Chondrolysis
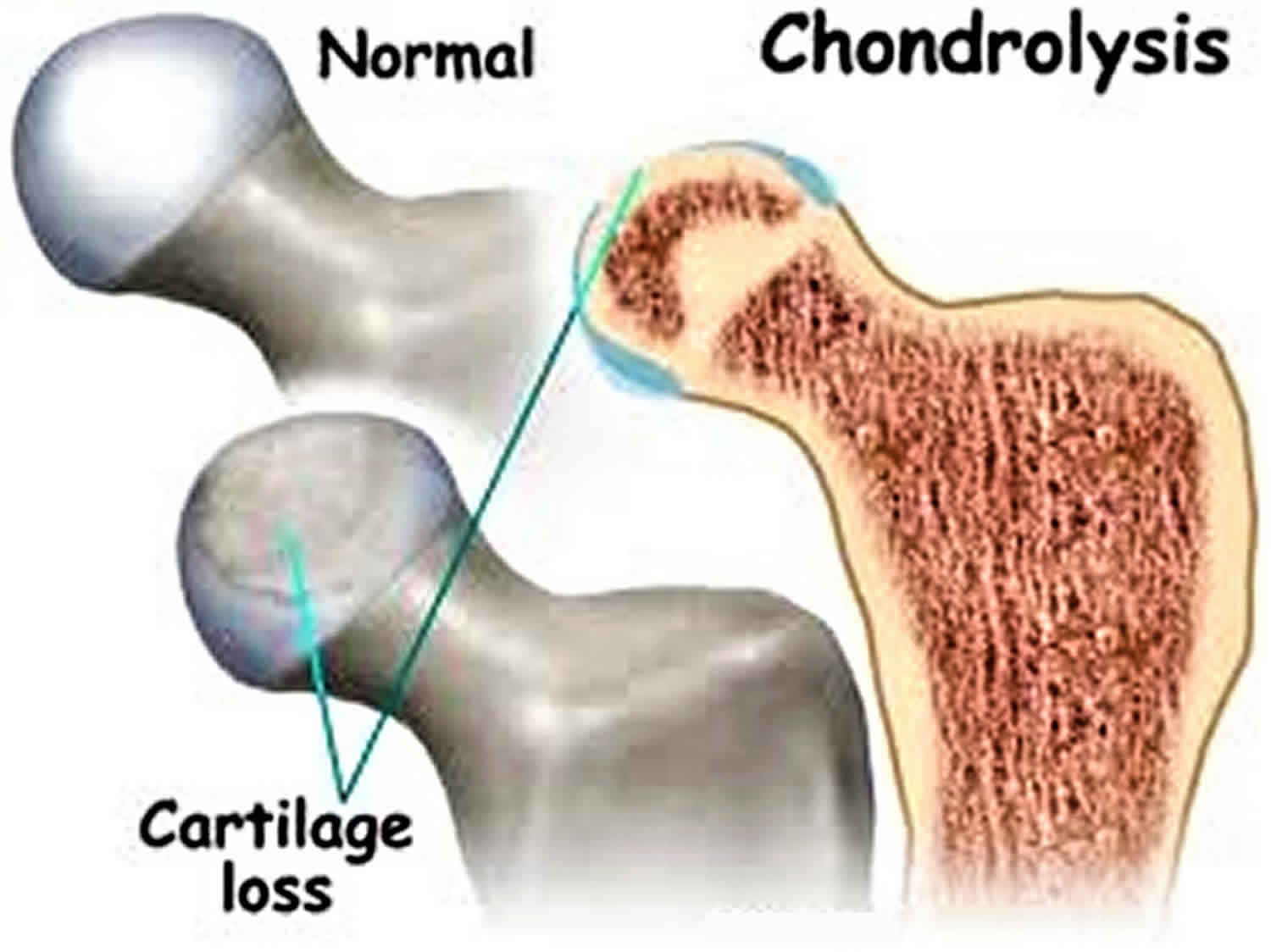
Chondrolysis also known as acute cartilage necrosis, is a rare disease with destruction of cartilage of joints such as hip, knee, ankle, shoulder and elbow 1. Chondrolysis occurs both in children and in adults 2. Chondrolysis has been reported among adolescent females after slipped capital femoral epiphysis 3. Other suggested risk factors include trauma, infections, and prolonged immobilization 4. Chondrolysis may also be associated with infection, specifically septic arthritis.
Chondrolysis is a poorly understood phenomenon. The relevant literature is virtually restricted to case reports and case series 4. The quoted incidence of chondrolysis is 5–7%. But it can be very variable, depending on the treatment options [e.g. percutaneous pinning 5, Spica cast 6]. Females are more likely to be affected than males.
Chondrolysis of the shoulder (glenohumeral chondrolysis) has been reported most frequently among young men 7. Recently, a case series described glenohumeral chondrolysis after shoulder arthroscopy 8, in two and eight cases after arthroscopic thermal capsuorrhaphy 9 and in two patients after color tests using gentian violet in two cases after a color test 10. Use of intra-articular pain pump infusing bupivacaine has also been associated with glenohumeral chondrolysis 11 in case series including 12 cases 12 and 23 cases 13 and in one case with bilateral shoulder arthroscopy in which chondrolysis developed at the side of pain catheter 14.
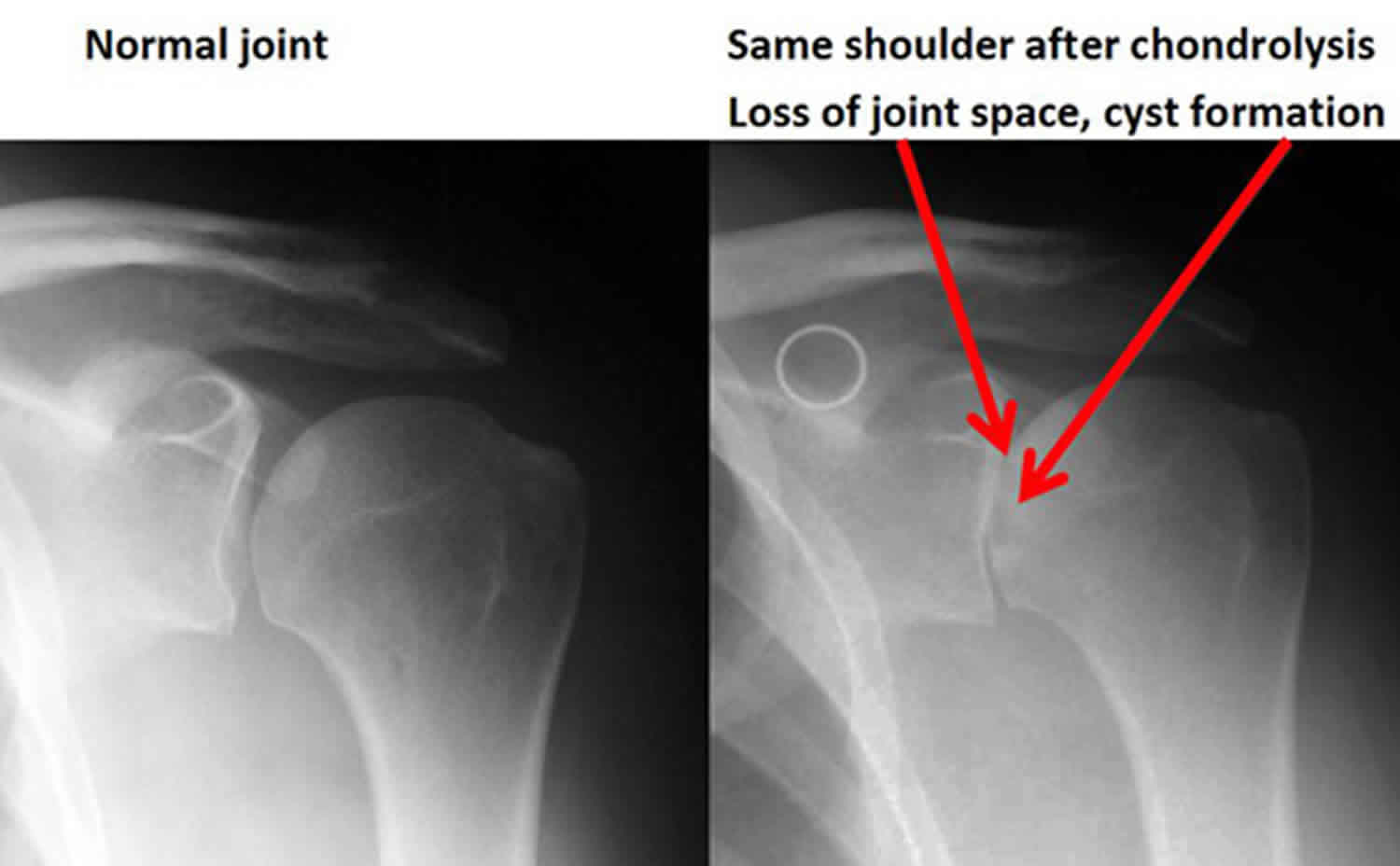
Chondrolysis shoulder
Chondrolysis shoulder also known as glenohumeral chondrolysis is a complication of arthroscopic shoulder surgery characterized by the dissolution of the articular cartilage of the glenoid and the humeral head 15. Chondrolysis is a severe type of shoulder arthritis in which the cartilage of the joint is abruptly lost. It can occur in otherwise healthy shoulders after arthroscopic procedures. Chondrolysis shoulder has been reported in association with intra-articular thermal energy, intra-articular injection of radiopaque contrast medium, and postoperative infusion of a local anesthetic for postoperative pain control (e.g., Bupivacaine [Marcaine] or Lidocaine [Xylocaine]) 16. The inclusion of epinephrine in the infusion may further increase the risk. Of the clinical cases of post-arthroscopic glenohumeral chondrolysis reported to date, approximately 60% have been associated with local anesthetic infusion and approximately 30% have been associated with intra-articular use of radiofrequency energy 15. Shoulder arthroscopy is the second most common procedure performed by those taking Part II of the American Board of Orthopaedic Surgery certification examination 17. Changes seen on radiographic and magnetic resonance imaging (MRI) include joint-space narrowing, periarticular bone edema, subchondral cysts, and a lack of osteophyte formation 18.
Treatment of shoulder chondrolysis may require a ream and run procedure or a total shoulder replacement.
Figure 1. Chondrolysis shoulder
Chondrolysis shoulder symptoms
The onset of shoulder chondrolysis is characteristically marked by unexpected progressive pain and loss of joint motion weeks to months following arthroscopic shoulder surgery 19.
Idiopathic chondrolysis of the hip
Chondrolysis of the hip is characterized by rapidly progressive destruction of the articular cartilage of the femoral head and acetabulum with resultant joint space narrowing and restricted movement 20. Rapid loss of articular cartilage was first described as “acute cartilage necrosis” in the first reported case involving the hip, which was published in 1930 by Waldenstrom 21. The onset is early in the second decade of life with an approximately 6:1 female gender predominance 22. The clinical course is variable. Some hips will progress to end stage arthritis or even spontaneous fusion, whereas others may completely heal 23. In the early stages, the destruction appears to be reversible with conservative treatment focusing on pain relief, traction, physiotherapy, and walking with crutches to alleviate weight bearing. Without treatment the disease terminates in spontaneous fusion which needs surgical intervention. Examination under anesthesia to determine the degree of fixed contractures, physical therapy and continuous use of a passive motion machine, protected weight bearing, and nonsteroidal anti-inflammatory medications have been reported methods of nonoperative management 24. Aggressive surgical release 25 and hinged hip distraction 26 may be needed in recalcitrant cases.
Slipped capital femoral epiphysis 27, severe trauma, prolonged immobilization, infective arthritis, juvenile idiopathic arthritis, and Perthes disease are other known causes of chondrolysis of hip in children 20. In 1971, Jones 28 reported about cases of chondrolysis of the hip, for which no cause could be identified and hence named as idiopathic chondrolysis of the hip. Similar cases were also reported by Duncan et al. 29 and also by Wenger et al. 30 idiopathic chondrolysis of hip is a rare pediatric musculoskeletal disorder mainly seen in Africo-Asian adolescents and young children, predominantly in females, as a painful stiff hip of unknown etiology. Synovial fluid aspirate analysis and synovial biopsy can be performed to rule out inflammatory or infectious causes.
There is no specific diagnostic criteria for idiopathic chondrolysis of hip 4. In clinical practice, the diagnosis is made by exclusion of other more common causes of acute or chronic monoarticular hip pain such as trauma, slipped capital femoral epiphysis, septic arthritis, tuberculosis, Perthes’ disease, pigmented villonodular synovitis, synovioma and monoarticular rheumatoid arthritis. The typical clinical presentation is an adolescent female with insidious onset of hip pain, limping and contracture of the hip joint (most common in flexed, abducted and externally rotated position) 31.
Laboratory values are normal. ESR may be slightly raised 5 (≤30 mm/hr). The radiographic findings are characteristic. The radiological hallmark of this condition has been described as symmetric narrowing of the hip joint space(below than 3 mm), without frank osteophyte formation, in conjunction with periarticular osteopenia 32. A variety of possible radiographic findings without significant pathological related has been reported 32.
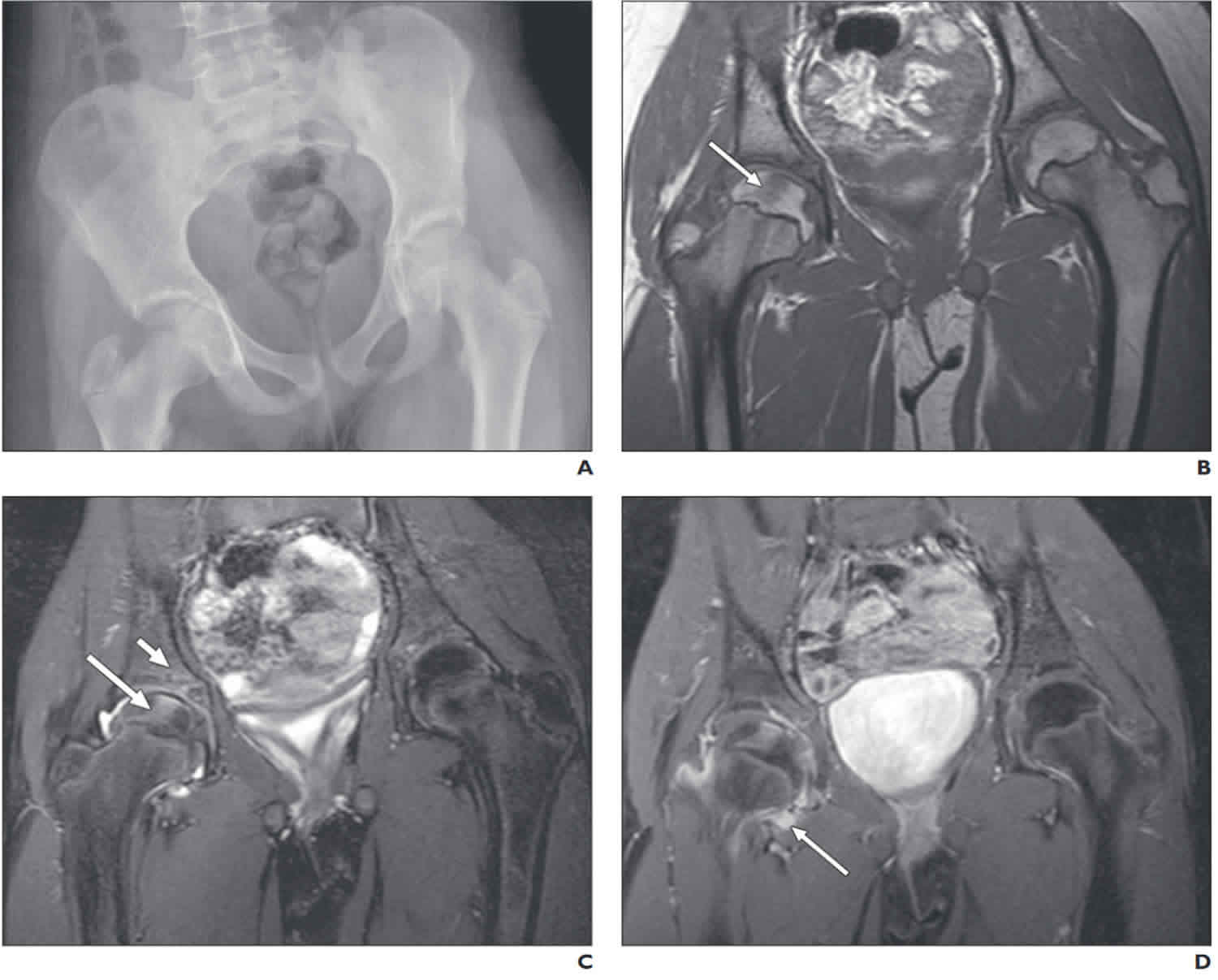
Imaging forms the cornerstone for differential diagnosis. Magnetic resonance imaging (MRI) has a high sensitivity and specificity as a diagnostic tool for early identification of idiopathic chondrolysis of hip 33. In addition to providing early diagnosis, MRI also allows accurate assessment of the course, severity of the disease, helps in staging of the disease process, in the prediction and evaluation of associated complications, in defining the disease, and in the differentiation of idiopathic chondrolysis of hip from other epiphyseal lesions. MRI depicts the exact extent of the femoral head and acetabular involvement more precisely and also does not expose the pediatric patient to the potentially harmful effects of ionizing radiation. MRI can diagnose and clearly differentiate Stages 1 and 2. Stage 3, usually being end-stage hip disease, is very nonspecific.
Radiographs may show normal hip in the early stages, which later show up reduction in hip joint space. As opposed to idiopathic chondrolysis of hip, in infections the hip joint space is usually increased. Monoarticular juvenile rheumatoid arthritis rarely affects the hip, and in the early stages, typically demonstrates a widened joint space with joint effusion, and an increased ESR and C-reactive protein 34. Thus, the radiographic finding of a narrowed hip joint space in patients presenting with hip pain is definitely an important distinction that narrows down the differential diagnosis. The radiographic diagnosis of fractures, neoplasms, slipped capital femoral epiphysis and Legg-Calve-Perthes disease 35 are clearly apparent. Plain X-ray cannot accurately differentiate between Stage 1 and Stage 2; however, it helps in picking up the important finding of joint space narrowing 30 and degenerative changes in the later stages. No criteria are available to classify the severity of joint space narrowing. Isotopic bone scan reveals periarticular increased uptake within the femoral head and acetabulum, which are highly sensitive but not specific 36. CT scan is not useful in the early stages and is associated with added risk of ionizing radiation.
Histological features of idiopathic chondrolysis of hip include thickening of the capsule with edematous changes in the capsule and synovium. There are articular surface changes with fibrillation, fragmentation, and progressive loss of cartilage. An infiltration of lymphocytes is seen within the synovium, and there may be degeneration of chondrocyte nuclei and loss of cells in the lacunae 37.
Figure 2. Chondrolysis of the hip
Footnote: 10-year-4-month-old girl with right hip and leg pain, stif fness, and limp for 2– 3 weeks. (A) Frontal radiograph shows pelvic tilt to right with medial hip joint space narrowing. (B) Coronal T1-weighted image (TR / TE, 800/6.9) of pelvis obtained at 3 T shows geometric focus of abnormal signal intensity (arrow) in middle one third of proximal right femoral epiphysis. (C) Coronal fast spin-echo T2-weighted image (3,000/58) with fat suppression obtained at 3 T shows that same abnormal focus depicted in A now appears with increased signal intensity (long arrow). Minimal abnormal increased signal intensit y is seen in ipsilateral supraacetabular iliac bone (short arrow), just superior to triradiate cartilage. Minimal abnormal increased signal intensity is present within joint. (D) Coronal T1-weighted image (800/6.9) with fat suppression after IV contrast administration. Geographic abnormal signal in right proximal femoral epiphysis shows diffuse enhancement. There is mild synovial hyper trophy (arrow), but very lit tle unenhanced joint fluid
Chondrolysis causes
The cause of chondrolysis still remains unknown. Chondrolysis can occur spontaneously, before any treatment, or may be found when the patient first presents with slipped capital femoral epiphysis. Chondrolysis can also occur after any type of treatment but it is particularly associated with pin joint penetration. Theories include autoimmune process 37 alteration in the synovial nutrition to the articular cartilage, mechanical injury, cartilage dysplasia, ischemia, abnormal intracapsular pressure, and inherent abnormal chondrocyte metabolism 38. The above-mentioned factors usually cause bilateral involvement, whereas idiopathic chondrolysis of hip is predominantly unilateral. Genetic predisposition to idiopathic chondrolysis of hip is a possibility.
Chondrolysis symptoms
Typically, symptoms develop between 2 and 4 months after treatment, but occasionally they are present on the initial presentation before treatment.
Stiffness and persistent pain in the groin or upper thigh are reported. Walking and other activities are adversely affected.
Reduction in the arc of motion of the hip in all planes and motion is usually painful during the hip examination.
Chondrolysis treatment
The natural history of chondrolysis can follow two major courses:
- some children will undergo a late reconstitution of the joint space to a certain degree
- others will undergo nearly complete ankylosis, often in a bad position
The three aims of treatment are pain relief, deformity correction and restoration of motion 32. Therapy for idiopathic chondrolysis remains controversial, and none has been clearly effective 39. The treatments are mainly symptomatic and non-operative. The role of surgery is controversial. Section of tendons and muscles, capsulotomy and subtotal capsulectomy have all been performed with variable success 22. Pain is the symptom that has shown the most improvement after treatment 31.
Conservative treatment includes analgesics and antiinflammatory medications. Load reduction of the hip with passive motion, intermittent traction, or forced ankylosis in a functional position has also been used 39. Surgical therapy, which includes a subtotal capsulectomy with muscle release as needed to relieve joint contracture, followed by aggressive nonweightbearing rangeof motion rehabilitation has been successful in a small cohort of patients 40. All patients in our group underwent a subtotal capsulectomy, muscle release as needed, and aggressive rehabilitation with varying results. To date, three patients in our study have a normal or nearnormal hip joint on radiography, two have moderate space narrowing of the affected side, and one with bilateral chondrolysis underwent total hip replacements.
Regarding treatment, a large study is required to validate the best treatment options for chondrolysis. Even though in early chondrolysis stages results are good, long-term follow-up is needed for assessing the final outcome of the patients. Duration for progression from one stage to another, with and without treatment could not be assessed; however, there is a definite halt in the progression of the chondrolysis in treated patients. Since there is no clinical staging available till today, no correlation is done between clinical and radiological staging.
From assessing all the Stage 3 cases, scientists found that failure to diagnose chondrolysis in early stages can lead to progression of the disease from a stage which is reversible by conservative treatment to an irreversible stage causing damage to the hip joint, flexion contracture of the hip, lumbar lordosis causing difficulty even in standing, which all may need surgical treatment and can result from the progression of the disease. In these later stages, the outcome is poor even after surgery.
References- Christiansen CF, Thygesen SK, Pedersen L. Incidence and risk of chondrolysis in Denmark: A nationwide population-based study. Clin Epidemiol. 2010;2:85–89. Published 2010 Aug 9. doi:10.2147/clep.s10216 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2943176
- Wada Y, Higuchi F, Inoue A. Adult idiopathic chondrolysis of the hip report of 2 cases. Kurume Med J. 1995;42:121–8.
- Ingram AJ, Clarke MS, Clarke CS, Jr, Marshall WR. Chondrolysis complicating slipped capital femoral epiphysis. Clin Orthop Relat Res. 1982;(165):99–109.
- Yarbrough R, Gross R. Chondrolysis: an update. J Pediatr Orthop. 2005;25(5):702–704.
- Kennedy JP, Weiner DS: Results of slipped capital femoral epiphysis in the black population. J Pediatr Orthop 1990; 10:224.
- Meier MC, Meyer LC, Ferguson RL: Treatment of slipped capital femoral epiphysis with a spica cast [see comments]. J Bone Joint Surg Am 1992; 74:1522.
- Solomon DJ, Navaie M, Stedje-Larsen ET, Smith JC, Provencher MT. Glenohumeral chondrolysis after arthroscopy: a systematic review of potential contributors and causal pathways. Arthroscopy. 2009;25(11):1329–1342.
- Petty DH, Jazrawi LM, Estrada LS, Andrews JR. Glenohumeral chondrolysis after shoulder arthroscopy: case reports and review of the literature. Am J Sports Med. 2004;32(2):509–515.
- Good CR, Shindle MK, Kelly BT, Wanich T, Warren RF. Glenohumeral chondrolysis after shoulder arthroscopy with thermal capsulorrhaphy. Arthroscopy. 2007;23(7):797–5.
- Shibata Y, Midorikawa K, Koga T, Honjo N, Naito M. Chondrolysis of the glenohumeral joint following a color test using gentian violet. Int Orthop. 2001;25(6):401–403.
- Busfield BT, Romero DM. Pain pump use after shoulder arthroscopy as a cause of glenohumeral chondrolysis. Arthroscopy. 2009;25(6):647–652.
- Hansen BP, Beck CL, Beck EP, Townsley RW. Postarthroscopic glenohumeral chondrolysis. Am J Sports Med. 2007;35(10):1628–1634.
- Bailie DS, Ellenbecker TS. Severe chondrolysis after shoulder arthroscopy: a case series. J Shoulder Elbow Surg. 2009;18(5):742–747.
- Saltzman M, Mercer D, Bertelsen A, Warme W, Matsen F. Postsurgical chondrolysis of the shoulder. Orthopedics. 2009;32(3):215.
- Risk Factors for Chondrolysis of theGlenohumeral Joint. J Bone Joint Surg Am. 2011;93:1-9. doi:10.2106/JBJS.I.01386 https://orthop.washington.edu/sites/default/files/Portals/21/www/Patient%20Care/Our%20Services/Shoulder%20%26%20Elbow/Articles/PDFs/Risk%20Factors%20for%20Chondrolysis%20of%20the%20Glenohumeral%20Joint.pdf
- Kang RW, Frank RM, Nho SJ, Ghodadra NS, Verma NN, Romeo AA, ProvencherMT. Complications associated with anterior shoulder instability repair. Arthroscopy.2009;25:909-20.
- Garrett WE Jr, Swiontkowski MF, Weinstein JN, Callaghan J, Rosier RN, Berry DJ,Harrast J, Derosa GP. American Board of Orthopaedic Surgery Practice of theOrthopaedic Surgeon: Part-II, certification examination case mix. J Bone Joint SurgAm. 2006;88:660-7.
- Sanders TG, Zlatkin MB, Paruchuri NB, Higgins RW. Chondrolysis of the gleno-humeral joint after arthroscopy: findings on radiography and low-field-strength MRI.AJR Am J Roentgenol. 2007;188:1094-8.
- Scheffel PT, Clinton J, Lynch J, Warme WJ, Matsen FA III. Characteristics ofchondrolysis associated with intra-articular pain-pump after shoulder surgery. Pre-sented at AAOS Annual Meeting; 2009; Las Vegas, NV.
- Amarnath C, Muthaiyan P, Mary TH, Mohanan S, Gopinathan K. Idiopathic chondrolysis of hip in children: New proposal and implication for radiological staging. Indian J Radiol Imaging. 2018;28(2):205–213. doi:10.4103/ijri.IJRI_185_17 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6038227
- Waldenström H. On necrosis of the joint cartilage by epiphyseolysis capitis femoris. Acta Chir Scand. 1930;67:936–46.
- Segaren N, Abdul-Jabar HB, Segaren N, Hashemi-Nejad A. Idiopathic chondrolysis of the hip: presentation, natural history and treatment options. J Pediatr Orthop B. 2014;23:112–116.
- Bleck EE. Idiopathic chondrolysis of the hip.J Bone Joint Surg Am. 1983 Dec;65(9):1266-75.
- Segaren N, Abdul-Jabar HB, Segaren N, Hashemi-Nejad A. Idiopathic chondrolysis of the hip: presentation, natural history, and treatment options. J Pediatr Orthop B. 2014; 23:112-116.
- Roy DR, Crawford AH. Idiopathic chondrolysis of the hip: management by subtotal capsulectomy and aggressive rehabilitation.J Pediatr Orthop. 1988 Mar-Apr;8(2):203-7.
- Thacker MM, Feldman DS, Madan SS, Straight JJ, Scher DM. Hinged distraction of the adolescent arthritic hip. J Pediatr Orthop. 2005 Mar-Apr;25(2):178-82
- Goldman AB, Schneider R, Martel W. Acute chondrolysis complicating slipped capital femoral epiphysis. Am J Roentgenol. 1978;130:945–50.
- Sparks LT, Dall G. Idiopathic chondrolysis of the hip joint in adolescents: Case reports. S Afr Med J. 1982;63:883–6.
- Duncan JW, Schrantz JL, Nasca RJ. The bizarre stiff hip: Possible idiopathic chondrolysis. JAMA. 1975;231:382–5.
- Wenger DR, Mickelson MR, Ponseti IV. Idiopathic chondrolysis of the hip: Report of two cases. J Bone Joint Surg Am. 1975;57:268–71.
- Del Couz Garcia A, Fernandez PL, Gonzalez MP. Idiopathic chondrolysis of the hip: long-term evolution. J Pediatr Orthop. 1999;19(4):449–454.
- Korula RJ, Jebaraj I, David KS. Idiopathic chondrolysis of the hip: medium-to long-term results. ANZ J Surg. 2005;75:750–753.
- Laor T. Idiopathic chondrolysis of the hip in children: Early MRI findings. AJR Am J Roentgenol. 2009;192:526–31.
- Gils-Morin VM, Graham TB, Blebea JS, Dardzinski BJ, Laor T, Johnson ND, et al. Knee in early juvenile rheumatoid arthritis: MR imaging findings. Radiology. 2001;220:696–706.
- Rush BH, Bramson RT, Ogden JA. Legg-Calvé-Perthes disease: Detection of cartilaginous and synovial change with MR imaging. Radiology. 1988;167:473–6.
- Rachinsky I, Boguslavsky L, Cohen E, Hertzanu Y, Lantsberg S. Bilateral idiopathic chondrolysis of the hip: A case report. Clin Nucl Med. 2000;25:1007–9.
- Ippolito E, Bellocci M, Santori FS, Ghera S. Idiopathic chondrolysis of the hip: An ultrastructural study of the articular cartilage of the femoral head. Orthopedics. 1986;9:1383–7.
- François J, Mulier M. Idiopathic chondrolysis of the hip; A case report. Acta Orthop Belg. 2007;73:653–7.
- del Couz Garciá A, Fernández PL, González MP, García AC, González LR, Jiménez JP. Idiopathic chondrolysis of the hip: longterm evolution. J Pe-diatr Orthop 1999; 19:449–454
- Roy DR, Crawford AH. Idiopathic chondrolysis of the hip: management by subtotal capsulectomy and aggressive rehabilitation. J Pediatr Orthop1988; 8:203–207