What is floppy eyelid syndrome
Floppy eyelid syndrome is an ophthalmologic disorder characterized by laxity of the upper eyelids leading to spontaneous eversion of the eyelids during sleep and other activities. Floppy eyelid syndrome is characterized by chronic papillary conjunctivitis in upper palpebral conjunctiva that is poorly respondent to topical lubrication and steroids. Floppy eyelid syndrome is often seen in overweight male patients with floppy, rubbery, and easily everted upper eyelids associated with a variable chronic papillary conjunctivitis of the upper palpebral conjunctiva. Floppy eyelid syndrome is generally associated with several systemic, non-ophthalmologic conditions, such as obstructive sleep apnea (OSA) and obesity, and causes significant ophthalmic comorbidities of the conjunctiva, cornea, lid, and tear film 1.
Floppy eyelid syndrome was originally described in middle-aged, obese men with papillary conjunctivitis in the setting of elastic, pliable upper eyelids 2. While it is still most commonly diagnosed in overweight men between the ages of 40-69 years old, the condition has also been reported in a broader patient population, including women and children 3. The diagnosis floppy eyelid syndrome is frequently found in patients with comorbid conditions such as obesity, hypertension, diabetes, hyperlipidemia, hyperglycinemia, Down syndrome, and conditions causing chronic eye rubbing (e.g. psoriasis, cocaine use, epibulbar nodular fasciitis, etc.) 4.
One of the strongest comorbid associations in floppy eyelid syndrome is with obstructive sleep apnea (OSA), which may have both diagnostic and therapeutic implications. An association between the two conditions was first described by Gonnering and Sonelland in 1987 5. Several studies have described the prevalence of obstructive sleep apnea in patients suffering from floppy eyelid syndrome and have found that between 31.3% and 96% of patients with floppy eyelid syndrome also have obstructive sleep apnea 4. Furthermore, a systematic review detailing the inverse relationship (the prevalence of floppy eyelid syndrome in patients with obstructive sleep apnea) found that up to 45.2% of patients with obstructive sleep apnea suffered from floppy eyelid syndrome 6. The importance of mandatory sleep testing for any patient with floppy eyelid syndrome cannot be overstated. Because obesity, male gender, and age are all independent risk factors for both obstructive sleep apnea and floppy eyelid syndrome, the causality of the relationship is less clear. However, it is known that patients’ sleeping postures, often affected by obstructive sleep apnea, can determine the laterality of their symptoms. That is, the eye affected by floppy eyelid syndrome typically corresponds to the side the patient sleeps on. If the patient alternates sides or sleeps face down, both eyes can be affected 7. Furthermore, as the severity of obstructive sleep apnea increases, as measured by the apnea-hypopnea index, the likelihood of floppy eyelid syndrome increases 8.
Patients with floppy eyelid syndrome typically present with non-specific eye complaints that are often unilateral, but can be bilateral. Irritation, tearing, discharge, itching, foreign body sensation, and general discomfort of the eye may be mentioned 4. The nonspecific nature of these complaints frequently leads to missed diagnosis, thus prolonging the patient’s clinical course.
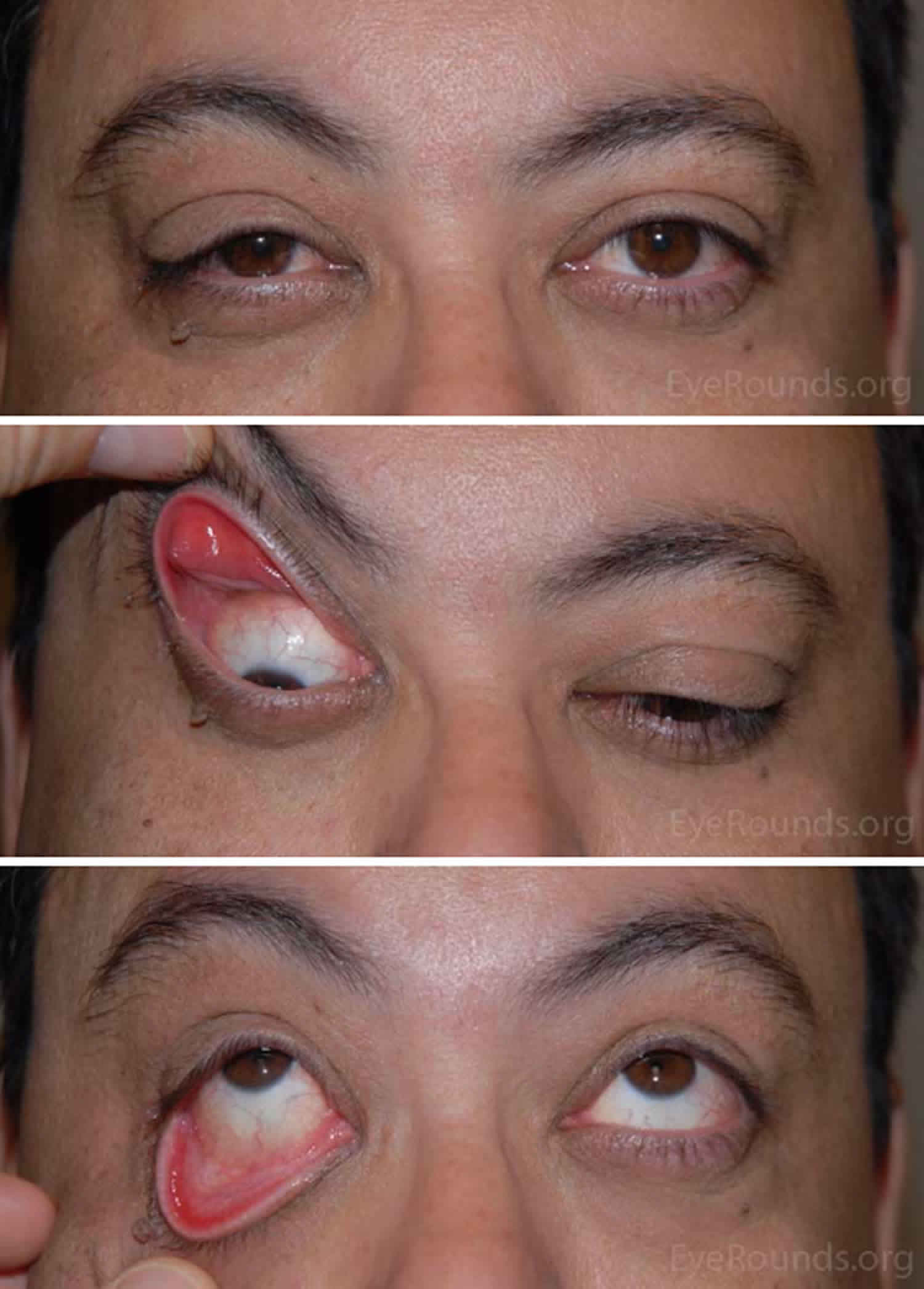
Figure 1. Floppy eyelid syndrome
Floppy eyelid syndrome causes
The extensive lid laxity can be attributed to significant decrease in elastin content when was tested by special stains, immunohistochemistry, and electron microscopy 9. Collagen content was not noted to be decreased in floppy eyelid syndrome patients. This was noticed to cause spontaneous eversion of the eyelid leading to chronic irritation and inflammation of the lid and palpebral conjunctiva and being mechanically irritated by constant rubbing of the palpebral conjunctiva with the pillow. The theory was further confirmed by the fact that patients who sleep on one side more than the other side tend to have more severe changes on that side. This finding suggests mechanical injury as the primary cause of the papillary conjunctivitis. Other postulated pathophysiology suggests that the cause of the chronic conjunctivitis is poor apposition of the lax upper eyelid to the globe with inadequate spreading of the tear film. This condition leads to corneal and conjunctival compromise, rather than direct mechanical irritation.
The pathophysiology of floppy eyelid syndrome and the frequently encountered ocular comorbidities are primarily thought to be caused by mechanical irritation. The initial insult is presumed to be chronic mechanical injury from eversion and/or rubbing of the eyelid. Several authors have speculated these mechanical forces may lead to loss of tarsal elasticity from pressure-induced ischemia-reperfusion, abnormalities in elastin, enzymatic breakdown of elastin, abnormal eyelid apposition, genetic predisposition or some combination thereof 10. Whatever the mechanism, the increased eyelid laxity results in the eyes becoming prone to exposure from nocturnal eversion and lagophthalmos. The prolonged and frequent nocturnal eversion results in exposure keratopathy that is nearly universally seen in these patients. Chronic irritation and inflammation of the cornea can progress to scarring and neovascularization. One of the most serious corneal complications associated with floppy eyelid syndrome is keratoconus, which has been found in 4% to 32% of patients suffering from floppy eyelid syndrome 11. In addition, chronic irritation of the conjunctiva manifloppy eyelid syndrometing as papillary conjunctivitis is frequently seen, as well as meibomitis, eyelash ptosis, and loss of eyelash parallelism 4.
Risk factors for floppy eyelid syndrome
Risk factors for floppy eyelid syndrome include:
- Obstructive sleep apnea (OSA)
- Obesity
- Male gender
- Hypertension
- Hyperlipidemia
- Chronic eye rubbing
- Down syndrome
Floppy eyelid syndrome signs and symptoms
Patients initially present with non-specific symptoms including eye irritation and a long history of unilateral or bilateral ocular redness and discharge. They may describe the eyelids spontaneously “flipping over” when they sleep due to rubbing on the pillow. Some patients may have a history of preexisting obstructive sleep apnea and/or history of heavy snoring. These symptoms in association with increased body mass index and a diagnosis of obstructive sleep apnea should alert the ophthalmologist about the high likelihood of having floppy eyelid syndrome. However, many reports have also documented the symptoms and signs of floppy eyelid syndrome in patients of both genders and without a history of obesity of sleep disorders.
Floppy eyelid syndrome symptoms may include:
- Irritation/foreign body sensation
- Tearing
- Itching
- Redness
- Discharge
Floppy eyelid syndrome signs:
- Easily everted upper eyelid with a soft, foldable tarsus
- Abnormal thickness of eyelid
- Rubbery consistency of superior eyelid
- Corneal findings:
- Punctate epitheliopathy
- Keratoconus
- Conjunctival findings:
- Papillary conjunctivitis
- Periorbital:
- Dermatochalasis, blepharochalasis, blepharoptosis, blepharitis, tear dysfunction, ectropion, lash ptosis
Floppy eyelid syndrome diagnosis
The diagnosis of floppy eyelid syndrome is made clinically, defined broadly as rubbery, malleable, and easily everted upper eyelids 12. Easy eversion of the eyelid without excess manipulation or even spontaneous eversion is an important examination mark for floppy eyelid syndrome with subsequent increased horizontal laxity and redundancy of the lid (see Figure 1). The lateral upper eyelid may appear elongated and imbricate (overlap) over the edge of the lower lid margin. Chronic severe papillary conjunctivitis with whitish mucus discharge.
Superficial punctate erosions, corneal, abrasions and microbial keratitis,and eyelashes ptosis are common clinical findings. Dry eyes with low tear meniscus. May be associated with keratoconus. Keratoconus can be linked to frequent rubbing and mechanical effect on the cornea.
Many authors have attempted to more narrowly and precisely define the syndrome; diagnostic criteria have been proposed and include objective measurements of clinical findings such as horizontal distraction, snapback, and vertical lid pull 4. Iyengar et al. 13 measured a series of patients’ upper eyelid laxity and demonstrated that there was a statistically significant difference in the measurement of anterior eyelid distraction in the patients’ symptomatic eyes versus asymptomatic eyes. Regardless of the specific criteria considered, the diagnosis of floppy eyelid syndrome should be considered when a patient presents with any of the symptoms listed below in the setting of loose, easily everted upper eyelids.
Eyelid
- Dermatochalasis
- Blepharitis
- Blepharoptosis
- Meibomitis
- Upper lid lash ptosis
- Lower lid laxity
- Extropion (lower lid)
- Entropion (upper lid)
Cornea
- Superficial punctate kertopathy
- Erosions/ulcers
- Neovascularization
- Keratoconus
Sclera/Conjuctiva
- Papillary conjunctivitis
- Epidulbar nodular fasciitis
- Dry eye
- Pseudopterygium
- Keratoconjuncitivitis
Other
- Lipid tear film deficiency
- Glaucoma
- Meibomian gland dysfunction
Floppy eyelid syndrome treatment
The treatment of floppy eyelid syndrome depends on both the severity of the patient’s symptoms and, if present, the treatment of patients’ underlying obstructive sleep apnea (OSA). Conservative management may be used initially and includes eye shields and lubricating ointment at night. The shields prevent nocturnal eversion of the lids and often results in a rapid resolution of the symptoms. In addition, treatment of the sleep apnea with continuous positive airway pressure (CPAP) alone will result in resolution of the symptoms.
Floppy eyelid syndrome surgery
Surgical intervention involves tightening the eyelids by removing excess tissue. Several surgical methods have been used and include full thickness wedge excision, medial/lateral tarsal strip, and medial/lateral canthal tendon plication 4. There is evidence to suggest that the tarsal strip and canthal tendon plication surgeries show better long-term outcome in terms of symptom recurrence when compared to the full thickness wedge excision 14. It is important to note that, because floppy eyelid syndrome may be the presenting symptom in a patient with obstructive sleep apnea, the patient should be referred for polysomnography prior to surgical intervention for floppy eyelid syndrome. Surgery should be considered only once the patient’s obstructive sleep apnea is treated, otherwise the same mechanical stresses will “stretch” the patient’s eyelids necessitating further treatment and surgical repair. In addition, treatment of the eyelid laxity is necessary prior to treating any coexisting eyelid abnormalities such as ptosis, as the instability of a lax lid may lead to unpredictable surgical results.
References- Pham, Thu T., and Julian D. Perry. “Floppy eyelid syndrome.” Current opinion in ophthalmology 18.5 (2007): 430-433.
- Culbertson, William W., and H. Bruce Ostler. “The floppy eyelid syndrome.” American journal of ophthalmology 92.4 (1981): 568-575.
- Gross, Robert H., and Mark J. Mannis. “Floppy eyelid syndrome in a child with chronic unilateral conjunctivitis.” American journal of ophthalmology 124.1 (1997): 109-110.
- Ezra, Daniel G., Michèle Beaconsfield, and Richard Collin. “Floppy eyelid syndrome: stretching the limits.” Survey of ophthalmology 55.1 (2010): 35-46.
- Gonnering, Russell S., and Paula R. Sonneland. “Meibomian gland dysfunction in floppy eyelid syndrome.” Ophthalmic Plastic & Reconstructive Surgery 3.2 (1987): 99-104.
- Huon, Leh-Kiong, et al. “The association between ophthalmologic diseases and obstructive sleep apnea: a systematic review and meta-analysis.” Sleep and Breathing (2016): 1-10.
- McNab, Alan A. “The eye and sleep apnea.” Sleep medicine reviews 11.4 (2007): 269-276.
- Acar, Mutlu, et al. “Ocular surface assessment in patients with obstructive sleep apnea–hypopnea syndrome.” Sleep and Breathing 17.2 (2013): 583-588.
- Floppy eyelid syndrome. https://eyewiki.org/Floppy_eyelid_syndrome
- Schlötzer-Schrehardt, Ursula, et al. “The pathogenesis of floppy eyelid syndrome: involvement of matrix metalloproteinases in elastic fiber degradation.” Ophthalmology 112.4 (2005): 694-704.
- Pihlblad, Matthew S., and Daniel P. Schaefer. “Eyelid laxity, obesity, and obstructive sleep apnea in keratoconus.” Cornea 32.9 (2013): 1232-1236.
- Floppy eyelid syndrome. https://webeye.ophth.uiowa.edu/eyeforum/cases/240-Floppy-Eyelid-Syndrome.htm
- Iyengar, Srinivas S., and Jemshed A. Khan. “Quantifying upper eyelid laxity in symptomatic floppy eyelid syndrome by measurement of anterior eyelid distraction.” Ophthalmic Plastic & Reconstructive Surgery 23.3 (2007): 255.
- Ezra, Daniel G., et al. “Long-term outcomes of surgical approaches to the treatment of floppy eyelid syndrome.” Ophthalmology 117.4 (2010): 839-846.





