syndrome, can be treated by surgical resection, radiation therapy in selected patients, and a dopamine agonist in the case of prolactinoma.
References- Nambiar R, Nair SG. Cavernous sinus syndrome. Proc (Bayl Univ Med Cent). 2017 Oct;30(4):455-456. doi: 10.1080/08998280.2017.11930227
- Toro J, Burbano LE, Reyes S, et al. Cavernous sinus syndrome: need for early diagnosis. Case Reports 2015;2015:bcr2014206999
- Cavernous Sinus Syndromes. https://emedicine.medscape.com/article/1161710-overview#a6
- Jefferson G. On the saccular aneurysms of the internal carotid artery in the cavernous sinus. Br J Surg. 1938;26:267–302.
- Ishikawa H. Clinical anatomy of the cavernous sinus. Shinkei Ganka (Neuroophthalmol Jpn) 1996;13:357–63.
- Yoshihara M, Saito N, Kashima Y, Ishikawa H. The Ishikawa classification of cavernous sinus lesions by clinico-anatomical findings. Jpn J Ophthalmol. 2001 Jul-Aug;45(4):420-4. doi: 10.1016/s0021-5155(01)00335-5
- Bhatkar S, Goyal MK, Takkar A, Modi M, Mukherjee KK, Singh P, Radotra BD, Singh R, Lal V. Which Classification of Cavernous Sinus Syndrome is Better – Ishikawa or Jefferson? A Prospective Study of 73 Patients. J Neurosci Rural Pract. 2016 Dec;7(Suppl 1):S68-S71. doi: 10.4103/0976-3147.196448
- Alioglu B, Ustun H, Sonmez A, Kaplan H, Arikan FI, Dallar Y. A rare presentation of central nervous system in a pediatric patient with Hodgkin disease: cavernous sinus syndrome. J Pediatr Hematol Oncol. 2009 Oct;31(10):774-7. doi: 10.1097/MPH.0b013e3181a712f3
- Harris FS, Rhoton AL. Anatomy of the cavernous sinus. A microsurgical study. J Neurosurg. 1976 Aug;45(2):169-80. doi: 10.3171/jns.1976.45.2.0169
- Das S, Bendok BR, Novakovic RL, Parkinson RJ, Rosengart AJ, Macdonald RL, Frank JI. Return of vision after transarterial coiling of a carotid cavernous sinus fistula: case report. Surg Neurol. 2006 Jul;66(1):82-5; discussion 85. doi: 10.1016/j.surneu.2005.10.008
- Gaillard, F., Hacking, C. Cavernous sinus. Reference article, Radiopaedia.org. https://doi.org/10.53347/rID-5258
- Raz, E., Gaillard, F. Cavernous sinus contents (mnemonic). Reference article, Radiopaedia.org. https://doi.org/10.53347/rID-1805
- Tubbs RS, Hill M, May WR, Middlebrooks E, Kominek SZ, Marchase N, Shoja MM, Loukas M, Oakes WJ. Does the maxillary division of the trigeminal nerve traverse the cavernous sinus? An anatomical study and review of the literature. Surg Radiol Anat. 2008 Feb;30(1):37-40. doi: 10.1007/s00276-007-0280-7
- Yasuda A, Campero A, Martins C, Rhoton AL Jr, de Oliveira E, Ribas GC. Microsurgical anatomy and approaches to the cavernous sinus. Neurosurgery. 2008 Jun;62(6 Suppl 3):1240-63. doi: 10.1227/01.neu.0000333790.90972.59
- Tamhankar MA, Biousse V, Ying GS, Prasad S, Subramanian PS, Lee MS, Eggenberger E, Moss HE, Pineles S, Bennett J, Osborne B, Volpe NJ, Liu GT, Bruce BB, Newman NJ, Galetta SL, Balcer LJ. Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study. Ophthalmology. 2013 Nov;120(11):2264-9. doi: 10.1016/j.ophtha.2013.04.009
- Kawase T, van Loveren H, Keller JT, Tew JM. Meningeal architecture of the cavernous sinus: clinical and surgical implications. Neurosurgery. 1996 Sep;39(3):527-34; discussion 534-6. doi: 10.1097/00006123-199609000-00019
- Ebright JR, Pace MT, Niazi AF. Septic thrombosis of the cavernous sinuses. Arch Intern Med. 2001 Dec 10-24;161(22):2671-6. doi: 10.1001/archinte.161.22.2671
- Vascular supply of the brain. Waxman S.G.(Ed.), (2017). Clinical Neuroanatomy, 28e. McGraw Hill. https://accessmedicine.mhmedical.com/content.aspx?bookid=1969§ionid=147037147
- Deng, F., Knipe, H. Cavernous sinus syndrome. Reference article, Radiopaedia.org. https://doi.org/10.53347/rID-67259
- Keane JR. Cavernous sinus syndrome. Analysis of 151 cases. Arch Neurol. 1996 Oct;53(10):967-71. doi: 10.1001/archneur.1996.00550100033012
- Lopes da Silva R. Spectrum of neurologic complications in chronic lymphocytic leukemia. Clin Lymphoma Myeloma Leuk. 2012 Jun;12(3):164-79. doi: 10.1016/j.clml.2011.10.005
- Soni AJ, Lee-Pan EB. Recurrent Hodgkin’s Disease Presenting as a Clinically Isolated Cavernous Sinus Syndrome. Case Rep Neurol Med. 2021 Aug 7;2021:3946231. doi: 10.1155/2021/3946231
- Fernández S, Godino O, Martínez-Yélamos S, Mesa E, Arruga J, Ramón JM, Acebes JJ, Rubio F. Cavernous sinus syndrome: a series of 126 patients. Medicine (Baltimore). 2007 Sep;86(5):278-281. doi: 10.1097/MD.0b013e318156c67f
- Cavernous Sinus Syndromes. https://emedicine.medscape.com/article/1161710-overview#a5
- Shimizu Y, Tsutsumi S, Yasumoto Y, Ito M. Carotid cavernous sinus fistula caused by dental implant-associated infection. Am J Otolaryngol. 2012 May-Jun;33(3):352-5. doi: 10.1016/j.amjoto.2011.08.002
- Razek AA, Castillo M. Imaging lesions of the cavernous sinus. AJNR Am J Neuroradiol. 2009 Mar;30(3):444-52. doi: 10.3174/ajnr.A1398. Epub 2008 Dec 18. Erratum in: AJNR Am J Neuroradiol. 2009 Aug;30(7):E115.
- Shelton JB, Ramakrishnaiah R, Glasier CM, Phillips PH. Cavernous sinus syndrome from an internal carotid artery aneurysm in an infant with tuberous sclerosis. J AAPOS. 2011 Aug;15(4):389-91. doi: 10.1016/j.jaapos.2011.03.013
- Goyal P, Lee S, Gupta N, Kumar Y, Mangla M, Hooda K, Li S, Mangla R. Orbital apex disorders: Imaging findings and management. Neuroradiol J. 2018 Apr;31(2):104-125. doi: 10.1177/1971400917740361
- Pollock BE, Stafford SL, Link MJ, Garces YI, Foote RL. Single-fraction radiosurgery for presumed intracranial meningiomas: efficacy and complications from a 22-year experience. Int J Radiat Oncol Biol Phys. 2012 Aug 1;83(5):1414-8. doi: 10.1016/j.ijrobp.2011.10.033
- Spiegelmann R, Cohen ZR, Nissim O, Alezra D, Pfeffer R. Cavernous sinus meningiomas: a large LINAC radiosurgery series. J Neurooncol. 2010 Jun;98(2):195-202. doi: 10.1007/s11060-010-0173-1
- Sheehan JP, Pouratian N, Steiner L, Laws ER, Vance ML. Gamma Knife surgery for pituitary adenomas: factors related to radiological and endocrine outcomes. J Neurosurg. 2011 Feb;114(2):303-9. doi: 10.3171/2010.5.JNS091635
- Kuo JS, Chen JC, Yu C, Zelman V, Giannotta SL, Petrovich Z, MacPherson D, Apuzzo ML. Gamma knife radiosurgery for benign cavernous sinus tumors: quantitative analysis of treatment outcomes. Neurosurgery. 2004 Jun;54(6):1385-93; discussion 1393-4. doi: 10.1227/01.neu.0000124750.13721.94
- Kupersmith MJ, Berenstein A, Choi IS, Ransohoff J, Flamm ES. Percutaneous transvascular treatment of giant carotid aneurysms: neuro-ophthalmologic findings. Neurology. 1984 Mar;34(3):328-35. doi: 10.1212/wnl.34.3.328
- de Keizer R. Carotid-cavernous and orbital arteriovenous fistulas: ocular features, diagnostic and hemodynamic considerations in relation to visual impairment and morbidity. Orbit. 2003 Jun;22(2):121-42. doi: 10.1076/orbi.22.2.121.14315
- Boghen D, Chartrand JP, Laflamme P, Kirkham T, Hardy J, Aube M. Primary aberrant third nerve regeneration. Ann Neurol. 1979 Nov;6(5):415-8. doi: 10.1002/ana.410060507
- O’Leary S, Hodgson TJ, Coley SC, Kemeny AA, Radatz MW. Intracranial dural arteriovenous malformations: results of stereotactic radiosurgery in 17 patients. Clin Oncol (R Coll Radiol). 2002 Apr;14(2):97-102. doi: 10.1053/clon.2002.0072
- Desa V, Green R. Cavernous sinus thrombosis: current therapy. J Oral Maxillofac Surg. 2012 Sep;70(9):2085-91. doi: 10.1016/j.joms.2011.09.048
- Southwick FS, Richardson EP Jr, Swartz MN. Septic thrombosis of the dural venous sinuses. Medicine (Baltimore). 1986 Mar;65(2):82-106. doi: 10.1097/00005792-198603000-00002
- Canhão P, Cortesão A, Cabral M, Ferro JM, Stam J, Bousser MG, Barinagarrementeria F; ISCVT Investigators. Are steroids useful to treat cerebral venous thrombosis? Stroke. 2008 Jan;39(1):105-10. doi: 10.1161/STROKEAHA.107.484089
- HUNT WE, MEAGHER JN, LEFEVER HE, ZEMAN W. Painful opthalmoplegia. Its relation to indolent inflammation of the carvernous sinus. Neurology. 1961 Jan;11:56-62. doi: 10.1212/wnl.11.1.56
- Zurawski J, Akhondi H. Tolosa-Hunt syndrome–a rare cause of headache and ophthalmoplegia. Lancet. 2013 Sep 7;382(9895):912. doi: 10.1016/S0140-6736(13)61442-7
- Sugano H, Iizuka Y, Arai H, Sato K. Progression of Tolosa-Hunt syndrome to a cavernous dural arteriovenous fistula: a case report. Headache. 2003 Feb;43(2):122-6. doi: 10.1046/j.1526-4610.2003.03029.x
- Smith JR, Rosenbaum JT. A role for methotrexate in the management of non-infectious orbital inflammatory disease. Br J Ophthalmol. 2001 Oct;85(10):1220-4. doi: 10.1136/bjo.85.10.1220
- Halabi T, Sawaya R. Successful Treatment of Tolosa-Hunt Syndrome after a Single Infusion of Infliximab. J Clin Neurol. 2018 Jan;14(1):126-127. doi: 10.3988/jcn.2018.14.1.126