Facial fractures
Facial fractures are commonly caused by blunt or penetrating trauma at moderate or high levels of force. Facial fractures may be sustained during a fall, physical assault, motor vehicle collision, or gunshot wound. Sports like football, baseball, and hockey account for a high percentage of facial injuries among young adults. The facial bones are thin and relatively fragile making them susceptible to injury.
Facial fractures may be associated with head and cervical spine injuries 1. A review by Boden et al 2 of catastrophic injuries associated with high school and college baseball demonstrated 1.95 direct catastrophic injuries annually, including severe head injuries, cervical injuries, and associated facial fractures.
Males are affected more commonly than females, and facial fractures are most common in the third decade, i.e. 20-30 years 3.
Fractures of the facial bones require a significant amount of force. The physician must take into account the mechanism of the injury as well as the physical examination findings when assessing the patient.
Forces that are required to produce a fracture of the facial bones are as follows 4:
- Nasal fracture – 30 G (30 times the force of gravity)
- Zygoma fractures – 50 G (50 times the force of gravity)
- Mandibular (angle) fractures – 70 G (70 times the force of gravity)
- Frontal region fractures – 80 G
- Maxillary (midline) fractures – 100 G
- Mandibular (midline) fractures – 100 G
- Supraorbital rim fractures – 200 G
Note: 1 G equal to the conventional value of gravitational acceleration on Earth, g, of about 9.8 m/s² or 9.8 m/second/second 5.
The extent and pattern of soft tissue and bony facial injuries varies according energy of impact. Isolated fracture is most common with lower energy trauma, whereas high energy blunt and penetrating trauma results in more complex, less predictable injury pattern.
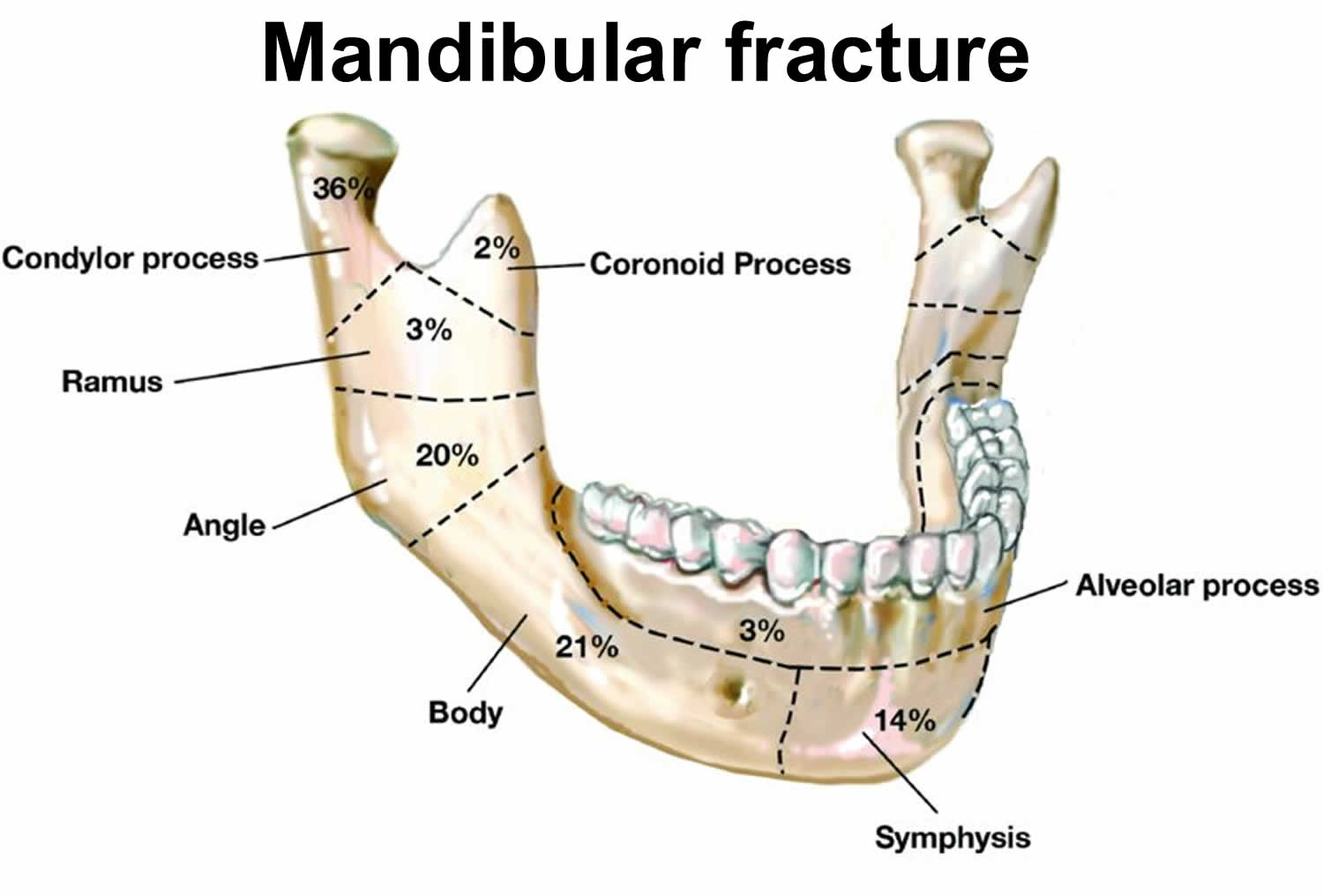
The most commonly fracture facial bones (in isolation) are the nasal bones, followed by the mandible and the bony orbit 6. Fractures involving more than one bone most commonly affect the orbital floor and zygomaticomaxilla 3.
Sports participation is the most common cause of mandibular fractures (31.5%), followed closely by motor vehicle accidents (27.2%). A study of facial fractures sustained during recreational baseball and softball demonstrated that the zygoma or zygomatic arch was the most common fracture subtype, followed by temporoparietal skull fractures and orbital blow-out fractures 7. A number of studies in the medical literature, however, indicate that the nasal bones are the most commonly fractured bones in the face, but because many of these patients do not seek medical treatment or the injuries are managed in the outpatient setting, the statistics may not reflect this trend 1. It is likely that the nasal bones are more commonly fractured because of the lesser degree of force that is required to fracture the bone 8.
Fractures of the orbit occur more commonly in young adult and adolescent males: the mean age for adult males is 32 years; the mean age for children, 12.5 years, and the majority of orbital fractures occur in boys. In addition to sports-related injuries, injuries sustained in motor vehicle collisions, assaults, and occupational injuries account for the majority of orbital fractures 9.
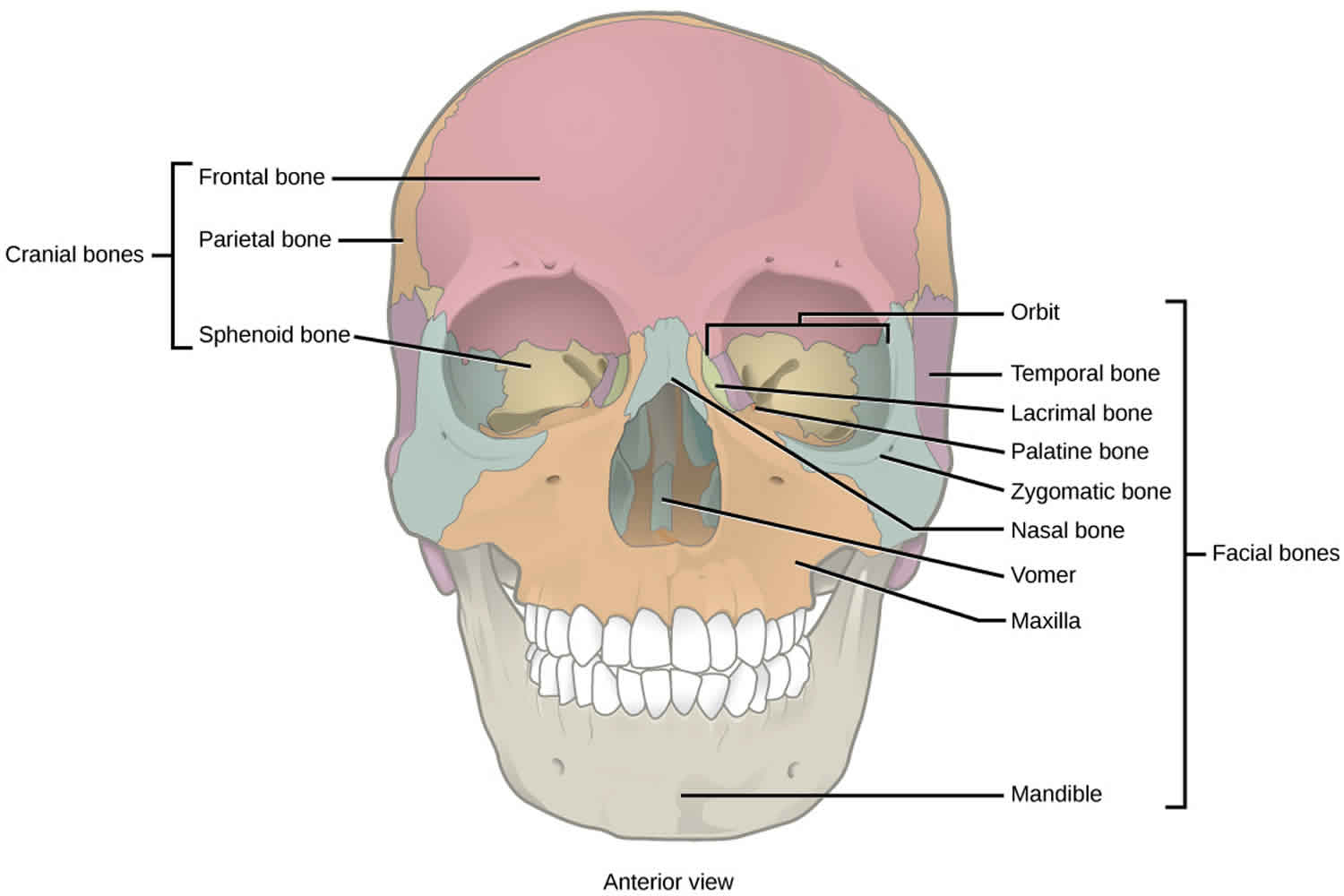
Figure 1. Facial bones
Facial fractures anatomy
Frontal sinus
Both the anterior and posterior wall may be damaged. Because the posterior wall is adjacent to the dura mater, damage in this region could result in central nervous system (CNS) complications such as a cerebrospinal fluid (CSF) leak or meningitis.
Eye socket (orbit)
The bony orbit is composed of 7 bones of varying thickness. The frontal bone forms the supraorbital rim and orbital roof. The medial surface consists of the ethmoid, whereas the greater wing of the sphenoid and the zygoma create the lateral margin. Inferiorly, the floor and infraorbital rim are formed by the zygoma and maxilla. This portion is very thin; therefore, it is the most common site of fracture within the orbit. Fracture of the orbital floor, also known as a blow-out fracture, can result in entrapment of the inferior rectus muscle, limiting upward gaze.
The most common fracture to the orbital rim involves the orbital zygomatic region; this fracture, which typically results from a high-impact blow to the lateral orbit, often results in a fracture to the orbital floor as well 9.
Orbital fractures are typically caused by a hard blow to the face. There are two primary types of orbital fractures:
- Indirect floor fractures: Also known as “blowout fractures,” these are the most common type of orbital trauma. They occur when the thin floor of the eye socket cracks, leaving the rim unaffected. The crack or hole in the orbital floor can trap eye muscles and surrounding tissues, impeding normal eye movement.
- Orbital rim fractures: These breaks affect both the floor and the rim of the eye socket. They typically occur after a severe blow, which could also affect other facial bones and the optic nerve.
Nose
The nose is the most prominent feature of the facial structures and is the most commonly fractured of all facial bones 10. The upper third of the nose is supported by the paired nasal bones and the frontal process of the maxilla, whereas the lower two thirds of the nose are maintained by cartilaginous structures 8. A more serious injury, a nasoorbitoethmoid fracture, occurs with trauma to the bridge of the nose. This injury involves extension into the frontal and maxillary bones and can result in disruption of the cribriform plate with concomitant CSF rhinorrhea.
Zygomatic or zygomaticomaxillary complex
The zygoma, like the nasal bones, is a prominent facial bone and, therefore, is prone to injury. Commonly, a breakage in this area involves a central depression with fractures at both ends. The central fragment may impinge upon the temporalis muscles, resulting in trismus. Because of its thickness, isolated fractures of the zygoma are rare, often involving extension into the thinner bones of the orbit or maxilla, otherwise known as zygomaticomaxillary (ie, tetrapod or tripod fractures).
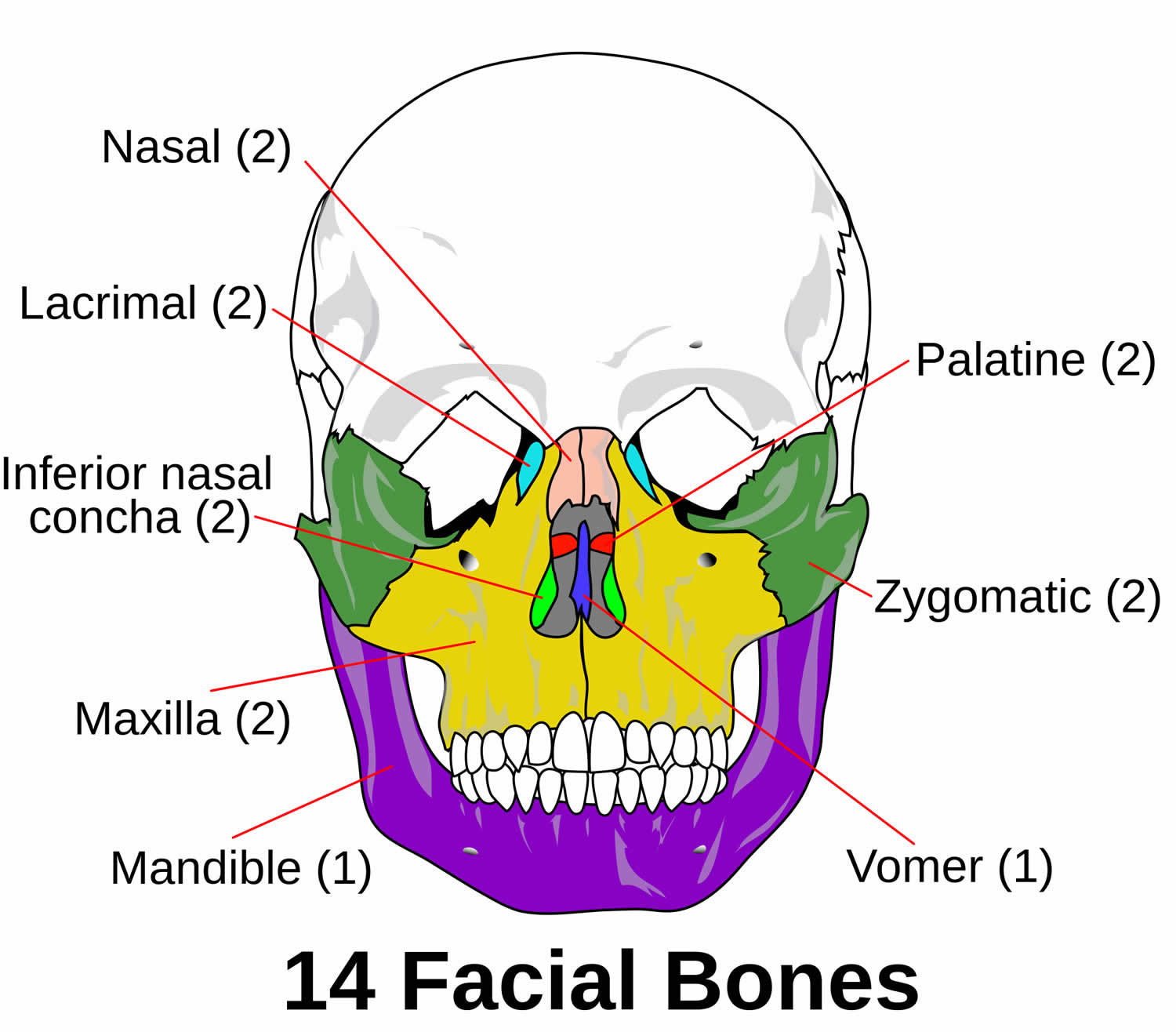
Maxillary (Le Fort)
Rene Le Fort first described fractures of the maxillary region in the 1900s 11. Le Fort conducted experiments on 35 cadavers inflicting varying facial trauma by dropping cannon balls and striking them with a bat. He would then boil the heads to remove soft tissue and record the results 11. Classification of maxillary fractures is based on the most superior level of the fracture site 10.
- Le Fort 1 injuries involve a transverse fracture of the maxilla above the level of the root apices and through or below the level of the nose.
- Le Fort 2 injuries traverse the nose, infraorbital rim, and orbital floor and then proceed laterally through the lateral buttress and posteriorly through the pterygomaxillary buttress.
- Le Fort 3 injuries, also known as craniofacial dysjunction, result from motor vehicle or motorcycle accidents and are the result of the mid face being separated from the cranial base.
Figure 2. Maxillary bone fracture (Le Fort fracture)
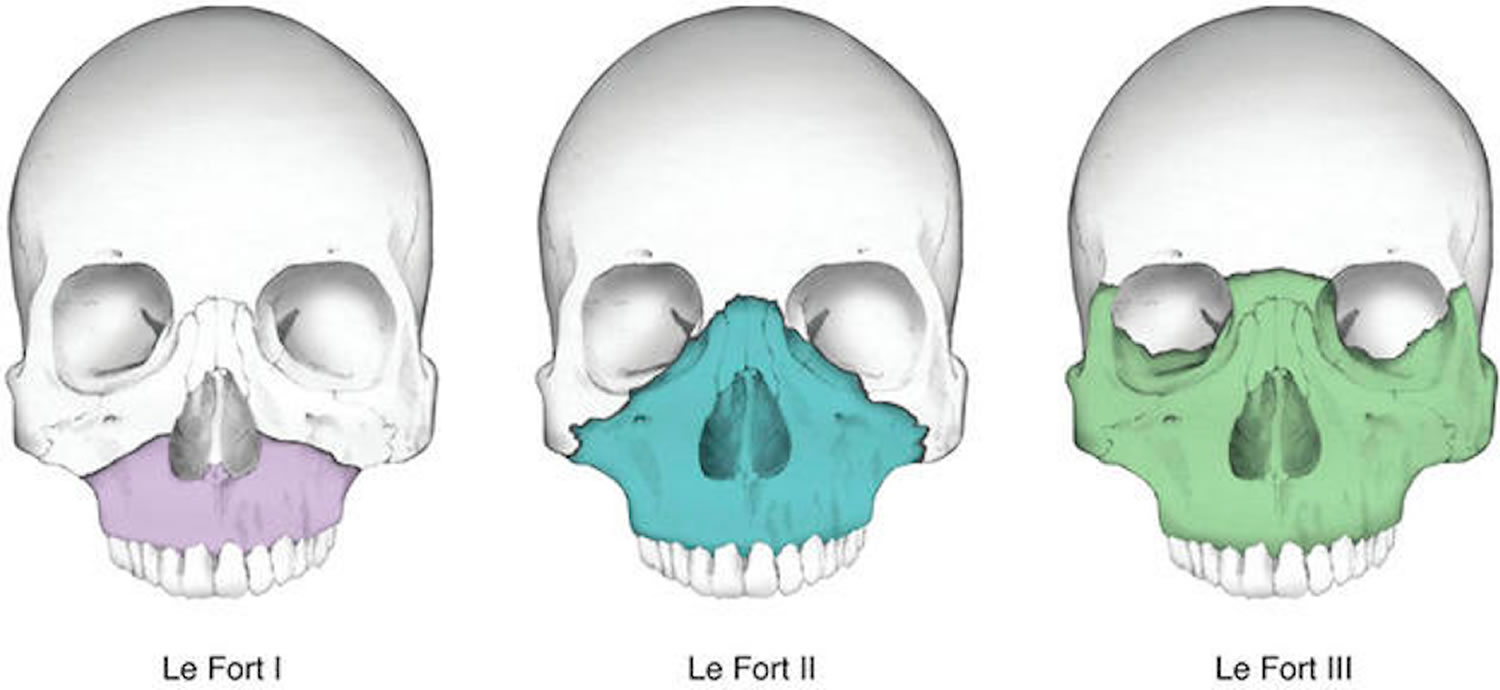
Mandibular
Fractures of the mandible can involve the symphysis, body, angle, ramus, condyle, and subcondyle regions. Fractures of the mandibular body, condyle, and angle occur with nearly equal frequency, followed by fractures of the ramus and coronoid process 10. Generally, motor vehicle accidents result in fractures of the condylar and symphysis regions because the force is directed against the chin, whereas injuries from boxing are more likely to be located in the mandibular angle, as the result of a right-handed punch. Over 50% of mandible fractures are multiple; the presence of one mandibular fracture mandates evaluation for additional fractures, perhaps contralateral to the affected side 10.
Figure 3. Mandibular fracture
Types of facial fractures
Facial fractures have been categorized according to multiple schemas, most famously according to a simplified three-tier Le Fort classification for complex midface fractures. The concept of ‘facial buttresses’ has also been used to elucidate structurally-meaningful skeletal struts which play important in facial integrity.
More recently, advances in surgical technique enable surgeons to consider reduction, stabilization, and reconstruction of complex midfacial fractures according to five midface subunits 12:
- Nasoseptal fractures
- Naso-orbitoethmoid complex fractures
- Orbital fractures
- Zygomaticomaxillary complex fractures
- Isolated zygomatic arch fractures
- Occlusion-bearing maxillary fractures
- Alveolar process fractures
Beyond the midface, other clinically-significant fractures of the facial area include:
- Frontal sinus fracture
- Paranasal sinus fractures
- Mandibular fracture
Le Fort fracture classification
Le Fort fractures are fractures of the midface or fractures of the maxillary region, which collectively involve separation of all or a portion of the midface from the skull base. In order to be separated from the skull base, the pterygoid plates of the sphenoid bone need to be involved as these connect the midface to the sphenoid bone dorsally. The Le Fort classification system attempts to distinguish according to the plane of injury.
The commonly used Le Fort classification is as follows:
- Le Fort type 1
- horizontal maxillary fracture, separating the teeth from the upper face
- fracture line passes through the alveolar ridge, lateral nose and inferior wall of the maxillary sinus
- Le Fort type 2
- pyramidal fracture, with the teeth at the pyramid base, and nasofrontal suture at its apex
- fracture arch passes through the posterior alveolar ridge, lateral walls of maxillary sinuses, inferior orbital rim and nasal bones
- uppermost fracture line can pass through the nasofrontal junction or the frontal process of the maxilla 13
- Le Fort type 3
- craniofacial dysjunction
- transverse fracture line passes through nasofrontal suture, maxillo-frontal suture, orbital wall, and zygomatic arch / zygomaticofrontal suture
- because of the involvement of the zygomatic arch, there is a risk of the temporalis muscle impingement
A memory aid is:
- Le Fort 1 is a floating palate (horizontal)
- Le Fort 2 is a floating maxilla (pyramidal)
- Le Fort 3 is a floating face (transverse)
Any combination is possible. For example, there may be type 2 on one side and contralateral type 3, or there may be unilateral type 1 and 2 fractures. It should be noted that Le Fort fractures are often associated with other facial fractures, neuromuscular injury and dental avulsions.
Practical points
- fracture of the pterygoid plates is mandatory to diagnose Le Fort fractures
- anterolateral margin of the nasal fossa involvement
- if fractured, it is a type 1 fracture
- if intact, it excludes a type 1 fracture
- inferior orbital rim involvement
- if fractured, it is a type 2 fracture
- if intact, it excludes a type 2 fracture
- zygomatic arch involvement
- if fractured, it is a type 3 fracture
- if intact, it excludes a type 3 fracture
- nasofrontal suture involvement indicates either a type 2 or 3 fracture
- a combination of fractures may occur on the same side
- bilateral fractures may be asymmetric
Facial fractures prevention
In a report by Laskin 14, the author observed that more than 100,000 sport-related injuries could be prevented annually by wearing appropriate head and face protection. Adherence to the rules and guidelines established by the specific sports governing body is most important. Almost all eye injuries are preventable, but other fractures can and do occur in sports with high levels of physical contact. Visual acuity, protective gear, and adherence to the rules of the sport are the best ways to limit the risk of facial fractures.
Mouthguards have been shown to prevent some facial injuries; however, no evidence supports them preventing concussions 15.
Facial fracture symptoms
Injuries to the head and neck frequently involve the airway or major vessels. The initial assessment, therefore, should begin with airway, breathing, and circulation (ABCs).
First, protect the airway by removing any foreign bodies and by placing the patient in a sitting position or on the side to facilitate expectoration of blood. If severe maxillofacial trauma is present, the athlete is at risk for airway obstruction because of a lack of tongue support from the mandibular structures. Consider placing an oral airway or, if necessary, performing endotracheal intubation. Second, assess the athlete for breathing and circulation. Lastly, evaluate the cervical spine. In the literature, cervical spine injuries have been shown to be present in 1-4% of patients with facial fractures. Because of the force necessary to fracture the facial bones, one should consider the cervical spine is fractured until proven otherwise, and cervical spine immobilization should be maintained.
Following initial stabilization of the airway, breathing, and circulation (ABCs), the examiner should proceed with the history and physical examination. In addition to obtaining a basic history of the injury and past medical problems, the clinician should seek to answer the following questions 16:
- Can you breathe out of both sides of your nose?
- Are you having any trouble speaking?
- Do you have double vision or any other trouble with your vision?
- Is your hearing normal?
- Are you experiencing any numbness of your face?
- Have you had any previous facial injuries or surgeries, including procedures to correct vision (eg, LASIK [laser-assisted in situ keratomileusis])?
- Do your teeth come together the way they normally would?
- Are any of your teeth painful or loose?
The patient should be questioned regarding the mechanism of the injury, the presence of numbness or pain over any parts of the face, and visual disturbances.
Frontal sinus fractures
This injury results from a severe blow to the frontal or supraorbital region, which can result in fracture of the anterior and/or posterior wall.
The patient may report numbness in the distribution of the supraorbital nerve.
Orbital fractures
Blow-out fractures generally occur with blunt trauma to the orbit with an object larger in diameter than the orbital entrance (eg, baseball, fist).
A blow-in fracture results when a fracture fragment is displaced into the orbit, resulting in decreased orbital volume and impingement on orbital soft tissues, such as from high-velocity trauma (eg, falls from a height, severe blows to the orbit with a weapon).
Patients may report diplopia.
Nasal fractures
With the exception of nasoorbitoethmoid fractures, nasal fractures are typically diagnosed based upon the history and physical examination findings. Often a history of a blow to the nose and epistaxis is present.
Zygomatic and zygomaticomaxillary complex fractures
The athlete may report a forceful blow to the cheek with a bat or an elbow.
Fractures of the zygomaticomaxillary complex may result in trismus or numbness in the distribution of the infraorbital nerve.
Maxillary (Le Fort) fractures
- Le Fort 1 is a transverse fracture of the maxilla just above the teeth.
- Le Fort 2 is a pyramid fracture of the maxilla, the apex of which is above the bridge of the nose and which extends laterally and inferiorly through the infraorbital rims.
- Le Fort 3 is a complete craniofacial disruption and involves fractures of the zygoma, infraorbital rims, and maxilla. This injury requires a significant causative force and, therefore, is relatively uncommon in athletes; however, it may be observed with an injury from a hockey puck, baseball pitch, or baseball bat. Athletes with this injury may report diplopia, malocclusion, or numbness.
Mandibular fractures
The patient may report malocclusion and jaw pain or numbness.
Physical examination
The physical examination should be performed in a methodic, sequential manner. One approach organizes the examination from inside out and bottom up and involves inspection, palpation, and sensory and motor testing.
Examine the oral pharynx for lacerations, tooth fragments, or other foreign bodies. Look closely at the dentition to assess for tooth avulsion or tooth mobility, which can indicate underlying skeletal fractures. Then, carefully evaluate each region of the face, including the mandibular, maxillary, zygomal, nasal, orbital, and frontal bones.
Any areas of obvious trauma, such as a laceration, swelling, depression, or ecchymosis, should be examined more closely. Evaluate the mandible for trismus and mobility. The mid face should be assessed for stability and depression of the bones.
After inspection and palpation, test the motor and sensory function of the facial nerves and muscles. Hypoesthesia in the region of the infraorbital or supraorbital nerve may suggest an orbital fracture, whereas decreased sensation of the chin may result from inferior alveolar nerve compression from a mandibular fracture. Trismus, spasm of the muscles of the jaw, which results in the inability to open and close the mouth, can be secondary to mandibular or zygomatic fractures.
Any fluid from the nose should be inspected for possible CSF rhinorrhea, indicating disruption of the anterior cranial base. Lastly, examine the eyes, including the pupils, extraocular movements, visual acuity, and, if clinically indicated, intraocular pressure and corneal fluorescein. Findings for specific fractures include the following:
Frontal sinus fractures
Look for a visible or palpable depression in the region of the frontal sinus.
A fracture of the posterior wall implies fracture of the dura and may be manifested by CNS depression, CSF rhinorrhea, or visible brain matter.
Orbital fractures
Patients with orbital fractures may present with ecchymosis and edema of the eyelids, subconjunctival hemorrhage, diplopia with limitation in upgaze or downgaze, enophthalmos, infraorbital nerve anesthesia, or emphysema of the orbits/eyelids.
One of the significant clinical features of a fracture to the orbital floor is entrapment of the inferior rectus muscle, resulting in impaired upward gaze on the affected side. Entrapment of the inferior orbital nerve may result from a fracture of the orbital floor and is manifested by decreased sensation to the cheek, upper lip, and upper gingival region on the affected side.
Entrapment of these structures may be more commonly encountered in children, whose bones may be more flexible and demonstrate a linear pattern that snaps back to create a “trap-door” fracture; in adults, the floor of the orbit is thinner and more likely to shatter completely. Other features commonly encountered with fractures of the orbit include enophthalmos, in which the eye appears to recede into the orbit, and orbital dystopia, in which the eye on the affected side appears lower in the horizontal plane relative to the unaffected side 9.
Nasal fractures
Evidence of a nasal fracture includes epistaxis, swelling, tenderness, deformity, crepitus, nasal airway obstruction, and periorbital ecchymosis.
Always evaluate for septal deviation or septal hematoma. A bulging, bluish, tender septal mass requires evacuation. Failure to do so can result in necrosis of the nasal septum. Widening of the intercanthal distance suggests the possibility of a nasoorbitoethmoid fracture.
Zygomatic and zygomaticomaxillary complex fractures
Impingement of the temporalis muscle may result in trismus, although this is only occasionally observed.
Depression of the inferior orbital rim, paresthesia in the distribution of the infraorbital nerve, or diplopia suggests extension into the orbit or maxilla.
Maxillary (Le Fort) fractures
Physical examination findings include facial distortion in the form of an elongated face, a mobile maxilla, or mid-face instability and malocclusion.
Mandibular fractures
In a report, Schwab et al 17 looked at physical examination characteristics that predicted a mandibular fracture. The tongue blade test assesses the ability of patients to grasp a tongue depressor in between the teeth and patients’ ability to hold the blade against mild resistance by the examiner on each hemimandible.
Inability to hold the tongue depressor had a negative predictive value of 96%, whereas malocclusion had an negative predictive value of 87%; facial asymmetry, 76%; and trismus, 75% 17.
Facial fracture diagnosis
Facial fractures that necessitate urgent evaluation and management include 16:
- Nasoethmoid fractures to monitor for cerebrospinal fluid (CSF) leak and possible complications including meningitis
- Zygomatic arch fractures associated with trismus to observe for potential airway complications
- LeFort-type fractures of the midface requiring surgical repair
- Facial fractures in patients with multiple other significant injuries
- Tripod fractures associated with ocular findings require emergent ophthalmologic evaluation and management
Imaging studies
Generally, computed tomography (CT) scanning utilizing fine cuts and both coronal and sagittal reconstructions is the study of choice when evaluating facial fractures because visualization of fractures among the complex curves of facial bones is best achieved using this modality. (Ref 29) Radiographic evaluation, however, should not be substituted for a complete external and internal examination 18.
- Frontal sinus fractures: Plain posteroanterior, lateral, and Waters radiographic projections demonstrate the fracture, whereas a CT scan with a thin 2-mm cut through the sinuses demonstrates the anatomy, the integrity of the posterior wall, and any pneumocephali that are pathognomonic for a posterior wall fracture.
- Orbital fractures: Facial CT scanning in the axial and coronal planes with thin cuts through the orbits is the study of choice. Herniation of the orbital contents into the maxillary sinus, observed as clouding of the maxillary sinuses on plain radiographs, suggests an orbital floor fracture.
- Nasal fractures: Radiographs are not usually necessary to diagnose this injury. Plain radiographs, moreover, are often not helpful in diagnosing nasal fractures in children since the nasal bones of children are poorly visualized on plain radiograph because they are not fused and are composed primarily of cartilage. [16] However, plain nasal radiographs that consist of a lateral view that cones down on the nose and a Waters view can confirm the diagnosis. If a nasoorbitoethmoid fracture is suspected, facial CT scanning confirms the diagnosis.
- Zygomatic and zygomaticomaxillary fractures: If a fracture is suspected, a facial CT scan with coronal and axial cuts elucidates the injury. A plain Waters view may be used as a scout radiograph.
- Maxillary (Le Fort) fractures: These fractures are very difficult to assess with plain radiography. If the clinical examination findings are equivocal, then a plain Waters image may provide additional information; otherwise, facial CT scanning with coronal and axial cuts is the criterion standard. Radiographically, Le Fort 1 fracture is the only one of the 3 Le Fort fractures to involve the nasal fossa; Le Fort 2 fracture is the only one of the 3 Le Fort fractures to involve the inferior orbital rim; and Le Fort 3 fracture is the only one of the 3 Le Fort fractures to involve the zygomatic arch 10.
- Mandibular fractures: The study of choice is panoramic radiography. Simple radiographs of the mandible are less sensitive for detecting fractures when compared to panoramic radiographs and can miss condylar fractures 16. If this study is not available, then a mandibular series consisting of a right and left lateral oblique, posteroanterior, and Towne view may be obtained. Fractures of the condyle may require coronal plane CT scanning. A case series of 102 mandible fractures assessed by CT scanning demonstrated 42 percent involved only a single fracture rather than a pair of fractures as traditional teaching usually states 16.
Laboratory studies
Consider ordering preoperative laboratory studies, such as a complete blood cell (CBC) count, prothrombin time/active partial thromboplastin time (PT/aPTT), and blood type and crossmatch, for the consulting surgeon.
Other tests
CSF rhinorrhea
- Two methods exist to determine if CSF is present in nasal or ear secretions. The first involves placing a drop of the nasal fluid onto filter paper or a bed sheet. The CSF migrates farther than blood, forming a target shape with blood in the center and blood-tinged CSF on the outer ring.
- An additional way to delineate CSF is by checking the glucose content of the nasal fluid as compared to the patient’s serum. CSF generally contains 60% of the glucose of serum, and nasal mucus contains none. Keep in mind that neither of these tests is sensitive or specific.
Foreign-body aspiration
Chest radiography may assist in detecting aspiration of a foreign body.
Spinal injuries
A cervial spine series detects any bony injuries to the cervical spine.
Facial fracture treatment
Once a fracture has been identified, an appropriate surgeon or specialist (ie, plastic surgeon; ophthalmologist; ear, nose, and throat specialist; oral-maxillofacial surgeon; or neurosurgeon) provides the definitive care. Special consideration should be given to the athlete who suffers a traumatic injury that involves the globe—emergent evaluation by an ophthalmologist is recommended 19.
Nasal packing
If the mid face is stable, the nares can be treated with drops of a vasoconstrictor (eg, Afrin) and packed with gauze.
If the mid face is unstable, this method does not work. Instead, insert a Foley catheter into the nares and inflate the balloon with air. Gently pull the balloon back to close off the posterior choanae. Then, pack the nasal chamber with gauze.
Lateral canthotomy
Lateral canthotomy can help relieve intraocular pressure if the physical examination reveals a proptotic and tense globe, which is suggestive of a retrobulbar hematoma. Using local anesthetic, an incision is made on the lateral canthus between the upper and lower eyelid to the orbital bone.
Temporomandibular joint reduction
The mandible dislocates forward and superiorly. Reduction is performed by placing gauze-covered thumbs on the third molars of the mandible with the fingers curled under the symphysis of the mandible. Then, downward pressure is exerted on the molars, with slight upward pressure on the symphysis to lever the condyles downward. A relaxant (eg, diazepam) may be useful if the muscle spasms. If the injury is trauma related, obtain a radiograph to rule out the presence of a fracture.
Frontal fracture
Repair of the anterior wall may be delayed, but posterior wall fractures require immediate neurosurgical evaluation. The decision regarding whether prophylaxis with antibiotics is needed should be left to the consulting surgeon.
Orbital fracture
The initial treatment is generally supportive, including head elevation, ice, and analgesics. The indications for surgical repair are controversial and may include diplopia that persists 2 weeks after the injury, large fractures, and enophthalmos. Orbital fractures that result in inferior rectus muscle entrapment, inferior orbital nerve entrapment, enophthalmos, or orbital dystopia may result in both cosmetic and functional impairment and should be referred to a specialist (ie, ophthalmologist, oral-maxillofacial surgeon, or plastic surgeon) within 24 hours to insure prompt resolution 9. Orbital fractures that involve a sinus should receive antibiotic prophylaxis 19.
Nasal fracture
An angulated nasal fracture can be reduced by exerting firm, quick pressure with the thumbs toward the midline or by inserting a soft probe in the nares to elevate the depressed or deviated septum into anatomic position 20. Ongoing management of these injuries consists of control of epistaxis and supportive care with analgesics. Operative repair is best performed early, within 1-2 hours following the injury, or in 10-14 days following the injury once the swelling and edema has receded. Any open wounds require antibiotics.
Zygomatic and zygomaticomaxillary fracture
Open reduction and internal fixation to restore the normal contour is the standard of care.
Maxillary (Le Fort) fracture
Open reduction with internal fixation is the standard. If CSF rhinorrhea is present, a neurosurgeon should be consulted. Prophylactic antibiotics are warranted if the fracture extends through the tooth-bearing region or through the nasal or sinus mucosa.
Mandibular fracture
Most cases require admission with fixation. These fractures often require antibiotics because of their location in the tooth-bearing region. Penicillin or clindamycin are acceptable choices.
Facial fractures recovery
Evidence-based research to recommend return to play for athletes who have sustained facial fractures is lacking. Studies have demonstrated that bone healing begins with an inflammatory reaction hematoma stage for up to 5 days following the fracture, followed by callus formation stage 4-40 days following the fracture, and the remodeling stage occurring 25-50 days after the fracture. Based on this healing schedule, it has been recommended that the athlete not participate in activity for the first 20 days following the fracture, light activity days 21-30, noncontact drills days 31-40, and lastly, full-contact training and game play after day 41. The exception to this rule is combat sports in which return to activity is recommended no sooner than 3 months following the fracture 10.
In fractures that involve or approximate the eye, visual acuity is the most important factor in return to play. Any unexplained loss of acuity needs a complete workup. The aforementioned 20/40 criteria to play still apply. Any athlete returning to competition without complete bone healing needs adequate protection, such as a full face shield, modified batting helmets, extended hockey eye visors, or larger football face masks.
Athletes need to regain their confidence in returning to play. An athlete who has physically recovered may not be mentally recovered from the trauma of the injury and, thus, is at risk of further injury. This is often observed in baseball players hit in the face by a pitch or hit ball. Psychologic recovery from facial fractures can be assessed in controlled practice situations. A consultation with a sports psychologist may be necessary if difficulties linger.
Return-to-play recommendations are not affected after orofacial fractures 21.
References- Costello BJ, Papadopoulos H, Ruiz R. Pediatric craniomaxillofacial trauma. Clin Pediatr Emerg Med. 2005. 6(1):32-40.
- Boden BP, Tacchetti R, Mueller FO. Catastrophic injuries in high school and college baseball players. Am J Sports Med. 2004 Jul-Aug. 32(5):1189-96.
- Hwang K, You SH. Analysis of facial bone fractures: An 11-year study of 2,094 patients. Indian J Plast Surg. 2010;43 (1): 42-8. doi:10.4103/0970-0358.63959
- Facial fractures. https://emedicine.medscape.com/article/84613-overview
- How to Convert Newtons to G-Force. https://sciencing.com/convert-newtons-gforce-8720337.html
- Iida S, Kogo M, Sugiura T, Mima T, Matsuya T. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg. 2001 Aug. 30(4):286-90.
- Bak MJ, Doerr TD. Craniomaxillofacial fractures during recreational baseball and softball. J Oral Maxillofac Surg. 2004 Oct. 62(10):1209-12.
- Reyes Mendez D, Lapointe A. Nasal trauma and fractures in children. UpToDate. May 2007.
- Neuman MI, Bachur RG. Orbital fractures. UpToDate. September 2006.
- Reehal P. Facial injury in sport. Curr Sports Med Rep. 2010 Jan-Feb. 9(1):27-34.
- Le Fort R. Étude expérimentale sur les fractures de la machoire supérieure (Part l) Rev Chir. 1901;23:208–227
- Dreizin D, Nam AJ, Diaconu SC, Bernstein MP, Bodanapally UK, Munera F. Multidetector CT of Midfacial Fractures: Classification Systems, Principles of Reduction, and Common Complications. (2018) Radiographics : a review publication of the Radiological Society of North America, Inc. 38 (1): 248-274. doi:10.1148/rg.2018170074
- Hopper RA, Salemy S, Sze RW. Diagnosis of midface fractures with CT: what the surgeon needs to know. Radiographics. 2006;26 (3): 783-93. doi:10.1148/rg.263045710
- Laskin DM. Protecting the faces of America. J Oral Maxillofac Surg. 2000 Apr. 58(4):363.
- Navarro RR. Protective equipment and the prevention of concussion – what is the evidence?. Curr Sports Med Rep. 2011 Jan-Feb. 10(1):27-31.
- Initial evaluation and management of facial trauma in adults. https://www.uptodate.com/contents/initial-evaluation-and-management-of-facial-trauma-in-adults
- Schwab RA, Genners K, Robinson WA. Clinical predictors of mandibular fractures. Am J Emerg Med. 1998 May. 16(3):304-5.
- Nasal trauma and fractures in children. https://www.uptodate.com/contents/nasal-trauma-and-fractures-in-children
- Neuman MI, Bachur RG. Orbital fractures. Up To Date. Accessed: July 5, 2013.
- Romeo SJ, Hawley CJ, Romeo MW, Romeo JP. Facial injuries in sports: a team physician’s guide to diagnosis and treatment. Phys Sportsmed. 2005 Apr. 33(4):45-53.
- Tesini DA, Soporowski NJ. Epidemiology of orofacial sports-related injuries. Dent Clin North Am. 2000 Jan. 44(1):1-18, v.