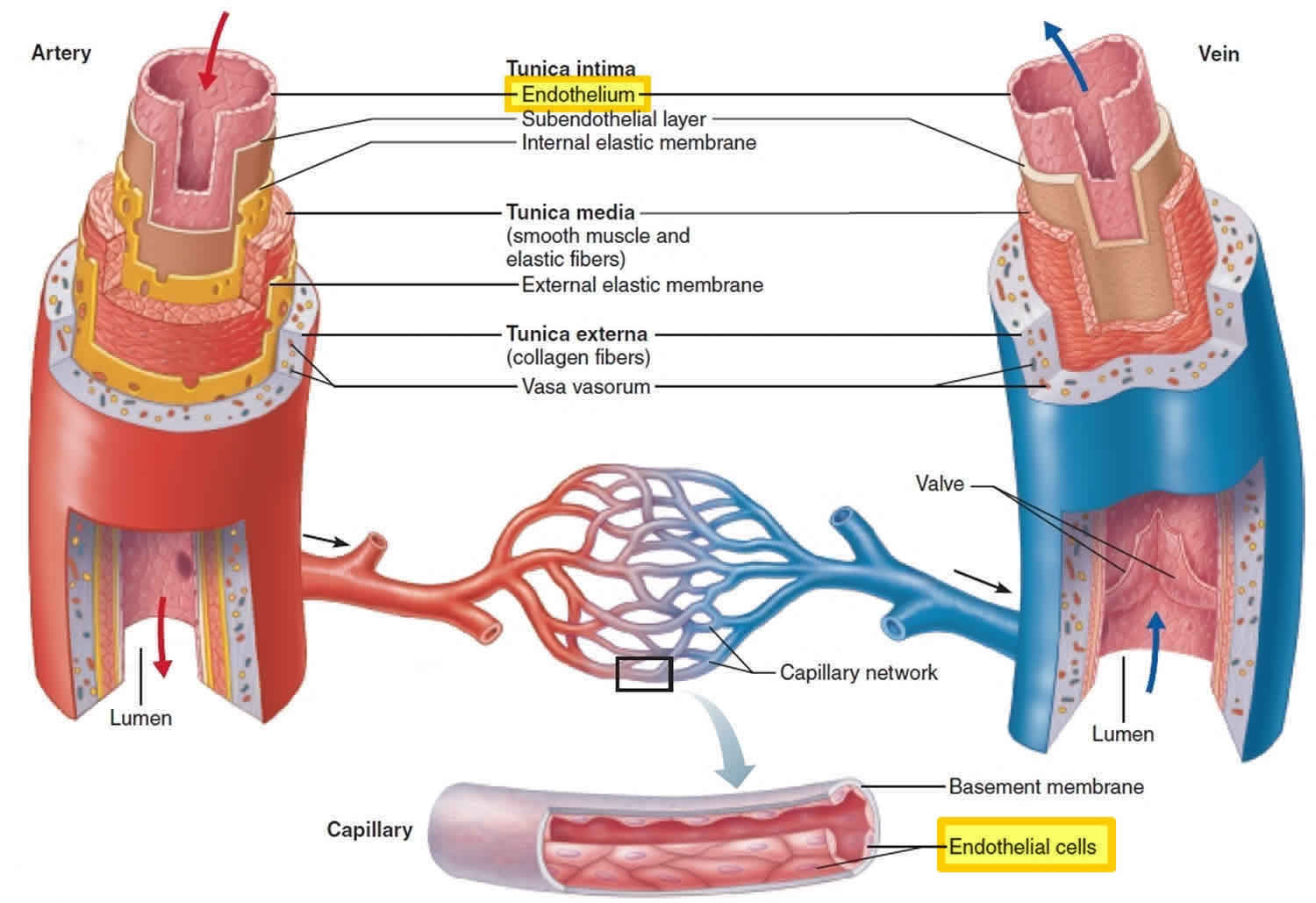
Endothelium
Endothelium is the thin layer of cells that line the interior surface of blood vessels including arteries and veins as well as the innermost lining of the heart and lymphatic vessels, forming an interface between circulating blood in the lumen and the rest of the vessel wall. Endothelial cells line the entire circulatory system, from the heart to the smallest capillary. These cells reduce friction of the flow of blood allowing the fluid to be pumped further.
Endothelial tissue is a specialized type of epithelium tissue (one of the four types of biological tissue in animals). More specifically, it is simple squamous epithelium.
The surface are of endothelial cells in the body is as large as a tennis court. There are a trillion endothelial cells in the body.
Endothelium of the interior surfaces of the heart chambers are called endocardium. Both blood and lymphatic capillaries are composed of a single layer of endothelial cells.
Figure 1. Vascular endothelium
Endothelium function
Endothelial cells are involved in many aspects of vascular biology, including:
- vasoconstriction and vasodilation, and hence the control of blood pressure
- blood clotting (thrombosis and fibrinolysis)
- atherosclerosis
- formation of new blood vessels (angiogenesis)
- inflammation and swelling (edema)
Endothelial cells also control the passage of materials — and the transit of white blood cells — into and out of the bloodstream.
In some organs, there are highly differentiated endothelial cells to perform specialized ‘filtering’ functions. Examples of such unique endothelial structures include the renal glomerulus and the blood-brain barrier.
Endothelial dysfunction
Endothelial dysfunction or the loss of proper endothelial function, is a hallmark for vascular diseases, and often leads to atherosclerosis. This is very common in patients with diabetes mellitus, hypertension or other chronic pathophysiological conditions. One of the main mechanisms of endothelial dysfunction is the diminishing of nitric oxide, often due to high levels of asymmetric dimethylarginine, which interfere with the normal L-arginine-stimulated nitric oxide synthesis.
Normal functions of endothelial cells include mediation of coagulation, platelet adhesion, immune function, control of volume and electrolyte content of the intravascular and extravascular spaces. Endothelial dysfunction can result from disease processes, as occurs in septic shock, hypertension, hypercholesterolaemia, diabetes as well as from environmental factors, such as from smoking tobacco products.
Endothelial dysfunction is thought to be a key event in the development of atherosclerosis and predates clinically obvious vascular pathology by many years. Endothelial dysfunction has also been shown to be of prognostic significance in predicting vascular events including stroke and heart attacks.
A key feature of endothelial dysfunction is the inability of arteries and arterioles to dilate fully in response to an appropriate stimulus. This can be tested by a variety of methods including iontophoresis of acetylcholine, intra-arterial administration of various vasoactive agents, localised heating of the skin and temporary arterial occlusion by inflating a blood pressure cuff to high pressures. Testing can also take place in the coronary arteries themselves but this is invasive and not normally conducted unless there is a clinal reason for intracoronary catheterisation. These techniques are thought to stimulate the endothelium to release nitric oxide (NO) and possibly some other agents, which diffuse into the surrounding vascular smooth muscle causing vasodilation.
Dysfunctional endothelial cells are unable to produce NO to the same extent (or there is increased and rapid destruction of NO) as healthy endothelial cells and therefore vasodilatation is reduced. This creates a detectable difference in subjects with endothelial dysfunction verses a normal, healthy endothelium.
Unfortunately the variability in such tests means that no technique has yet been identified that would allow endothelial testing to attain routine clinical significance.
Endothelial function can be improved significantly by exercise and improved diet. A study published in 2005 has determined that a positive relationship exists between the consumption of trans fat (commonly found in hydrogenated products such as margarine) and the development of endothelial dysfunction 1. Other factors have been identified as improving endothelial function and include cessation of smoking, loss of weight and treatment of hypertension and hypercholesterolemia amongst other things.
Endothelial dysfunction has been observed in a 2001 study of women where it was found that this disorder is present in approximately half of women with chest pain, in the absence of overt blockages in large coronary arteries 2. This endothelial dysfunction cannot be predicted by typical risk factors for atherosclerosis (e.g., obesity, cholesterol, smoking) and hormones.
References- Lopez-Garcia E, Schulze MB, Meigs JB, Manson JE, Rifai N, Stampfer MJ, Willett WC, Hu FB, “Consumption of trans fatty acids is related to plasma biomarkers of inflammation and endothelial dysfunction”, Journal of Nutrition, Mar 2005;135(3):562-6.
- Reis SE, Holubkov R, Smith AJC, Kelsey SF, Sharaf BL, Reichek N, Rogers WJ, Merz NB, Sopko G, Pepine CJ, “Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: Results from the NHLBI WISE Study,” Am Heart J, V. 141, No. 5 (May 2001), pp. 735-741