What is FSH
FSH is short for follicle-stimulating hormone. FSH is a hormone associated with reproduction and the development of eggs in women and sperm in men. FSH is made by the anterior pituitary gland, a grape-sized organ located at the base of the brain. Control of FSH production is a complex system involving the hypothalamus in the brain, the pituitary gland, and the hormones produced by the ovaries or testicles. The hypothalamus releases gonadotropin-releasing hormone (GnRH), which stimulates the pituitary to release FSH and luteinizing hormone (LH), a closely related hormone also involved in reproduction. Secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) is low in both males and females prior to puberty. Following puberty, more luteinizing hormone (LH) than follicle-stimulating hormone (FSH) is secreted. During the menstrual cycle there is a dramatic increase in the serum concentrations of both hormones at the time of ovulation, and the secretion of both hormones increases 10- to 15-fold in postmenopausal women.
- In women, FSH stimulates the growth and maturation of eggs (follicles) in the ovaries during the follicular phase of the menstrual cycle. The menstrual cycle is divided into the follicular and the luteal phases, with each phase lasting about 14 days. During this follicular phase, FSH initiates the production of estradiol by the follicle, and the two hormones work together in the further development of the egg follicle. Near the end of the follicular phase, there is a surge of FSH and luteinizing hormone. Release of the egg from the ovary (ovulation) occurs shortly after this surge of hormones. The hormone inhibin as well as estradiol and progesterone help control the amount of FSH released by the pituitary gland. FSH also facilitates the ability of the ovary to respond to LH. As a woman ages and menopause approaches, ovarian function wanes and eventually ceases. As this occurs, FSH and LH levels rise.
- In men, FSH stimulates the testicles to produce mature sperm and also promotes the production of androgen binding proteins. FSH levels are relatively constant in men after puberty.
- In infants and children, FSH levels rise shortly after birth and then fall to very low levels by 6 months in boys and 1-2 years in girls. Concentrations begin to rise again before the beginning of puberty and the development of secondary sexual characteristics.
Disorders affecting the hypothalamus, pituitary, and/or the ovaries or testicles can cause the production of too much or too little FSH, resulting in a variety of conditions such as infertility, abnormal menstrual cycles, or early (precocious) or delayed sexual maturation (puberty).
Pulsatile secretion of gonadotropin-releasing hormone (GnRH) into the hypophyseal portal circulation represents the initial neuroendocrine step in the regulation of the hypothalamo-pituitary-gonadal axis in both sexes. Thus, this specialized gonadotropin-releasing hormone (GnRH) neuronal network plays a commanding role in this biologic hierarchy and controls episodic gonadotropin secretion, modulates gonadal steroid feedback, and ultimately determines the initiation or suppression of pubertal development and fertility across the life cycle 1.
Under normal conditions, the gonadotropin-releasing hormone (GnRH) neuronal network undergoes a series of dynamic changes from fetal life to adulthood. The initiation of gonadotropin-releasing hormone (GnRH) secretion is initiated in early fetal life and remains active until the first several months of infancy (representing the “mini-puberty”), and then becomes remarkably dampened during the years of the childhood “quiescence” 2. At puberty, unknown biologic triggers re-ignite gonadotropin-releasing hormone (GnRH) secretion, resulting in full sexual maturation. Therefore, the controls of the reproductive axis are in dynamic flux, turning on and turning off in response to as-yet-unknown biologic signals at various points in the reproductive life cycle.
- In boys, luteinizing hormone (LH) and follicle-stimulating hormone (FSH) work together to get the testes to begin producing testosterone, the hormone responsible for the physical changes of puberty and the production of sperm. Testosterone is the hormone that causes most of the changes in a boy’s body during puberty. Sperm cells must be produced for men to reproduce.
- In girls, luteinizing hormone (LH) and follicle-stimulating hormone (FSH) prompt the ovaries to begin producing the hormone estrogen, which causes a girl’s body to mature and prepares her for menstruation. Estrogen, along with luteinizing hormone (LH) and follicle-stimulating hormone (FSH), causes a girl’s body to mature and prepares her for pregnancy.
- In men, follicle-stimulating hormone (FSH) stimulates the development of spermatozoa, in large part by acting on special cells in the testes called Sertoli cells. Luteinizing hormone (LH) stimulates the secretion of androgen (male) hormones by specialized cells in the testes called Leydig cells.
- In women, follicle-stimulating hormone (FSH) stimulates the synthesis of estrogens and the maturation of cells lining the spherical egg-containing structures known as Graafian follicles. In menstruating women, there is a preovulatory surge in serum follicle-stimulating hormone (FSH) and luteinizing hormone (LH) concentrations. The preovulatory surge of luteinizing hormone (LH) is essential for rupture of the Graafian follicle (ovulation), after which the egg enters the fallopian tube and travels to the uterus. The empty Graafian follicle becomes filled with progesterone-producing cells, transforming it into a corpus luteum. Luteinizing hormone (LH) stimulates the production of progesterone by the corpus luteum.
- Inhibin, a hormone secreted by the Graafian follicles of the ovaries and by the Sertoli cells of the testes, inhibits the secretion of follicle-stimulating hormone (FSH) from the pituitary gonadotrophs.
Patients with diseases involving the anterior pituitary gland often have gonadotropin deficiency. Thus, the disappearance of menstrual periods may be the first sign of a pituitary tumor or other pituitary disease in women. In men the most common symptoms of gonadotropin deficiency are loss of libido and erectile dysfunction. Isolated deficiencies of both luteinizing hormone (LH) and follicle-stimulating hormone (FSH) do occur but only rarely. In men isolated luteinizing hormone (LH) deficiency (“fertile eunuch”) is characterized by symptoms and signs of androgen deficiency; however, there is sufficient secretion of follicle-stimulating hormone (FSH) to permit the maturation of spermatozoa. Some pituitary tumors produce an excess of luteinizing hormone (LH) or follicle-stimulating hormone (FSH), whereas other pituitary tumors produce the hormonally inactive alpha chain subunit of the glycoprotein hormones.
Because luteinizing hormone (LH) and follicle-stimulating hormone (FSH) work so closely with each other, doctors often perform these tests together, as well as tests for testosterone (the major male sex hormone) and estradiol (a form of estrogen, the major female sex hormone). Taken together, the results can often provide a more complete picture of a person’s sexual maturation, and the well-being of the endocrine glands that produce these hormones.
Figure 1. The pituitary gland location
Figure 2. Pituitary gland
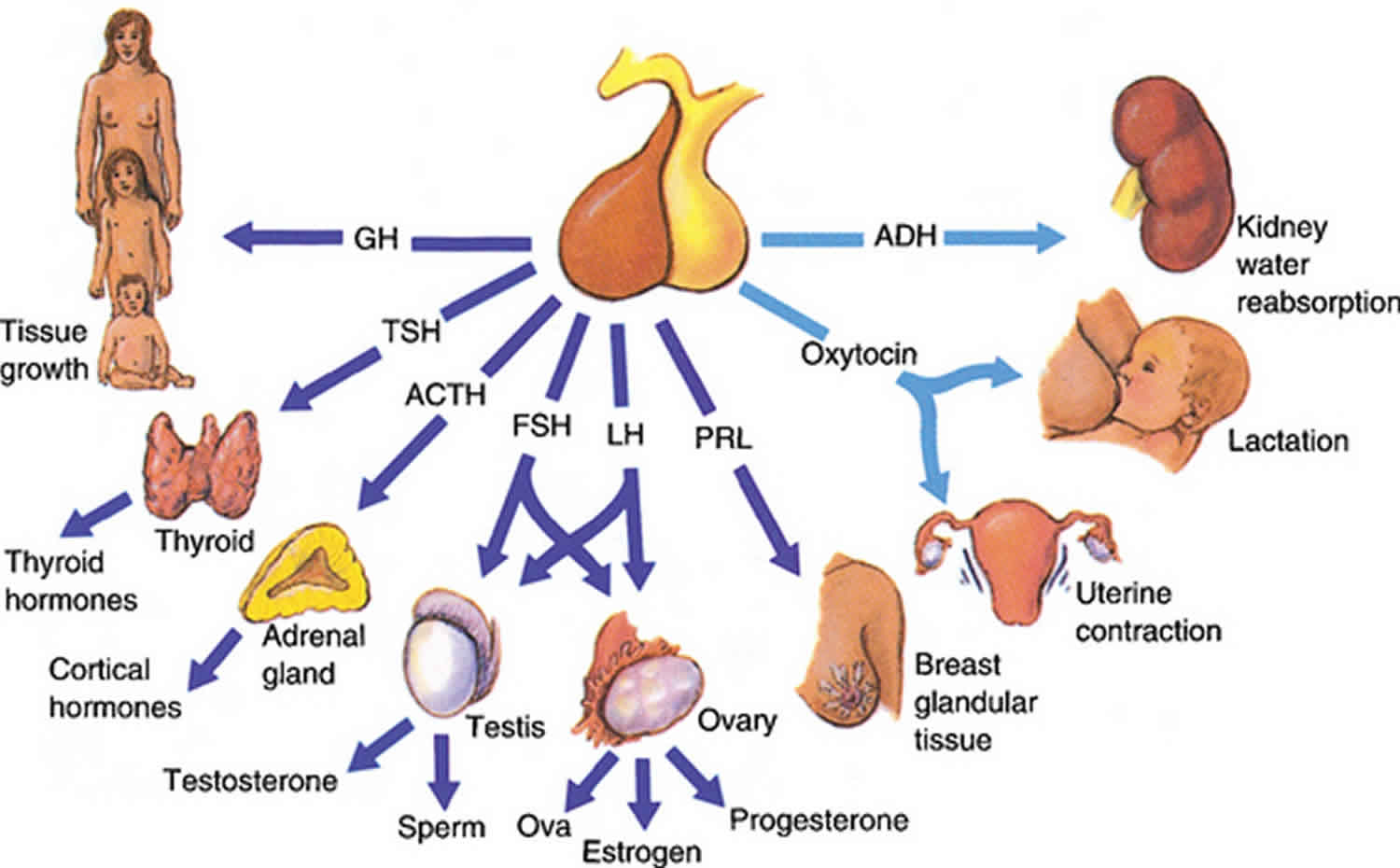
Figure 3. Gonadotropins (FSH and LH)
Figure 4. Pituitary gland hormones under the influence of the hypothalamus controlling the ovaries production of egg cell, ovulation and development of the female secondary sex characteristics
Figure 5. Ovarian activity during the Menstrual cycle
FSH function
FSH and LH regulate the functions of the ovaries and the testes.
In females, FSH stimulates growth and development of follicles in preparation for ovulation and secretion of estrogens by the mature Graafian follicle. LH triggers ovulation and stimulates the secretion of progesterone by the corpus luteum.
In males, FSH is required for spermatogenesis, and LH stimulates testosterone secretion by Leydig cells.
FSH test
FSH blood test measures FSH in your blood, a hormone associated with reproduction and the development of eggs in women and sperm in men, has several uses.
In both women and men, the FSH test may be used with other hormone tests such as luteinizing hormone (LH), testosterone, estradiol, and/or progesterone to help:
- Determine the cause of infertility
- Diagnose conditions associated with dysfunction of the ovaries or testicles
- Aid in the diagnosis of pituitary or hypothalamus disorders, which can affect FSH production
In women, FSH levels are also useful in:
- The investigation of menstrual irregularities
- Predicting onset or confirmation of menopause
In men, FSH levels are used to help determine the reason for a low sperm count.
In children, FSH and LH are used to help diagnose delayed or precocious (early) puberty. Irregular timing of puberty may be an indication of a more serious problem involving the hypothalamus, the pituitary gland, the ovaries or testicles, or other systems. The measurement of LH and FSH may differentiate between benign symptoms and true disease. Once it is established that symptoms are a result of true disease, further testing can be done to discern the underlying cause.
When is FSH test ordered?
For a woman, an FSH test may be ordered when she is having difficulty getting pregnant or has irregular or an absence of menstrual periods.
FSH may be ordered when a woman’s menstrual cycle has stopped or become irregular, to determine if the woman has entered menopause.
For a man, the test may be ordered when his partner cannot get pregnant, when he has a low sperm count, or when he has low muscle mass or decreased sex drive, for example.
In both women and men, testing may be ordered when a health practitioner suspects that a pituitary disorder is present. A pituitary disorder can affect the production of several different hormones, so there may be signs and symptoms in addition to some of those listed above. They can include fatigue, weakness, unexplained weight loss, and decreased appetite to name a few.
In children, FSH and LH may be ordered when a boy or girl does not appear to be entering puberty at an appropriate age (either too late or too soon). Signs of puberty may include:
- Breast enlargement in girls
- Growth of pubic hair
- Growth of the testicles and penis in boys
- Beginning of menstruation in girls
Normal FSH levels
Males
- Age <12 months: < or =3.3 IU/L
- Age > or =12 months-< or =5 years: < or =1.9 IU/L
- Age >5 years-< or =10 years: < or =2.3 IU/L
- Age >10 years-< or =15 years: 0.6-6.9 IU/L
- Age >15 years-< or =18 years: 0.7-9.6 IU/L
- Age >18 years: 1.2-15.8 IU/L
MALE TANNER STAGES*
- Stage l: <1.5 IU/L
- Stage ll: <3.0 IU/L
- Stage lll: 0.4-6.2 IU/L
- Stage lV: 0.6-5.1 IU/L
- Stage V: 0.8-7.2 IU/L
*Puberty onset occurs for boys at a median age of 11.5 (+/- 2) years. For boys there is no proven relationship between puberty onset and body weight or ethnic origin. Progression through Tanner stages is variable. Tanner stage V (adult) should be reached by age 18.
Females
- Age <12 months: 1.2-12.5 IU/L
- Age > or =12 months -< or =10 years: 0.5-6.0 IU/L
- Age >10 years-< or =15 years: 0.9-8.9 IU/L
- Age >15 years-< or =18 years: 0.7-9.6 IU/L
FEMALE TANNER STAGES*
- Stage l: 0.6-4.1 IU/L
- Stage ll: 0.3-5.8 IU/L
- Stage lll: 0.1-7.2 IU/L
- Stage lV: 0.3-7.0 IU/L
- Stage V: 0.4-8.6 IU/L*Puberty onset (transition from Tanner stage I to Tanner stage II) occurs for girls at a median age of 10.5 (+/- 2) years. There is evidence that it may occur up to 1 year earlier in obese girls and in African American girls. Progression through Tanner stages is variable. Tanner stage V (adult) should be reached by age 18.
Premenopausal:
- Follicular: 2.9-14.6 IU/L
- Midcycle: 4.7-23.2 IU/L
- Luteal: 1.4-8.9 IU/L
Postmenopausal: 16.0-157.0 IU/L
What are Tanner Stages?
Tanner Staging, also known as Sexual Maturity Rating, is an objective classification system that healthcare providers use to document and track the development and sequence of secondary sex characteristics of children during puberty 3. Tanner Staging was developed by Marshall and Tanner while conducting a longitudinal study during the 1940s-1960s in England. Based on observational data, they developed separate scales for the development of external genitalia: phallus, scrotum, and testes volume in males; breasts in females; and pubic hair in both males and females.
Below are the Tanner Stages described in detail for clinical reference. For all three sites of development, Tanner Stage 1 corresponds to the pre-pubertal form with progression to Tanner Stage 5, the final adult form. Breast and genital staging, as well as other physical markers of puberty such as height velocity, should be relied on more than pubic hair staging to assess pubertal development because of the independent maturation of adrenal axis.
Pubic Hair Scale (both males and females)
- Stage 1: No pubic hair at all (prepubertal) (typically age 10 and younger)
- Stage 2: Downy hair with slight pigmentation at the base of the penis and scrotum (males) or on the labia majora (females) (age 10–11.5)
- Stage 3: Scant terminal hair – hair becomes more coarse and curly, and begins to extend laterally (age 11.5–13)
- Stage 4: Terminal hair that fills the entire triangle overlying the pubic region but sparing medial thighs (age 13–15)
- Stage 5: Terminal hair that extends beyond the inguinal crease onto the thigh (age 15+)
Female Breast Development Scale
- Stage 1: No glandular breast tissue palpable – areola follows the skin contours of the chest (prepubertal) (typically age 10 and younger)
- Stage 2: Breast bud palpable under areola (1st pubertal sign in females) – areola begins to widen (age 10–11.5)
- Stage 3: Breast begins to become more elevated, and extends beyond the borders of the areola, which continues to widen but remains in contour with surrounding breast (age 11.5–13)
- Stage 4: Areola elevated above contour of the breast, forming “double scoop” appearance (age 13–15)
- Stage 5: Areolar mound recedes back into single breast contour with areolar hyperpigmentation, papillae development and nipple protrusion (age 15+)
Figure 6. Tanner Stage Female
Male External Genitalia Scale
- Stage 1: Testicular volume < 4 ml or long axis < 2.5 cm
- Stage 2: 4 ml-8 ml (or 2.5-3.3 cm long), 1st pubertal sign in males
- Stage 3: 9 ml-12 ml (or 3.4-4.0 cm long)
- Stage 4: 15-20 ml (or 4.1-4.5 cm long)
- Stage 5: > 20 ml (or > 4.5 cm long)
Figure 7. Tanner Stage Male
What does abnormal FSH test result mean?
Results of an FSH test are typically considered with results of other hormone tests, such as LH , estrogens, and/or testosterone.
In both males and females, primary hypogonadism results in an elevation of basal follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels.
FSH and LH are generally elevated in:
- Primary gonadal failure
- Complete testicular feminization syndrome
- Precocious puberty (either idiopathic or secondary to a central nervous system lesion)
- Menopause (postmenopausal FSH levels are generally >40 IU/L)
- Primary ovarian hypofunction in females
- Primary hypogonadism in males
FSH levels can also be increased with use of certain drugs, including cimetidine, clomiphene, digitalis, and levodopa.
Normal or decreased FSH in:
- Polycystic ovary disease in females
FSH and LH are both decreased in failure of the pituitary or hypothalamus.
FSH levels can also be decreased with oral contraceptives, phenothiazines, and hormone treatments. FSH will also be low when women are pregnant. A recent nuclear medicine scan may interfere with results of the FSH test if it is measured by a radioimmunoassay, which is seldom used any more.
And as part of an infertility workup, a high or low FSH is not diagnostic but provides a piece of information on what may be the cause. For example, a hormone imbalance may affect a woman’s menstrual cycle and/or ovulation. A health practitioner will consider all the information from the workup to establish a diagnosis.
Note: Some patients who have been exposed to animal antigens, either in the environment or as part of treatment or imaging procedures, may have circulating antianimal antibodies present. These antibodies may interfere with the assay reagents to produce unreliable results.
In Women
FSH and LH levels can help to differentiate between primary ovarian failure (failure of the ovaries themselves) and secondary ovarian failure (failure of the ovaries due to disorders of either the pituitary or the hypothalamus).
High levels of FSH and LH are consistent with primary ovarian failure. Some causes of primary ovarian failure are listed below.
Developmental defects:
- Failure to develop ovaries (ovarian agenesis)
- Chromosomal abnormality, such as Turner syndrome
- Defect in the steroid production by the ovaries, such as 17 alpha hydroxylase deficiency
Premature failure of the ovaries due to:
- Radiation exposure
- Chemotherapy
- Autoimmune disease
Chronic failure to ovulate (anovulation) due to:
- Polycystic ovary syndrome (PCOS)
- Adrenal disease
- Thyroid disease
- Ovarian tumor
When a woman enters menopause and her ovaries stop working, FSH levels will rise.
Low levels of FSH and LH are consistent with secondary ovarian failure due to a pituitary disorder or hypothalamic problem. Low FSH serum levels have been associated with increased risk of ovarian cancer.
In Men
High FSH levels are due to primary testicular failure. This can be the result of developmental defects in testicular growth or to testicular injury, as indicated below.
Developmental defects:
- Failure to develop gonads (gonadal agenesis)
- Chromosomal abnormality, such as Klinefelter syndrome
Testicular failure:
- Viral infection (mumps)
- Trauma
- Radiation exposure
- Chemotherapy
- Autoimmune disease
- Germ cell tumor
Low levels are consistent with pituitary or hypothalamic disorders.
In Children
High levels of FSH and LH with the development of secondary sexual characteristics at an unusually young age are an indication of precocious puberty. This is much more common in girls than in boys. This premature development is usually due to a problem with the central nervous system and can have a few different underlying causes. Examples include:
- Central nervous system tumor
- Brain injury, trauma
- Inflammation within the central nervous system (e.g. meningitis, encephalitis)
- Brain surgery
Normal prepubescent levels of LH and FSH in children exhibiting some signs of pubertal changes may indicate a condition call “precocious pseudopuberty.” The signs and symptoms are brought on by elevated levels of the hormones estrogen or testosterone. This may be caused by:
- Hormone-secreting tumors
- Adrenal gland tumors
- Ovarian tumors or cysts
- Testicular tumors
Normal FSH and LH levels with a few signs of puberty can also be a benign form of precocious puberty with no underlying or discernable cause or may just be a normal variation of puberty.
In delayed puberty, LH and FSH levels can be normal or below what is expected for a youth within this age range. Some of the causes for delayed puberty can include:
- Dysfunction of the ovaries or testicles
- Hormone deficiency
- Turner syndrome
- Klinefelter syndrome
- Chronic infections
- Cancer
- Eating disorder (anorexia nervosa)
What is menopause?
Menopause is the stage in women’s life when menstruation stops for at least 12 months. The time before this is called perimenopause and could last for several years. You may reach menopause in your early 40’s or as late as your 60’s.
I’m having a hard time getting pregnant. What tests do I need?
Basic tests for infertility often include measuring FSH and luteinizing hormone (LH) levels. Your healthcare provider may also ask you to keep track of your body temperature, which rises slightly during ovulation. Other hormonal tests as well as a postcoital (after intercourse) examination may be done. A hysterosalpingogram (image of fallopian tubes) may be ordered to see whether your fallopian tubes are blocked. Your partner may be asked to give a specimen of semen for analysis.
Why would a woman have multiple FSH tests done and a man only have one?
Multiple FSH tests may be performed for a woman in order to track FSH concentrations over time. In women, concentrations of FSH are cyclic, peaking each month; men have more stable FSH levels.
Why would a man need a test for FSH and LH; I thought these were female hormones?
Men also produce FSH and LH. These hormone levels are important for male reproduction too. In men, FSH stimulates the testicles to produce sperm just as in women FSH stimulates the ovaries to produce eggs. In men, LH can be measured if testosterone levels are low.
Is there a home test for FSH?
Yes. There is an FDA-approved self-test that measures the level of FSH in a urine sample. It is used as an indicator of perimenopause, which is associated with a rise in FSH levels. For more information, visit this FDA website (https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/HomeUseTests/ucm125824.htm).
What type of FSH test is this?
FSH self-test (FSH home urine test) is a qualitative test — you find out whether or not you have elevated FSH levels, not if you definitely are in menopause or perimenopause.
Are the home menopause tests similar to the ones my doctor uses?
Some home menopause tests are identical to the one your doctor uses. However, doctors would not use this test by itself. Your doctor would use your medical history, physical exam, and other laboratory tests to get a more thorough assessment of your condition.
Why should I do FSH self-test?
You should use FSH self-test if you want to know if your symptoms, such as irregular periods, hot flashes, vaginal dryness, or sleep problems are part of menopause. While many women may have little or no trouble when going through the stages of menopause, others may have moderate to severe discomfort and may want treatment to alleviate their symptoms. FSH self-test may help you be better informed about your current condition when you see your doctor.
How accurate is FSH self-test?
FSH self-tests will accurately detect FSH about 9 out of 10 times. FSH self-test does not detect menopause or perimenopause. As you grow older, your FSH levels may rise and fall during your menstrual cycle. While your hormone levels are changing, your ovaries continue to release eggs and you can still become pregnant.
Your FSH self-test will depend on whether you:
- used your first morning urine,
- drank large amounts of water before the test,
- use, or recently stopped using, oral or patch contraceptives, hormone replacement therapy, or estrogen supplements.
How do I do FSH self-test?
In FSH self-test, you put a few drops of your urine on a test device, put the end of the testing device in your urine stream, or dip the test device into a cup of urine. Chemicals in the test device react with FSH and produce a color. Read the instructions with the FSH self-test you buy to learn exactly what to look for in this test.
Does a positive FSH self-test mean I’m in menopause?
A positive FSH self-test indicates that you may be in a stage of menopause. If you have a positive test, or if you have any symptoms of menopause, you should see your doctor. Do not stop taking contraceptives based on the results of these tests because they are not foolproof and you could become pregnant.
Do negative FSH self-test results indicate that I’m not in menopause?
If you have a negative FSH self-test result, but you have symptoms of menopause, you may be in perimenopause or menopause. You should not assume that a negative test means you have not reached menopause, there could be other reasons for the negative result. You should always discuss your symptoms and your test results with your doctor. Do not use these FSH self-tests to determine if you are fertile or can become pregnant. These tests will not give you a reliable answer on your ability to become pregnant.
References- Crowley WF Jr, Filicori M, Spratt DI, Santoro NF. The physiology of gonadotropin-releasing hormone (GnRH) secretion in men and women. Recent Prog Horm Res. 1985;41:473–531.
- Waldhauser F, Weissenbacher G, Frisch H, Pollak A. Pulsatile secretion of gonadotropins in early infancy. Eur J Pediatr. 1981;137:71–4
- Emmanuel M, Bokor BR. Tanner Stages. [Updated 2017 Dec 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470280