Exercise intolerance
Exercise intolerance is defined as the reduced ability to perform activities involving dynamic movement because of symptoms of dyspnea or fatigue, is the most common clinical symptom among patients with heart failure 1. Exercise intolerance is defined as the primary symptom of chronic diastolic heart failure 2. Exercise intolerance was defined as a peak exercise capacity of 7 metabolic equivalents (METs) or less 3. Exercise intolerance is part of the definition of heart failure and is intimately linked to its pathophysiology. Furthermore, exercise intolerance affects the diagnosis and prognosis of heart failure. In addition, understanding the mechanisms of exercise intolerance can lead to developing and testing rationale treatments for heart failure.
Heart failure is a very common condition. About 5.7 million people in the United States have heart failure. Both children and adults can have the condition, although the symptoms and treatments differ. Currently, heart failure has no cure. However, treatments—such as treating the underlying cause of your heart failure, medicines, and lifestyle changes—can help people who have the condition live longer and more active lives. Heart transplantation if other treatments fail.
Not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing sodium in your diet, managing stress and losing weight — can improve your quality of life. Researchers continue to study new ways to treat heart failure and its complications.
One way to prevent heart failure is to prevent and control conditions that cause heart failure, such as coronary artery disease, high blood pressure, diabetes or obesity.
The weakening of the heart’s pumping ability causes:
- Blood and fluid to back up into the lungs
- The buildup of fluid in the feet, ankles and legs – called edema
- Tiredness and shortness of breath
Heart failure develops over time as the heart’s pumping action grows weaker. The condition can affect the right side of the heart only, or it can affect both sides of the heart. Most cases involve both sides of the heart.
Right-side heart failure occurs if the heart can’t pump enough blood to the lungs to pick up oxygen. Left-side heart failure occurs if the heart can’t pump enough oxygen-rich blood to the rest of the body.
Right-side heart failure may cause fluid to build up in the feet, ankles, legs, liver, abdomen, and the veins in the neck. Right-side and left-side heart failure also may cause shortness of breath and fatigue (tiredness).
Exercise intolerance can be objectively quantified using semiquantitative assessments, such as interview (New York Heart Association classification) and surveys (Minnesota Living with Heart Failure or Kansas City Cardiomyopathy questionnaires), and quantitative methods, including timed walking tests (6 minute walk distance) and graded exercise treadmill or bicycle exercise tests 4. Cardiopulmonary exercise testing on a treadmill or a bicycle ergometer provides the most accurate, reliable, and reproducible assessments of exercise tolerance, and yields multiple important outcomes, including metabolic equivalents (METS), exercise time, exercise workload, blood pressure and heart rate responses, and rate-pressure product. Using commercially available instruments that perform automated expired gas analysis, for both concentration and volume, one can assess at both rest and during exercise, simultaneous measures of oxygen consumption (VO2), carbon dioxide generation, and ventilatory response. Patient effort is an important modifier of data quality, and can itself be assessed simultaneously and objectively by expired gas analysis as the respiratory exchange ratio, and by the somewhat subjective but more easily obtained measures of perceived effort by the Borg scale and percent age-predicted maximal heart rate.
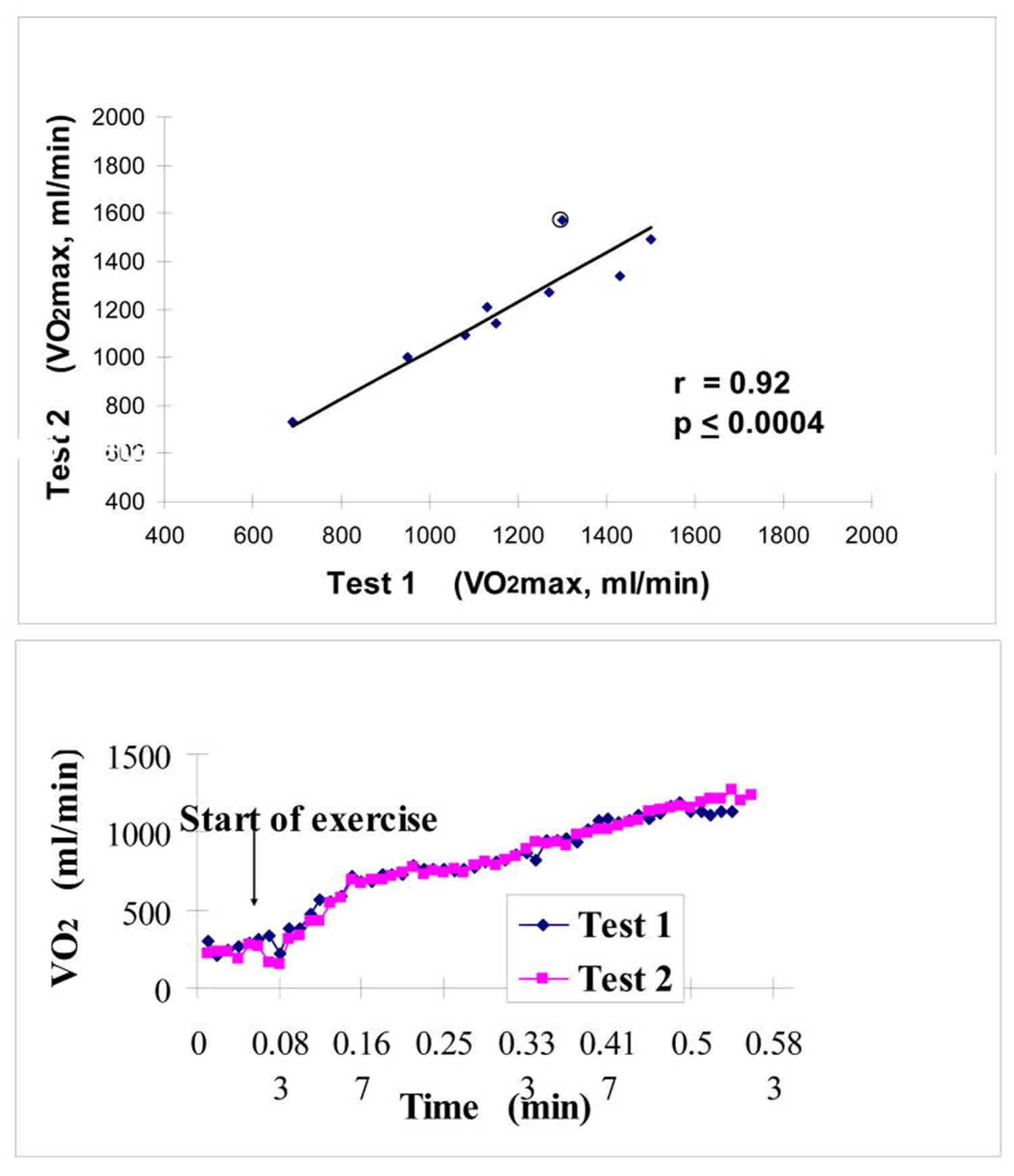
Submaximal exercise is in some ways a more important outcome variable than peak exercise capacity because it is more applicable to everyday life and is relatively effort independent. Submaximal exercise capacity can be assessed as the ventilatory anaerobic threshold by expired gas analysis, using either the Wasserman-Whipp or the V-slope method. Cardiopulmonary exercise testing measurements and expired gas analysis with automated, commercially available instruments provides measure of both peak oxygen consumption and ventilatory anaerobic threshold that are valid and highly reproducible in elderly patients with diastolic as well as systolic heart failure (Figure 1). Another variable provided by these methods, the minute ventilation carbon dioxide production relationship (VE/VCO2) slope, is a strong predictor of survival, independent of VO2 5. It’s been shown that minute ventilation carbon dioxide production relationship (VE/VCO2) slope is abnormal in patients with diastolic heart failure, though not as abnormal as in those with systolic heart failure 6.
Figure 1. Exercise intolerance test
Footnote: Excellent reproducibility of peak exercise VO2 in older heart failure patients, including those with LV ejection fraction. Group data shown in top panel; representative patient with 15 second averaged data shown in bottom.
[Source 7 ]Exercise intolerance causes
Heart failure sometimes known as congestive heart failure, is a condition in which your heart muscle doesn’t pump blood as well as it should to meet your body’s needs. Heart failure is defined as a syndrome in which cardiac output is insufficient to meet metabolic demands 8. Heart failure does not mean that your heart has stopped or is about to stop working. It means that your heart is not able to pump blood the way it should. It can affect one or both sides of the heart. Heart failure often develops after other conditions have damaged or weakened your heart. The leading causes of heart failure are diseases that damage the heart. Examples include ischemic heart disease, high blood pressure, and diabetes. Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or too stiff to fill and pump efficiently. It is more common in people who are 65 years old or older, African Americans, people who are overweight, and people who have had a heart attack. Men have a higher rate of heart failure than women.
In heart failure, the main pumping chambers of your heart (the ventricles) may become stiff and not fill properly between beats. In some cases of heart failure, your heart muscle may become damaged and weakened, and the ventricles stretch (dilate) to the point that the heart can’t pump blood efficiently throughout your body.
Over time, the heart can no longer keep up with the normal demands placed on it to pump blood to the rest of your body.
An ejection fraction is an important measurement of how well your heart is pumping and is used to help classify heart failure and guide treatment. In a healthy heart, the ejection fraction is 50 percent or higher — meaning that more than half of the blood that fills the ventricle is pumped out with each beat.
But heart failure can occur even with a normal ejection fraction. This happens if the heart muscle becomes stiff from conditions such as high blood pressure.
Heart failure can involve the left side (left ventricle), right side (right ventricle) or both sides of your heart. Generally, heart failure begins with the left side, specifically the left ventricle — your heart’s main pumping chamber.
| Type of heart failure | Description |
|---|---|
| Left-sided heart failure | Fluid may back up in your lungs, causing shortness of breath. |
| Right-sided heart failure | Fluid may back up into your abdomen, legs and feet, causing swelling. |
| Systolic heart failure | The left ventricle can’t contract vigorously, indicating a pumping problem. |
| Diastolic heart failure (also called heart failure with preserved ejection fraction) | The left ventricle can’t relax or fill fully, indicating a filling problem. |
Any of the following conditions can damage or weaken your heart and can cause heart failure. Some of these can be present without your knowing it:
- Coronary artery disease and heart attack. Coronary artery disease is the most common form of heart disease and the most common cause of heart failure. The disease results from the buildup of fatty deposits (plaque) in your arteries, which reduce blood flow and can lead to heart attack.
- Diabetes. Having diabetes increases your risk of high blood pressure and coronary artery disease.
- High blood pressure (hypertension). If your blood pressure is high, your heart has to work harder than it should to circulate blood throughout your body. Over time, this extra exertion can make your heart muscle too stiff or too weak to effectively pump blood.
- Faulty heart valves. The valves of your heart keep blood flowing in the proper direction through the heart. A damaged valve — due to a heart defect, coronary artery disease or heart infection — forces your heart to work harder, which can weaken it over time.
- Damage to the heart muscle (cardiomyopathy). Heart muscle damage (cardiomyopathy) can have many causes, including several diseases, infections, alcohol abuse and the toxic effect of drugs, such as cocaine or some drugs used for chemotherapy. Genetic factors also can play a role.
- Myocarditis. Myocarditis is an inflammation of the heart muscle. It’s most commonly caused by a virus and can lead to left-sided heart failure.
- Heart defects you’re born with (congenital heart defects). If your heart and its chambers or valves haven’t formed correctly, the healthy parts of your heart have to work harder to pump blood through your heart, which, in turn, may lead to heart failure.
- Abnormal heart rhythms (heart arrhythmias). Abnormal heart rhythms may cause your heart to beat too fast, creating extra work for your heart. A slow heartbeat also may lead to heart failure.
- Other diseases. Chronic diseases — such as HIV/AIDS, thyroid disorders (having either too much [hyperthyroidism] or too little thyroid hormone in the body [hypothyroidism]) or a buildup of iron (hemochromatosis) or protein (amyloidosis) — also may contribute to heart failure.
- Other factors also can injure the heart muscle and lead to heart failure. Examples include:
- Alcohol abuse or cocaine and other illegal drug use
- Too much vitamin E
- Treatments for cancer, such as radiation and chemotherapy
Causes of acute heart failure include viruses that attack the heart muscle, severe infections, allergic reactions, blood clots in the lungs, the use of certain medications or any illness that affects the whole body.
Risk factors for heart failure
A single risk factor may be enough to cause heart failure, but a combination of factors also increases your risk.
Risk factors include:
- High blood pressure. Your heart works harder than it has to if your blood pressure is high.
- Coronary artery disease. Narrowed arteries may limit your heart’s supply of oxygen-rich blood, resulting in weakened heart muscle.
- Heart attack. A heart attack is a form of coronary disease that occurs suddenly. Damage to your heart muscle from a heart attack may mean your heart can no longer pump as well as it should.
- Diabetes. Having diabetes increases your risk of high blood pressure and coronary artery disease.
- Some diabetes medications. The diabetes drugs rosiglitazone (Avandia) and pioglitazone (Actos) have been found to increase the risk of heart failure in some people. Don’t stop taking these medications on your own, though. If you’re taking them, discuss with your doctor whether you need to make any changes.
- Certain medications. Some medications may lead to heart failure or heart problems. Medications that may increase the risk of heart problems include nonsteroidal anti-inflammatory drugs (NSAIDs); certain anesthesia medications; some anti-arrhythmic medications; certain medications used to treat high blood pressure, cancer, blood conditions, neurological conditions, psychiatric conditions, lung conditions, urological conditions, inflammatory conditions and infections; and other prescription and over-the-counter medications. Don’t stop taking any medications on your own. If you have questions about medications you’re taking, discuss with your doctor whether he or she recommends any changes.
- Sleep apnea. The inability to breathe properly while you sleep at night results in low blood oxygen levels and increased risk of abnormal heart rhythms. Both of these problems can weaken the heart.
- Congenital heart defects. Some people who develop heart failure were born with structural heart defects.
- Valvular heart disease. People with valvular heart disease have a higher risk of heart failure.
- Viruses. A viral infection may have damaged your heart muscle.
- Alcohol use. Drinking too much alcohol can weaken heart muscle and lead to heart failure.
- Tobacco use. Using tobacco can increase your risk of heart failure.
- Obesity. People who are obese have a higher risk of developing heart failure.
- Irregular heartbeats. These abnormal rhythms, especially if they are very frequent and fast, can weaken the heart muscle and cause heart failure.
Non-cardiac causes of exercise intolerance
Neurological disorders
- Multiple Sclerosis
Respiratory disorders
- Cystic fibrosis: Cystic fibrosis can cause skeletal muscle atrophy, however more commonly it can cause exercise intolerance. The exercise intolerance is associated with reduced pulmonary function that is the origin of cystic fibrosis 9.
- Bronchiectasis
Chronic fatigue syndrome
Orthostatic intolerance occurs in chronic fatigue syndrome. Orthostatic intolerance includes exercise intolerance as one of the main symptoms. It also includes fatigue, nausea, headaches, cognitive problems and visual disturbances as other less major symptoms 10.
Post-concussion syndrome
- Exercise intolerance is present in those with post-concussion syndrome however their intolerance to exercise may reduce over time 11.
- Individuals with postconcussion syndrome may also experience a level of exercise intolerance, however there is little known comparatively about exercise intolerance in post-concussion syndrome patients 12.
Musculoskeletal disorders
- Spinal muscular atrophy: symptoms include exercise intolerance, cognitive impairment and fatigue 13.
- Rhabdomyolysis: a condition in which muscle degrades, releasing intracellular muscle content into the blood as reflected by elevated blood levels of creatine kinase 14. Exercise tolerance is significantly compromised 15.
Mutations
- Mitochondrial complex III: Currently it is suggested that there are 27 different mutations identified in cytochrome b (mitochondrial complex III is one of those mutations). This mutation can often lead to skeletal muscle weakness and as a result exercise intolerance 16.
- Cytochrome C oxidase deficiency (COX deficiency) is a condition that can affect several parts of the body including the skeletal muscles, heart, brain and liver. There are four types of COX deficiency differentiated by symptoms and age of onset: benign infantile mitochondrial type, French-Canadian type, infantile mitochondrial myopathy type, and Leigh syndrome 17. The range and severity of signs and symptoms can vary widely among affected individuals (even within the same subtype and same family) and depend on the form of the condition present. Features in mildly affected individuals may include muscle weakness and hypotonia; in more severely affected individuals, brain dysfunction; heart problems; an enlarged liver; lactic acidosis; and/or a specific group of features known as Leigh syndrome may also be present. Cytochrome C oxidase deficiency (COX deficiency) is caused by mutations in any of at least 14 genes; the inheritance pattern depends on the gene involved. The condition is frequently fatal in childhood, but mildly affected individuals may survive into adolescence or adulthood 18.
- Skeletal muscle respiratory chain defect: This can result in severe exercise intolerance which is manifested by the following symptoms of Skeletal muscle respiratory chain defect; muscle fatigue and lactic acidosis 19. Exercise tolerance reflects the combined capacity of components in the oxygen cascade to supply adequate oxygen for ATP resynthesis. In individuals with diseases such as cancer, certain therapies can affect one or more components of this cascade and therefore reduce the body’s ability to utilize or deliver oxygen, leading to exercise intolerance 20.
Primary cause of symptoms of exercise intolerance
Despite the many exercise physiological studies that have been performed in heart failure patients, there remains uncertainty regarding the final stimulus that causes heart failure patients to stop exercising at lower workloads than healthy subjects 21. It had been thought that increased exercise pulmonary wedge pressure and stimulation of pulmonary J-receptors cause reflex hyperventilation and hypoxia leading to the sensation of severe dyspnea, causing the patient to stop exercise prematurely. However, about 50% of heart failure patients, whether systolic or diastolic, discontinue exercise primarily due to general fatigue or leg fatigue rather than dyspnea. In addition, investigators 22 have demonstrated that arterial hypoxia does not occur during exercise in heart failure patients, and that excess ventilation is related to pulmonary hypoperfusion and reduced cardiac output rather than elevated left-ventricular (LV) filling pressures. Furthermore, exercise intolerance, as measured objectively by peak oxygen consumption (VO2), is unrelated to invasively measure pulmonary capillary wedge pressures, including in patients with diastolic heart failure 23. The decreased exercise cardiac output likely causes skeletal muscle hypoperfusion, a potent stimulus for early anaerobic metabolism, and subsequent generation of muscle lactate and other metabolites which could produce the sensation of peripheral and central fatigue 24. In the studies where lactate production during exercise has been reported, it has been abnormal compared to normals 25.
Based on the extensive experience in seeking to understand exercise intolerance in patients with systolic heart failure, it is likely that several factors in addition to those discussed above may contribute to exercise intolerance in patients with diastolic heart failure, including: anemia which is highly prevalent in diastolic heart failure as it is in systolic heart failure 26 and skeletal muscle bulk, fiber type, and function 27. There have been particularly compelling findings regarding skeletal muscle in systolic heart failure 28. Despite this, there has been no information regarding skeletal muscle in diastolic heart failure. This could be even more relevant in diastolic heart failure given increasing data regarding the role of skeletal muscle atrophy and dysfunction in older patients with a variety of disabling chronic syndromes, this appears a particularly promising area for future investigation 29. In addition, the degree of adipose between skeletal muscle bundles appears to be a potential modifier of skeletal muscle function and exercise capacity as well. This will likely be a fruitful area for future research, particularly since skeletal muscle bulk and function appear potentially modifiable through nutrition and exercise interventions 30.
Pathophysiology of exercise intolerance
In order to understand the pathophysiology of exercise intolerance in diastolic heart failure, we performed a comparative study of maximal exercise testing with expired gas in 119 older subjects in 3 distinct, well-defined groups: heart failure with severe LV systolic dysfunction (mean EF 30%); isolated diastolic heart failure (EF ≥ 50% and no significant coronary, valvular, pericardial, or pulmonary disease and no anemia); and age-matched controls.(3) In comparison to the controls, peak exercise oxygen consumption (VO2) was severely reduced in the patients with diastolic heart failure and to a similar degree as those with systolic heart failure (Fig. 2).(3) submaximal exercise capacity, as measured by the ventilatory anaerobic threshold, was similarly reduced in diastolic heart failure vs. systolic heart failure patients. This was accompanied by reduced health-related quality of life.(3)
By the Fick equation, peak VO2 during exercise is the product of cardiac output and arteriovenous oxygen (A-VO2) difference, indicating that exercise intolerance will be related to one or both of these factors and to the variables that influence them. Measurement of peak exercise VO2 and at least one of these other 2 factors (cardiac output or arteriovenous oxygen difference) allows one to calculate the remaining unknown factor and begin to isolate specific factors that contribute to exercise intolerance within individual patients and groups.(Figure 3).
Exercise intolerance signs and symptoms
Exercise intolerance is defined as the reduced ability to perform activities involving dynamic movement because of symptoms of dyspnea or fatigue, is the most common clinical symptom among patients with heart failure 1. Exercise intolerance is defined as the primary symptom of chronic diastolic heart failure 2. Exercise intolerance was defined as a peak exercise capacity of 7 metabolic equivalents (METs) or less 3.
Exercise intolerance diagnosis
Exercise intolerance can be objectively quantified using semiquantitative assessments, such as interview (New York Heart Association classification) and surveys (Minnesota Living with Heart Failure or Kansas City Cardiomyopathy questionnaires), and quantitative methods, including timed walking tests (6 minute walk distance) and graded exercise treadmill or bicycle exercise tests. Cardiopulmonary exercise testing on a treadmill or a bicycle ergometer provides the most accurate, reliable, and reproducible assessments of exercise tolerance, and yields multiple important outcomes, including METS, exercise time, exercise workload, blood pressure and heart rate responses, and rate-pressure product.
Exercise intolerance treatment
During exercise in normal subjects, systolic and pulse pressure increase substantially, and this response is magnified by increased arterial stiffness. Data from animal models suggest that the exercise related increase in systolic blood pressure is mediated, in part, by exercise-induced increases in circulating angiotensin-2. In a randomized, double-blind, placebo-controlled cross-over trial, angiotensin receptor blockade reduced the exaggerated exercise increase in systolic and pulse pressures, resulting in significantly improved exercise treadmill time and quality of life 31.
Aronow et al 32 showed in a group of NYHA class III heart failure patients and presumed diastolic dysfunction (EF >50%) that the ACE inhibitor enalapril significantly improved functional class, exercise duration, ejection fraction, diastolic filling, and left ventricular mass.
In hypertrophic cardiomyopathy, a disorder in which diastolic dysfunction is common, verapamil appears to improve symptoms and objectively measured exercise capacity 33. This agent also improves ventricular vascular coupling and exercise performance in aged individuals with hypertension 34. In laboratory animal models calcium antagonists, particularly dihydropyridines, prevent ischemia-induced increases in left-ventricular diastolic stiffness 35 and in improve diastolic performance in pacing-induced heart failure 36. However, negative inotropic calcium antagonists significantly impair early relaxation 37 and have in general shown a tendency toward adverse outcome in patients with systolic heart failure 36. Despite this, Setaro 38 examined 22 men (mean age 65) with clinical heart failure despite ejection fraction >45% in a randomized, double-blind, placebo-controlled crossover trial of verapamil. There was a 33% improvement in exercise time and significant improvements in clinicoradiographic heart failure scoring and peak filling rate.
Little et al 39 compared the calcium channel antagonist verapamil in a randomized, cross-over, blinded trial to the angiotensin receptor antagonist candesartan with the outcomes of peak exercise blood pressure, exercise time and quality of life. While both agents blunted the peak systolic blood pressure response to exercise, only candesartan, and not verapamil, improved exercise time and quality of life 39.
A subsequent trial with similar randomized, cross-over, blinded design, the diuretic hydrochlorothiazide was compared with the angiotensin receptor antagonist losartan on the outcomes of peak exercise blood pressure, exercise time and quality of life 40. While both agents blunted the peak systolic blood pressure response to exercise, only losartan, but not hydrochlorothiazide, improved exercise time and quality of life 40.
The addition of low dose spironolactone (12.5–50 mg daily) to standard therapy has been shown to improve exercise tolerance in patients with severe systolic heart failure. Aldosterone antagonism has numerous potential benefits in patients with diastolic heart failure, including left-ventricle remodeling, reversal of myocardial fibrosis, and improved left-ventricular diastolic function and vascular function 41. However few data are presently available regarding aldosterone antagonism in diastolic heart failure. In one small study, low dose spironolactone was well tolerated and appeared to improve exercise capacity and quality of life in older women with isolated diastolic heart failure 42. In another, spironolactone improved measures of myocardial function in hypertensive patients with diastolic heart failure 43.
Glucose cross-links increase with aging and diabetes, and cause increased vascular and myocardial stiffness. Alagebrium, a novel cross-link breaker, improved vascular and left-ventricular stiffness in dogs. In a small, open label, 4-month trial of this agent in elderly patients 44, left-ventricular mass, quality of life, and tissue Doppler diastolic function indexes improved, but there were no significant improvements in exercise capacity or aortic distensibility, the primary outcomes of the trial. A variety of other agents and strategies are currently being evaluated or under consideration for this syndrome, including a selective endothelin antagonist.
Aerobic exercise training has the potential to improve a variety of key abnormalities in patients with heart failure and normal ejection fraction, including left-ventricular diastolic compliance, aortic distensibility, blood pressure, and skeletal muscle function 45. In systolic heart failure, aerobic exercise training has been shown to improve exercise tolerance, likely via favorable effects on multiple factors 46. A recent report indicates that left-ventricular diastolic compliance is preserved in older masters athletes compared to their age matched and young counterparts, suggesting that exercise training may be beneficial in diastolic heart failure as well 47. A preliminary report indicates that exercise training improves exercise tolerance and quality of life in older patients with heart failure and normal ejection fraction 48. A recent report from a clinical exercise rehabilitation program suggests that exercise training may also benefit patients with diastolic heart failure 49. Although the role of exercise training in the clinical management of this syndrome remains to be defined, as is the accepted practice in systolic heart failure, it would seem prudent to recommend regular, moderate physical activity as tolerated. The effect of exercise training on survival in systolic heart failure patients is being examined in a large, National Institute of Health-sponsored, multicenter, randomized, controlled trial (heart failure-ACTION). Presently, there is no trial examining mortality and exercise training in patients with heart failure and normal ejection fraction.
References- Heart Failure: A Companion to Braunwald’s Heart Disease 2nd Edition, 2011. ISBN 978-1-4160-5895-3 https://doi.org/10.1016/C2009-0-48074-7
- Kitzman DW, Groban L. Exercise intolerance. Heart Fail Clin. 2008;4(1):99–115. doi:10.1016/j.hfc.2007.12.002 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2700357
- Yi, J. E., Lee, Y. S., Choi, E. K., Cha, M. J., Kim, T. H., Park, J. K., … Park, J. (2018). CHA2DS2-VASc score predicts exercise intolerance in young and middle-aged male patients with asymptomatic atrial fibrillation. Scientific reports, 8(1), 18039. doi:10.1038/s41598-018-36185-7
- Kitzman, D. W., & Groban, L. (2008). Exercise intolerance. Heart failure clinics, 4(1), 99–115. doi:10.1016/j.hfc.2007.12.002 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2700357
- Francis DP, Shamin W, Davies LC, Piepoli M, Ponikowski P, Anker SD, et al. Cardiopulmonary exercise testing for prognosis in chronic heart failure: continuous and independent prognostic value from VE/VCO2 slope and peak VO2. Eur Heart J. 2000;21:154–161.
- Moore B, Brubaker PH, Stewart KP, Kitzman DW. VE/VCO2 Slope in Older Heart Failure Patients With Normal Versus Reduced Ejection Fraction Compared With Age-Matched Healthy Controls. Journal of Cardiac Failure. 2007;13(4):259–262.
- Marburger et al, Am J. Cardiol 1998;82:905–909.
- Kitzman, D. W., & Groban, L. (2011). Exercise intolerance. Cardiology clinics, 29(3), 461–477. doi:10.1016/j.ccl.2011.06.002 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3694583
- Van de Weert-van Leeuwen, Pauline (2013). “Infection, inflammation and exercise in cystic fibrosis”. Respiratory Research. 14: 32. doi:10.1186/1465-9921-14-3
- Leonard, Jason (2014-01-01). “Predictors of post-infectious chronic fatigue syndrome in adolescents”. Health Psychology and Behavioural Medicine. 2 (1): 41–51. doi:10.1080/21642850.2013.869176
- Kozlowski, Karl F. (2013). “Exercise Intolerance in Individuals With Postconcussion Syndrome”. Journal of Athletic Training. 48 (5): 627–35. doi:10.4085/1062-6050-48.5.02
- Kozlowski, Karl F; Graham, James (2013). “Exercise Intolerance in Individuals With Postconcussion Syndrome”. Journal of Athletic Training. 48 (5): 627–635. doi:10.4085/1062-6050-48.5.02
- Brum, Marisa (2014). “Motor Neuron Syndrome as a New Phenotypic Manifestation of Mutation 9185T>C in Gene MTATP6”. Case Rep Neurol Med. 2014: 701761. doi:10.1155/2014/701761
- Chavez, L. O.; Leon, M; Einav, S; Varon, J (2016). “Beyond muscle destruction: A systematic review of rhabdomyolysis for clinical practice”. Critical Care. 20 (1): 135. doi:10.1186/s13054-016-1314-5
- Quinlivan, R; Jungbluth, H (2012). “Myopathic causes of exercise intolerance with rhabdomyolysis”. Developmental Medicine and Child Neurology. 54 (10): 886–91. doi:10.1111/j.1469-8749.2012.04320.x
- Barel, Ortal (2008). “Mitochondrial Complex III Deficiency Associated with a Homozygous Mutation in UQCRQ”. The American Journal of Human Genetics. 82 (5): 1211–6. doi:10.1016/j.ajhg.2008.03.020
- Cytochrome C Oxidase Deficiency. https://rarediseases.org/rare-diseases/cytochrome-c-oxidase-deficiency
- Cytochrome c oxidase deficiency. https://ghr.nlm.nih.gov/condition/cytochrome-c-oxidase-deficiency
- Haller, R.G (1989). “Exercise intolerance, lactic acidosis, and abnormal cardiopulmonary regulation in exercise associated with adult skeletal muscle cytochrome c oxidase deficiency”. The Journal of Clinical Investigation. 84 (1): 155–61. doi:10.1172/JCI114135
- Jones, Lee W.; Eves, Neil D.; Haykowsky, Mark; Freedland, Stephen J.; MacKey, John R. (2009). “Exercise intolerance in cancer and the role of exercise therapy to reverse dysfunction”. The Lancet Oncology. 10 (6): 598–605. doi:10.1016/S1470-2045(09)70031-2
- Wilson JR, Rayos G, Yeoh TK, Gothard P, Bak K. Dissociation between exertional symptoms and circulatory function in patients with heart failure. Circulation. 1995;92(1):47–53.
- Sullivan M, Higginbotham MB, Cobb FR. Increased exercise ventilation in patients with chronic heart failure: intact ventilatory control despite hemodynamic and pulmonary abnormalities. Circulation. 1988;77:552–559.
- Kitzman DW, Higginbotham MB, Cobb FR, Sheikh KH, Sullivan M. Exercise intolerance in patients with heart failure and preserved left ventricular systolic function: failure of the Frank-Starling mechanism. J Am Coll Cardiol. 1991;17:1065–1072.
- Sullivan M, Cobb FR. The anaerobic threshold in chronic heart failure. Circulation. 1990;81:II-47–II-58.
- Kitzman DW, Little WC, Brubaker PH, Anderson RT, Hundley WG, Marburger CT, et al. Pathophysiological characterization of isolated diastolic heart failure in comparison to systolic heart failure. JAMA. 2002;288(17):2144–2150.
- Brucks S, Little WC, Chao T, Rideman RL, Upadhya B, Wesley-Farrington D, et al. Relation of anemia to diastolic heart failure and the effect on outcome. Am J Cardiol. 2004;93(8):1055–1057.
- Deedwania PC, Gottlieb S, Ghali JK, Waagstein F, Wikstrand JC. Efficacy, safety and tolerability of beta-adrenergic blockade with metoprolol CR/XL in elderly patients with heart failure. Eur Heart J. 2004;25(15):1300–1309.
- Sullivan JJ, Green HJ, Cobb FR. Skeletal muscle biochemistry and histology in ambulatory patients with long-term heart failure. Circulation. 1990;81:518–527.
- Buchner D, deLateur B. The importance of skeletal muscle strength to physical function in older adults. Behav Med Annals. 1991;13:4206–4214.
- Menshikova EV, Ritov VB, Toledo FGS, Ferrell RE, Goodpaster BH, Kelley DE. Effects of weight loss and physical activity on skeletal muscle mitochondrial function in obesity. Am J Physiol Endocrinol Metab. 2005;288(4):E818–E825.
- Warner JG, Metzger C, Kitzman DW, Wesley DJ, Little WC. Losartan improves exercise tolerance in patients with diastolic dysfunction and a hypertensive response to exercise. J Am Coll Cardiol. 1999;33:1567–1572.
- Aronow WS, Kronzon I. Effect of enalapril on congestive heart failure treated with diuretics in elderly patients with prior myocardial infarction and normal left ventricular ejection fraction. Am J Cardiol. 1993;71:602–604.
- Udelson J, Bonow RO. Left ventricular diastolic function and calcium channel blockers in hypertrophic cardiomyopathy. In: Gaasch WH, editor. Left Ventricular Diastolic Dysfunction and Heart Failure. Malvern, Pennsylvania: Lea & Febiger; 1996. pp. 465–489.
- Chen CH, Nakayama M, Talbot M, Nevo E, Fetics B, Gerstenblith G, et al. Verapamil acutely reduces ventricular-vascular stiffening and improves aerobic exercise performance in elderly individuals. J Am Coll Cardiol. 1999;33:1602–1609.
- Serizawa T, Shin-Ichi M, Nagai Y, Ogawa T, Sato T, Nezu Y, et al. Diastolic abnormalities in low-flow and pacing tachycardia-induced ischemia in isolated rat hearts-modification by calcium antagonists. In: Lorell BH, Grossman W, editors. Diastolic Relaxation of the Heart. Norwell, Massachusetts: Kluwer Academic Publishers; 1996. pp. 266–274.
- Little WC, Cheng CP, Elvelin L, Nordlander M. Vascular selective calcium entry blockers in the treatment of cardiovascular disorders: Focus on felodipine. Cardiovasc Drugs Ther. 1995;9(5):657–663.
- Hess OM, Murakami T, Krayenbuehl HP. Does verapamil improve left ventricular relaxation in patients with myocardial hypertrophy? Circulation. 1996;74:530–543.
- Setaro JF, Zaret BL, Schulman DS, Black HR. Usefulness of verapamil for congestive heart failure associated with abnormal left ventricular diastolic filling and normal left ventricular systolic performance. Am J Cardiol. 1990;66:981–986.
- Little WC, Wesley-Farrington DJ, Hoyle J, Brucks S, Robertson S, Kitzman DW, et al. Effect of candesartan and verapamil on exercise tolerance in diastolic dysfunction. J Cardiovasc Pharmacol. 2004;43(2):288–293.
- Little WC, Zile MR, Klein AL, Appleton CP, Kitzman DW, Wesley-Farrington DJ. Effect of Losartan and Hydrochlorothiazide on Exercise Tolerand in Exertional Hypertension and Diastolic Dysfunction. Am J Cardiol. 2006;98(3):383–385.
- Pitt B, Reichek N, Willenbrock R, Zannad F, Phillips RA, Roniker B, et al. Effects of eplerenone, enalapril, and eplerenone/enalapril in patients with essential hypertension and left ventricular hypertrophy: the 4E-left ventricular hypertrophy study. Circulation. 2003;108(15):1831–1838.
- Daniel KR, Wells GL, Fray B, Stewart KP, Kitzman DW. The effect of spironolactone on exercise tolerance and quality of life in elderly women with diastolic heart failure. Am J Geriatr Cardiol. 2003;12(2):131.
- Mottram PM, Haluska B, Leano R, Cowley D, Stowasser M, Marwick TH. Effect of aldosterone antagonism on myocardial dysfunction in hypertensive patients with diastolic heart failure. Circulation. 2004;110(5):558–565.
- Little WC, Zile MR, Kitzman DW, Hundley WG, O’Brien TX, deGroof RC. The Effect of Alagebrium Chloride(ALT-711), a Novel Glucose Cross-Link Breaker, in the Treatment of Elderly Patients with Diastolic Heart Failure. J Card Fail 5 AD. 11(3):191–195.
- Sullivan M. Role of exercise conditioning in patients with severe systolic left ventricular dysfunction. In: Fletcher GF, editor. Cardiovascular Response to Exercise. Mount Kisco: Futura Publishing Company; 1994. pp. 359–372.
- Pina IL, Apstein CS, Balady GJ, Belardinelli R, Chaitman BR, Duscha BD, et al. Exercise and heart failure: A statement from the American Heart Association Committee on exercise, rehabilitation, and prevention. Circulation. 2003;107(8):1210–1225.
- Arbab-Zadeh A, Dijk E, Prasad A, Fu Q, Torres P, Zhang R, et al. Effect of aging and physical activity on left ventricular compliance. Circulation. 2004;110(13):1799–1805.
- Kitzman DW, Brubaker PH, Abdelahmed A, Stewart KP. Effect of Exercise Training on Exercise Capacity, Quality of Life, and Flow-Mediated Arterial Dilation in Elderly Patients with Diastolic Heart Failure. J Am Coll Cardiol. 2004;110(17):III-558.
- Smart N, Haluska B, Jeffriess L, Marwick TH. Exercise training in systolic and diastolic dysfunction: Effects on cardiac function, functional capacity, and quality of life. American Heart Journal. 2007;153(4):530–536.