Olecranon fracture
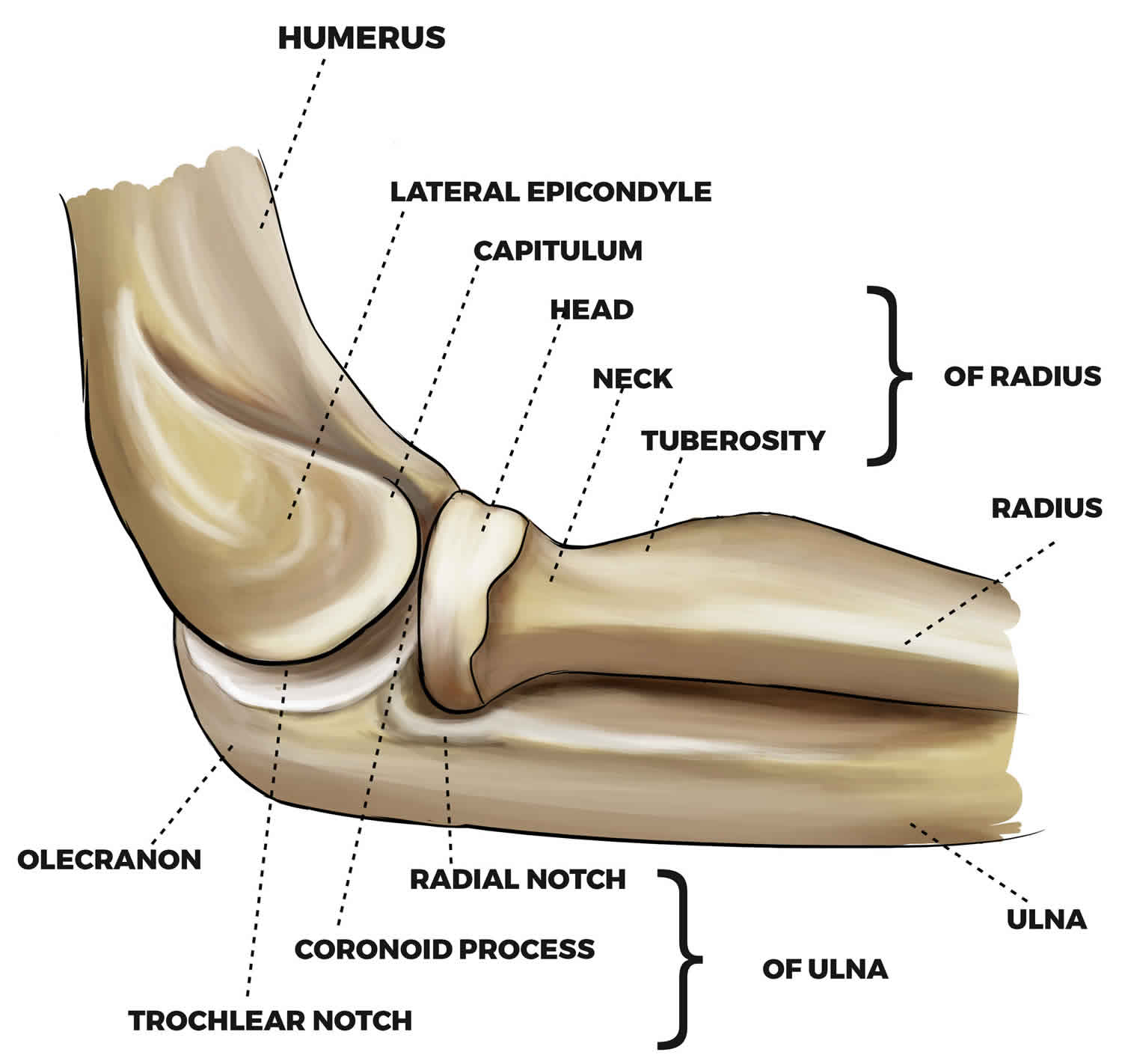
Olecranon fracture is a break in the bony “tip” of the elbow. This pointy segment of bone is part of the ulna, one of the three bones that come together to form the elbow joint. The olecranon is the part of the ulna that “cups” the lower end of the humerus, creating a hinge for elbow movement.
The olecranon is positioned directly under the skin of the elbow, without much protection from muscles or other soft tissues. It can break easily if you experience a direct blow to the elbow or fall on an outstretched arm. A fracture can be very painful and make elbow motion difficult or impossible.
Olecranon fractures are fairly common. Although they usually occur on their own, with no other injuries, they can also be part of a more complex elbow injury.
In an olecranon fracture, the bone can crack just slightly or break into many pieces. The broken pieces of bone may line up straight or may be far out of place (displaced fracture).
In some cases, the bone breaks in such a way that bone fragments stick out through the skin or a wound penetrates down to the bone. This is called an open fracture. Open fractures are particularly serious because, once the skin is broken, infection in both the wound and the bone are more likely to occur. Immediate treatment is required to prevent infection.
Olecranon fractures account for 5% of all fractures of the elbow region with the incidence of 12 per 10,000 person-years 1. The mean age of occurrence is 57, with males more likely to sustain an injury at a younger age. Olecranon fractures are often associated with other elbow injuries (e.g. radial head dislocation [Monteggia fracture], lateral condyle fracture, radial neck fracture or supracondylar fracture) 2. These usually occur as a result of direct trauma to the flexed elbow or indirect forces such as a fall on the outstretched hand, with a varus or valgus stress to the elbow joint. Close to 6.4% of injuries are open fractures 1.
Treatment for an olecranon fracture depends upon the severity of the injury. Some simple fractures can be treated by wearing a splint until the bone heals. In most olecranon fractures, however, the pieces of bone move out of place when the injury occurs. For these fractures, surgery is required to restore both the normal anatomy of the elbow and motion in the joint.
Figure 1. Elbow joint bones
Figure 2. Elbow joint
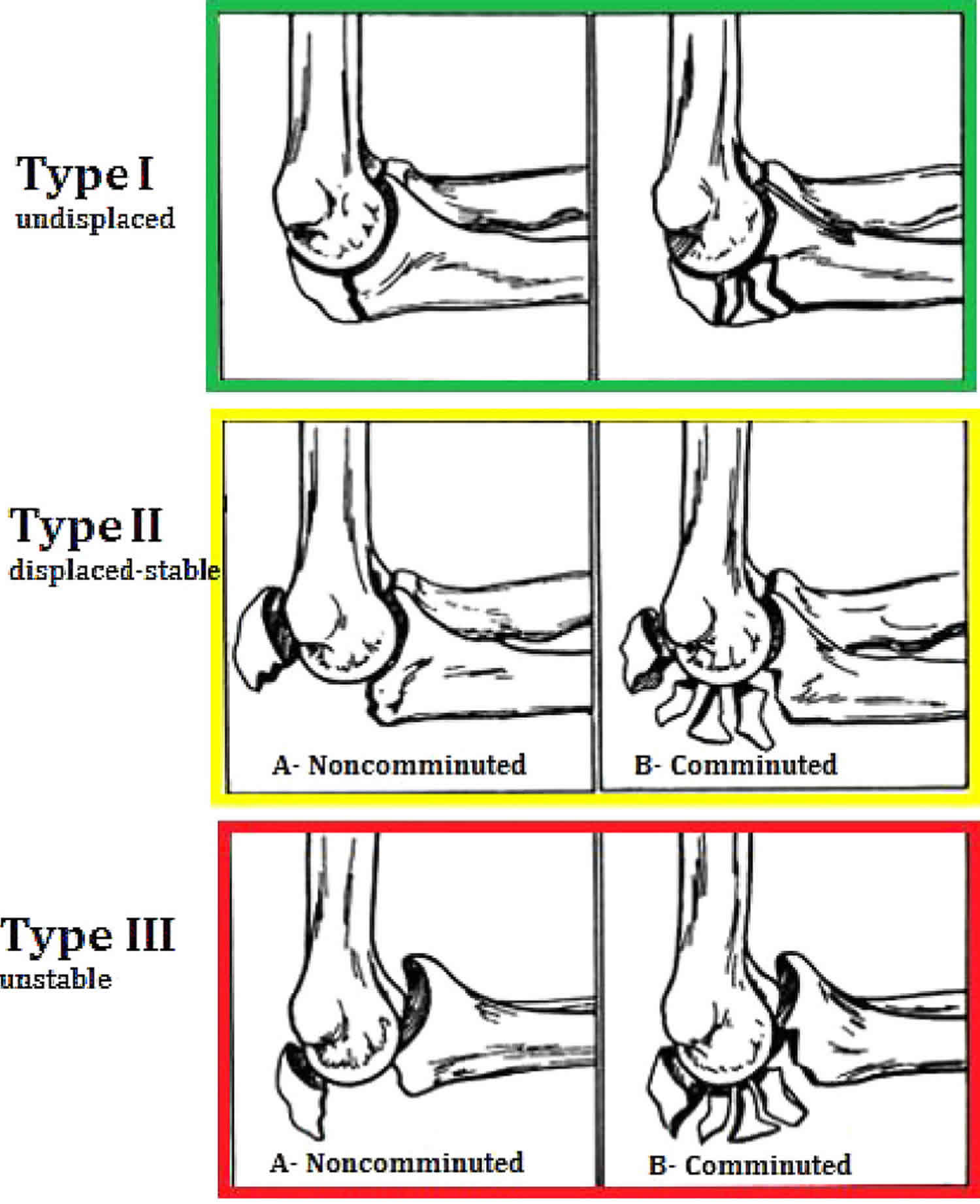
Olecranon fracture classification
There are several classifications systems of olecranon fractures. The most commonly used is the Mayo classification first described by Morrey in 1993. The goal of this system was to simplify the classification of olecranon fractures based on fracture comminution, displacement, and stability of the ulno-humeral joint. There are three types, each one further subdivided into type A and B, indicating non-comminuted and comminuted respectively 3.
- Type I fractures are undisplaced.
- Type II fractures are displaced at least 3mm, however, the ulnohumeral articulation is maintained indicating intact collateral ligaments.
- Type III injuries the fracture is displaced and the ulnohumeral joint is unstable. This injury is a fracture-dislocation, collateral ligaments may be incompetent causing instability 4.
The most common fracture pattern is Type II, which occurs in 80-85% of olecranon fractures. Type I injuries account for 5-12% of cases and approximately 6% are type III injuries 1.
Figure 3. Olecranon fracture classification (Mayo classification)
Type I injuries are undisplaced and can be treated with an initial period of immobilization in an above elbow back-slab and collar and cuff followed by early progressive active range of motion exercises with avoidance of active extension 5. If treated non-operatively, patients should be monitored with radiographs to ensure that the fracture does not displace.
Type II and III injuries generally require surgical intervention. Although there have been reports of non-operative management of type II injuries, this is not the norm 6. There is however, evidence which suggests that conservative management of displaced fractures in those over 70 years old can still lead to satisfactory function 7. They will lose full elbow extension due to disruption of the extensor mechanism but in some patients this is thought to be preferential to the risks of surgery.
Displaced, stable, non-comminuted fractures (Mayo type 2A) may be amenable to tension band wiring. This construct converts the tension force from the pull of the triceps into a compressive force at the articular surface. It requires an intact dorsal cortex. Fractures treated with tension band wiring should not have significant comminution, or they will cause collapse and narrowing of the distance between the coronoid and olecranon 3.
Plate and screw fixation is recommended for unstable fracture patterns with significant comminution or a fracture line exiting distal to the semilunar notch (Mayo Type 2B) and fracture-dislocations (Mayo Type 3) 8. An oblique fracture line may be amenable to a lag screw alongside the plate. Plate options include: one third tubular plates, hook plates, limited contact dynamic compression plates, and frequently fracture specific locked plates 5. Care should be taken to obtain an anatomic reduction. There is a bare area on the articular surface of the olecranon which lacks articular cartilage. This should be reduced to maintain joint congruity 9. The plate is typically placed on the dorsal aspect.
Intramedullary nails are now available and may be suitable for some fracture types. Intramedullary devices may avoid the wound complications related to the superficial location of traditional hardware used to treat olecranon fractures 8.
Although typically reserved as a salvage procedure, excision and triceps advancement is an option in elderly, low demand individuals where the fragment is too small for fixation or where less than 50% of the joint surface is involved. Cadaveric studies have shown that excising over 50% of the olecranon results in elbow instability, therefore this is the maximum recommended resection 10. It is vital to ensure that the collateral ligaments, distal radioulnar joint and intraosseous membrane are intact to prevent instability occurring. It involves removal of the fracture fragment and reattachment of the triceps muscle to the proximal ulna.
Olecranon fracture causes
Olecranon fractures are most often caused by:
- Falling directly on the elbow
- Receiving a direct blow to the elbow from something hard, like a baseball bat or a dashboard or car door during a vehicle collision.
- Falling on an outstretched arm with the elbow held tightly to brace against the fall. In this situation, the triceps muscle, which attaches to the olecranon, can pull a piece of the bone off of the ulna. Injuries to the ligaments around the elbow may occur with this type of injury, as well.
Most olecranon fractures occur in individuals aged 50 years or greater after a fall from standing height 8. Younger individuals are likely to have injuries related to a higher energy injury mechanism 5. Olecranon fractures can occur from forced elbow hyperextension or a direct blow to the elbow at 90 degrees of flexion. Avulsion injuries may also occur from eccentric contraction of the triceps tendon 11. These typically have a transverse or oblique fracture line and tend to be more common in osteoporotic patients.
Olecranon fracture symptoms
An olecranon fracture usually causes sudden, intense pain and can prevent you from moving your elbow. Other signs and symptoms of a fracture may include:
- Swelling over the “tip” or back of the elbow
- Bruising around the elbow. Sometimes, this bruising travels up the arm towards the shoulder or down the forearm towards the wrist.
- Tenderness to the touch
- Numbness in one or more fingers
- Pain with movement of the elbow or with rotation of the forearm
- A feeling of instability in the joint, as if your elbow is going to “pop out.”
Olecranon fracture diagnosis
Your doctor will talk with you about your medical history and general health and ask about your symptoms. He or she will then examine your elbow to determine the extent of the injury. During the exam, your doctor will:
- Check your skin for cuts and lacerations. In severe fractures, bone fragments can break through the skin, increasing the risk of infection.
- Palpate (feel) all around your elbow to determine if there are any other areas of tenderness. This could indicate other broken bones or injuries, such as a dislocated elbow.
- Check your pulse at the wrist to ensure that there is good blood flow to your hand and fingers.
- Check to see that you can move your fingers and wrist, and can feel things with your fingers.
Although you may have pain only at the elbow, your doctor may also examine your shoulder, upper arm, forearm, wrist, and hand to ensure that you do not have any other injuries.
X-rays
X-rays provide images of dense structures, such as bones. Your doctor will order x-rays of your elbow to help diagnosis your fracture. Depending on your symptoms, he or she may also order x-rays of your upper arm, forearm, shoulder, wrist, and/or hand to determine if you have other injuries.
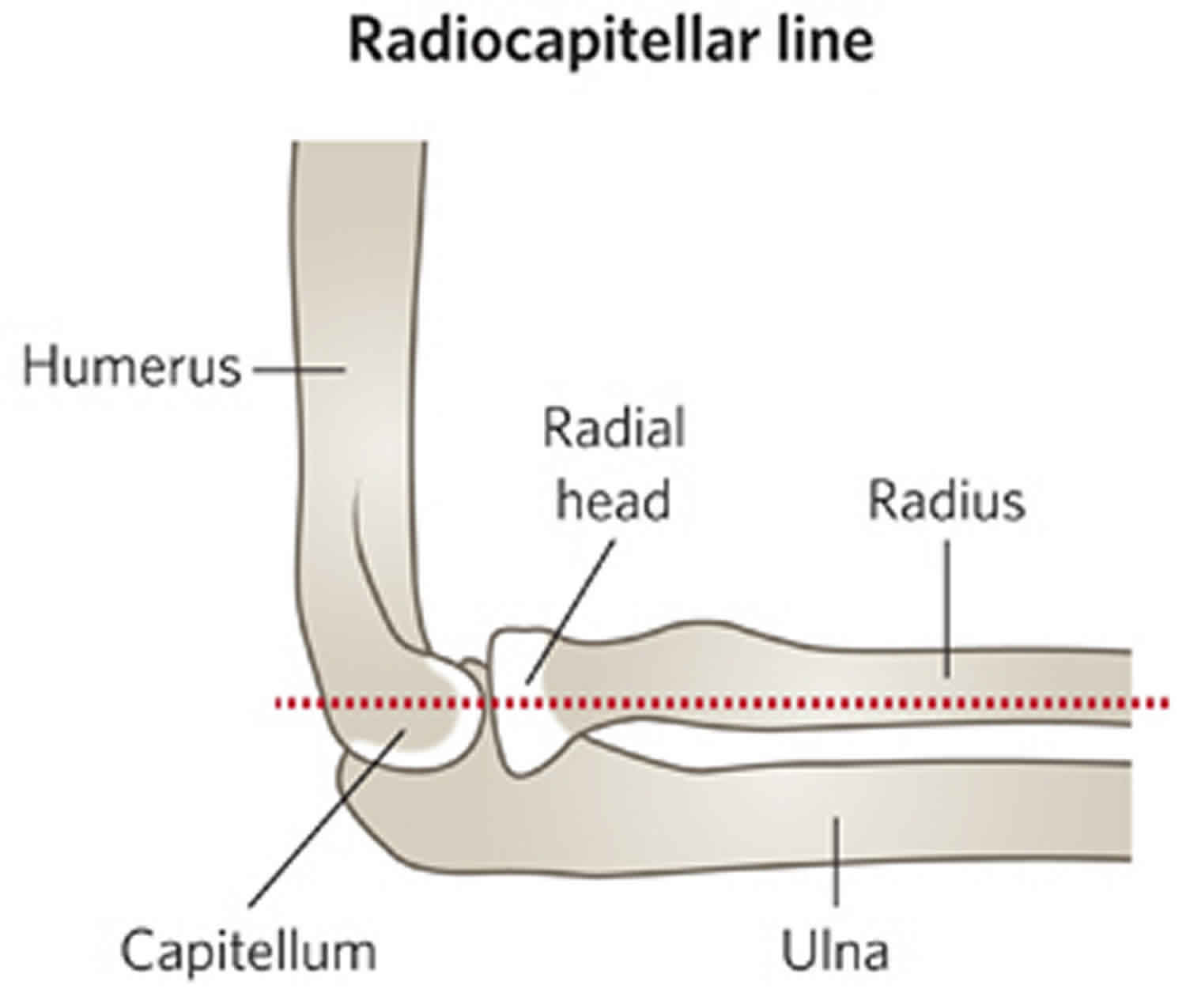
An anteroposterior (AP) and lateral view of the elbow should be obtained. It important that the lateral view is a true lateral and that the anteroposterior (AP) clearly shows the relationship of the proximal radius and ulna to the humerus.
X-rays of the entire forearm are indicated if a radial head dislocation (Monteggia fracture) is suspected on the initial elbow films.
TIP:A line drawn down the shaft of the radius should point to the center of the capitellum in both AP and lateral x-ray views to exclude radial head dislocation.
Figure 4. Olecranon fracture radiocapitellar line
Olecranon fracture treatment
While you are in the emergency room, your doctor will apply a splint (like a cast) to your elbow, and give you a sling to help keep the elbow in position. Immediate treatment may also include:
- Applying ice to reduce pain and swelling
- Medications to relieve pain
Whether or not your fracture requires surgery will be determined. Not all olecranon fractures will require surgery. Approximately 80% of olecranon fractures are undisplaced or minimally displaced and require immobilization only. All displaced fractures are unstable and will require reduction and fixation.
Nonsurgical treatment
If the pieces of bone are not out of place (displaced), a fracture can sometimes be treated with a splint to hold the elbow in place during healing. During the healing process, your doctor will take frequent x-rays to make sure the bone has not shifted out of place.
Splints are typically worn for 6 weeks before gentle motion is started. If the fracture shifts in position during this time, you may need surgery to put the bones back together.
Surgical treatment
Surgery is usually required for olecranon fractures in which:
- The bones have moved out of place (displaced fracture)
- Pieces of bone have punctured the skin (open fracture)
Surgery for olecranon fractures typically involves putting the broken pieces of bone back into position and preventing them from moving out of place until they are healed.
Because of the increased risk of infection, open fractures are scheduled for surgery as soon as possible, usually within hours. Patients are given antibiotics by vein (intravenous) in the emergency room, and may receive a tetanus shot. During surgery, the cuts from the injury and the surfaces of the broken bone are thoroughly cleaned out. The bone will typically be repaired during the same surgery.
Surgical procedures
Open reduction and internal fixation (ORIF)
This is the procedure most often used to treat olecranon fractures. During the procedure, the bone fragments are first repositioned (reduced) into their normal alignment. The pieces of bone are then held in place with screws, wires, pins, or metal plates attached to the outside of the bone.
Bone graft
If some of the bone has been lost through the wound or is crushed, the fracture may require bone graft to fill the gaps. Bone graft can be taken from a donor (allograft) or from another bone in your own body (autograft)—most often the hip. In some cases, an artificial material can be used.
Removal of the fracture fragment
If the broken bone fragment is too small to repair, it is sometimes removed. When this is done, the triceps tendon, which is attached to the fragment, is reattached to the remaining portion of the ulna.
Complications of surgery
There are risks associated with all surgery. If your doctor recommends surgery, he or she thinks that the possible benefits outweigh the risks.
Potential complications include:
- Infection. There is a risk of infection with any surgery. Your doctor will take specific measures to help prevent infection.
- Hardware irritation. A small percentage of patients may experience irritation from the metal implants used to repair the fracture.
- Damage to nerves and blood vessels. There is a minor risk of damage to nerves and blood vessels around the elbow. This is an unusual side effect.
- Nonunion. Sometimes, a fracture does not heal. The fracture may pull apart and the screws, plates, or wires may shift or break. This can occur for a number of reasons, including:
- The patient does not follow directions after surgery.
- The patient has a health problem, such as diabetes, that slows healing. Smoking or using other tobacco products also slows healing.
- If the fracture was associated with a cut in the skin (open fracture), healing is often slower.
- Infections can also slow or prevent healing.
If the fracture fails to heal, further surgery may be needed.
Olecranon fracture recovery
Most fractures hurt moderately for a few days to a couple of weeks. Many patients find that using ice, elevation (holding their arm up above their heart), and simple, non-prescription medications for pain relief are all that are needed to relieve pain.
If your pain is severe, your doctor may suggest a prescription-strength medication, such as an opioid, for a few days.
Be aware that although opioids help relieve pain after surgery, opioid dependency and overdose has become a critical public health issue. For this reason, opioids are typically prescribed for a short period of time. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids.
Rehabilitation
Whether your treatment is surgical or nonsurgical, full recovery from an olecranon fracture requires a good effort at rehabilitation.
Nonsurgical treatment
Because nonsurgical treatment can sometimes require long periods of splinting or casting, your elbow may become very stiff. For this reason, you may need a longer period of physical therapy to regain motion.
During rehabilitation, your doctor or a physical therapist will provide you with exercises to help:
- Improve range of motion
- Decrease stiffness
- Strengthen the muscles within the elbow
You will not be allowed to lift, push, or pull anything with your injured arm for a few weeks. Your doctor will talk with you about specific restrictions.
Surgical treatment
Depending on the complexity of the fracture and the stability of the repair, your elbow may be splinted or casted for a short period of time after surgery.
- Physical therapy. Patients will usually begin exercises to improve motion in the elbow and forearm shortly after surgery, sometimes as early as the next day. It is extremely important to perform the exercises as often as directed. The exercises will only make a difference if they are done regularly.
- Restrictions. You will not be allowed to lift heavy objects with your injured arm for at least 6 weeks. You will also be restricted from pushing and pulling activities, such as opening doors or pushing up while rising from a chair. You may be allowed to use your arm for bathing, dressing, and feeding activities. Your doctor will give you specific instructions. He or she will also let you know when it is safe to drive a car.
Olecranon fracture complications
Even with successful treatment, some patients with olecranon fractures may experience long-term complications.
Hardware irritation
Irritation leading to hardware removal is the most common complication due to the subcutaneous nature of the proximal olecranon. There is a variable rate of hardware removal for tension band wiring and plate fixation in the literature. A recent prospective randomized control study reported a hardware removal rate of 50% with tension band wiring and 22% with plate fixation 12. Intramedullary devices are less prominent and have a lower risk of a secondary operation for hardware irritation 8. Wire migration can occur in conjunction with wire breakage and fracture displacement.
Wound complications and infection
The subcutaneous nature of the olecranon provides little soft tissue coverage over hardware used for fixation. Placing plates on the side of the olecranon where there is a more robust soft tissue envelope may reduce the risk. Kirshner wires (k-wires) may back out and create wound problems or soft tissue irritation. Engaging the distal tip of the wire in the anterior cortex of the ulna 13 and turning the wires 180 degrees and burying them 14 can reduce the risk of the wires backing out. Injury to the anterior interosseus nerve and ulnar artery due to penetration of the k-wire through the anterior cortex can be mitigated by placing wires at an angle of 20-30 degrees from the longitudinal axis of the ulna on the lateral view 15. Pins that are too long can restrict supination by impinging on the radial neck, or damaging the biceps tendon or supinator muscle. One series reported a higher rate of infection in patients treated with plate fixation compared to tension band wiring (13% vs 0%) 12.
Loss of motion
In some cases, a patient may not be able to regain full motion in the affected elbow. In most of these cases, the patient cannot fully extend or straighten his or her arm. Patients commonly have loss of terminal elbow extension of 10-15 degrees. Fortunately, the loss of a few degrees of straightening does not usually affect the overall function of the arm. One study reported a 39% incidence of a flexion contracture >10 degrees after plate fixation which did not significantly impact functional outcome scores 16. General stiffness is thought to occur in up to 50% of patients but usually does not affect function. Patients who have significant loss of motion may require intensive physical therapy, special bracing, or further surgery. This is uncommon for olecranon fractures.
Posttraumatic arthritis
Posttraumatic arthritis is a type of arthritis that develops in a joint after an injury. Even when your bones heal normally, the cartilage lining the joint surfaces can be damaged, leading to pain and stiffness over time.
Posttraumatic arthritis is a relatively common complication of olecranon fractures. It can occur shortly after the fracture occurs or can take years to develop. Some patients with posttraumatic arthritis may need further surgery to relieve their symptoms. However, for many patients, there is little pain and no need for further treatment.
Heterotopic ossification
This can occur in approximately 13% of patients
Ulnar nerve neuritis
This is an infrequent complication which occurs in approximately 2-12% of cases 8. The majority of cases will resolve with conservative management. Recalcitrant cases may require neurolysis and ulnar nerve transposition.
Nonunion
The risk of nonunion is approximately 1% 8. Treatment options include: conservative measures, internal fixation with or without bone graft, excision and triceps advancement, and elbow arthroplasty 17.
Malunion
This may be intra-articular or extra-articular. Interarticular malunion may occur from an inadequate reduction of a comminuted fracture, leading narrowing of the sigmoid notch. Early arthritis will likely occur and may require an arthroplasty procedure. Extra-articular malunion presents with radial head subluxation and can be treated with an osteotomy 8.
Olecranon fracture prognosis
Most patients can return to their normal activities within about 4 months, although full healing can take more than a year. Recovering strength in your arm often takes longer than might be expected.
Although x-rays may show that the fracture has healed completely, some patients report that they still have limitations in movement. These patients will usually continue to improve over time. Approximately 10-15 degrees loss of terminal extension may occur, although this is usually not clinically significant 16. Long-term follow-up ranging 15-25 years reported good or excellent functional outcome in 96% of patients 18. Fractures have a high rate of healing with a nonunion rate of approximately 1% 19.
References- Duckworth AD, Clement ND, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of fractures of the proximal ulna. Injury. 2012 Mar;43(3):343-6.
- Sullivan CW, Hayat Z. Olecranon Fracture. [Updated 2019 Jan 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537295
- Morrey BF. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instr Course Lect. 1995;44:175-85.
- Morrey BF. Current concepts in the management of complex elbow trauma. Surgeon. 2009 Jun;7(3):151-61.
- Wiegand L, Bernstein J, Ahn J. Fractures in brief: Olecranon fractures. Clin. Orthop. Relat. Res. 2012 Dec;470(12):3637-41.
- Putnam MD, Christophersen CM, Adams JE. Pilot report: non-operative treatment of Mayo Type II olecranon fractures in any-age adult patient. Shoulder Elbow. 2017 Oct;9(4):285-291.
- Gallucci GL, Piuzzi NS, Slullitel PA, Boretto JG, Alfie VA, Donndorff A, De Carli P. Non-surgical functional treatment for displaced olecranon fractures in the elderly. Bone Joint J. 2014 Apr;96-B(4):530-4.
- Baecher N, Edwards S. Olecranon fractures. J Hand Surg Am. 2013 Mar;38(3):593-604.
- Newman SD, Mauffrey C, Krikler S. Olecranon fractures. Injury. 2009 Jun;40(6):575-81.
- An KN, Morrey BF, Chao EY. The effect of partial removal of proximal ulna on elbow constraint. Clin. Orthop. Relat. Res. 1986 Aug;(209):270-9.
- Hak DJ, Golladay GJ. Olecranon fractures: treatment options. J Am Acad Orthop Surg. 2000 Jul-Aug;8(4):266-75.
- Duckworth AD, Clement ND, White TO, Court-Brown CM, McQueen MM. Plate Versus Tension-Band Wire Fixation for Olecranon Fractures: A Prospective Randomized Trial. J Bone Joint Surg Am. 2017 Aug 02;99(15):1261-1273.
- Mullett JH, Shannon F, Noel J, Lawlor G, Lee TC, O’Rourke SK. K-wire position in tension band wiring of the olecranon – a comparison of two techniques. Injury. 2000 Jul;31(6):427-31.
- McKay PL, Katarincic JA. Fractures of the proximal ulna olecranon and coronoid fractures. Hand Clin. 2002 Feb;18(1):43-53.
- Catalano LW, Crivello K, Lafer MP, Chia B, Barron OA, Glickel SZ. Potential dangers of tension band wiring of olecranon fractures: an anatomic study. J Hand Surg Am. 2011 Oct;36(10):1659-62.
- De Giacomo AF, Tornetta P, Sinicrope BJ, Cronin PK, Althausen PL, Bray TJ, Kain MS, Marcantonio A, Sagi C, James CR. Outcomes after plating of olecranon fractures: A multicenter evaluation. Injury. 2016 Jul;47(7):1466-71.
- Rotini R, Antonioli D, Marinelli A, Katusić D. Surgical treatment of proximal ulna nonunion. Chir Organi Mov. 2008 Feb;91(2):65-70.
- Karlsson MK, Hasserius R, Karlsson C, Besjakov J, Josefsson PO. Fractures of the olecranon: a 15- to 25-year followup of 73 patients. Clin. Orthop. Relat. Res. 2002 Oct;(403):205-12.
- Papagelopoulos PJ, Morrey BF. Treatment of nonunion of olecranon fractures. J Bone Joint Surg Br. 1994 Jul;76(4):627-35.