Fentanyl
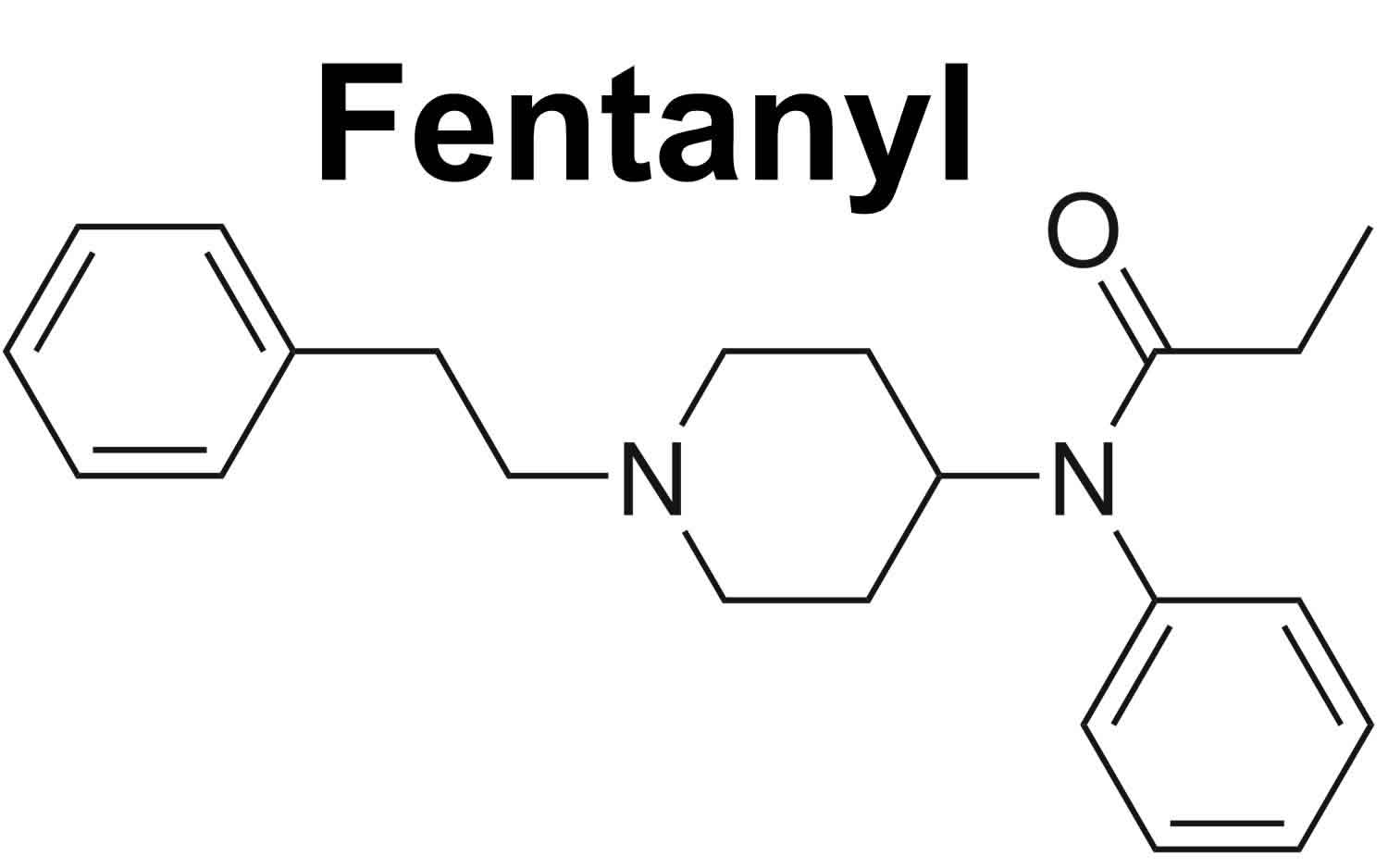
Fentanyl is a powerful synthetic opioid (synthetic phenylpiperidine) that is similar to morphine but is 50 to 100 times more potent 1. Fentanyl is in a class of medications called narcotic (opiate) analgesics. Opioids are a group of medicines that may be prescribed by a doctor to treat pain. Opioids work by interacting with the opioid receptors in your brain. Like morphine, fentanyl is an agonist for the µ (mu) type opiate receptors which are found in the central nervous system but also on heart, lung, vascular and intestinal cells 2. Opioids reduce feelings of pain by interrupting the way nerves signal pain between your brain and your body. Fentanyl is a prescription opioid drug that is also made and used illegally or obtained illegally for non-prescribed use. Like morphine, fentanyl is a medicine that is typically used to treat patients with severe acute pain caused by major trauma or surgery 3. Fentanyl is used as needed to treat breakthrough pain but not more often than four times a day. Fentanyl also reduces the anxiety and stress caused by pain. Fentanyl is also sometimes used to treat patients with chronic (long-term) pain caused by cancer who are physically tolerant to other opioids 4. Tolerance occurs when you need a higher and/or more frequent amount of a drug to get the desired effects. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. How long you need to take fentanyl for will depend on why it has been prescribed. For example, fentanyl patches for cancer pain or in people receiving palliative care are approved for life-long use, while fentanyl used in acute pain or anesthesia will be used only for a short time. Talk to your doctor about the risks of using fentanyl.
Current fentanyl indications are as an adjunct (add-on) to general anesthesia (intravenous, epidural or intrathecal) and for management of moderate-to-severe pain that is not responsive to nonopiate analgesics. Fentanyl is available in multiple formulations, including solutions for injection in multiple concentrations for anesthesia and acute pain management, and as transdermal patches, a sublingual (underneath the tongue) tablet (Abstral) and a lozenge on a handle (Actiq), a film (Onsolis), and a buccal (between the gum and cheek) tablet (Fentora) to dissolve in the mouth and nasal sprays for management of chronic pain. Fentanyl is available generically and under commercial names including Sublimaze (solution for injection), Duragesic and Ionsys (transdermal patches), Actiq and Fentora (lollipop and tablets for transmucosal delivery) in multiple dose formulations. Swallow the buccal tablet whole; do not split, chew, or crush. Also do not chew or bite the lozenge on a handle; only suck on this medication as directed.
Your doctor will probably start you on a low dose of fentanyl and gradually increase your dose until you find the dose that will relieve your breakthrough pain. If you still have pain 30 minutes after using fentanyl films (Onsolis), your doctor may tell you to use another pain medication to relieve that pain, and may increase your dose of fentanyl films (Onsolis) to treat your next episode of pain. Talk to your doctor about how well fentanyl is working and whether you are experiencing any side effects so that your doctor can decide whether your dose should be adjusted.
Do not use fentanyl more than four times a day. Call your doctor if you experience more than four episodes of breakthrough pain per day. Your doctor may need to adjust the dose of your other pain medication(s) to better control your pain.
Do not stop using fentanyl without talking to your doctor. Your doctor may decrease your dose gradually. If you suddenly stop using fentanyl, you may experience unpleasant withdrawal symptoms.
Side effects of fentanyl resemble those of other opioids (e.g., heroin) and include sedation, respiratory depression (which, if extensive and untreated, may lead to arrest), confusion, euphoria, agitation, dizziness, headache, drowsiness, nausea and vomiting, visual disturbances, dyskinesia, hallucinations, delirium, a subset of the latter known as “narcotic delirium,” analgesia, constipation, narcotic ileus, muscle rigidity, diarrhea, abdominal bloating, addiction, loss of consciousness, hypotension, coma, and even death. Fentanyl and its congeners (phenylpiperidine analogues of fentanyl, e.g., alfentanil, remifentanil and sufentanil) are controlled substances and classified as Schedule 2 drugs, indicating that they have medical usefulness, but also a high potential for physical and psychological dependency and abuse. Indeed, deaths have been reported due to fentanyl patches and transbuccal formulations either from inadvertent overdose, accidental ingestion (by children for instance) or abuse. Synthetic opioids, including fentanyl, are now the most common drugs involved in drug overdose deaths in the United States. In 2017, 59 percent of opioid-related deaths involved fentanyl compared to 14.3 percent in 2010 5. Rates of overdose deaths involving synthetic opioids other than methadone, which includes fentanyl and fentanyl analogs, increased over 16% from 2018 to 2019. Overdose deaths involving synthetic opioids were nearly 12 times higher in 2019 than in 2013. More than 36,000 people died from overdoses involving synthetic opioids in 2019 6. The latest provisional drug overdose death counts through May 2020 suggest an acceleration of overdose deaths during the COVID-19 pandemic 7.
Alcohol and other drugs (i.e., cocaine, heroin) can synergistically exacerbate fentanyl’s side effects, creating multi-layered clinical scenarios that can be complex to manage. These substances, taken together, generate undesirable conditions that complicate the patient’s prognosis 8.
Fentanyl may be habit forming, especially with prolonged use. Use fentanyl exactly as directed. Do not use a larger dose of fentanyl, use the medication more often, or use it for a longer period of time than prescribed by your doctor. While using fentanyl, discuss with your health care provider your pain treatment goals, length of treatment, and other ways to manage your pain. Tell your doctor if you or anyone in your family drinks or has ever drunk large amounts of alcohol, uses or has ever used street drugs, or has overused prescription medications, or has had an overdose, or if you have or have ever had depression or another mental illness. There is a greater risk that you will overuse fentanyl if you have or have ever had any of these conditions. Talk to your health care provider immediately and ask for guidance if you think that you have an opioid addiction or call the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-HELP.
Fentanyl should only be prescribed by doctors who are experienced in treating pain in cancer patients. It should be used only to treat breakthrough cancer pain (sudden episodes of pain that occur despite around-the-clock treatment with pain medication) in cancer patients at least 18 years of age (or at least 16 years of age if using Actiq brand lozenges) who are taking regularly scheduled doses of another narcotic (opiate) pain medication, and who are tolerant (used to the effects of the medication) to narcotic pain medications. This medication should not be used to treat pain other than chronic cancer pain, especially short-term pain such as migraines or other headaches, pain from an injury, or pain after a medical or dental procedure. Fentanyl may cause serious breathing problems or death if it is used by people who are not being treated with other narcotic medications or who are not tolerant to narcotic medications.
Fentanyl may cause serious harm or death if used accidentally by a child or by an adult who has not been prescribed the medication. Even partially used fentanyl may contain enough medication to cause serious harm or death to children or other adults. Keep fentanyl out of reach of children, and if you are using the lozenges, ask your doctor how to obtain a kit from the manufacturer containing child safety locks and other supplies to prevent children from getting the medication. Dispose of partially used lozenges according to the manufacturer’s directions immediately after you remove them from your mouth. If fentanyl is used by a child or an adult who has not been prescribed the medication, try to remove the medication from the person’s mouth and get emergency medical help.
Fentanyl should be used along with your other pain medication(s). Do not stop taking your other pain medication(s) when you begin your treatment with fentanyl. If you stop taking your other pain medication(s) you will need to stop using fentanyl.
If you still have pain after using one lozenge or tablet, your doctor may tell you to use a second lozenge or tablet. You may use the second lozenge (Actiq) 15 minutes after you finish the first lozenge, or use the second tablet (Abstral, Fentora) 30 minutes after you started using the first tablet. Do not use a second lozenge or tablet to treat the same episode of pain unless your doctor tells you that you should. If you are using fentanyl film (Onsolis), you should not use a second dose to treat the same episode of pain. After you treat an episode of pain using 1 or 2 doses of fentanyl as directed, you must wait at least 2 hours after using fentanyl (Abstral or Onsolis) or 4 hours after using fentanyl (Actiq or Fentora) before treating another episode of breakthrough cancer pain.
Taking certain medications with fentanyl may increase the risk that you will develop serious or life-threatening breathing problems, sedation, or coma. Tell your doctor if you are taking any of the following medications: amiodarone (Nexterone, Pacerone); certain antibiotics such as clarithromycin (Biaxin, in PrevPac), erythromycin (Erythocin), telithromycin (Ketek), and troleandomycin (TAO) (not available in the US); certain antifungals such as fluconazole (Diflucan), itraconazole (Onmel, Sporanox), and ketoconazole (Nizoral); aprepitant (Emend); benzodiazepines such as alprazolam (Xanax), chlordiazepoxide (Librium), clonazepam (Klonopin), diazepam (Diastat, Valium), estazolam, flurazepam, lorazepam (Ativan), oxazepam, temazepam (Restoril), and triazolam (Halcion); cimetidine (Tagamet); diltiazem (Cardizem, Taztia, Tiazac, others); certain medications for human immunodeficiency virus (HIV) such as amprenavir (Agenerase), fosamprenavir (Lexiva), indinavir (Crixivan), nelfinavir (Viracept), ritonavir (Norvir, in Kaletra), and saquinavir (Invirase); medications for mental illness and nausea; muscle relaxants; nefazodone; sedatives; sleeping pills; tranquilizers; or verapamil (Calan, Covera, Verelan). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you use fentanyl with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Fentanyl comes as four different transmucosal products and several other types of products. The medication in each product is absorbed differently by the body, so one product cannot be substituted for any other fentanyl product. If you are switching from one product to another, your doctor will prescribe a dose that is best for you.
A program has been set up for each fentanyl product to decrease the risk of using the medication. Your doctor will need to enroll in the program in order to prescribe fentanyl and you will need to have your prescription filled at a pharmacy that is enrolled in the program. As part of the program, your doctor will talk with you about the risks and benefits of using fentanyl and about how to safely use, store, and dispose of the medication. After you talk with your doctor, you will sign a form acknowledging that you understand the risks of using fentanyl and that you will follow your doctor’s instructions to use the medication safely. Your doctor will give you more information about the program and how to get your medication and will answer any questions you have about the program and your treatment with fentanyl.
Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with fentanyl and each time you get more medication. Read the information carefully and ask your doctor or pharmacist if you have any questions. You can also visit the Food and Drug Administration (FDA) website (https://www.fda.gov/drugs/drug-safety-and-availability/medication-guides) or the manufacturer’s website to obtain the Medication Guide.
Fentanyl special precautions
The presence of other medical problems may affect the use of fentanyl. Make sure you tell your doctor if you have any other medical problems, especially:
- Adrenal problems or
- Brain tumor, history of or
- Breathing or lung problems (eg, COPD, respiratory depression, sleep apnea) or
- Cor pulmonale (serious heart condition) or
- Drug dependence, especially with narcotics, or history of or
- Head injury, history of or
- Heart disease or
- Hypokalemia (low potassium levels in the blood) or
- Hypomagnesemia (low magnesium levels in the blood)—Use with caution. May increase risk for more serious side effects.
- Bradycardia (slow heart rhythm) or
- Gallbladder problems or
- Heart rhythm problems (eg, QT prolongation) or
- Hypertension (high blood pressure) or
- Hypotension (low blood pressure) or
- Pancreatitis (inflammation or swelling of the pancreas) or
- Seizures, history of—Use with caution. May make these conditions worse.
- Kidney disease or
- Liver disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
Before using fentanyl:
- tell your doctor and pharmacist if you are allergic to fentanyl patches, injection, nasal spray, tablets, lozenges, or films; any other medications; or any of the ingredients in fentanyl tablets, lozenges, or films. Ask your pharmacist or check the Medication Guide for a list of the ingredients.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, and nutritional supplements you are taking or plan to take. Be sure to mention the medications listed in the IMPORTANT WARNING section and any of the following medications: antihistamines; barbiturates such as phenobarbital; buprenorphine (Buprenex, Subutex, in Suboxone); butorphanol (Stadol); carbamazepine (Carbatrol, Epitol, Tegretol); efavirenz (Sustiva, in Atripla); modafinil (Provigil); nalbuphine (Nubain); naloxone (Evzio, Narcan); nevirapine (Viramune); oral steroids such as dexamethasone, methylprednisolone (Medrol), and prednisone (Rayos); oxcarbazepine (Trileptal); pentazocine (Talwin); phenytoin (Dilantin, Phenytek); pioglitazone (Actos, in Actoplus Met, in Duetact); rifabutin (Mycobutin); and rifampin (Rifadin, Rimactane, in Rifamate, in Rifater). Also tell your doctor or pharmacist if you are taking any of the following medications or if you have stopped taking them within the past two weeks: monoamine oxidase (MAO) inhibitors including isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor what herbal products you are taking, especially St. John’s wort.
- tell your doctor if you or anyone in your family drinks or has ever drunk large amounts of alcohol or uses or has ever used street drugs or excessive amounts of prescription medications. Also tell your doctor if you have or have ever had a head injury, a brain tumor, a stroke, or any other condition that caused high pressure inside your skull; seizures; slowed heartbeat or other heart problems; low blood pressure; mental problems such as depression, schizophrenia (a mental illness that causes disturbed or unusual thinking, loss of interest in life, and strong or inappropriate emotions), or hallucinations (seeing things or hearing voices that do not exist); breathing problems such as asthma and chronic obstructive pulmonary disease (COPD; a group of lung diseases that includes chronic bronchitis and emphysema); or kidney or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while using fentanyl, call your doctor.
- you should know that fentanyl may decrease fertility in men and women. Talk to your doctor about the risks of using fentanyl.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are using fentanyl.
- you should know that fentanyl may make you drowsy or dizzy. Do not drive a car or operate machinery until you know how this medication affects you.
you should know that fentanyl may cause dizziness, lightheadedness, and fainting when you get up too quickly from a lying position. This is more common when you first start using fentanyl. To avoid this problem, get out of bed slowly, resting your feet on the floor for a few minutes before standing up. - if you have diabetes, you should know that each fentanyl lozenge (Actiq) contains about 2 grams of sugar.
- if you will be using the lozenges (Actiq), talk to your dentist about the best way to care for your teeth during your treatment. The lozenges contain sugar and may cause tooth decay and other dental problems.
- you should know that fentanyl may cause constipation. Talk to your doctor about changing your diet and using other medications to treat or prevent constipation.
Check with your doctor at regular times while using fentanyl. Be sure to report any side effects. It is very important that your doctor check your or your child’s progress while using fentanyl. This will allow your doctor to see if fentanyl is working properly and to decide if you should continue to take it. Blood and urine tests may needed to check for unwanted effects.
Do not touch the sticky side of the patch or the gel. Fentanyl can be quickly absorbed through your eyes and mouth and can be extremely dangerous. If you do touch the sticky side of the fentanyl patch or gel, let your nurse or doctor know right away and rinse the area with large amounts of water. Do not use soaps or other cleansers.
After you have been using fentanyl for awhile, “breakthrough” pain may occur more often than usual, and it may not be relieved by your regular dose of fentanyl. If this occurs, do not increase the amount of fentanyl skin patch or other narcotic that you are using without first checking with your doctor.
Fentanyl will add to the effects of alcohol and other central nervous system (brain and spinal cord) depressants. Central nervous system depressants are medicines that slow down the nervous system, which may cause drowsiness or make you less alert. Some examples of central nervous system depressants are antihistamines or medicine for hay fever, other allergies, or colds, sedatives, tranquilizers, or sleeping medicine, other prescription pain medicine or narcotics, benzodiazepines, medicine for seizures or barbiturates, muscle relaxants, or anesthetics, including some dental anesthetics. This effect may last for a few days after you stop using this medicine. Check with your doctor before taking any of the medicines listed while you are using this medicine.
The Ionsys® patch must be removed before a procedure called a magnetic resonance imaging (MRI) scan. It may cause skin burns if left in place during the procedure.
The Ionsys® patch may cause serious skin reactions. Call you doctor right away if you have blistering, lesions, a rash, redness, or swelling of the skin, especially at the site of application.
Fentanyl may cause some people to become drowsy, dizzy, or lightheaded, or to feel a false sense of well-being. Do not drive or do anything else that could be dangerous until you know how this medicine affects you. These effects usually go away after a few days of treatment, when your body gets used to the medicine. However, check with your doctor if drowsiness that is severe enough to interfere with your activities continues for more than a few days.
Dizziness, lightheadedness, or even fainting may occur when you get up suddenly from a lying or sitting position. Getting up slowly may help lessen this problem. Also, lying down for a while may relieve dizziness or lightheadedness.
Nausea or vomiting may occur, especially during the first several days of treatment. Lying down for a while may relieve these effects. However, if they are especially bothersome or if they continue for more than a few days, check with your doctor. You may be able to take another medicine to help prevent these problems.
Using narcotics for a long time may cause severe constipation. To prevent this, your doctor may direct you to take laxatives, drink a lot of fluids, or increase the amount of fiber in your diet. Be sure to follow the directions carefully, because continuing constipation can lead to more serious problems.
Heat can cause the fentanyl in the patch to be absorbed into your body faster. This may increase the chance of serious side effects or an overdose. While you are using this medicine, do not use a heating pad, electric blanket, heat or tanning lamps, sauna, a sunlamp, or a heated water bed, and do not sunbathe, or take long baths or showers in hot water. Also, check with your doctor if you get a fever.
Be careful about letting other people come in contact with your patch. The patch could stick to someone else, such as when you hug them or if someone helps you put the patch on. If any medicine gets on another person, wash it off right away with clear water.
Before having any kind of surgery (including dental surgery) or emergency treatment, tell the medical doctor or dentist in charge that you are using fentanyl. Serious side effects can occur if your medical doctor or dentist gives you certain other medicines without knowing that you are using fentanyl.
You may bathe, shower, or swim while wearing a fentanyl skin patch. However, be careful to wash and dry the area around the patch gently. Rubbing may cause the patch to get loose or come off. If this does occur, throw away the patch and apply a new one in a different place. Make sure the area is completely dry before applying the new patch.
If you have been using fentanyl regularly for several weeks or more, do not suddenly stop using it without first checking with your doctor. You may be directed to gradually reduce the amount you are using before stopping treatment completely to lessen the chance of withdrawal side effects.
Using too much fentanyl skin patch, or taking too much of another narcotic with fentanyl skin patch, may cause an overdose. If this occurs, get emergency help right away. An overdose can cause severe breathing problems (breathing may even stop), unconsciousness, and death. Serious signs of an overdose include: very slow breathing (fewer than 8 breaths a minute) and drowsiness that is so severe that you are not able to answer when spoken to, or, if asleep, cannot be awakened. Other signs of an overdose may include: cold, clammy skin, low blood pressure, pinpoint pupils of the eyes, and slow heartbeat. It may be best to have a family member or a friend check on you several times a day when you start using a narcotic regularly, and whenever your dose is increased, so that he or she can get help for you if you cannot do so yourself.
Fentanyl may cause sleep-related breathing problems (e.g., sleep apnea, sleep-related hypoxemia). Your doctor may decrease your dose if you have sleep apnea (stop breathing for short periods during sleep) while using this medicine.
Do not use a fentanyl patch if you have taken a monoamine oxidase (MAO) inhibitor in the past 2 weeks. Some examples of MAO inhibitors are isocarboxazid (Marplan®), phenelzine (Nardil®), selegiline (Eldepryl®), and tranylcypromine (Parnate®). If you use the 2 medicines close together it may cause serious side effects like confusion, agitation, restlessness, stomach or intestinal symptoms, a sudden high temperature, an extremely high blood pressure, or severe convulsions.
Check with your doctor right away if you have anxiety, restlessness, a fast heartbeat, fever, sweating, muscle spasms, twitching, nausea, vomiting, diarrhea, or see or hear things that are not there. These may be symptoms of a serious condition called serotonin syndrome. Your risk may be higher if you also take certain other medicines that affect serotonin levels in your body.
Using fentanyl while you are pregnant may cause serious unwanted effects, including neonatal opioid withdrawal syndrome in your newborn baby. Tell your doctor right away if you think you are pregnant or if you plan to become pregnant while using fentanyl.
Using too much of fentanyl may cause reduced infertility (unable to have children). Talk with your doctor before using fentanyl if you plan to have children.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Fentanyl and pregnancy
Very little is known about how fentanyl might affect a baby’s development in the womb and it is therefore not possible to say that it is safe. Fentanyl is generally not recommended during pregnancy. In early pregnancy, it’s been linked to some problems for your baby. If you take fentanyl at the end of pregnancy there’s a risk that your baby may get withdrawal symptoms or be born addicted to fentanyl. However, it’s important to treat severe pain in pregnancy. For some pregnant women with severe pain, fentanyl might be the best option. Any assessment of safety needs to weigh up the risks and benefits to both mother and baby of using fentanyl against those of not using fentanyl. The outcome of this assessment will vary from person to person and will depend on the severity of the mother’s condition. Your doctor is the best person to help you decide what’s right for you and your baby.
When deciding whether to use fentanyl during pregnancy it is therefore important to weigh up how necessary it is to your health against any possible risks to you or your baby, some of which might depend on how many weeks pregnant you are.
Recreational use of fentanyl in pregnancy is not advised as there is no benefit to the health of the mother or baby in this context. Recreational fentanyl use also carries a high risk of overdose and death. If you are pregnant and use fentanyl recreationally it is important that your doctor or midwife is aware of this. If necessary, they will be able to get you help and support to safely stop using fentanyl.
Can using fentanyl in early pregnancy cause my baby to be born with birth defects?
A baby’s body and most internal organs are formed during the first 12 weeks of pregnancy. It is mainly during this time that some medicines are known to cause birth defects.
There are currently no large scientific studies that have investigated whether fentanyl use during the first trimester of pregnancy can cause birth defects in the baby. Experts have been able to identify case studies of only four babies who were born to pregnant women who used fentanyl in the first trimester. None of these babies had birth defects, however information on many more pregnancies needs to be collected before it is possible to accurately assess whether fentanyl causes birth defects.
Can taking fentanyl in pregnancy cause miscarriage, stillbirth, preterm birth, or my baby to be small at birth (low birth weight)?
No studies have specifically analysed whether these outcomes are more or less common in pregnant women taking fentanyl.
Can using fentanyl in pregnancy cause other health problems in the baby/child?
Withdrawal symptoms at birth
Withdrawal symptoms are thought to occur as the newborn baby’s body has to adapt to no longer getting certain types of medicines through the placenta. Medicines related to fentanyl are known to increase the risk of withdrawal symptoms in the baby when used around the time of delivery.
There are a small number of reports in the scientific literature of babies who had withdrawal symptoms after being exposed to fentanyl in the womb. If you have used fentanyl regularly in pregnancy it is important to let your doctor or midwife know as it might be advisable that your baby is born in a unit with facilities to monitor and treat withdrawal symptoms if necessary.
Learning and behavioural problems in the child
A baby’s brain continues to develop right up until the end of pregnancy. It is therefore possible that taking certain medicines at any stage of pregnancy could have a lasting effect on a child’s learning or behavior.
There are no studies that have been specifically designed to investigate whether fentanyl exposure in the womb might affect a child’s learning and behaviour. Nearly all medicines still need to be studied to determine whether exposure in the womb might affect a child’s learning or behaviour.
Will I or my baby need extra monitoring during pregnancy?
Most women will be offered a scan at around 20 weeks of pregnancy to look for birth defects as part of their routine antenatal care.
Because the effects of taking fentanyl in early pregnancy are largely unknown, your doctor may suggest extra monitoring of your baby, including more detailed or earlier scans to detect birth defects, and more frequent reviews of your baby’s growth in the womb.
Women with some of the underlying conditions that fentanyl can be used to treat might be more closely monitored to ensure that their baby is growing and moving as expected. Women who use fentanyl recreationally might also receive extra monitoring.
Fentanyl and breastfeeding
Fentanyl is not usually recommended if you’re breastfeeding. Small amounts of fentanyl pass into breast milk and can cause breathing problems for your baby. Speak to your doctor as they may want to recommend a different painkiller.
The results of studies on the effect of epidural fentanyl on breastfeeding initiation and duration are mixed and controversial, because of the many different combinations of drugs, dosages and patient populations studied as well as the variety of techniques used and deficient designs of many of the studies. It has been suggested that a cumulative dose of over 150 mcg of fentanyl during labor and delivery reduces breastfeeding success 9, but another study found no marked decrease in breastfeeding success with doses above 150 mcg in motivated women with previous breastfeeding success 10. In infants placed skin-to-skin after a normal vaginal delivery, epidural fentanyl given during labor may delay the infant’s first suckling in a dose-dependent manner 11, perhaps because it can persist in the infant’s serum for over 24 hours after discontinuation 12. However, it appears that with good breastfeeding support, epidural fentanyl plus bupivacaine has little overall effect on breastfeeding success 13.
No waiting period or discarding of milk is required before resuming breastfeeding after fentanyl is used for short procedures (e.g., for endoscopy) 14. After general anesthesia, breastfeeding can be resumed as soon as the mother has recovered sufficiently from anesthesia to nurse. When a combination of anesthetic agents is used for a procedure, follow the recommendations for the most problematic medication used during the procedure. Limited information indicates that transdermal fentanyl in a dosage of 100 mcg/hour results in undetectable fentanyl concentrations in breastmilk.
Newborn infants seem to be particularly sensitive to the effects of even small dosages of narcotic analgesics. Once the mother’s milk comes in, it is best to provide pain control with a nonnarcotic analgesic and limit maternal intake of fentanyl to a few days at a low dosage with close infant monitoring 15. If the baby shows signs of increased sleepiness (more than usual), difficulty breastfeeding, breathing difficulties, or limpness, a physician should be contacted immediately.
What special dietary instructions should I follow?
Do not eat grapefruit or drink grapefruit juice while using fentanyl.
Grapefruit juice can increase the amount of fentanyl in your body so it’s a good idea not to drink more than a large glass of it.
It’s best not to drink alcohol when you first start taking or using fentanyl until you see how it affects you.
Fentanyl is not generally affected by food so you can eat normally.
Can I drink alcohol with fentanyl?
It’s best not to drink alcohol when you first start taking or using fentanyl until you see how it affects you.
Drinking alcohol while taking fentanyl will make you more sleepy and increases the risk of serious side effects.
What are the risks associated with fentanyl?
Opioids are strong pain medicines and can cause life-threatening or fatal breathing difficulties. Your doctor will monitor how you use fentanyl to reduce your risk of harm, including through misuse or abuse.
You can also develop tolerance when you take fentanyl — this means that you may need to take larger amounts of the opioid to get the same effect. As the dosage increases, so does the risk of side effects.
Continue to take fentanyl for as long as your doctor tells you to. Suddenly stopping fentanyl can cause withdrawal symptoms.
Fentanyl may make it difficult for you to drive or operate heavy machinery. If you have recently started taking an opioid medication or changed dosage, you may be at higher risk of having an accident.
If your kidney or liver function is impaired, your doctor may decide that fentanyl is not appropriate for you. There are also other factors that may limit your use of fentanyl — for example, if you drink alcohol or take other medicines that can cause drowsiness.
Your doctor is the best person to guide you on whether fentanyl is the right medicine for you, how much you need and how long to take it for.
Who can and cannot take fentanyl?
Fentanyl can be used by most adults.
Some patches can be used in children from the age of 2 years and over. However, young children and older people are more likely to get side effects.
Fentanyl patches are usually only used if you’ve already been taking other strong opioid painkillers. Your doctor will work out how much fentanyl to give you depending on what dose of other opioids you have been taking. This is to reduce the risk of an overdose.
Fentanyl is not suitable for some people. Tell your doctor before starting this medicine if you:
- have ever had an allergic reaction to fentanyl or any other medicines
- have breathing difficulties such as asthma or a lung condition
- are addicted to alcohol or a heavy drinker
- have a head injury or condition that causes fits or seizures
- have irregular heartbeats (arrhythmia)
- have adrenal gland problems
- have kidney or liver problems
- have an enlarged prostate
- have low blood pressure
- are trying to get pregnant, are pregnant or breastfeeding
Can I drive or ride a bike?
Do not drive a car or ride a bike if fentanyl makes you sleepy, gives you blurred vision or makes you feel dizzy, clumsy or unable to concentrate or make decisions.
This may be more likely when you first start on fentanyl but could happen at any time – for example when starting another medicine.
It’s an offence to drive a car if your ability to drive safely is affected. It’s your responsibility to decide if it’s safe to drive. If you’re in any doubt, do not drive.
Even if your ability to drive is not affected, the police have the right to request a saliva sample to check how much fentanyl is in your body.
Are there any alternatives to fentanyl?
Different pain relief medicines are used in different circumstances. If you have been prescribed fentanyl and are still in pain, speak with your doctor about other ways you can manage your pain.
If you have chronic (long-term) pain, your doctor might suggest lifestyle changes to help manage the discomfort. These might include physical fitness and activity pacing, social activities, relaxation techniques and overall health management.
Will fentanyl affect my fertility?
There’s no clear evidence to suggest that fentanyl reduces fertility in women or men.
Speak to a pharmacist or your doctor if you’re trying for a baby. They may want to review your treatment.
Will fentanyl affect my contraception?
Fentanyl does not affect any type of contraception including the combined pill or emergency contraception.
But if fentanyl makes you sick (vomit) your contraceptive pills may not protect you from pregnancy.
If this happens, follow the instructions in the leaflet that comes with your contraceptive pills.
Will recreational drugs affect fentanyl?
If you take recreational drugs, such as cannabis, cocaine and heroin, while you’re taking fentanyl, you’re more likely to get the serious side effects. These include breathing difficulties, heart problems such as high blood pressure, seizure or fits and even going into a coma.
Some recreational drugs, such as cannabis, will also increase the risk of side effects from fentanyl – it may make you feel really sleepy or dizzy.
Taking heroin while you’re on fentanyl is especially dangerous. You’re more likely to get all the side effects of fentanyl.
Tell your doctor if you think you may take recreational drugs while you’re on fentanyl.
How do people use fentanyl?
When prescribed by a doctor, fentanyl can be given as a shot, a patch that is put on a person’s skin, or as lozenges that are sucked like cough drops 16.
The illegally used fentanyl most often associated with recent overdoses is made in labs. This synthetic fentanyl is sold illegally as a powder, dropped on blotter paper like small candies, put in eye droppers and nasal sprays, or made into pills that look like real prescription opioids 17.
Some drug dealers are mixing fentanyl with other drugs, such as heroin, cocaine, methamphetamine, and MDMA. This is because it takes very little to produce a high with fentanyl, making it a cheaper option. This is especially dangerous when people taking drugs don’t realize they might contain fentanyl as a cheap but dangerous additive. They might be taking stronger opioids than their bodies are used to and can be more likely to overdose.
How does fentanyl affect the brain?
Like heroin, morphine, and other opioid drugs, fentanyl works by binding to the body’s opioid receptors, which are found in areas of the brain that control pain and emotions 18. After taking opioids many times, the brain adapts to the drug, diminishing its sensitivity, making it hard to feel pleasure from anything besides the drug. When people become addicted, drug seeking and drug use take over their lives.
Fentanyl’s effects include:
- extreme happiness
- drowsiness
- nausea
- confusion
- constipation
- sedation
- problems breathing
- unconsciousness
Can you overdose on fentanyl?
Yes, a person can overdose on fentanyl. An overdose occurs when a drug produces serious adverse effects and life-threatening symptoms. When people overdose on fentanyl, their breathing can slow or stop. This can decrease the amount of oxygen that reaches the brain, a condition called hypoxia. Hypoxia can lead to a coma and permanent brain damage, and even death.
Can fentanyl use lead to addiction?
Yes, fentanyl is addictive because of its potency. A person taking prescription fentanyl as instructed by a doctor can experience dependence, which is characterized by withdrawal symptoms when the drug is stopped. A person can be dependent on a substance without being addicted, but dependence can sometimes lead to addiction. If you need to take fentanyl for a long time, your body can become tolerant to it. That means you need higher doses to control your pain over time. However, if you’re using fentanyl to relieve pain (rather than using it as a recreational drug) it’s very unlikely you will get addicted to it because you’re not using it to get a “high”. You’re more likely to get addicted if you use fentanyl when you’re not in pain. It is also more likely if you’ve been addicted to alcohol or drugs in the past, or you have severe depression or anxiety.
Addiction is the most severe form of a substance use disorder. Substance use disorders are characterized by compulsive drug seeking and drug use that can be difficult to control, despite harmful consequences. When someone is addicted to drugs, they continue to use them even though they cause health problems or issues at work, school, or home. An substance use disorder can range from mild to severe.
If you’re addicted to fentanyl you may find it difficult to stop using it or feel you want to use it more often than you need to.
This does not mean you cannot use fentanyl. However, your doctor will need to know about your past and current drug and alcohol use to be able to prescribe fentanyl safely. They will help you watch out for any warning signs of addiction.
People addicted to fentanyl who stop using it can have severe withdrawal symptoms that begin as early as a few hours after the drug was last taken. These symptoms include:
- muscle and bone pain
- sleep problems
- diarrhea and vomiting
- cold flashes with goose bumps
- uncontrollable leg movements
- severe cravings
These symptoms can be extremely uncomfortable and are the reason many people find it so difficult to stop taking fentanyl. There are medicines being developed to help with the withdrawal process for fentanyl and other opioids. The FDA has approved lofexidine, a non-opioid medicine designed to reduce opioid withdrawal symptoms. Also, the NSS-2 Bridge device is a small electrical nerve stimulator placed behind the person’s ear, that can be used to try to ease symptoms for up to five days during the acute withdrawal phase. In December 2018, the FDA cleared a mobile medical application, reSET®, to help treat opioid use disorders 19. This application is a prescription cognitive behavioral therapy (CBT) and should be used in conjunction with treatment that includes buprenorphine and contingency management.
What will happen if I stop taking fentanyl?
If you need to take fentanyl for a long time your body can become tolerant to it. This is not usually a problem. However, you could get withdrawal symptoms if you stop taking it suddenly.
If you want to stop taking fentanyl, talk to your doctor first. Do not stop taking it without speaking to your doctor first. Your dose can be reduced gradually so you do not get withdrawal symptoms.
If you stop taking fentanyl suddenly it can make you:
- feel agitated
- feel anxious
- shaky
- sweat a lot
How is fentanyl addiction treated?
Like other opioid addictions, medication with behavioral therapies has been shown to be effective in treating people with a fentanyl addiction.
- Medications: Buprenorphine and methadone work by binding to the same opioid receptors in the brain as fentanyl, reducing cravings and withdrawal symptoms. Another medicine, naltrexone, blocks opioid receptors and prevents fentanyl from having an effect. People can discuss treatment options with their health provider.
- Counseling: Behavioral therapies for addiction to opioids like fentanyl can help people modify their attitudes and behaviors related to drug use, increase healthy life skills, and help them stick with their medication. Some examples include:
- Cognitive Behavioral Therapy (CBT), which helps modify the patient’s drug use expectations and behaviors, and effectively manage triggers and stress.
- Contingency management, which uses a voucher-based system giving patients “points” based on negative drug tests. They can use the points to earn items that encourage healthy living.
- Motivational interviewing, which is a patient-centered counseling style that addresses a patient’s mixed feelings to change.
These behavioral treatment approaches have proven effective, especially when used along with medicines.
Fentanyl drug interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are receiving fentanyl, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using fentanyl with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Mifepristone
- Nalmefene
- Naltrexone
- Safinamide
- Samidorphan
Using fentanyl with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abametapir
- Acepromazine
- Alefacept
- Alfentanil
- Almotriptan
- Alprazolam
- Amifampridine
- Amineptine
- Amiodarone
- Amitriptyline
- Amitriptylinoxide
- Amobarbital
- Amoxapine
- Amphetamine
- Amprenavir
- Anileridine
- Aprepitant
- Aripiprazole
- Armodafinil
- Asciminib
- Asenapine
- Atazanavir
- Avacopan
- Baclofen
- Belzutifan
- Benperidol
- Benzhydrocodone
- Benzphetamine
- Berotralstat
- Boceprevir
- Bosentan
- Bromazepam
- Bromopride
- Brompheniramine
- Buprenorphine
- Bupropion
- Buspirone
- Butabarbital
- Butorphanol
- Calcium Oxybate
- Cannabidiol
- Carbamazepine
- Carbinoxamine
- Cariprazine
- Carisoprodol
- Carphenazine
- Ceritinib
- Cetirizine
- Chloral Hydrate
- Chlordiazepoxide
- Chlorpheniramine
- Chlorpromazine
- Chlorzoxazone
- Ciprofloxacin
- Citalopram
- Clarithromycin
- Clobazam
- Clomipramine
- Clonazepam
- Clopidogrel
- Clorazepate
- Clozapine
- Cobicistat
- Cocaine
- Codeine
- Conivaptan
- Crizotinib
- Cyclobenzaprine
- Cyclosporine
- Darunavir
- Delavirdine
- Desipramine
- Desmopressin
- Desvenlafaxine
- Dexamethasone
- Dexmedetomidine
- Dextroamphetamine
- Dextromethorphan
- Dezocine
- Diazepam
- Dibenzepin
- Dichloralphenazone
- Difenoxin
- Dihydrocodeine
- Diltiazem
- Diphenhydramine
- Diphenoxylate
- Dolasetron
- Donepezil
- Doxepin
- Dronedarone
- Droperidol
- Duloxetine
- Efavirenz
- Eletriptan
- Eluxadoline
- Enflurane
- Enzalutamide
- Erdafitinib
- Erythromycin
- Escitalopram
- Esketamine
- Eslicarbazepine Acetate
- Estazolam
- Eszopiclone
- Ethchlorvynol
- Ethopropazine
- Ethylmorphine
- Etravirine
- Fenfluramine
- Fexinidazole
- Flibanserin
- Fluconazole
- Fluoxetine
- Fluphenazine
- Flurazepam
- Fluspirilene
- Fluvoxamine
- Fosamprenavir
- Fosaprepitant
- Fosnetupitant
- Fosphenytoin
- Fospropofol
- Frovatriptan
- Furazolidone
- Gabapentin
- Gabapentin Enacarbil
- Granisetron
- Halazepam
- Haloperidol
- Halothane
- Hexobarbital
- Hydrocodone
- Hydromorphone
- Hydroxytryptophan
- Hydroxyzine
- Idelalisib
- Imatinib
- Imipramine
- Indinavir
- Iproniazid
- Isocarboxazid
- Isoflurane
- Itraconazole
- Ivacaftor
- Ketamine
- Ketobemidone
- Ketoconazole
- Lanreotide
- Lasmiditan
- Lefamulin
- Lemborexant
- Levocetirizine
- Levomilnacipran
- Levorphanol
- Linezolid
- Lisdexamfetamine
- Lithium
- Lofepramine
- Lofexidine
- Lomitapide
- Lopinavir
- Lorazepam
- Lorcaserin
- Lorlatinib
- Loxapine
- Lumacaftor
- Magnesium Oxybate
- Meclizine
- Melitracen
- Melperone
- Meperidine
- Mephobarbital
- Meprobamate
- Meptazinol
- Mesoridazine
- Metaxalone
- Methadone
- Methamphetamine
- Methdilazine
- Methocarbamol
- Methohexital
- Methotrimeprazine
- Methylene Blue
- Metoclopramide
- Mibefradil
- Midazolam
- Milnacipran
- Mirtazapine
- Mitotane
- Mobocertinib
- Moclobemide
- Modafinil
- Molindone
- Moricizine
- Morphine
- Morphine Sulfate Liposome
- Nafcillin
- Nalbuphine
- Naratriptan
- Nefazodone
- Nelfinavir
- Netupitant
- Nevirapine
- Nialamide
- Nicardipine
- Nicomorphine
- Nifedipine
- Nilotinib
- Nitrazepam
- Nitrous Oxide
- Nortriptyline
- Octreotide
- Olanzapine
- Ondansetron
- Opipramol
- Opium
- Opium Alkaloids
- Orphenadrine
- Oxazepam
- Oxcarbazepine
- Oxycodone
- Oxymorphone
- Ozanimod
- Palbociclib
- Palonosetron
- Papaveretum
- Paregoric
- Paroxetine
- Pazopanib
- Pentazocine
- Pentobarbital
- Perampanel
- Perazine
- Periciazine
- Perphenazine
- Phenelzine
- Phenobarbital
- Phenytoin
- Pimozide
- Piperacetazine
- Pipotiazine
- Piritramide
- Posaconazole
- Potassium Oxybate
- Prazepam
- Prednisone
- Pregabalin
- Primidone
- Procarbazine
- Prochlorperazine
- Promazine
- Promethazine
- Propofol
- Protriptyline
- Quazepam
- Quetiapine
- Ramelteon
- Ranitidine
- Ranolazine
- Rasagiline
- Remifentanil
- Remimazolam
- Remoxipride
- Ribociclib
- Rifabutin
- Rifampin
- Rifapentine
- Ritonavir
- Rizatriptan
- Saquinavir
- Scopolamine
- Secobarbital
- Selegiline
- Selpercatinib
- Sertindole
- Sertraline
- Sibutramine
- Sodium Oxybate
- Sotorasib
- St John’s Wort
- Sufentanil
- Sulpiride
- Sumatriptan
- Suvorexant
- Tacrolimus
- Tapentadol
- Telaprevir
- Telithromycin
- Temazepam
- Thiethylperazine
- Thiopental
- Thiopropazate
- Thioridazine
- Tianeptine
- Tilidine
- Tizanidine
- Tolonium Chloride
- Topiramate
- Tramadol
- Tranylcypromine
- Trazodone
- Triazolam
- Trifluoperazine
- Trifluperidol
- Triflupromazine
- Trimeprazine
- Trimipramine
- Tryptophan
- Tucatinib
- Venlafaxine
- Verapamil
- Vilazodone
- Voriconazole
- Vortioxetine
- Voxelotor
- Zaleplon
- Ziprasidone
- Zolmitriptan
- Zolpidem
- Zopiclone
- Zotepine
Other interactions
Using fentanyl with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use fentanyl, or give you special instructions about the use of food, alcohol, or tobacco.
- Ethanol
- Grapefruit Juice
How does fentanyl work?
Fentanyl works directly on opioid receptors in the central nervous system (brain and spinal cord) and reduces feelings of pain by interrupting the way nerves signal pain between the brain and the body. Biochemically, fentanyl is a Mu-selective opioid agonist. However, it has the capability to activate other opioid system receptors such as the delta and potentially the kappa-receptors 20. Consequently, the activation of these receptors, particularly the Mu-receptors, produces analgesia. Also, the neurotransmitter dopamine is increased in the reward areas of the brain, which elicits the stereotypical exhilaration and relaxation effects, and is typically associated with the addiction to fentanyl 21.
Fentanyl is available in several formulations in different strengths, including patches, lozenges, tablets that disintegrate in your mouth and sublingual (under the tongue) tablets. Fentanyl is also given by injection for severe acute pain or as part of anaesthesia before surgery.
How long does fentanyl take to work?
This depends on the type of fentanyl you take.
A fentanyl injection into a vein gives the quickest pain relief. It works almost straight away and is usually only given in hospital.
Fast-acting fentanyl tablets, lozenges and nasal sprays take around 15 to 30 minutes to work but they wear off after 4 to 6 hours.
Fentanyl patches can take up to a day or two to start working but they will last longer. Patches are usually given after fentanyl tablets. This is to make sure that you have pain relief from the tablets until the patches start to work.
How long will I use fentanyl for?
Depending on why you’re taking fentanyl, you may only need to take it for a short time.
For example, if you’re in pain after an injury or operation, you may only need to take fentanyl for a few days or weeks.
You may need to take it for longer if you have a long-term condition.
Can I take fentanyl for a long time?
For some people with conditions that need long-term pain relief it may be necessary to take fentanyl for a long time.
If you need to take it for a long time your body can become tolerant to it. That means you need higher doses to control your pain over time.
Some people can become more sensitive to pain (hyperalgesia). If this happens, your doctor will reduce your dose gradually to help these symptoms.
It is possible to become addicted to fentanyl. For this reason, your dose will be reviewed to make sure you are only taking the amount you need to control your pain.
Your treatment plan may include details of how and when you will stop taking fentanyl.
If you are having treatment for cancer pain or other severe pain, your pain control will be carefully monitored. Speak to your doctor if you are worried about tolerance, hyperalgesia or becoming addicted.
How is fentanyl different to other opioids?
Fentanyl acts on different pain signals in the brain to some other opioids. The pain relief and side effects will be different for everyone. Your doctor may prescribe fentanyl if you have had side effects from other opioids.
The way you take fentanyl is different to some other painkillers. Fentanyl is not absorbed very well by swallowing tablets. Instead your body absorbs it through your skin, your nostrils, or your tongue or the inside of your cheek.
Some people find skin patches more convenient as it means they do not need to take tablets or capsules regularly.
Fentanyl uses
Fentanyl has a rapid onset and short duration of action, making it particularly effective in anesthesia induction as well as maintenance 2. Fentanyl was approved for use in general anesthesia in the United States in 1968 and is still widely used in anesthesia practice 2. With the development of transdermal and buccal formulations of fentanyl, it was approved for use in pain management and has become the most widely used synthetic opioid in clinical practice.
Fentanyl is used to treat breakthrough pain (sudden episodes of pain that occur despite round the clock treatment with pain medication) in cancer patients at least 18 years of age (or at least 16 years of age if using Actiq brand lozenges) who are taking regularly scheduled doses of another narcotic (opiate) pain medication, and who are tolerant (used to the effects of the medication) to narcotic pain medications. Tolerance occurs when you need a higher and/or more frequent amount of a drug to get the desired effects. Fentanyl should not be prescribed for other uses; ask your doctor or pharmacist for more information.
How often to take or use fentanyl
How often you take or use fentanyl depends on the type that you’ve been prescribed:
- fentanyl patches – apply a new patch every 3 days (remove the old one first)
- fentanyl tablets, lozenges and nasal spray – usually only when you need them
Some patches keep working after they’ve been removed as they “store” fentanyl under the skin. Fentanyl patches take longer to start working but last longer. They’re used for when pain lasts for a long time. Do not apply more than 1 patch at a time, unless your doctor tells you to. Using more patches than recommended could lead to a fatal overdose. If you need to apply more than 1 patch at a time, place the patches far enough apart so that the edges do not touch or overlap each other.
Sometimes your doctor may prescribe a fentanyl patch with a fast-acting painkiller. This is to manage sudden flare-ups of pain that “break through” the relief the patches give.
How to use fentanyl lozenges (Actiq)
- Check the blister package and the handle of the lozenge to make sure the lozenge contains the dose of medication you have been prescribed.
- Use scissors to cut open the blister package and remove the lozenge. Do not open the blister package until you are ready to use the medication.
- Place the lozenge in your mouth, between your cheek and gum. Actively suck on the lozenge, but do not chew, crush, or bite it. Move the lozenge around in your mouth, from one side to the other, using the handle. Twirl the handle often.
- Do not eat or drink anything while the lozenge is in your mouth.
- Finish the lozenge in about 15 minutes.
- If you begin to feel dizzy, very sleepy, or nauseated before you have finished the lozenge, remove it from your mouth. Dispose of it immediately as described below or put it in the temporary storage bottle for later disposal.
- If you finish the entire lozenge, throw the handle away in a garbage can that is out of the reach of children. If you did not finish the entire lozenge, hold the handle under hot running water to dissolve all the medication, and then throw the handle away in a garbage can that is out of the reach of children and pets.
How to use fentanyl buccal tablets (Fentora)
- Separate one blister unit from the blister card by tearing along the perforations. Peel back the foil to open the blister unit. Do not try to push the tablet through the foil. Do not open the blister unit until you are ready to use the tablet.
- Place the tablet in your mouth above one of your upper back teeth between your cheek and your gum.
- Leave the tablet in place until it dissolves completely. You may notice a gentle bubbling feeling between your cheek and gum as the tablet dissolves. It may take 14 to 25 minutes for the tablet to dissolve. Do not split, chew, bite, or suck the tablet.
- If any of the tablet is left in your mouth after 30 minutes, swallow it with a drink of water.
- If you begin to feel dizzy, very sleepy, or nauseated before the tablet dissolves, rinse your mouth with water and spit the remaining pieces of tablet into the sink or toilet. Flush the toilet or rinse the sink to wash away the tablet pieces.
How to use fentanyl sublingual tablets (Abstral)
- Take a sip of water to moisten your mouth if it is dry. Spit out or swallow the water. Make sure your hands are dry before handling the tablet.
- Separate one blister unit from the blister card by tearing along the perforations. Peel back the foil to open the blister unit. Do not try to push the tablet through the foil. Do not open the blister unit until you are ready to use the tablet.
- Place the tablet under your tongue as far back as you can. If more than 1 tablet is needed for your dose, spread them around on the floor of your mouth under your tongue.
- Leave the tablet in place until it dissolves completely. Do not suck, chew, or swallow the tablet.
- Do not eat or drink anything until the tablet is completely dissolved and you no longer feel it in your mouth.
How to use fentanyl films (Onsolis)
- Use scissors to cut along the arrows of the foil package to open it. Separate the layers of the foil package and remove the film. Do not open the foil package until you are ready to use the medication. Do not cut or tear the film.
- Use your tongue to wet the inside of your cheek, or if needed, rinse your mouth with water to wet the area where you will place the film.
- Hold the film on a clean, dry finger, with the pink side facing up. Place the film in your mouth, with the pink side against the inside of your moistened cheek. With your finger, press the film against your cheek for 5 seconds. Then remove your finger and the film will stick to the inside of your cheek. If more than one film is needed for your dose, do not put the films on top of each other. You may place the films on either side of your mouth.
- Leave the film in place until it dissolves completely. The film will release a minty flavor as it dissolves. It may take 15 to 30 minutes for the film to dissolve. Do not chew or swallow the film.
- Do not touch or move the film while it dissolves.
- You may drink liquids after 5 minutes, but do not eat anything until the film dissolves completely.
Fentanyl contraindications
The use of fentanyl is contraindicated in patients in the following situations 20:
- After operative interventions in the biliary tract, as these may slow hepatic elimination of the drug.
- With respiratory depression or obstructive airway diseases (i.e., asthma, COPD, obstructive sleep apnea, obesity hyperventilation, also know as, Pickwickian syndrome)
- With liver failure
- With known intolerance to fentanyl or other morphine-like drugs, including codeine
- With known hypersensitivity (i.e., anaphylaxis) or any common drug delivery excipients (i.e., sodium chloride, sodium hydroxide).
The drug fentanyl should not be used concomitant with certain medications such as CYP3A4 inhibitors like macrolide antibiotics or azole-antifungal agents, and protease inhibitors may increase plasma concentrations of fentanyl, extending the opioid drug action and exacerbating the opioid-induced respiratory depression. On the other hand, the cessation of a CYP3A4 inducer medication (i.e., carbamazepine, phenytoin) in patients treated with fentanyl citrate injections may potentially increase fentanyl plasma concentrations prolonging the opioid adverse reactions.
Fentanyl dosage
The different types of fentanyl come in a range of strengths:
- Fentanyl patches – these release 12 micrograms to 100 micrograms of fentanyl every hour
- Fentanyl nasal spray – 50 micrograms to 400 micrograms
- Fentanyl tablets – 100 micrograms to 800 micrograms
- Fentanyl lozenges – 200 micrograms to 1,600 micrograms
The dose of fentanyl will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of fentanyl. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of fentanyl that you take depends on the strength of the fentanyl. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take fentanyl depend on the medical problem for which you are using fentanyl.
Discontinue all other extended-release opioids when beginning therapy.
Due to the risk of respiratory depression, the transdermal patch is for use in opioid-tolerant patients only; opioid tolerant patients have been taking at least: morphine 60 mg daily, oral oxycodone 30 mg daily, oral hydromorphone 8 mg daily, or an equianalgesic dose of another opioid for 1 week or longer.
Dose for chronic pain
For transdermal dosage form (Duragesic® skin patch):
- For relief of chronic pain:
- Adults and children 2 years of age and older: Your doctor will decide which dose of the patch you need based on your present daily narcotic dose. The patch is applied to the skin and left in place for 3 days (72 hours). Your doctor may adjust your dose as needed.
- Children younger than 2 years of age: Use and dose must be determined by your doctor.
For transdermal dosage form (Ionsys® skin patch) (the Ionsys® patch is not for use at home):
- For short-term relief of acute pain after surgery:
- Adults—Your doctor will decide which dose of the patch you need based on your present daily narcotic dose. The patch is applied by your healthcare provider to your upper outer arm or chest. Your doctor will show you how to adjust your dose as needed while in the hospital.
Adult dose for breakthrough pain
For the management of breakthrough pain in patients who are already receiving and who are tolerant to around-the-clock opioid therapy for their underlying persistent cancer pain.
Transmucosal products
- For use in patients who are opioid-tolerant and taking around-the-clock opioids. Opioid tolerant patients have been taking at least: morphine 60 mg daily, oral oxycodone 30 mg daily, oral hydromorphone 8 mg daily, or an equianalgesic dose of another opioid for 1 week or longer.
- All transmucosal products must be individually titrated to an effective and tolerable dose. Once titrated, these products are used to treat up to 4 episodes of breakthrough pain a day; if a patient is experiencing more than 4 breakthrough episodes per day, the around-the-clock opioid dose should be re-evaluated. If the around-the-clock opioid dose is adjusted, re-adjustment of the transmucosal product may be necessary.
- Transmucosal fentanyl products are not bioequivalent; patients should not be interchanged on a mcg per mcg basis from 1 fentanyl product to any other fentanyl product
Transmucosal lozenge (Actiq)
The lozenge should be placed in mouth between cheek and lower gum and sucked; occasionally move from side to side using the handle; do not chew. If signs of excessive opioid effects appear before the lozenge is consumed, the lozenge should be removed immediately and subsequent doses should be decreased.
- Initial dose: 200 mcg consumed over 15 minutes
- Dose titration: If breakthrough pain is not relieved 15 minutes after completion of 1 unit (30 minutes after start), 1 additional unit of the same strength may be taken; Patients must wait at least 4 hours before re-treating. If breakthrough pain had not been relieved with 1 unit, the dose should be increased to the next highest strength with subsequent episodes of pain.
- Maintenance dose: An effective dose is achieved when 1 unit is mostly sufficient to treat an episode of breakthrough pain; however, if there is inadequate analgesia a second dose of the same strength may be given 15 minutes after completion (30 minutes after start); no more than 2 doses should be used to treat any episode of breakthrough pain.
- Maximum dose: 4 breakthrough episodes per day at intervals of at least 4 hours
Nasal spray (Lazanda)
- Initial dose: 100 mcg sprayed in 1 nostril
- Dose titration: If adequate analgesia is not achieved after 30 minutes, the dose should be escalated in a step-wise manner over consecutive episodes. Patients must wait at least 2 hours between doses. Patients should confirm the dose that works for them with a second episode of breakthrough pain.
- Maintenance dose: Once an effective dose has been established, patients should use that dose for each subsequent breakthrough episode.
- Maximum dose: 800 mcg per dose; 4 breakthrough episodes per day at intervals of at least 2 hours
Sublingual tablet (Abstral)
The sublingual tablet should be placed on the floor of the mouth and allowed to completely dissolve; do not eat or drink until the tablet is completely dissolved. The initial dose of the sublingual tablet is always 100 mcg except in patients receiving the transmucosal lozenge – see dose adjustment section for initial dosing recommendations for these patients.
- Initial dose: 100 mcg sublingually
- Dose titration: If adequate analgesia is not obtained after 30 minutes, a second dose of the same strength may be taken. Patients must wait at least 2 hours before re-treating. Dose escalation should proceed in a stepwise manner (200 to 300 to 400 to 600 to 800 mcg) as needed. During titration, multiples of 100 mcg and/or 200 mcg tablets may be used for any single dose. Patients should not use more than 4 tablets at one time.
- Maintenance dose: An effective dose is achieved when 1 dose is sufficient to treat most episodes of breakthrough pain; however, if there is inadequate analgesia a second dose of the same strength may be given after 30 minutes; no more than 2 doses should be used to treat any episode of breakthrough pain. Patients should limit treatment to 4 or fewer breakthrough episodes per day.
- Maximum dose: 4 episodes per day; 800 mcg per dose at intervals of at least 2 hours
Sublingual spray
Spray into mouth underneath the tongue. The initial dose of is always 100 mcg except in patients receiving the transmucosal lozenge – see dose adjustment section for initial dosing recommendations for these patients.
- Initial dose: 100 mcg sprayed sublingually
- Dose titration: If adequate analgesia is not obtained after 30 minutes, a second dose of the same strength may be used. Patients must wait at least 4 hours before re-treating. If breakthrough pain is not relieved with the 100 mcg dose, dose escalation should proceed in a stepwise manner (200 to 400 to 600 to 800 to 1200 to 1600 mcg) for subsequent episodes of pain.
- Maintenance dose: An effective dose is achieved when 1 dose is sufficient to treat most episodes of breakthrough pain; however, if there is inadequate analgesia a second dose of the same strength may be given after 30 minutes; no more than 2 doses should be used to treat any episode of breakthrough pain. Patients should limit treatment to 4 or fewer breakthrough episodes per day.
- Maximum dose: 4 episodes per day at intervals of at least 4 hours
Buccal tablet (Fentora)
Tablet should be placed in the buccal cavity (above the rear molar, between the upper cheek and gum); alternatively, may be placed under the tongue. The initial dose of is always 100 mcg except in patients receiving the transmucosal lozenge – see dose adjustment section for initial dosing recommendations for these patients.
- Initial dose: 100 mcg buccally
- Dose titration: If adequate analgesia is not obtained after 30 minutes, a second dose of the same strength may be taken. Patients must wait at least 4 hours before re-treating. If breakthrough pain is not relieved with 100 mcg, the next dose should be two 100 mcg tablets (one on each side of the mouth in the buccal cavity). The patient may be further titrated in a stepwise manner. During titration, multiples of 100 mcg or 200 mcg tablets may be used for any single dose. Patients should not use more than 4 tablets at one time.
- Maintenance dose: An effective dose is achieved when 1 dose is sufficient to treat most episodes of breakthrough pain; however, if there is inadequate analgesia a second dose of the same strength may be given after 30 minutes; no more than 2 doses should be used to treat any episode of breakthrough pain. Patients should limit treatment to 4 or fewer breakthrough episodes per day.
- Maximum dose: 4 episodes per day; at intervals of at least 4 hours
Adult dose for anesthesia
Premedication for anesthesia:
- 50 to 100 mcg IM, 30 to 60 minutes prior to surgery.
- Lozenge: 5 mcg/kg (400 mcg is the maximum dose).
- Lower doses should be used for vulnerable patients.
General Anesthesia:
- Total Low dose: 2 mcg/kg (minor procedures).
- Maintenance low dose: Infrequently needed.
- Total Moderate dose: 2 to 20 mcg/kg.
- Maintenance moderate dose: 25 to 100 mcg IV/IM.
- Total high dose: 20 to 50 mcg/kg (prolonged surgeries).
- Maintenance high dose: 25 mcg to half of the initial dose.
Adjunct to regional anesthesia:
- 50 to 100 mcg IM or slow IV over 3 to 5 minutes as required.
Postoperative:
- 50 to 100 mcg IM. May repeat dose in 1 to 2 hours as needed.
Pediatric dose for anesthesia
Doses should be titrated to appropriate effects; a wide range of doses is possible depending upon desired degree of analgesia/anesthesia, clinical environment, patient’s status, and presence of opioid tolerance.
Neonates analgesia (International Evidence-Based Group for Neonatal Pain recommendations):
- Intermittent doses: Slow IV push: 0.5 to 3 mcg/kg/dose
- Continuous IV infusion: 0.5 to 2 mcg/kg/hour
- Sedation/analgesia: Slow IV push: 1 to 4 mcg/kg/dose; may repeat every 2 to 4 hours
- Continuous sedation/analgesia: Initial IV bolus: 1 to 2 mcg/kg, then 0.5 to 1 mcg/kg/hour; titrate upward
- Mean required dose: Neonates with gestational age less than 34 weeks: 0.64 mcg/kg/hour; neonates with gestational age greater than or equal to 34 weeks: 0.75 mcg/kg/hour
- Continuous sedation/analgesia during extracorporeal membrane oxygenation (ECMO): Initial IV bolus: 5 to 10 mcg/kg slow IV push over 10 minutes, then 1 to 5 mcg/kg/hour; titrate upward; tolerance may develop; higher doses (up to 20 mcg/kg/hour) may be needed by day 6 of ECMO.
Younger infants:
- Sedation/analgesia: Slow IV push: 1 to 4 mcg/kg/dose; may repeat every 2 to 4 hours
- Continuous sedation/analgesia: Initial IV bolus: 1 to 2 mcg/kg, then 0.5 to 1 mcg/kg/hour; titrate upward
- Continuous sedation/analgesia during extracorporeal membrane oxygenation ECMO: Initial IV bolus: 5 to 10 mcg/kg slow IV push over 10 minutes, then 1 to 5 mcg/kg/hour; titrate upward; tolerance may develop; higher doses (up to 20 mcg/kg/hour) may be needed by day 6 of ECMO.
Older Infants and Children 1 to 12 years:
- Sedation for minor procedures/analgesia: IM or IV: 1 to 2 mcg/kg/dose; may repeat at 30 to 60 minute intervals. Note: Children 18 to 36 months of age may require 2 to 3 mcg/kg/dose.
- Intranasal: Children greater than or equal to 10 kg: 1.5 mcg/kg once (maximum: 100 mcg/dose); reported range: 1 to 2 mcg/kg; some studies allowed for additional incremental doses of 0.5 mcg/kg to be administered every 5 minutes, not to exceed a total dose of 3 mcg/kg depending on pain type and severity.
- Continuous sedation/analgesia: Initial IV bolus: 1 to 2 mcg/kg then 1 mcg/kg/hour; titrate upward; usual: 1 to 3 mcg/kg/hour; some require 5 mcg/kg/hour
Children greater than or equal to 5 years and less than 50 kg:
- Patient-controlled analgesia (PCA): IV: Opioid-naive: Note: patient-controlled analgesia has been used in children as young as 5 years of age; however, clinicians need to assess children 5 to 8 years of age to determine if they are able to use the patient-controlled analgesia device correctly. All patients should receive an initial loading dose of an analgesic (to attain adequate control of pain) before starting patient-controlled analgesia for maintenance. Adjust doses, lockouts, and limits based on required loading dose, age, state of health, and presence of opioid tolerance. Use lower end of dosing range for opioid-naive. Assess patient and pain control at regular intervals and adjust settings if needed.
Usual concentration: Determined by weight; some clinicians use the following:
- Children less than 12 kg: 10 mcg/mL
- Children 12 to 30 kg: 25 mcg/mL
- Children greater than 30 kg: 50 mcg/mL
- Demand dose: Usual initial: 0.5 to 1 mcg/kg/dose; usual range: 0.5 to 1 mcg/kg/dose
- Lockout: Usual initial: 5 doses/hour
- Lockout interval: Range: 6 to 8 minutes
- Usual basal rate: 0 to 0.5 mcg/kg/hour
Children greater than 12 years to adult:
- Sedation for minor procedures/analgesia: IV: 0.5 to 1 mcg/kg/dose; may repeat after 30 to 60 minutes; or 25 to 50 mcg, repeat full dose in 5 minutes if needed, may repeat 4 to 5 times with 25 mcg at 5 minute intervals if needed. Note: Higher doses are used for major procedures.
- Continuous sedation/analgesia:
- Less than 50 kg: Initial IV bolus: 1 to 2 mcg/kg; continuous infusion rate: 1 to 2 mcg/kg/hour
- Greater than 50 kg: Initial IV bolus: 1 to 2 mcg/kg or 25 to 100 mcg/dose; continuous infusion rate: 1 to 2 mcg/kg/hour or 25 to 200 mcg/hour
- Patient-controlled analgesia (PCA): IV: Children greater than 50 kg, Adolescents greater than 50 kg, and Adults: Note: All patients should receive an initial loading dose of an analgesic (to attain adequate control of pain) before starting patient-controlled analgesia for maintenance. Adjust doses, lockouts, and limits based on required loading dose, age, state of health, and presence of opioid tolerance. Use lower end of dosing range for opioid-naive. Assess patient and pain control at regular intervals and adjust settings if needed:
- Usual concentration: 50 mcg/mL
- Demand dose: Usual initial: 20 mcg; usual range: 10 to 50 mcg
- Lockout interval: Usual initial: 6 minutes; usual range: 5 to 8 minutes
- Usual basal rate: less than or equal to 50 mcg/hour
Preoperative sedation, adjunct to regional anesthesia, postoperative pain: IM, IV: 25 to 100 mcg/dose
Adjunct to general anesthesia: Slow IV:
- Low dose: 0.5 to 2 mcg/kg/dose depending on the indication
- Moderate dose: Initial: 2 to 20 mcg/kg/dose; Maintenance (bolus or infusion): 1 to 2 mcg/kg/hour. Discontinuing fentanyl infusion 30 to 60 minutes prior to the end of surgery will usually allow adequate ventilation upon emergence from anesthesia. For “fast-tracking” and early extubation following major surgery, total fentanyl doses are limited to 10 to 15 mcg/kg.
- High dose: 20 to 50 mcg/kg/dose; Note: High dose fentanyl as an adjunct to general anesthesia is rarely used, but is still described in the manufacturer label.
General anesthesia without additional anesthetic agents: IV: 50 to 100 mcg/kg with oxygen and skeletal muscle relaxant.
What if I take too much fentanyl?
It’s important not to take more than your prescribed fentanyl dose, even if you think it’s not enough to relieve your pain. Speak to your doctor first, if you think you need a different dose. Too much fentanyl can be dangerous. However, the amount that can lead to an overdose varies from person to person.
If you’ve taken too much you may feel very sleepy, sick or dizzy. You may also find it difficult to breathe. In serious cases you can become unconscious and may need emergency treatment in hospital.
Make sure the patch does not get stuck to someone else’s skin, especially a child’s, by accident – for example if it falls off in bed or if the patch falls on the floor.
Call your local emergency services number if:
- you’ve taken too much fentanyl and find it difficult to breathe
- you or someone else swallows a fentanyl patch
What should I do if I forget a dose?
Fentanyl is usually used as needed according to directions. If you forget to wear or change a fentanyl patch, put one on as soon as you can. If it is almost time to put on your next patch, wait until then to apply a new patch and skip the one you missed. Do not apply extra patches to make up for a missed dose.
Remove the Duragesic® patch 3 days (72 hours) after applying it.
Your healthcare provider will remove the Ionsys® patch before you leave the hospital. The Ionsys® patch is not for use at home.
Fentanyl side effects
Like all medicines, fentanyl can cause side effects in some people but many people have no side effects or only minor ones. You are more likely to get side effects with higher doses of fentanyl.
All opioids, including fentanyl, can have side effects including life-threatening breathing problems — the risk of these is higher:
- when first taking fentanyl
- after a dosage increase
- if you are older
- if you have an existing lung problem
Fentanyl common side effects
Common side effects happen in more than 1 in 100 people.
Talk to your doctor or pharmacist if the side effects bother you or do not go away:
- constipation
- feeling or being sick (nausea or vomiting)
- stomach pain
- feeling sleepy or tired
- feeling dizzy or a sensation of spinning (vertigo)
- confusion
- headaches
- itching or skin rashes
Fentanyl affects everyone differently, so if you have any of these side effects while taking fentanyl, or if you notice anything that is making you feel unwell, speak with your pharmacist or doctor.
Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- stomach pain
- gas
- heartburn
- weight loss
- difficulty urinating
- changes in vision
- anxiety
- depression
- unusual thinking
- unusual dreams
- difficulty falling asleep or staying asleep
- dry mouth
- sudden reddening of the face, neck, or upper chest
- uncontrollable shaking of a part of the body
- back pain
- chest pain
- pain, sores, or irritation in the mouth in the area where you placed the medication
- swelling of the hands, arms, feet, ankles, or lower legs.
These are not all the side effects of fentanyl. For the full list, see the leaflet inside you medicines packet.
How to cope with side effects
What to do about:
- constipation – try to eat more high-fibre foods such as fresh fruit and vegetables and cereals. Try to drink several glasses of water or squash each day. If you can, it may also help to do some gentle exercise. Speak to your doctor about medicine to help prevent or treat constipation caused by fentanyl if your symptoms do not go away. Watch a short video on how to treat constipation.
- feeling or being sick – this side effect should normally wear off after a few days. Stick to simple meals and do not eat rich or spicy food. Drink plenty of fluids, such as water or squash, to avoid dehydration. If you’re being sick, take small, regular sips of water. Ask your doctor about anti-sickness medicine if it gets worse or lasts longer than a few days.
- stomach pain – try to rest and relax. It can help to eat and drink slowly and have smaller and more frequent meals. Putting a heat pad or covered hot water bottle on your stomach may also help. If you are in a lot of pain, speak to your pharmacist or doctor.
- feeling sleepy or tired – these side effects should wear off within a week or two as your body gets used to fentanyl. Talk to your doctor if they carry on for longer. Do not drink alcohol as it will make these side effects worse.
- feeling dizzy or a sensation of spinning (vertigo) – stop what you’re doing and sit or lie down until you feel better. Do not drink alcohol as it will make these side effects worse. If the feeling does not go away, do not take any more medicine and speak to a pharmacist or your doctor. Do not drive, ride a bike or use tools or machinery.
- confusion – talk to your doctor if you feel confused, your dose may need to be changed.
- headaches – make sure you rest and drink plenty of fluids. Do not drink alcohol while taking fentanyl as this can make headaches worse. Ask your pharmacist to recommend a painkiller. Headaches should usually go away after the first week of taking fentanyl. Talk to your doctor if they last longer than a week or are severe.
- itching or rashes – it may help to take an antihistamine, which you can buy from a pharmacy. Check with the pharmacist to see what type is suitable for you. If symptoms do not go away or it gets worse talk to your doctor as you may need to try a different painkiller.
Fentanyl serious side effects
Serious side effects happen in less than 1 in 100 people.
Some side effects can be serious. If you experience any of these symptoms, call your doctor immediately (if you are wearing a fentanyl patch, remove your patch):
- changes in heartbeat
- agitation, hallucinations (seeing things or hearing voices that do not exist), fever, sweating, confusion, fast heartbeat, shivering, severe muscle stiffness or twitching, loss of coordination, nausea, vomiting, or diarrhea
- your muscles feel stiff for no obvious reason
- you feel dizzy, tired and have low energy – all of these together could be a sign of low blood pressure
- nausea, vomiting, loss of appetite, weakness, or dizziness
- inability to get or keep an erection
- irregular menstruation
- decreased sexual desire
- seizures
- hives
- rash
- itching
If you experience any of these symptoms, stop using fentanyl and call your doctor immediately or get emergency medical treatment:
- slow, shallow breathing
- decreased urge to breathe
- difficulty breathing or swallowing
- extreme drowsiness
- dizziness
- confusion
- fainting
Fentanyl may cause other side effects. Call your doctor if you have any unusual problems while using fentanyl.
Fentanyl overdose
While using fentanyl, you should talk to your doctor about having a rescue medication called naloxone readily available (e.g., home, office). Naloxone (NARCAN® and KLOXXADO®) is used to reverse the life-threatening effects of a Fentanyl overdose. Naloxone works by blocking the effects of opiates to relieve dangerous symptoms caused by high levels of opiates in the blood. Your doctor may also prescribe you naloxone if you are living in a household where there are small children or someone who has abused street or prescription drugs. You should make sure that you and your family members, caregivers, or the people who spend time with you know how to tell recognize an overdose, how to use naloxone, and what to do until emergency medical help arrives. Your doctor or pharmacist will show you and your family members how to use the medication. Ask your pharmacist for the instructions or visit the manufacturer’s website to get the instructions. If symptoms of an overdose occur, a friend or family member should give the first dose of naloxone, call your local emergency services number immediately, and stay with you and watch you closely until emergency medical help arrives. Your symptoms may return within a few minutes after you receive naloxone. If your symptoms return, the person should give you another dose of naloxone. Additional doses may be given every 2 to 3 minutes, if symptoms return before medical help arrives.
Symptoms of fentanyl overdose may include the following:
- drowsiness or sleepiness
- dizziness
- confusion
- slow, shallow breathing or stopped breathing
- difficulty breathing
- choking or gurgling sounds
- discolored skin (especially in lips and nails)
- smaller pupils or “pinpoint pupils” (black circles in the middle of the eyes)
- falling asleep or losing consciousness
- limp body
- unable to respond or wake up
- cold and/or clammy skin.
How can a fentanyl overdose be treated?
As mentioned above, many drug dealers mix the cheaper fentanyl with other drugs like heroin, cocaine, MDMA and methamphetamine to increase their profits, making it often difficult to know which drug is causing the overdose. Naloxone is a medicine that can treat a fentanyl overdose when given right away. It works by rapidly binding to opioid receptors and blocking the effects of opioid drugs. But fentanyl is stronger than other opioid drugs like morphine and might require multiple doses of naloxone.
Because of this, if you suspect someone has overdosed, the most important step to take is to call your local emergency services number so they can receive immediate medical attention. Most states have laws that may protect a person who is overdosing or the person who called for help from legal trouble. Once medical personnel arrive, they will administer naloxone if they suspect an opioid drug is involved.
Naloxone is available as an injectable (needle) solution and nasal sprays (NARCAN® and KLOXXADO®). ** Naloxone is a life-saving medication that can reverse the effects of opioid overdose and save lives. It is available in all 50 states and can be purchased from a local pharmacy without a prescription in most states.
People who are given naloxone should be monitored for another two hours after the last dose of naloxone is given to make sure breathing does not slow or stop.
Some states have passed laws that allow pharmacists to dispense naloxone without a personal prescription. Friends, family, and others in the community can use the nasal spray versions of naloxone to save someone who is overdosing.
References- Volpe DA, Tobin GAM, Mellon RD, et al. Uniform assessment and ranking of opioid Mu receptor binding constants for selected opioid drugs. Regul Toxicol Pharmacol. 2011;59(3):385-390. doi:10.1016/j.yrtph.2010.12.007
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Fentanyl. [Updated 2019 Apr 25]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548026
- Nelson L, Schwaner R. Transdermal fentanyl: Pharmacology and toxicology. J Med Toxicol. 2009;5(4):230-241. doi:10.1007/BF03178274
- Garnock-Jones KP. Fentanyl Buccal Soluble Film: A Review in Breakthrough Cancer Pain. Clin Drug Investig. 2016;36(5):413-419. doi:10.1007/s40261-016-0394-y
- Jones CM, Einstein EB, Compton WM. Changes in Synthetic Opioid Involvement in Drug Overdose Deaths in the United States, 2010-2016. JAMA. 2018;319(17):1819-1821.
- Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and Geographic Patterns in Drug and Synthetic Opioid Overdose Deaths — United States, 2013–2019. MMWR Morb Mortal Wkly Rep 2021;70:202–207. DOI: http://dx.doi.org/10.15585/mmwr.mm7006a4
- Increase in Fatal Drug Overdoses Across the United States Driven by Synthetic Opioids Before and During the COVID-19 Pandemic. https://emergency.cdc.gov/han/2020/han00438.asp
- Mars, S. G., Rosenblum, D., & Ciccarone, D. (2019). Illicit fentanyls in the opioid street market: desired or imposed?. Addiction (Abingdon, England), 114(5), 774–780. https://doi.org/10.1111/add.14474
- Beilin Y, Bodian CA, Weiser J, Hossain S, Arnold I, Feierman DE, Martin G, Holzman I. Effect of labor epidural analgesia with and without fentanyl on infant breast-feeding: a prospective, randomized, double-blind study. Anesthesiology. 2005 Dec;103(6):1211-7. doi: 10.1097/00000542-200512000-00016
- Lee AI, McCarthy RJ, Toledo P, Jones MJ, White N, Wong CA. Epidural Labor Analgesia-Fentanyl Dose and Breastfeeding Success: A Randomized Clinical Trial. Anesthesiology. 2017 Oct;127(4):614-624. doi: 10.1097/ALN.0000000000001793
- Brimdyr K, Cadwell K, Widström AM, Svensson K, Neumann M, Hart EA, Harrington S, Phillips R. The Association Between Common Labor Drugs and Suckling When Skin-to-Skin During the First Hour After Birth. Birth. 2015 Dec;42(4):319-28. doi: 10.1111/birt.12186
- Moore A, el-Bahrawy A, Hatzakorzian R, Li-Pi-Shan W. Maternal Epidural Fentanyl Administered for Labor Analgesia Is Found in Neonatal Urine 24 Hours After Birth. Breastfeed Med. 2016 Jan-Feb;11(1):40-1. doi: 10.1089/bfm.2015.0173
- French CA, Cong X, Chung KS. Labor Epidural Analgesia and Breastfeeding: A Systematic Review. J Hum Lact. 2016 Aug;32(3):507-20. doi: 10.1177/0890334415623779
- ASGE Standard of Practice Committee, Shergill AK, Ben-Menachem T, Chandrasekhara V, Chathadi K, Decker GA, Evans JA, Early DS, Fanelli RD, Fisher DA, Foley KQ, Fukami N, Hwang JH, Jain R, Jue TL, Khan KM, Lightdale J, Pasha SF, Sharaf RN, Dominitz JA, Cash BD. Guidelines for endoscopy in pregnant and lactating women. Gastrointest Endosc. 2012 Jul;76(1):18-24. doi: 10.1016/j.gie.2012.02.029. Epub 2012 May 12. Erratum in: Gastrointest Endosc. 2013 May;77(5):833.
- Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Library of Medicine (US); 2006-. Fentanyl. [Updated 2021 Feb 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK501222
- American Academy of Pediatrics Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics. 2001;108(3):776-789.
- Drug Enforcement Administration. Acetyl fentanyl Fact Sheet. July 2015. http://www.deadiversion.usdoj.gov/drug_chem_info/acetylfentanyl.pdf
- Drug Enforcement Administration. Acetyl fentanyl Fact Sheet. July 2015. http://www.deadiversion.usdoj.gov/drug_chem_info/acetylfentanyl.pdf
- FDA clears mobile medical app to help those with opioid use disorder stay in recovery programs. https://www.fda.gov/news-events/press-announcements/fda-clears-mobile-medical-app-help-those-opioid-use-disorder-stay-recovery-programs
- Ramos-Matos CF, Bistas KG, Lopez-Ojeda W. Fentanyl. [Updated 2021 Mar 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459275
- Comer SD, Cahill CM. Fentanyl: Receptor pharmacology, abuse potential, and implications for treatment. Neurosci Biobehav Rev. 2019 Nov;106:49-57. doi: 10.1016/j.neubiorev.2018.12.005