Galeazzi fracture
Galeazzi fracture dislocation is a fracture of the distal third and middle third of the radius with dislocation of distal radioulnar joint and an intact ulna. A Galeazzi-equivalent fracture is a distal radial fracture with a distal ulnar physeal fracture 1.
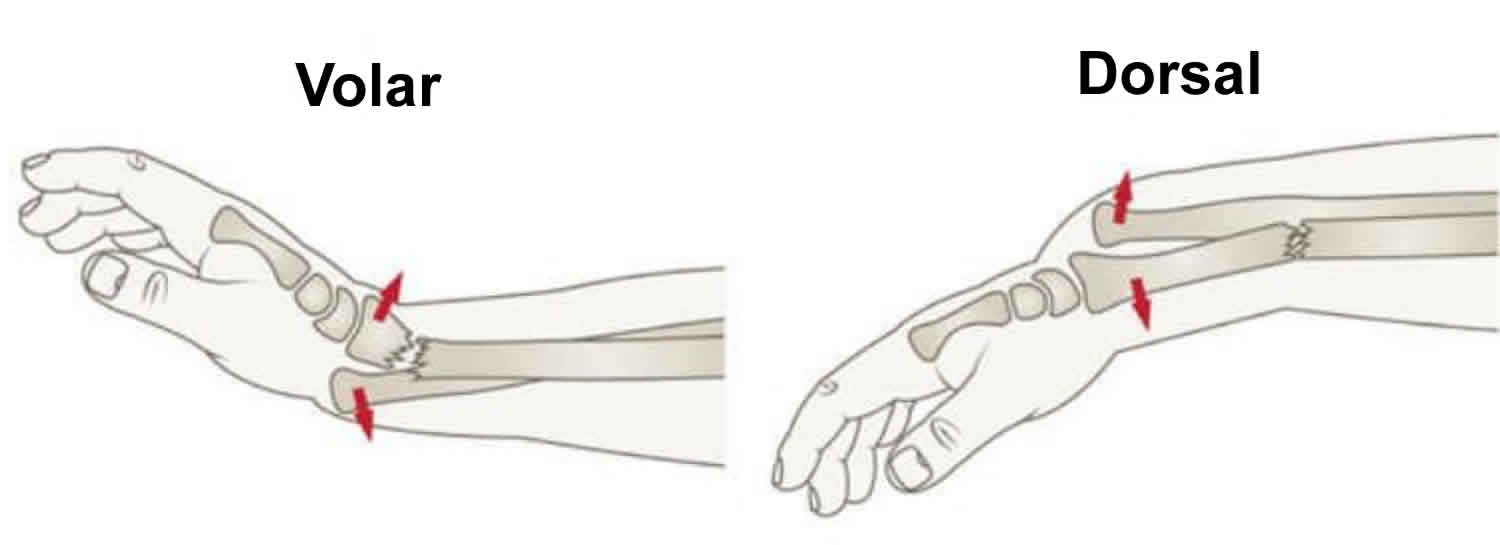
Galeazzi fractures can be classified by the direction of the ulna displacement:
- Dorsal Galeazzi: dorsal ulna displacement
- Volar Galeazzi: volar (anterior) ulna displacement
Galeazzi fractures account for 3-7% of all forearm fractures. Galeazzi fractures are primarily encountered in children, with a peak incidence at age 9-12 years 2. Although Galeazzi fracture patterns are reportedly uncommon, they are estimated to account for 7% of all forearm fractures in adults 2.
Galeazzi fracture dislocation are unstable and operative fixation is usually required to reduce and fix the radial fracture, with arm immobilization in pronation 3. The exact mode of fixation depends on the location of the radial fracture 3:
- diaphysis: elastic nail
- metaphyseal-diaphyseal junction: plate and screw
- distal radius: Kirschner wires (K-wires)
In Galeazzi-equivalent fractures, ulnar physeal arrest is frequent, seen in 55% of cases.
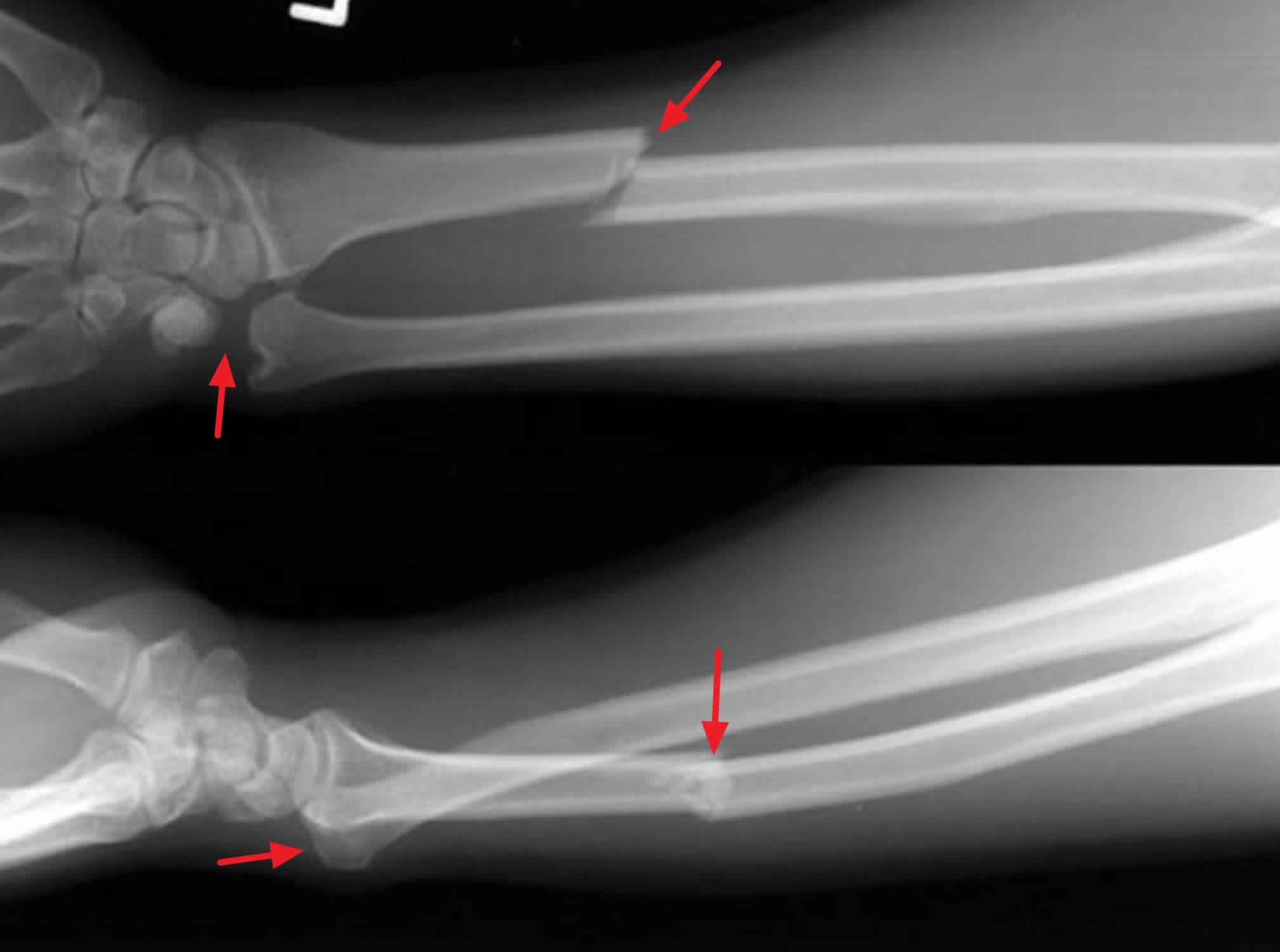
Figure 1. Galeazzi fracture dislocation
Galeazzi fracture anatomy
The forearm is composed of the radius and ulna bones. The radius and ulna are stabilized by three groups of ligamentous structures: distally the triangular fibrocartilage complex, the interosseous membrane, and proximally the annular ligament. The interosseous membrane is responsible for dispersing axial load force to the forearm, 60% to the radiocapitellar joint and 40% to the ulnohumeral joint. The radiocapitellar joint largely stabilizes the proximal forearm while the triangular fibrocartilage complex predominantly supports the distal forearm. Proximally the ulna consists of the olecranon and coronoid. Distally the ulnar head serves as an insertion point for the triangular fibrocartilage complex, supplementing the distal radioulnar joint. The proximal radial head articulates with the capitellum of the humerus (radiocapitellar joint), rotating within the annular ligament during pronation and supination. Distally the radius connects with the lunate and scaphoid bones of the wrist.
Galeazzi fracture causes
The cause of the Galeazzi fracture is thought to be a fall on an outstretched hand in association with hyper-pronation of the forearm. The energy from the radius fracture gets transmitted towards the radioulnar joint leading to dislocation of the distal radioulnar joint. These fractures occur with a bimodal distribution, diaphyseal forearm fractures in young males are commonly due to high-energy trauma (e.g., sports injuries, falls from height, motor vehicle collisions) and fractures in aging females are due to low-energy traumas such as falls from ground level 4.
Galeazzi fracture symptoms
Pain and soft-tissue swelling are present at the distal-third radial fracture site and at the wrist joint. Galeazzi fracture dislocation is confirmed on radiographic evaluation.
Forearm trauma may be associated with compartment syndrome.
Anterior interosseous nerve palsy may also be present, but it is often overlooked because there is no sensory component to this finding. A purely motor nerve, the anterior interosseous nerve is a division of the median nerve. Injury to the anterior interosseous nerve can cause paralysis of the flexor pollicis longus and flexor digitorum profundus to the index finger, resulting in loss of the pinch mechanism between the thumb and the index finger 5.
Galeazzi fracture complications
The complexity of Galeazzi fractures leads to a variety of outcomes. It is estimated that the overall complication rates of Galeazzi fractures are close to 40%. Children usually fare better than their adult counterparts. As time passes without the correct identified diagnosis, the more difficult it becomes to manage the injury, and the patient is more likely to have significant morbidity.
Forearm midshaft fractures have malunion or nonunion occurring in approximately 2% to 10% of cases, which is higher than the average forearm fracture nonunion rate (2%). Other notable complications include acute compartment syndrome (pre- and post-surgical), radioulnar synostosis (1% to 6%), elbow stiffness from protracted immobilization (adults), myositis ossificans, ulnohumeral osteoarthritis, and wound infections (0% to 3%).
Muscle-tendon entrapment may occur with significant injuries. The extensor carpi ulnaris, extensor digiti minimi, and flexor pollicis longus tendons are the most common to become entrapped with Galeazzi fractures. They can make reduction difficult and may require surgical repair to avoid chronic instability.
Branches of the radial nerve are the most common neurovascular structures to get injured. This is usually due to laceration of the radial sensory nerves during a volar surgical approach. The most common associated motor deficit is from injury to the posterior interosseous nerve, which can get damaged during a dorsal surgical approach. Transient injury to the anterior osseous nerve branch of the median nerve has been reported. Ulnar nerve injuries are rare. Nerve injuries rarely require treatment, and the majority of patients have complete resolution of symptoms in 9 to 12 weeks
Galeazzi fracture diagnosis
The diagnosis of a Galeazzi fracture is confirmed on radiographic examination. Standard anteroposterior (AP) and true lateral forearm views are obtained, which must include an anteroposterior (AP) or a posteroanterior (PA) view, as well as a lateral view, of the wrist, along with AP and lateral views of the elbow. Radiographs of the contralateral extremity can be obtained for comparison.
Plain radiographic findings suggestive of injury to the distal radioulnar joint are as follows:
- Fracture at the ulnar styloid base
- Widening of the distal radioulnar joint space on an anteroposterior (AP) radiograph
- Dislocation of the radius relative to the ulna on a true lateral radiograph, which is obtained with the shoulder abducted 90°
- Shortening of the radius by more than 5 mm relative to the distal ulna
Assessment of distal radioulnar joint integrity is often difficult with plain radiography alone. Bilateral axial computed tomography (CT) of the forearm is the preferred imaging study for diagnosing distal radioulnar joint disruption.
A study by Tsismenakis et al 6 found that the radiographic guidelines in general use were only moderately accurate in predicting distal radioulnar joint instability and that treatment was best determined on the basis of intraoperative assessment of the distal radioulnar joint after radial fixation.
Figure 2. Galeazzi fracture
Galeazzi fracture treatment
Galeazzi fractures are best treated with open reduction of the radius and the distal radioulnar joint. Closed reduction and cast application have led to unsatisfactory results. All adult Galeazzi fractures must be treated with open reduction and internal fixation (ORIF) 7. Anatomic surgical reduction of the radius and the distal radioulnar joint provides the best opportunity for healing.
Open forearm fractures constitute a surgical emergency. Open wounds may have to be incorporated into the surgical incision. Immediate stabilization of the radial fracture and the distal radioulnar joint is recommended.
Galeazzi fractures in skeletally immature patients are typically treated with closed reduction and casting because of the enhanced viscoelastic nature of pediatric bone, as well as the presence of a stout periosteal sleeve 8.
The only contraindication to surgical intervention is the existence of life-threatening conditions, which take priority. In these situations, definitive surgical management is deferred until the patient is stabilized.
In the future, statically locked intramedullary nailing may prove to be an option for the treatment of Galeazzi fractures, provided that it can neutralize and control the multiple deforming forces associated with these injuries. The indications for intramedullary nailing of forearm fractures have not been clearly defined.
Children
Children tend to have overall better long-term outcomes compared to adults. The approach is usually conservative with closed reduction and splinting 9. Above-elbow casting in supination is the preferred immobilization. Irreducible and unstable injuries, as well as variants of the Galeazzi fracture, may require surgical intervention with open reduction and internal fixation (ORIF).
Postoperative care
Postoperatively, elevate the upper extremity. Apply ice to the operative site as needed. Check neurologic and vascular status. Specifically, evaluate for function of the anterior interosseous nerve and for the presence of compartment syndrome. Immobilize the forearm in supination for 4 weeks, with removal of any percutaneous pins at 4 weeks 10. Immediately after surgery, institute occupational therapy for digital and shoulder range of motion.
Complications
The overall complication rate in the treatment of Galeazzi fractures approaches 40%. Complications include the following:
- Nonunion
- Malunion
- Infection
- Refracture following plate removal
- Radial sensory nerve and posterior interosseous nerve injury
- Instability of the distal radioulnar joint
Nonunion and malunion are primarily associated with closed reduction, plaster immobilization, intramedullary nailing, and inadequate plate fixation.
Radial nerve injury is reportedly the most common nerve injury to occur during either the volar or dorsal forearm approach to a Galeazzi fracture. The radial sensory nerve is reported to be the most frequently injured branch, with damage occurring in association with the Henry (volar) approach. The posterior interosseous nerve, another branch of the radial nerve, also is vulnerable (during the dorsal Thompson approach), especially when the posterior interosseous nerve has not been identified at the time of dissection.
Ulnar nerve injury, though rare, has been reported 11. The occurrence of tardy ulnar tunnel syndrome has been reported in the closed treatment of a Galeazzi fracture; this resulted from a malunion and the compression of a stretched vascular branch situated over the ulnar head 12.
Plate removal is not without risk and should be undertaken cautiously. A second approach to the forearm may put the posterior interosseous nerve at risk at a site that has already been surgically treated. Refracture of the radius is another possibility with plate removal. The patient should be advised of potential complications prior to pursuing hardware removal.
Instability of the distal radioulnar joint may occur for the following reasons:
- Failure to recognize the injury
- Failure to reduce the dislocation intraoperatively
- Nonanatomic radial reduction
- Interposed soft tissue that blocks reduction – Most often, the extensor carpi ulnaris is the interposed structure 13; other soft-tissue structures that have been implicated in the blockage of reduction include the extensor digitorum communis, the extensor digiti minimi, the flexor pollicis longus, and the median nerve
It is important to achieve an adequate assessment of the distal radioulnar joint preoperatively, intraoperatively, and postoperatively. Computed tomography (CT) may be necessary to confirm distal radioulnar joint reduction.
A case of late extensor pollicis longus tendon rupture after plate fixation of a Galeazzi fracture dislocation has been reported 14. Delayed complete rupture of the flexor digitorum superficialis and flexor digitorum profundus tendons in zone V 18 years after conservative treatment of Galeazzi fracture-dislocation with volar dislocation of the ulna from the distal radioulnar joint has been described 15.
Galeazzi fracture recovery
As with all fractures, length of recovery is dependent on multiple variables including the severity of the injury, individual’s ability to heal, and the intended use of the extremity. Rehabilitation usually begins six to eight weeks after surgical fixation. The goal of rehab is the return of full range of motion and fine motor skills with the absence of pain. Full return to activity depends upon the severity of the injury as well as the patient’s intended use of their upper extremities. Manual workers and athletes may require more prolonged rehabilitation. Typical return to full activity in patients with low physical demands can happen after 8 to 12 weeks. Patients with high demand activity (manual workers and athletes) may need up to 12 to 16 weeks of rehab. Surgical hardware is usually permanent, with less than 10% of patients needing hardware removal.
Galeazzi fracture prognosis
Successful treatment of Galeazzi fractures depends on the reduction of the radius and distal radioulnar joint and the restoration of the forearm axis. An unsatisfactory result—caused by a loss of reduction that, in turn, led to malunion—was identified in 92% of patients (35 of 38) treated with closed reduction and cast immobilization 16.
Hughston’s study attributed loss of reduction to the deforming force of the brachioradialis, the pull of the pronator quadratus (leading to rotation of the distal radial fragment towards the ulna), and the weight of the hand as a deforming force (leading to dorsal angulation of the radius and subluxation of the distal radioulnar joint) 16. These deforming forces cannot be controlled with plaster immobilization; operative management is required.
The incidence of nonunion of Galeazzi fractures is very low. The rate of union following the open reduction of forearm fractures has been reported to approach 98% 17.
Reckling and Moore separately reported satisfactory results with compression plating and immobilization in supination 18.
Eberl et al 8 retrospectively reported on Galeazzi lesions over a 3-year period in 26 patients. Casting after fracture reduction was possible in 22, of whom 13 were treated with immobilization in a below-elbow cast and nine were treated with an above-elbow cast. Four patients were treated operatively. Results were excellent in 23 cases and good in three. The authors noted that in all cases of distal forearm fractures, a possible Galeazzi lesion should be considered but that proper reduction of the radius with concomitant reduction of the distal radioulnar joint and cast immobilization provides good-to-excellent outcome even if the Galeazzi lesion is not recognized primarily 8.
Ploegmakers et al 19 retrospectively reviewed Galeazzi fractures to determine their effect on the strength of pronation and supination at a mean of 2 years after surgery. They found that the mean absolute loss of strength of supination in the injured arm compared with the noninjured arm throughout all ranges of forearm rotation was 16.1 kg, corresponding to a relative loss of 12.5%. For the strength of pronation, the mean loss was 19.1 kg, corresponding to a relative loss of 27.2% 19.
Loss of strength of supination following a Galeazzi fracture correlated with poor quick Disabilities of the Arm, Shoulder, and Hand and Patient-Rated Wrist Evaluation scores 19. Loss of strength of pronation (27.2%), and of supination (12.5%) in particular, after a Galeazzi fracture is associated with worse clinical scores, highlighting the importance of supination of the forearm in function of the upper limb.
Ilyas et al 20, in a study of 10 patients with AO type A and C distal radius fractures who underwent fracture fixation, found that intramedullary nailing for displaced distal radius fractures could result in good functional outcome but had a high incidence of complications. The authors did not identify any long-term soft tissue problems but noted that intramedullary nails should be limited to extra-articular and simple intra-articular distal radius fractures.
In this study 20, all cases maintained reduction between postoperative and final radiographs, except for two cases of AO type A3 fractures with a loss of volar tilt greater than 5º. Grip strength relative to the uninjured limb was 91%. According to the Disabilities of the Arm, Shoulder, and Hand questionnaire, eight results were excellent, one good, and one poor. There were two cases of transient superficial radial sensory neuritis and three cases of screw penetration into the distal radioulnar joint. There were no cases of infection, tendon injury, or hardware failure or removal.
References- Egol KA, Koval KJ, Zuckerman JD. Handbook of Fractures. (2010) ISBN:1605477605.
- Saffar P, Cooney WP. Fractures of the Distal Radius. Informa HealthCare. (1995) ISBN:1853171786.
- Benson M, Fixsen J, MacNicol M. Children’s Orthopaedics and Fractures. Springer Verlag. (2010) ISBN:1848826109.
- Suganuma S, Tada K, Yamamoto D, Tsuchiya H. Galeazzi-equivalent Fractures: Report of Two Cases and Literature Review. J Hand Surg Asian Pac Vol. 2017 Jun;22(2):232-235.
- Galanopoulos I, Fogg Q, Ashwood N, Fu K. A widely displaced Galeazzi-equivalent lesion with median nerve compromise. BMJ Case Rep. 2012 Aug 18. 2012
- Tsismenakis T, Tornetta P 3rd. Galeazzi fractures: Is DRUJ instability predicted by current guidelines?. Injury. 2016 Jul. 47 (7):1472-7.
- Lendemans S, Taeger G, Nast-Kolb D. [Dislocation fractures of the forearm. Galeazzi, Monteggia, and Essex-Lopresti injuries]. Unfallchirurg. 2008 Dec. 111 (12):1005-14; quiz 1015-6.
- Eberl R, Singer G, Schalamon J, Petnehazy T, Hoellwarth ME. Galeazzi lesions in children and adolescents: treatment and outcome. Clin Orthop Relat Res. 2008 Jul. 466 (7):1705-9.
- Johnson NP, Smolensky A. Galeazzi Fractures. [Updated 2019 Jul 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470188
- Park MJ, Pappas N, Steinberg DR, Bozentka DJ. Immobilization in supination versus neutral following surgical treatment of Galeazzi fracture-dislocations in adults: case series. J Hand Surg Am. 2012 Mar. 37 (3):528-31.
- Roettges P, Turker T. Ulnar Nerve Injury as a Result of Galeazzi Fracture: A Case Report and Literature Review. Hand (N Y). 2017 Sep. 12 (5):NP162-NP165.
- Saitoh S, Seki H, Murakami N, Hata Y, Takaoka K. Tardy ulnar tunnel syndrome caused by Galeazzi fracture-dislocation: a neuropathy with a new pathomechanism. J Orthop Trauma. 2000 Jan. 14 (1):66-70.
- Alexander AH, Lichtman DM. Irreducible distal radioulnar joint occurring in a Galeazzi fracture – case report. J Hand Surg Am. 1981 May. 6 (3):258-61.
- Sabat D, Dabas V, Dhal A. Late extensor pollicis longus rupture following plate fixation in Galeazzi fracture dislocation. Indian J Orthop. 2014 Jul. 48 (4):426-8.
- Nagy MT, Ghosh S, Shah B, Sankar T. Delayed rupture of flexor tendons in zone V complicated by neuritis 18 years following Galeazzi fracture-dislocation. BMJ Case Rep. 2014 Apr 16. 2014
- HUGHSTON JC. Fracture of the distal radial shaft; mistakes in management. J Bone Joint Surg Am. 1957 Apr. 39-A (2):249-64; passim.
- Wei SY, Born CT, Abene A, Ong A, Hayda R, DeLong WG Jr. Diaphyseal forearm fractures treated with and without bone graft. J Trauma. 1999 Jun. 46 (6):1045-8.
- Moore TM, Klein JP, Patzakis MJ, Harvey JP Jr. Results of compression-plating of closed Galeazzi fractures. J Bone Joint Surg Am. 1985 Sep. 67 (7):1015-21.
- Ploegmakers JJ, The B, Brutty M, Ackland TR, Wang AW. The effect of a Galeazzi fracture on the strength of pronation and supination two years after surgical treatment. Bone Joint J. 2013 Nov. 95-B (11):1508-13.
- Ilyas AM, Thoder JJ. Intramedullary fixation of displaced distal radius fractures: a preliminary report. J Hand Surg Am. 2008 Dec. 33 (10):1706-15.