Eosinophilic folliculitis
Eosinophilic folliculitis also known as eosinophilic pustular folliculitis or Ofuji disease, is a rare, recurrent skin disorder of unknown cause that is characterized by red or skin-colored bumps (folliculocentric papules), pustules (bumps containing pus) or plaques affecting the head, trunk, and extremities 1. Eosinophilic folliculitis is named after the fact that skin biopsies of this disorder find eosinophils (a type of immune cell) around hair follicles. The papules (skin bumps) mostly appear on the face, scalp, neck and trunk and may persist for weeks or months. Eosinophilic folliculitis affects males more than females 2. Eosinophilic folliculitis comprises 5 subtypes: classic eosinophilic pustular folliculitis (mainly occurring in adults in Japan); infantile eosinophilic pustular folliculitis (with onset from birth or within the first year of life); HIV-associated eosinophilic folliculitis also referred to as immunosuppression-associated eosinophilic pustular folliculitis; blood cancer–associated eosinophilic folliculitis 1 and medication-associated eosinophilic pustular folliculitis 3. All of them present with itchy papules or pustules. Whether these are distinct disorders rather than variants of one disorder is controversial, partly because the underlying cause of eosinophilic folliculitis is not known 2.
Eosinophilic folliculitis can be confused with insect bite reaction, bacterial folliculitis, folliculotropic mycosis fungoides (a form of of cutaneous T-cell lymphoma that involves hair follicles) and leukemia cutis 1.
Several treatments have been described with variable results, including various oral or topical medications and phototherapy. In patients with HIV-associated eosinophilic pustular folliculitis, antiretroviral therapy tends to greatly diminish symptoms or even eliminate the condition.
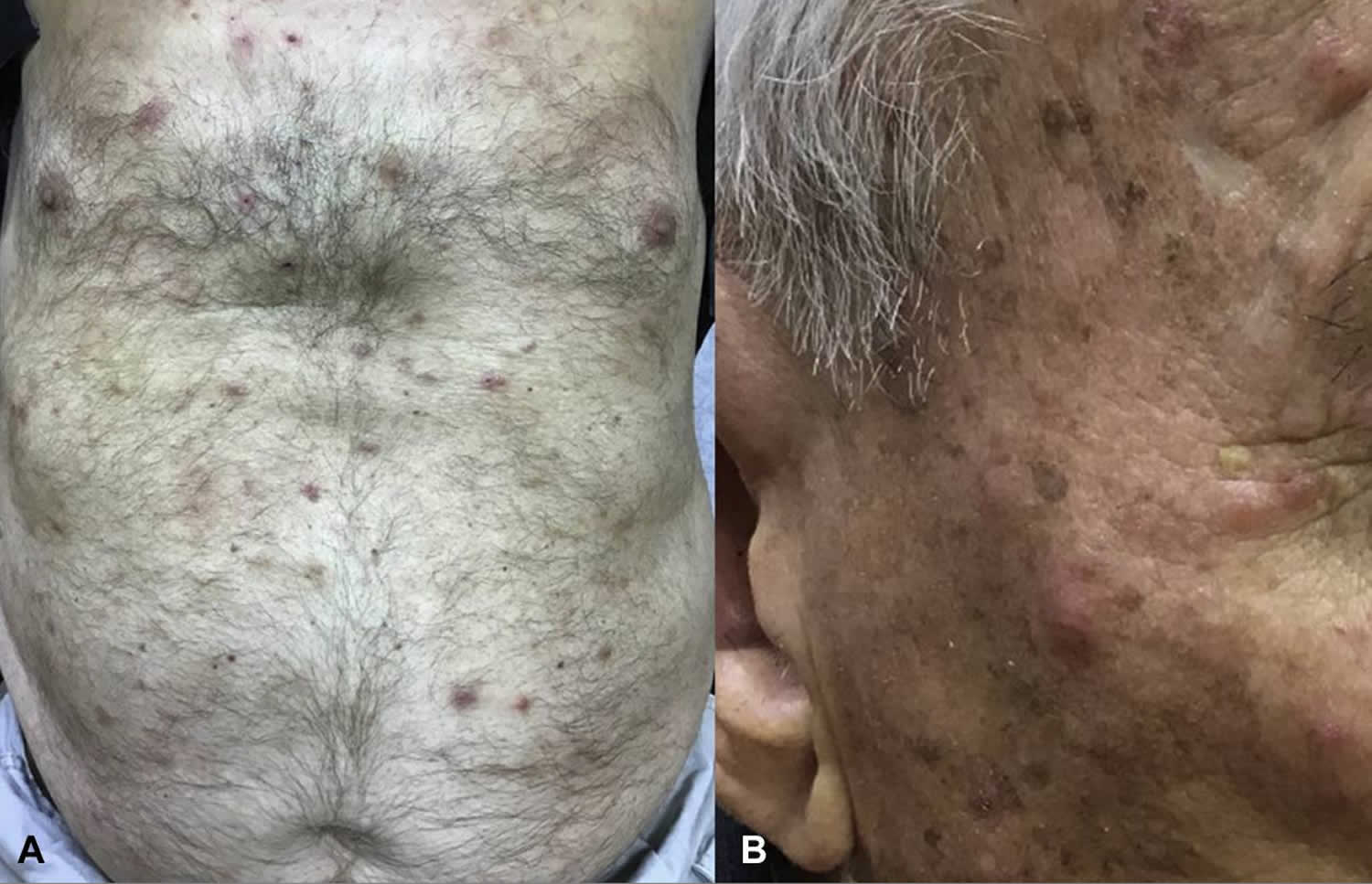
Figure 1. Eosinophilic folliculitis
Footnote: Excoriated papules and nodules on the chest and abdomen (A) and cheek (B).
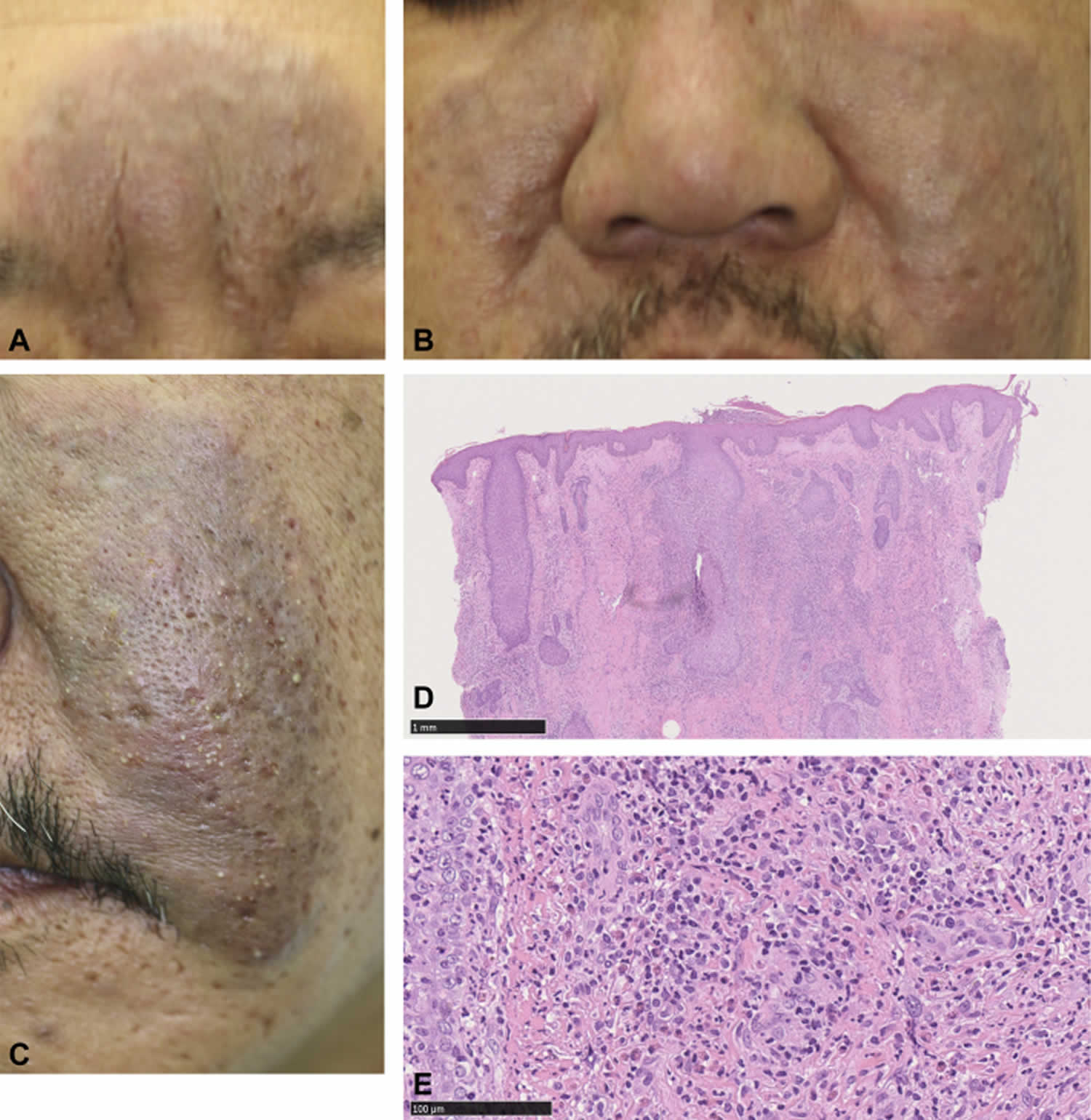
[Source 1 ]Figure 2. Eosinophilic pustular folliculitis
Footnote: (A-C) Eosinophilic pustular folliculitis: clinical features of the lesion. (A and B) At the initial presentation, well-defined erythematous, indurated plaques involving the nose, forehead (A), and the cheeks bilaterally (B) were seen. (C) The plaques had numerous pustules and crusts. (D and E) Eosinophilic pustular folliculitis: histopathologic features of the initial biopsy. (D) Epidermis is intact, and dense infiltration of inflammatory cells within and around the follicules can be seen. (E) Inflammatory cells are composed of lymphocytes, histiocytes and eosinophils. (D and E, Hematoxylin-eosin stain)
[Source 4 ]Does eosinophilic pustular folliculitis weaken the immune system?
Based on current knowledge, eosinophilic pustular folliculitis or eosinophilic folliculitis does not weaken the immune system. On the contrary, the development of eosinophilic folliculitis may indicate that a person’s immune system is compromised. However, eosinophilic folliculitis is also seen in people with apparently normal immune status 5.
Eosinophilic folliculitis causes
The cause of eosinophilic pustular folliculitis is unknown. The pathogenesis underlying eosinophilic folliculitis is likely immune dysregulation in response to a follicular antigen, with subsequent production of cytokines, chemotactic factors, and expression of intercellular adhesion molecules 1. In association with B-cell neoplasms, clonal expansion of T helper 2 cells with interleukin-5 production leads to recruitment of eosinophils 6. There is no proof that bacterial, fungal or viral secondary infection is the cause, although some researchers have postulated overgrowth of Malassezia or Demodex (the hair follicle mite) might be involved. Hypersensitivity to Demodex (the hair follicle mite) may also be contributory. In certain patients, a combination of Pityrosporum species and Demodex species might play a role in the pathogenesis of eosinophilic folliculitis. An aberrant helper T-cell type 2 immune response to a follicular antigen, such as Demodex, might be involved in the pathogenesis of HIV-associated eosinophilic pustular folliculitis. Eosinophilic pustular folliculitis has been described in atopic children 7 with hypersensitivity to Dermatophagoides pteronyssinus. Some authorities have suggested that patients with eosinophilic pustular folliculitis shoud be screened for the presence of coexisting T helper 2-mediated disorders 8.
The cause of eosinophilic pustular folliculitis of HIV is not known. Immunodeficiency appears to lead to increased risk of allergic-type skin diseases. An anaerobic organism similar in morphology to Leptotrichia buccalis has been found in one biopsy specimen of a patient with HIV-associated eosinophilic folliculitis; the disease responded to oral metronidazole. Others believe that at least the HIV-associated eosinophilic folliculitis is an autoimmune disorder with the sebaceous gland cell or a constituent of sebum serving as an autoantigen. Another theory is that there is a change in the immune system causing eosinophils to attack the sebum produced by sebaceous gland cells.
Reports have described Asian patients in whom eosinophilic pustular folliculitis seemed to be associated with silicone tissue augmentation 9 or autologous peripheral blood stem cell transplantation 10.
A middle-aged Japanese woman has been described in whom eosinophilic pustular folliculitis was induced by a combination of allopurinol and timepidium bromide as suggested by the results of an oral provocation test with both drugs 11. Moreover, allopurinol alone seemed to induce generalized eosinophilic pustular folliculitis 12.
Eosinophilic pustular folliculitis associated with pregnancy has been described 13.
A middle-aged man with eosinophilic pustular folliculitis apparently associated with hepatitis C virus infection has also been reported 8.
Hyperimmunoglobulin E syndrome may be evident as eosinophilic pustular folliculitis 14. Other additional linkages of eosinophilic pustular folliculitis besides HIV infection include the Sézary syndrome and cutaneous angiosarcoma 15.
Atypical eosinophilic pustular folliculitis was linked with use of the antimetabolite capecitabine 16.
Is eosinophilic pustular folliculitis an autoimmune disorder or an allergic disorder?
Because the underlying cause of eosinophilic pustular folliculitis or eosinophilic folliculitis is not known and its nature is poorly understood, it is difficult to categorize the condition. Eosinophilic folliculitis has not been described specifically as an autoimmune disease or an allergic disorder. Several journal articles have described eosinophilic folliculitis more broadly as an “inflammatory” disorder 17. While some inflammatory disorders are also autoimmune disorders, others are not. When the cause of eosinophilic folliculitis is better understood, researchers may be able to better categorize the condition.
That being said, many researchers do suspect that the immune system plays a key role in developing the condition. A growing number of reports on eosinophilic folliculitis in people with weakened immune systems indicates the contribution of a disturbed immune system 18. It has been suggested that in both children and adults, eosinophilic folliculitis should be viewed as a possible cutaneous (skin) sign of immunosuppression. In contrast to autoimmunity (when the body mistakenly attacks healthy cells), immunosuppression makes the immune system less able to detect and destroy infections. However, eosinophilic folliculitis is also seen in people with normal immune status 5.
Proposed triggers or causes of eosinophilic folliculitis have included:
- an exaggerated reaction to dermatophytes (skin fungi) or saprophytic fungi, in association with a disordered immune system. This theory is supported by the effectiveness of oral itraconazole therapy in some people with eosinophilic folliculitis.
- demodex, a mite that lives in the hair follicle, as a possible trigger
- a combination of Pityrosporum (yeast) and demodex
- a change in the immune system causing eosinophils to attack the sebum (oils produced in the skin) of sebaceous gland cells 19.
Eosinophilic folliculitis symptoms
Eosinophilic pustular folliculitis presents with itchy red or skin-colored dome-shaped papules and pustules. It may look like acne or other forms of folliculitis. The papules mostly appear on the face, scalp, neck and trunk and may persist for weeks or months. Less commonly, urticarial lesions are seen (these are larger red irritable weal-like patches similar to urticaria). Palms and soles may rarely develop similar papules and pustules, but in such cases, the condition should not be called folliculitis, as there are no follicles in these areas.
Longstanding cases may develop dermatitis or a form of prurigo, presumably because of the itching and scratching.
Patients with the classic eosinophilic pustular folliculitis have chronically recurrent crops of sterile follicular papulopustules with peripheral extension and central clearing 20. Small papules tend to enlarge and coalesce into large plaques 21.
Papulopustules with or without plaques tend to favor the face and the trunk (Figures 1 and 2), although the extremities may also be involved. With the classic eosinophilic folliculitis, the palms and the soles may also be affected. In children, the scalp, particularly at the vertex, is most frequently involved.
Some patients may have features of coexistent eosinophilic folliculitis and eosinophilic lymphoid granuloma (Kimura disease) 22.
Individual papulopustules may be larger in the classic form, up to 20-50 mm in diameter, rather than the 1-3 mm in diameter seen in patients with HIV disease and in infants; peripheral extension with central clearing may be much less frequent in these 2 forms than in the classic one, which often has an erythematous base. The latter tends to heal more commonly with postinflammatory hyperpigmentation.
No systemic involvement is evident, although a peripheral leukocytosis and eosinophilia may be seen. Atypical features, such as nonfollicular papules and urticarial plaques, are often evident in patients with HIV disease and in infants.
Eosinophilic folliculitis diagnosis
Skin biopsy reveals eosinophils under the skin surface and around the hair follicles and sebaceous glands. In many cases, blood tests show a mild rise in eosinophil cells and immunoglobulin-E (IgE), and reduced IgG and IgA levels.
Eosinophilic pustular folliculitis is often a feature of immunodeficiency. Eosinophilic pustular folliculitis associated with HIV infection presents when levels of CD4 lymphocyte cells drop below 300 cells/mm³, a level at which there is an increased risk of a secondary opportunistic infection. Cases of eosinophilic pustular folliculitis have also reported after bone marrow transplantation before the immune system is back to normal functioning, and in some individuals with inherited immune deficiencies.
Eosinophilic folliculitis treatment
A variety of treatment options for eosinophilic pustular folliculitis have been described with variable results. Individualized therapy should be tailored to the type of eosinophilic folliculitis present.
The effectiveness of oral non-steroidal anti-inflammatory drugs (NSAIDs) is well established for many cases of classic eosinophilic folliculitis (more than 70%), but the reason why remains unknown. There are cases in which NSAIDs are not effective. For cases of classic eosinophilic folliculitis, common NSAID options for treatment include indomethacin (orally or topically) and acemetacin. Naproxen has also been used with some success. For classic cases that are not responsive to NSAIDs, other treatment options include:
- Dapsone
- Topical and systemic steroids
- Isotretinoin and acitretin
- Itraconazole
- Permethrin cream (topical insecticide)
- Interferon
- Tetracycline antibiotics
- Other antibiotics including metronidazole
- Oral antihistamines such as cetirizine
Additional treatment options that may improve symptoms include:
- narrowband UVB phototherapy
- ultraviolet therapy with ultraviolet B or with ultraviolet A
- Psoralen plus ultraviolet A (PUVA)
- Calcineurin inhibitors such as tacrolimus ointment
- Colchicine
- Transdermal nicotine patches
The infantile eosinophilic folliculitis tends to respond well to topical corticosteroid therapy. It is important to recognize that infantile eosinophilic folliculitis typically resolves on it’s own before age 3 in over 80% of cases, so observation or avoiding aggressive treatment is often recommended.
In patients with HIV, eosinophilic pustular folliculitis is likely to improve or resolve with HAART (Highly Active Anti-Retroviral Treatment), as CD4 cell counts rise above 250/mm³. One may use topical itraconazole cream first in patients with HIV-associated eosinophilic folliculitis, adding an oral sedating antihistamine for bedtime use if pruritus is severe. Cetirizine seems to be a favorite because of its preferential effect on eosinophils, with some preferring 4 mg of cyproheptadine at bedtime 23. Some patients with HIV-associated eosinophilic pustular folliculitis may respond to oral metronidazole.
In classic eosinophilic folliculitis, common options for treatment include indomethacin (orally or topically) 24 and its newer derivative acemetacin 25, dapsone, topical and systemic steroids, isotretinoin, itraconazole, permethrin, interferon, and antibiotics 26. The experience of Japanese dermatologists is that indomethacin is by far the most effective in the classic form, although the mode of its action in eosinophilic folliculitis is still poorly understood 27. A multivariable analysis showed that females were more likely than males to exhibit a complete response to oral indomethacin 28. Naproxen has also been used with some success 29.
Narrowband UVB phototherapy may be effective 30. Ultraviolet therapy with ultraviolet B or with ultraviolet A and psoralen plus ultraviolet A may be beneficial 31.
Eosinophilic folliculitis prognosis
The long-term outlook (prognosis) for people with eosinophilic pustular folliculitis depends on the type of eosinophilic folliculitis present (classic, infantile, or immunosuppression-associated eosinophilic folliculitis).
Unfortunately, the classic/Japanese eosinophilic folliculitis usually continues for years with recurrent relapses and remissions. Individual lesions typically last more than 1-2 weeks, and relapse every 3-4 weeks. Except for skin involvement, people with classic eosinophilic folliculitis are generally in good health with no systemic symptoms. Some patients have achieved long-lasting remissions with indomethacin alone or in combination with dapsone.
Infantile eosinophilic folliculitis of the scalp in infancy/childhood generally also runs a benign course, and resolves on its own by 3 years of age in over 80% of cases. It is important to recognize that this form is self-limiting so as to avoid unnecessary aggressive treatment in affected infants. Children with this form also generally remain in good health without associated problems, although a possible association with atopy (tendency to develop allergies) has been speculated. Dermatosis that can be relieved by topical corticosteroids.
The immunosuppression-associated type of eosinophilic folliculitis is mainly associated with HIV infection, hematological malignancy (blood cancers), or other cancers, so recognizing that a person has this form of eosinophilic folliculitis is important. The overall prognosis beyond the skin symptoms largely depends on the prognosis associated with the underlying condition 17.
The main morbidity is chronic persistent pruritus, which, especially in the HIV-related eosinophilic folliculitis, can interfere with activities of daily living.
Patients with HIV-associated disease may benefit from highly active antiretroviral therapy. Treatment that restores immunity in individuals with HIV infection may clear their skin lesions, which otherwise are chronic and persistent. In the absence of improvement of the underlying immunodeficiency, HIV-associated eosinophilic folliculitis usually does not respond to any treatment; even with ultraviolet B and psoralen plus ultraviolet A phototherapy, the skin lesions recur on discontinuation of phototherapy.
References- Oum P, Satcher KG, Braswell D, Montañez-Wiscovich ME, Motaparthi K. Eosinophilic folliculitis in a patient with chronic myelomonocytic leukemia. JAAD Case Rep. 2019;5(8):656–659. Published 2019 Jul 31. doi:10.1016/j.jdcr.2019.05.021 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6677864
- Eosinophilic Pustular Folliculitis. https://emedicine.medscape.com/article/1070326-overview
- Eosinophilic pustular folliculitis. https://www.dermnetnz.org/topics/eosinophilic-pustular-folliculitis/
- Kinoshita Y, Kono T, Ansai SI, Saeki H. An aggressive case of granulomatous eosinophilic pustular folliculitis on the face. JAAD Case Rep. 2019;5(3):237–239. Published 2019 Feb 22. doi:10.1016/j.jdcr.2019.01.002 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6389553
- Nervi SJ, Schwartz RA, Dmochowski M. Eosinophilic pustular folliculitis: a 40 year retrospect. J Am Acad Dermatol. August, 2006; 55(2):285-289.
- Meiss F., Technau-Hafsi K., Kern J.S., May A.M. Eosinophilic dermatosis of hematologic malignancy: correlation of molecular characteristics of skin lesions and extracutaneous manifestations of hematologic malignancy. J Cutan Pathol. 2019;46(3):175–181.
- Boone M, Dangoisse C, André J, Sass U, Song M, Ledoux M. Eosinophilic pustular folliculitis in three atopic children with hypersensitivity to Dermatophagoides pteronyssinus. Dermatology. 1995. 190(2):164-8.
- Gul U, Kilic A, Demiriz M. Eosinophilic pustular folliculitis: the first case associated with hepatitis C virus. J Dermatol. 2007 Jun. 34(6):397-9.
- Wong TW, Tsai YM, Lee JY, Hsu ST, Sheu HM. Eosinophilic pustular folliculitis (Ofuji’s disease) in a patient with silicone tissue augmentation. J Dermatol. 2004 Sep. 31(9):727-30.
- Keida T, Hayashi N, Kawashima M. Eosinophilic pustular folliculitis following autologous peripheral blood stem-cell transplantation. J Dermatol. 2004 Jan. 31(1):21-6.
- Maejima H, Mukai H, Hikaru E. Eosinophilic pustular folliculitis induced by allopurinol and timepidium bromide. Acta Derm Venereol. 2002. 82(4):316-7.
- Ooi CG, Walker P, Sidhu SK, Gordon LA, Marshman G. Allopurinol induced generalized eosinophilic pustular folliculitis. Australas J Dermatol. 2006 Nov. 47(4):270-3.
- Matsudate Y, Miyaoka Y, Urano Y. Two cases of eosinophilic pustular folliculitis associated with pregnancy. J Dermatol. 2016 Feb. 43 (2):218-9.
- Lo CS, Yang CY, Ko JH, Lee WY, Shih IH, Lin YC. Hyperimmunoglobulin E syndrome presenting as eosinophilic pustular folliculitis: a case report. Int J Dermatol. 2015 Feb. 54(2):211-4.
- Jiang YY, Zeng YP, Jin HZ. Eosinophilic Pustular Folliculitis Associated with Cutaneous Angiosarcoma. Chin Med J (Engl). 2018 Jan 5. 131 (1):115-116.
- Takeuchi A, Nomura T, Kaku Y, Egawa G, Kabashima K. A case of atypical eosinophilic pustular folliculitis that emerged following the administration of capecitabine. J Eur Acad Dermatol Venereol. 2018 Feb 14.
- Hai Long, Guiying Zhang, Ling Wang, Qianjin Lu. Eosinophilic Skin Diseases: A Comprehensive Review. Clinical Reviews in Allergy & Immunology. April, 2016; 50(2):189-213.
- Katoh M, Nomura T, Miyachi Y, Kabashima K. Eosinophilic pustular folliculitis: a review of the Japanese published works. J Dermatol. January, 2013; 40(1):15-20.
- Eosinophilic pustular folliculitis. https://www.dermnetnz.org/topics/eosinophilic-pustular-folliculitis
- Kostler E, Gossrau G, Kuster P, Bergner V, Seebacher C. [Sterile eosinophilic pustulosis (Ofuji). A rare entity in Europe]. Hautarzt. 1995 Sep. 46(9):643-6.
- Kinoshita Y, Kono T, Ansai SI, Saeki H. An aggressive case of granulomatous eosinophilic pustular folliculitis on the face. JAAD Case Rep. 2019 Mar. 5 (3):237-239.
- Kudejko J, Jablonska S, Chorzelski T. [Cutaneous changes combining features of Kimura’s disease and Ofuji’s disease (folliculitis pustulosa eosinophilica). A new disease entity?]. Przegl Dermatol. 1981 Jul-Aug. 68(4):487-95.
- Odyakmaz Demirsoy E, Demirsoy U, Ozod U, Kiran R. Eosinophilic pustular folliculitis of infancy suppressed with cetirizine. Pediatr Dermatol. 2019 Feb 21.
- Lee ML, Tham SN, Ng SK. Eosinophilic pustular folliculitis (Ofuji’s disease) with response to indomethacin. Dermatology. 1993. 186(3):210-2.
- Nishijima S, Sugiyama T, Nakagawa M, Odaka T, Takaishi K. Two cases of eosinophilic pustular folliculitis treated by acemetacin. J Dermatol. 1994 Oct. 21(10):779-82.
- Brazzelli V, Barbagallo T, Prestinari F, Ciocca O, Vassallo C, Borroni G. HIV seronegative eosinophilic pustular folliculitis successfully treated with doxicycline. J Eur Acad Dermatol Venereol. 2004 Jul. 18(4):467-70.
- Hashizume S, Ansai S, Kosaka M, Kawana S. Infantile case of eosinophilic pustular folliculitis successfully treated with topical indomethacin. J Dermatol. 2014 Feb. 41(2):196-7.
- Yamamoto Y, Nomura T, Kabashima K, Miyachi Y. Clinical epidemiology of eosinophilic pustular folliculitis: results from a nationwide survey in Japan. Dermatology. 2015. 230(1):87-92.
- Jin SP, Park SY, Yeom KB, Kim YC, Cho KH. Eosinophilic pustular folliculitis involving labial mucosa, which improved with naproxen. Ann Dermatol. 2013 Feb. 25(1):120-2.
- Lim HL, Chong WS. Recalcitrant eosinophilic pustular folliculitis of Ofuji with palmoplantar pustulosis: dramatic response to narrowband UVB phototherapy. Photodermatol Photoimmunol Photomed. 2012 Aug. 28(4):219-21.
- Lim HW, Vallurupalli S, Meola T, Soter NA. UVB phototherapy is an effective treatment for pruritus in patients infected with HIV. J Am Acad Dermatol. 1997 Sep. 37(3 Pt 1):414-7.