Hand foot and mouth disease
Hand, foot and mouth disease (HFMD) also called enteroviral vesicular stomatitis, is a common viral illness that mainly affects children under 5 years old, but can sometimes affect older children and adults 1. Hand, foot and mouth disease is usually caused by infection with the Coxsackievirus A16 (CV-A16) and human Enterovirus A71 (EV-A71) in most cases, but the infection can also be caused by many other strains of Coxsackievirus and Enterovirus family 2, 3, 4, 5, 6.
Hand, foot and mouth disease is not serious, but it is highly contagious. Frequent hand-washing and avoiding close contact with people who are infected with hand-foot-and-mouth disease may help reduce your child’s risk of infection.
Hand, foot, and mouth disease (HFMD) is often confused with foot-and-mouth disease also called hoof-and-mouth disease, which affects farm animals such as cattle, pigs, sheep, and goats. Humans do not get the animal disease or the foot and mouth disease (hoof-and-mouth disease), and animals do not get the human disease or the hand, foot, and mouth disease (HFMD). In other words, you can’t contract the foot and mouth disease (hoof-and-mouth disease) from pets or other animals, and you can’t transmit the hand, foot, and mouth disease (HFMD) to them.
Hand, foot, and mouth disease is common in infants and children younger than 5 years old. Hand-foot-and-mouth disease is most common in children in childcare settings because of frequent diaper changes and toilet training, and because little children often put their hands in their mouths. It spreads quickly at schools, day care centers, summer camps or within the family. These outbreaks are usually during the summer and early autumn in the United States and other temperate climates 1. In tropical climates, outbreaks occur year-round. The majority of people infected with coxsackievirus are children under the age of 10. Because the virus is shed in the stools for many weeks after the signs and symptoms are gone, that means your child still can infect others. Some studies indicate that family members and close contacts are also at risk for developing hand, foot and mouth disease 1. Some people, especially adults, can pass the virus without showing any signs or symptoms of the hand, foot and mouth disease.
Hand-foot-and-mouth disease is transmitted by fecal-oral, oral-oral, and respiratory droplet contact. You can get hand, foot, and mouth disease by 7:
- Contact with respiratory droplets containing virus particles after a sick person coughs or sneezes
- Touching an infected person or making other close contact, like kissing, hugging, or sharing cups or eating utensils
- Touching an infected person’s feces, such as changing diapers, then touching your eyes, nose, or mouth
- Touching objects and surfaces that have the virus on them, like doorknobs or toys, then touching your eyes, nose, or mouth
Oral ingestion is the main source of coxsackievirus infection and hand-foot-and-mouth disease. Rarely, you can also get the viruses by swallowing recreational water, such as water in swimming pools. This can happen if the water is not properly treated with chlorine and becomes contaminated with feces from a person who has hand, foot, and mouth disease 7.
Hand, foot and mouth disease main symptoms are fever and tiny blisters on the cheeks, gums and sides of the mouth and on the hands and feet. The blisters can also occur in the groin and elsewhere. Children may also have a sore throat. Children should stay home while they have symptoms of hand, foot, and mouth disease.
There is no specific treatment for hand, foot and mouth disease. But it’s possible to improve comfort by treating the symptoms with acetaminophen (paracetamol), rest and plenty to drink. Making sure your child remains well hydrated is important. Additionally, a mixture of liquid ibuprofen and liquid diphenhydramine can be used to gargle with which helps coat the mouth ulcers, reducing the pain 8.
Most children have mild symptoms for 7 to 10 days. The blisters usually last for 7 to 10 days.
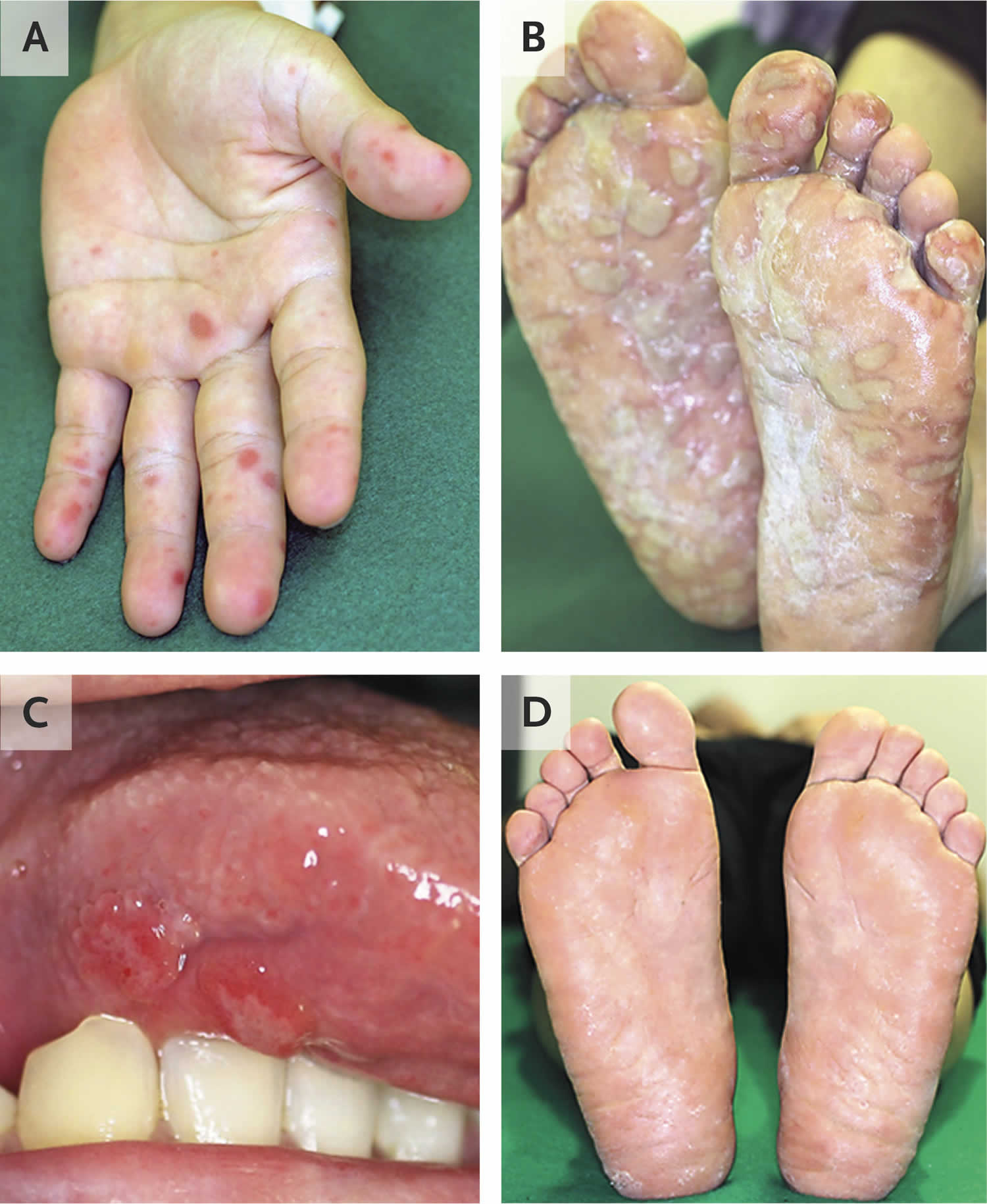
Figure 1. Hand foot and mouth disease rash
Figure 2. Hand foot and mouth disease rash
Footnote: Blisters on his palms (Panel A) and soles (Panel B) and ulcerations on the tongue (Panel C). Fluid from a blister on the patient’s right sole was tested by reverse-transcriptase–polymerase-chain-reaction (rt-PCR) assay, and an enterovirus species was identified; serologic testing for antibodies to coxsackievirus confirmed infection with coxsackievirus A16.
[Source 9 ]Figure 3. Hand foot and mouth disease rash
Hand-foot-and-mouth disease is usually a minor illness causing only a few days of fever and relatively mild signs and symptoms. See your doctor if mouth sores or a sore throat keep your child from drinking fluids. And see your doctor if after a few days, your child’s signs and symptoms worsen.
See a doctor if:
- Your child is not drinking enough to stay hydrated
- Your child’s fever lasts longer than 3 days
- Your child has a weakened immune system (body’s ability to fight germs and sickness)
- Symptoms are severe
- Symptoms do not improve after 10 days
- Your child is very young, especially younger than 6 months
Young children are at higher risk of serious infection than older children, teenagers and adults. Signs that a person might have a more serious form of hand, foot and mouth disease include any of the following:
- persistent fever (100.4 °F [38°C] or above for 72 hours or more)
- abnormal movements / jerking movements
- rapid breathing
- excessive tiredness, drowsiness
- excessive irritability
- difficulty walking
- showing signs of being dehydrated (such as not passing urine as often as usual)
- symptoms that are getting worse after a few days
- moving jerkily or can’t walk properly
If any of these signs are present, see your doctor urgently.
Is hand foot and mouth disease contagious?
Yes. Hand, foot and mouth disease is very contagious. People with hand, foot, and mouth disease are usually most contagious during the first week that they are sick. People can sometimes spread the virus to others for days or weeks after symptoms go away or if they have no symptoms at all.
Hand, foot, and mouth disease spreads easily through:
- Person-to-person contact
- Respiratory droplets containing virus particles when an infected person coughs or sneezes
- Contact with contaminated surfaces and objects
What is the incubation period for hand foot and mouth disease?
The usual incubation period (period from initial infection to the onset of signs and symptoms) is three to six days. A fever is often the first sign of hand-foot-and-mouth disease, followed by a sore throat and sometimes a poor appetite and feeling unwell. One or two days after the fever begins, painful sores may develop in the front of the mouth or throat. A rash on the hands and feet and possibly on the buttocks can follow within one or two days. Signs and symptoms of hand-foot-and-mouth disease usually clear up in seven to 10 days.
Does a child with hand foot and mouth disease have to stay off school?
As in the vast majority of cases, hand foot and mouth disease is a mild illness, there is no need to keep children from school once they are well enough to attend. In the United States, exclusion from childcare does not reduce the spread of the hand foot and mouth disease and is not recommended unless the child is unable to participate or staff are unable to care for the child without compromising the care of other children 10.
The blisters remain infective until they have dried up, which is usually within a few days. The stools are infective for up to a month after the illness. Thorough hand-washing will reduce the spread of the disease.
Hand foot and mouth disease in adults
Hand, foot, and mouth disease is a common mild and short-lasting viral infection most often affecting young children under the age of 10, and most are under 5 years of age (95%). Hand, foot, and mouth disease is characterized by blisters on the hands, feet and in the mouth. The infection may rarely affect adults. Hand, foot and mouth disease is usually caused by infection with the Coxsackievirus A16 (CV-A16) and human Enterovirus A71 (EV-A71).
Common causes of hand, foot, and mouth disease in the United States are 7:
- Coxsackievirus A16 (CV-A16) is typically the most common cause of hand, foot, and mouth disease in the United States. Other coxsackieviruses can also cause the illness.
- Coxsackievirus A6 (CV-A6) can also cause hand, foot and mouth disease and the symptoms may be more severe.
- Enterovirus 71 (EV-A71) has been associated with cases and outbreaks in East and Southeast Asia. Although rare, EV-A71 has been associated with more severe neurological complications and fatal outcomes such as encephalitis (swelling of the brain) 11.
A person infected with one of these viruses is contagious, which means that they can pass the virus to other people. The virus can spread to others through an infected person’s:
- Nose and throat secretions, such as saliva, drool, or nasal mucus
- Fluid from blisters or scabs
- Feces (poop)
People with hand, foot, and mouth disease are usually most contagious during the first week that they are sick. People can sometimes spread the virus to others for days or weeks after symptoms go away or if they have no symptoms at all.
You can get hand, foot, and mouth disease by:
- Contact with respiratory droplets containing virus particles after a sick person coughs or sneezes
- Touching an infected person or making other close contact, like kissing, hugging, or sharing cups or eating utensils
- Touching an infected person’s feces, such as changing diapers, then touching your eyes, nose, or mouth
- Touching objects and surfaces that have the virus on them, like doorknobs or toys, then touching your eyes, nose, or mouth
Oral ingestion is the main source of coxsackievirus infection and hand-foot-and-mouth disease. Rarely, you can also get the viruses by swallowing recreational water, such as water in swimming pools. This can happen if the water is not properly treated with chlorine and becomes contaminated with feces from a person who has hand, foot, and mouth disease.
Hand foot and mouth disease and pregnancy
Many adults, including pregnant women, are often exposed to hand, foot and mouth disease without symptoms. Pregnant women should contact their healthcare provider if they think they may have been exposed to hand, foot, and mouth disease or think they may have the disease. There is no clear evidence of risk to unborn babies from hand, foot and mouth disease. However, infected mothers (and siblings) can pass the infection onto newborn babies who rarely can have severe disease. In a study of neonatal hand, foot, and mouth disease due to coxsackievirus A6 (CV-A6) in Shanghai, China, where 16 neonates among the 12,608 diagnosed patients with hand, foot and mouth disease, the coxsackievirus A6 (CV-A6) infection in newborn babies was benign 12. None of the newborn babies with hand, foot and mouth disease experienced fever, onychomadesis (complete shedding of the nail plate from the nail bed due to severe toxicity to the nail matrix), or severe complications. The clinical symptoms receded about 1 week after onset. None of the neonates had complications 12. Some studies indicate that coxsackievirus infections may also be associated with spontaneous abortions or fetal growth retardation 13.
Breastfeeding does not impact the incidence of hand-foot-and-mouth disease. Mothers do not need to stop breastfeeding to prevent transmission of hand-foot-and-mouth disease 14.
How is hand foot and mouth disease transmitted?
Hand, foot, and mouth disease is caused by viruses. A person infected with one of these viruses is contagious, which means that they can pass the virus to other people.
Hand foot and mouth is passed on by direct contact with the skin, nasal and oral secretions of infected individuals, or by fecal contamination.
The virus can spread to others through an infected person’s:
- Nose and throat secretions, such as saliva, drool, or nasal mucus
- Fluid from blisters or scabs
- Feces (poop)
People with hand, foot, and mouth disease are usually most contagious during the first week that they are sick. People can sometimes spread the virus to others for days or weeks after symptoms go away or if they have no symptoms at all.
You can get hand, foot, and mouth disease by:
- Contact with respiratory droplets containing virus particles after a sick person coughs or sneezes
- Touching an infected person or making other close contact, like kissing, hugging, or sharing cups or eating utensils
- Touching an infected person’s feces, such as changing diapers, then touching your eyes, nose, or mouth
- Touching objects and surfaces that have the virus on them, like doorknobs or toys, then touching your eyes, nose, or mouth
Oral ingestion is the main source of coxsackievirus infection and hand-foot-and-mouth disease. Rarely, you can also get the viruses by swallowing recreational water, such as water in swimming pools. This can happen if the water is not properly treated with chlorine and becomes contaminated with feces from a person who has hand, foot, and mouth disease.
Hand foot and mouth disease causes
Hand, foot and mouth disease is usually caused by infection with the Coxsackievirus A16 (CV-A16) and human Enterovirus A71 (EV-A71) 15, 16, 17. The coxsackievirus belongs to a group of viruses called nonpolio enteroviruses. Human Enterovirus A71 (EV-A71) is a small, non-enveloped, icosahedral virus that belongs to the human enterovirus species A in the genus Enterovirus within the family Picornaviridae 4, 16. Several other enterovirus serotypes usually detected in sporadic cases or outbreaks of hand foot and mouth disease frequently co-circulate with human Enterovirus A71 (EV-A71) and Coxsackievirus A16 (CV-A16) in large epidemics. These enteroviruses include coxsackieviruses A2 (CV-A2), CV-A3, CV-A4, CV-A5, CV-A6, CV-A8, CV-A9, CV-A10, CV-A12, CV-A14, coxsackieviruses B CV-B1 to CV-B6 and echoviruses E-4, E-5, E-6, E-7, E-9, E-11, E-18, E-25, E-30 11
Common causes of hand, foot, and mouth disease in the United States are 7:
- Coxsackievirus A16 (CV-A16) is typically the most common cause of hand, foot, and mouth disease in the United States. Other coxsackieviruses can also cause the illness.
- Coxsackievirus A6 (CV-A6) can also cause hand, foot and mouth disease and the symptoms may be more severe.
- Enterovirus 71 (EV-A71) has been associated with cases and outbreaks in East and Southeast Asia. Although rare, EV-A71 has been associated with more severe neurological complications and fatal outcomes such as 11, 18:
- A poliolike syndrome
- Aseptic (viral) meningitis
- Encephalitis
- Encephalomyelitis
- Acute cerebellar ataxia
- Acute transverse myelitis
- Guillain-Barré syndrome
- Opsomyoclonus syndrome
- Benign intracranial hypertension
Hand, foot and mouth disease caused by Enterovirus 71 (EV-A71) has a higher incidence of neurologic involvement, including a poliolike syndrome, aseptic meningitis, encephalitis, encephalomyelitis, acute cerebellar ataxia, acute transverse myelitis, Guillain-Barré syndrome, opsomyoclonus syndrome, and benign intracranial hypertension. These neurological complications have been attributed to either immunopathology or virus-induced damage to gray matter 19.
Rarely, cardiopulmonary complications such as myocarditis, interstitial pneumonitis, and pulmonary edema may occur. Neurologic involvement with complications is less likely to occur in patients with hand, foot and mouth disease caused by coxsackievirus strains than with hand, foot and mouth disease caused by Enterovirus 71 (EV-A71). Chang et al 20 analyzed the Taiwan hand, foot and mouth disease epidemic of 1998 and revealed that 68% of the EV-71 cases were uncomplicated. Thirty-two percent of the cases had complications; 7.3% involved aseptic meningitis, 10% involved encephalitis, 2.3% involved poliolike syndrome, 4.5% involved encephalomyelitis, and 6.8% involved fatal pulmonary edema (7.9% of patients died and 4% of patients had complications). In the coxsackievirus A16 group, 94% of the cases of were uncomplicated; only 6.3% cases were complicated by aseptic meningitis; no fatalities or complications were reported.
Chong et al 18 observed vomiting, leukocytosis, and an absence of mouth ulcers as predictive risk factors for fatal cases of EV-71 hand, foot and mouth disease during the Singapore epidemic in 2000.
A person infected with one of these viruses is contagious, which means that they can pass the virus to other people. The virus can spread to others through an infected person’s:
- Nose and throat secretions, such as saliva, drool, or nasal mucus
- Fluid from blisters or scabs
- Feces (poop)
People with hand, foot, and mouth disease are usually most contagious during the first week that they are sick. People can sometimes spread the virus to others for days or weeks after symptoms go away or if they have no symptoms at all.
You can get hand, foot, and mouth disease by:
- Contact with respiratory droplets containing virus particles after a sick person coughs or sneezes
- Touching an infected person or making other close contact, like kissing, hugging, or sharing cups or eating utensils
- Touching an infected person’s feces, such as changing diapers, then touching your eyes, nose, or mouth
- Touching objects and surfaces that have the virus on them, like doorknobs or toys, then touching your eyes, nose, or mouth
Oral ingestion is the main source of coxsackievirus infection and hand-foot-and-mouth disease. Rarely, you can also get the viruses by swallowing recreational water, such as water in swimming pools. This can happen if the water is not properly treated with chlorine and becomes contaminated with feces from a person who has hand, foot, and mouth disease.
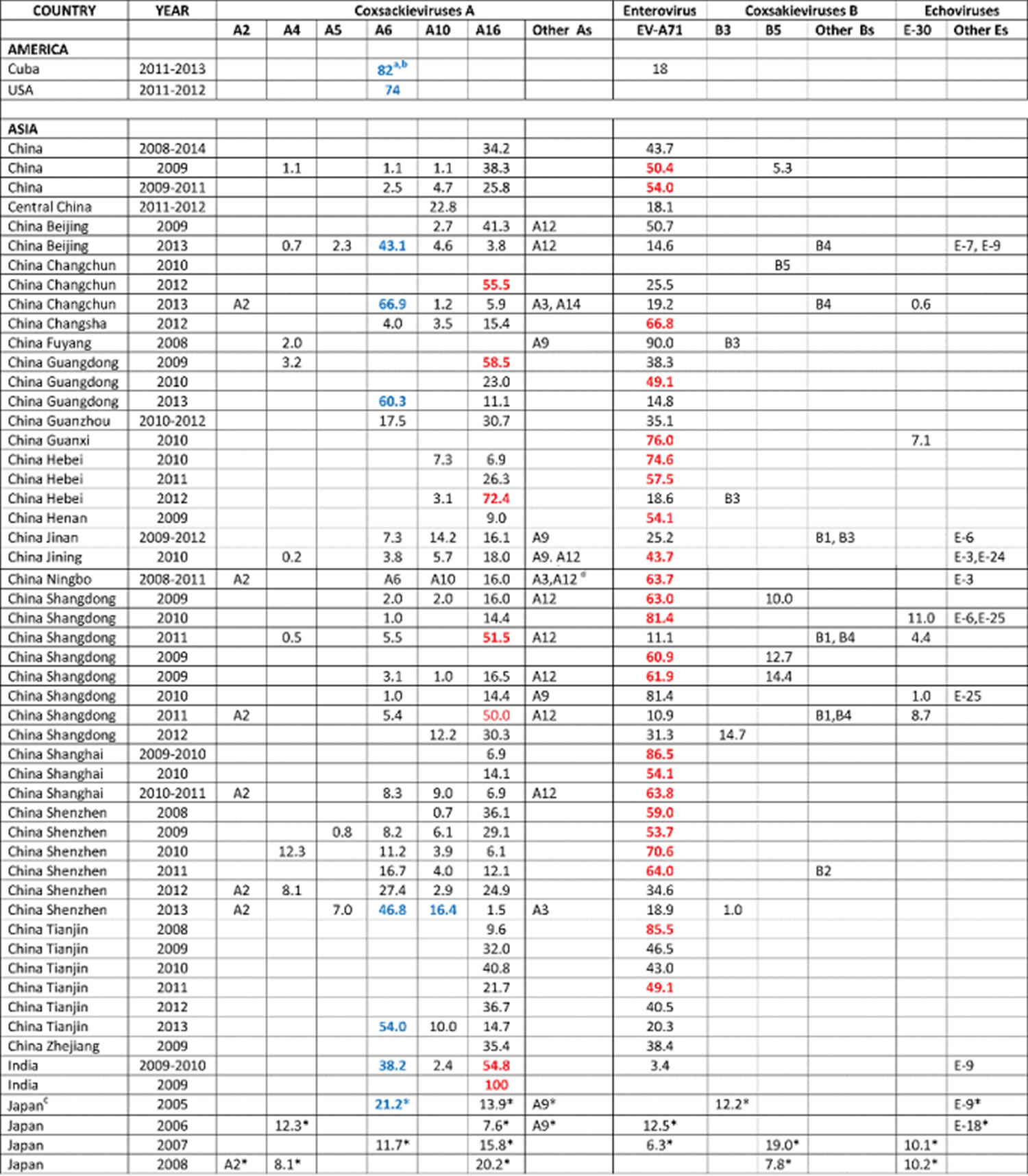
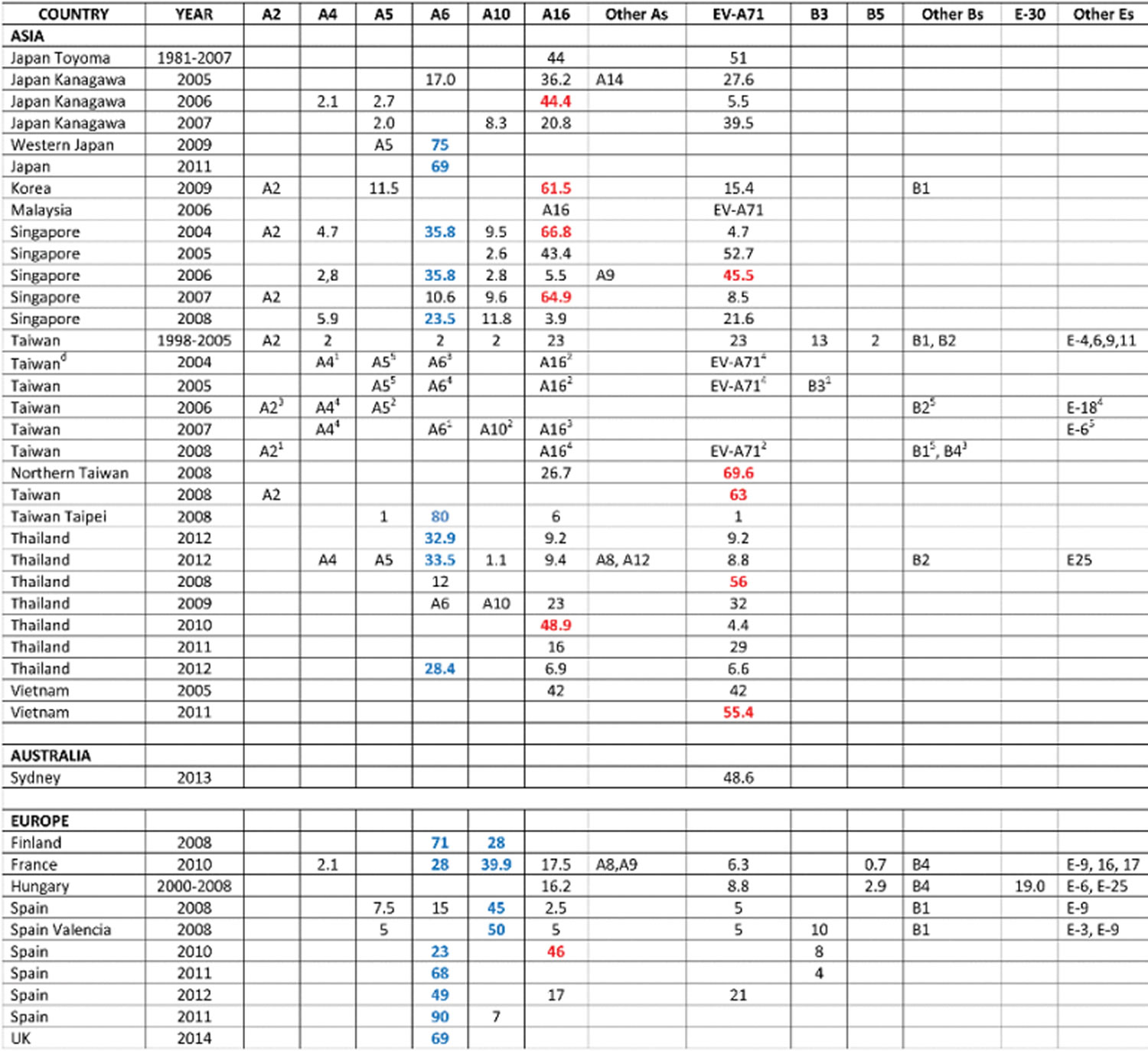
Table 1. Epidemiology of hand, foot and mouth disease from 2004 to 2014
Footnotes:
a Percentage of a serotype detected during an hand, foot and mouth disease outbreak whenever available in the literature. In the absence of such an information, the presence of a serotype during an outbreak is indicated by its symbol (Coxsackievirus A, A; coxsackievirus B, B; Echovirus E, E). Percentages have only been listed for serotypes that were pre-selected on the basis of their frequency during hand, foot and mouth disease outbreaks and their intrinsic pathogenicity.
b Percentages highlighted in bold characters correspond to the predominant strain(s) associated with disease during an epidemic. Percentages highlighted in red clearly indicate that the predominance of EV-A71 and CV-A16 during hand, foot and mouth disease epidemics alternates.
c The asterisks correspond to the top 5 strains which circulated during hand, foot and mouth disease epidemics in Japan from 2005 to 2008.
d The top 5 serotypes that circulated during hand, foot and mouth disease epidemics from 2004 to 2008 in Taiwan are indicated by their symbol with a number corresponding to their ranking in terms of respective percentages.
Risk factors for hand, foot and mouth disease
Hand, foot and mouth disease (HFMD) primarily affects children younger than age 10, often those under 5 years. Children in child care centers are especially susceptible to outbreaks of hand-foot-and-mouth disease because the infection spreads by person-to-person contact, and young children are the most susceptible.
Children usually develop immunity to hand-foot-and-mouth disease as they get older by building antibodies after exposure to the virus that causes the disease. However, it’s possible for adolescents and adults to get the disease.
Hand foot and mouth disease prevention
There is no vaccine in the United States to protect against the viruses that cause hand, foot, and mouth disease. You can help prevent catching or spreading the hand, foot, and mouth disease by following simple steps.
Wash your hands
Wash your hands often with soap and water for at least 20 seconds. If soap and water are not available, use an alcohol-based hand sanitizer.
Always wash your hands:
- After changing diapers
- After using the toilet
- After blowing your nose, coughing, or sneezing
- Before and after caring for someone who is sick
Help children wash their hands. Teach them how to wash their hands and make sure they wash them often.
Avoid touching your eyes, nose, and mouth
- You can get infected with hand, foot, and mouth disease if you have the virus on your hands and then touch your eyes, nose, or mouth. To lessen your chance of getting sick, don’t touch your eyes, nose, and mouth with unwashed hands.
Avoid close contact with sick people
- Avoid touching someone who has hand, foot, and mouth disease, such as hugging or kissing them.
- Stay home if you are sick with hand, foot, and mouth disease. Talk with your healthcare provider if you are not sure when you should return to work or when your child should return to school or daycare.
Isolate contagious people
- Because hand-foot-and-mouth disease is highly contagious, people with the hand, foot, and mouth disease should limit their exposure to others while they have active signs and symptoms. Keep children with hand-foot-and-mouth disease out of child care or school until fever is gone and mouth sores have healed. If you have the illness, stay home from work.
Clean and disinfect
- Clean and disinfect frequently touched surfaces and shared items, including toys and doorknobs.
- Child care centers should follow a strict schedule of cleaning and disinfecting all common areas, including shared items such as toys, as the virus can live on these objects for days.
- Clean your baby’s pacifiers often.
Hand foot and mouth disease signs and symptoms
Symptoms of hand, foot, and mouth disease usually include fever, mouth sores, and skin rash commonly found on the hands, mouth, and/or feet.
- The progression is from flat pink patches to small, elongated greyish blisters, and, within a week, these peel off leaving no scars.
- Small vesicles and ulcers in and around the mouth, palate, and pharynx. These are sometimes painful, so the child eats little, frets, and may complain of a sore throat or mouth sores.
- Red macules and papules on the buttocks and sometimes on the arms. Lesions can also occur on the genitalia.
Hand-foot-and-mouth disease may cause all of the following signs and symptoms or just some of them. They include:
- Fever
- Sore throat
- Feeling unwell
- Painful, red, blister-like lesions on the tongue, gums and inside of the cheeks
- A red rash, without itching but sometimes with blistering, on the palms, soles and sometimes the buttocks
- Irritability in infants and toddlers
- Loss of appetite
Atypical hand foot and mouth disease results in a more widespread rash. Features may include:
- Red, crusted papules
- No blisters or very large ones
- Targetoid lesions
- Involvement of unusual sites such as the ear
- In children with atopic dermatitis, lesions may select skin affected by eczema (eczema coxsackium).
Flat pink patches on the dorsal and palmar surfaces of the hands and feet are soon followed by small elongated greyish blisters. These resolve by peeling off within a week, without leaving scars.
Usually, there are also a few small oral vesicles and ulcers. These are sometimes painful, so the child eats little and frets. There may be a few on the skin around the mouth. In young children, a red rash may develop on the buttocks and sometimes on the arms.
Atypical hand foot and mouth disease due to Coxsackie A6 results in a more widespread rash, larger blisters and subsequent skin peeling and/or nail shedding.
The usual period from initial infection to the onset of signs and symptoms (incubation period) is three to six days. A fever is often the first sign of hand-foot-and-mouth disease, followed by a sore throat and sometimes a poor appetite and feeling unwell.
One or two days after the fever begins, painful sores may develop in the front of the mouth or throat. A rash on the hands and feet and possibly on the buttocks can follow within one or two days.
Sores that develop in the back of the mouth and throat may suggest that your child is infected with a related viral illness called herpangina. Herpangina is characterized by fever and painful vesiculo-ulcerative oral lesions and in some instances, seizure, without an accompanying skin rash 21. Sores that develop on the hands, feet or other parts of the body are very rare.
Hand foot and mouth disease complications
Hand, foot, and mouth disease is usually not serious. Nearly all people get better in 7 to 10 days with no or minimal medical treatment.
Complications from hand, foot, and mouth disease are rare. The most common complication of hand-foot-and-mouth disease is dehydration. The illness can cause sores in the mouth and throat, making swallowing painful and difficult.
Some people, especially young children, may get dehydrated if they are not able to swallow enough liquids because of painful mouth sores. Watch closely to make sure your child frequently sips fluid during the course of the illness. If dehydration is severe, intravenous (IV) fluids may be necessary.
Hand-foot-and-mouth disease is usually a minor illness causing only a few days of fever and relatively mild signs and symptoms. A rare and sometimes serious form of the coxsackievirus can involve the brain and cause other complications:
- Viral (aseptic) meningitis. This is a rare infection and inflammation of the membranes (meninges) and cerebrospinal fluid surrounding the brain and spinal cord. It causes fever, headache, stiff neck, or back pain and may require the infected person to be hospitalized for a few days.
- Encephalitis. This severe and potentially life-threatening disease involves brain inflammation caused by a virus. Encephalitis is extremely rare.
Very rarely, people may lose a fingernail or toenail after having hand, foot, and mouth disease. Most reports of fingernail and toenail loss have been in children. In these reported cases, the person usually lost the nail within a few weeks after being sick. The nail usually grew back on its own. However, there is no evidence that hand, foot, and mouth disease was the cause of the nail loss.
Serious enteroviral infection can lead to:
- Widespread vesicular rash
- Enteritis (gut infection)
- Myocarditis (heart muscle infection)
- Meningoencephalitis (brain infection)
- Acute flaccid paralysis (spinal cord infection)
- Pulmonary edema and pneumonia (lung infection)
- In pregnancy, first-trimester spontaneous abortion or fetal growth retardation.
Neurological involvement associated with Enterovirus A71 (EV-A71) infection may include:
- Aseptic meningitis
- Encephalitis
- Encephalomyelitis
- Acute cerebellar ataxia
- Acute transverse myelitis
- Guillain-Barré syndrome
- Opsomyoclonus syndrome. Symptoms include rapid, multi-directional eye movements (opsoclonus), quick, involuntary muscle jerks (myoclonus), uncoordinated movement (ataxia), irritability, and sleep disturbance.
- Benign intracranial hypertension
Fourteen children with culture-proven, Enterovirus A71 (EV-A71) induced neurological disease were identified in Australia 22. Nine patients (64%) developed severe neurological disease; 4 of these patients developed long-term neurological complications. Neurological syndromes included aseptic meningitis, Guillain-Barré syndrome, acute transverse myelitis, acute cerebellar ataxia, opso-myoclonus syndrome, benign intracranial hypertension, and a febrile convulsion. Clinical and magnetic resonance imaging data indicated that immunopathology was a major factor in the pathogenesis of neurological disease in this outbreak 22. This finding is in contrast to reports of previous EV71 epidemics, in which virus-induced damage to gray matter was the most frequent cause of neurological disease.
Hand foot and mouth disease diagnosis
Your doctor will likely be able to distinguish hand, foot, and mouth disease from other types of viral infections by evaluating:
- The age of the affected person
- The pattern of signs and symptoms
- The appearance of the rash or mouth sores
Your doctor may take a throat or blister swab or stool specimen and send it to the laboratory to determine which virus caused the illness.
While serology is not sensitive to make a diagnosis of hand, foot, and mouth disease, levels of immunoglobulin G (IgG) can be used to monitor recovery. In some centers, serology is used to differentiate Enterovirus A71 (EV-A71) from Coxsackievirus as this has prognostic significance. Today, polymerase chain reaction (PCR) assays are available in most centers to confirm the diagnosis of Coxsackievirus 1.
Hand foot and mouth disease treatment
There is no specific treatment for hand-foot-and-mouth disease. Signs and symptoms of hand-foot-and-mouth disease usually clear up in 7 to 10 days.
- The blisters should not be ruptured, to reduce contagion.
- Keep the blisters clean and apply non-adherent dressings to erosions.
A topical oral anesthetic may help relieve the pain of mouth sores. Over-the-counter pain medications other than aspirin, such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin, others) may help relieve general discomfort. Never give aspirin to children. Aspirin has been linked to Reye’s syndrome, a rare but serious condition that can be deadly without early treatment.
Drink enough liquids. Mouth sores can make it painful to swallow, so your child may not want to drink much. Make sure they drink enough to stay hydrated.
Additionally, a mixture of liquid ibuprofen and liquid diphenhydramine can be used to gargle with which helps coat the mouth ulcers, reducing the pain 8.
Over the past decade, researchers have developed specific treatments to manage Enterovirus A71 (EV-A71) induced hand, foot, and mouth disease because of its severe neurological complications. So far, no drug has been approved, but promising novel agents include molecular decoys, translation inhibitors, receptor antagonists and replication inhibitors. Ribavirin, quinacrine, amantadine, intravenous IgG (IVIG) and milrinone have all been used off-label to treat severe cases of Enterovirus A71 (EV-A71) induced hand, foot, and mouth disease disease 23, 24, 25. One new antiviral agent that has shown promise in the treatment of Enterovirus A71 (EV-A71) is pleconaril 26. Intravenous immunoglobulin and milrinone have shown some efficacy in a few reports.
Hand foot and mouth disease home remedies
Certain foods and beverages may irritate blisters on the tongue or in the mouth or throat. Try these tips to help make blister soreness less bothersome and eating and drinking more tolerable:
- Suck on ice pops or ice chips.
- Eat ice cream or sherbet.
- Drink cold beverages, such as milk or ice water.
- Avoid acidic foods and beverages, such as citrus fruits, fruit drinks and soda.
- Avoid salty or spicy foods.
- Eat soft foods that don’t require much chewing.
- Rinse your mouth with warm water after meals.
If your child is able to rinse without swallowing, swishing with warm salt water may be soothing. Combine ½ teaspoon salt with 1 glass of warm water and stir. Have your child do this several times a day or as often as needed to help reduce the pain and inflammation of mouth and throat sores caused by hand-foot-and-mouth disease.
Hand foot and mouth disease prognosis
The prognosis for the majority of patients with hand, foot, and mouth disease is excellent. Most patients recover within a few weeks without any residual sequelae. The acute illness usually lasts 10 to 14 days, and the infection rarely recurs or persists. However, some patients with hand, foot, and mouth disease may develop serious complications which include the following:
- Persistent stomatitis which is associated with painful mouth ulcers. The pain can be severe enough to limit intake of food and dehydration can result, especially in young children.
- Aseptic meningitis can occur, but this is more common with Enterovirus A71 (EV-A71). This particular virus is associated with a higher rate of neurological involvement compared to coxsackievirus. A previous study in Korea reported that headache and the presence of neurologic signs were significant risk factors for neurologic complications in hand, foot, and mouth disease 21. The individual may develop acute cerebellar ataxia, polio-like syndrome, encephalitis, cardiopulmonary failure, benign intracranial hypertension, Guillain-Barre syndrome or death 27. It is believed that the Enterovirus A71 (EV-A71) induces damage to the gray matter which then results in the motor dysfunction.
- Very rarely coxsackievirus can cause interstitial pneumonia, myocarditis, and pulmonary edema.
- Some studies indicate that coxsackievirus infections may also be associated with spontaneous abortions.
- Guerra AM, Orille E, Waseem M. Hand Foot And Mouth Disease. [Updated 2021 Nov 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431082
- Liu SL, Pan H, Liu P, Amer S, Chan TC, Zhan J, Huo X, Liu Y, Teng Z, Wang L, Zhuang H. Comparative epidemiology and virology of fatal and nonfatal cases of hand, foot and mouth disease in mainland China from 2008 to 2014. Rev Med Virol. 2015 Mar;25(2):115-28. doi: 10.1002/rmv.1827
- Mao, Q., Wang, Y., Yao, X., Bian, L., Wu, X., Xu, M., & Liang, Z. (2014). Coxsackievirus A16: epidemiology, diagnosis, and vaccine. Human vaccines & immunotherapeutics, 10(2), 360–367. https://doi.org/10.4161/hv.27087
- Yip, C. C., Lau, S. K., Woo, P. C., & Yuen, K. Y. (2013). Human enterovirus 71 epidemics: what’s next?. Emerging health threats journal, 6, 19780. https://doi.org/10.3402/ehtj.v6i0.19780
- McMinn PC. Recent advances in the molecular epidemiology and control of human enterovirus 71 infection. Curr Opin Virol. 2012 Apr;2(2):199-205. doi: 10.1016/j.coviro.2012.02.009
- Solomon T, Lewthwaite P, Perera D, Cardosa MJ, McMinn P, Ooi MH. Virology, epidemiology, pathogenesis, and control of enterovirus 71. Lancet Infect Dis. 2010 Nov;10(11):778-90. doi: 10.1016/S1473-3099(10)70194-8
- Hand, Foot, and Mouth Disease (HFMD) Causes & Transmission. https://www.cdc.gov/hand-foot-mouth/about/transmission.html
- Coates SJ, Davis MDP, Andersen LK. Temperature and humidity affect the incidence of hand, foot, and mouth disease: a systematic review of the literature – a report from the International Society of Dermatology Climate Change Committee. Int J Dermatol. 2019 Apr;58(4):388-399. doi: 10.1111/ijd.14188
- Murase C, Akiyama M. Hand, Foot, and Mouth Disease in an Adult. N Engl J Med. 2018 Apr 5;378(14):e20. doi: 10.1056/NEJMicm1713548
- Aronson SS, Shope TR, eds. Hand-foot-and-mouth disease. In: Managing Infectious Diseases in Child Care and Schools: A Quick Reference Guide. 4th ed. American Academy of Pediatrics; 2017:97–98.
- Klein, M., & Chong, P. (2015). Is a multivalent hand, foot, and mouth disease vaccine feasible?. Human vaccines & immunotherapeutics, 11(11), 2688–2704. https://doi.org/10.1080/21645515.2015.1049780
- Xu, S., Li, H., Qiao, P., Xu, G., Zhao, D., Lin, X., Qin, Y., Yu, H., Zhang, X., Zhang, W., & Huang, L. (2020). Neonatal hand, foot, and mouth disease due to coxsackievirus A6 in Shanghai. BMC pediatrics, 20(1), 364. https://doi.org/10.1186/s12887-020-02262-y
- Hand foot and mouth disease. https://dermnetnz.org/topics/hand-foot-and-mouth-disease
- Koh WM, Bogich T, Siegel K, et al. The epidemiology of hand, foot and mouth disease in Asia: a systematic review and analysis. Pediatr Infect Dis J. 2016;35(10):e285–e300.
- Muzumdar S, Rothe MJ, Grant-Kels JM. The rash with maculopapules and fever in children. Clin Dermatol. 2019 Mar-Apr;37(2):119-128. doi: 10.1016/j.clindermatol.2018.12.005
- Tsai, Y. H., Huang, S. W., Hsieh, W. S., Cheng, C. K., Chang, C. F., Wang, Y. F., & Wang, J. R. (2019). Enterovirus A71 Containing Codon-Deoptimized VP1 and High-Fidelity Polymerase as Next-Generation Vaccine Candidate. Journal of virology, 93(13), e02308-18. https://doi.org/10.1128/JVI.02308-18
- Nelson, B. R., Edinur, H. A., & Abdullah, M. T. (2019). Compendium of hand, foot and mouth disease data in Malaysia from years 2010-2017. Data in brief, 24, 103868. https://doi.org/10.1016/j.dib.2019.103868
- Chong CY, Chan KP, Shah VA, Ng WY, Lau G, Teo TE, et al. Hand, foot and mouth disease in Singapore: a comparison of fatal and non-fatal cases. Acta Paediatr. 2003 Oct. 92(10):1163-9.
- Chen SC, Chang HL, Yan TR, Cheng YT, Chen KT. An eight-year study of epidemiologic features of enterovirus 71 infection in Taiwan. Am J Trop Med Hyg. 2007 Jul. 77(1):188-91.
- Chang LY, Lin TY, Huang YC, Tsao KC, Shih SR, Kuo ML, et al. Comparison of enterovirus 71 and coxsackie-virus A16 clinical illnesses during the Taiwan enterovirus epidemic, 1998. Pediatr Infect Dis J. 1999 Dec. 18(12):1092-6.
- Kim, S. J., Kim, J. H., Kang, J. H., Kim, D. S., Kim, K. H., Kim, K. H., Kim, Y. H., Chung, J. Y., Bin, J. H., Jung, D. E., Kim, J. H., Kim, H. M., Cheon, D. S., Kang, B. H., Seo, S. Y., & Enteroviruses Complications Working Group (2013). Risk factors for neurologic complications of hand, foot and mouth disease in the Republic of Korea, 2009. Journal of Korean medical science, 28(1), 120–127. https://doi.org/10.3346/jkms.2013.28.1.120
- Peter McMinn, Ivan Stratov, Lakshmi Nagarajan, Stephen Davis, Neurological Manifestations of Enterovirus 71 Infection in Children during an Outbreak of Hand, Foot, and Mouth Disease in Western Australia, Clinical Infectious Diseases, Volume 32, Issue 2, 15 January 2001, Pages 236–242, https://doi.org/10.1086/318454
- Tan CW, Lai JK, Sam IC, Chan YF. Recent developments in antiviral agents against enterovirus 71 infection. J Biomed Sci. 2014. 21:14.
- Shih-Min Wang & Ching-Chuan Liu (2009) Enterovirus 71: epidemiology, pathogenesis and management, Expert Review of Anti-infective Therapy, 7:6, 735-742, DOI: 10.1586/eri.09.45
- Wang SM, Liu CC. Enterovirus 71: epidemiology, pathogenesis and management. Expert Rev Anti Infect Ther. 2009 Aug;7(6):735-42. doi: 10.1586/eri.09.45
- Kim, B., Moon, S., Bae, G. R., Lee, H., Pai, H., & Oh, S. H. (2018). Factors associated with severe neurologic complications in patients with either hand-foot-mouth disease or herpangina: A nationwide observational study in South Korea, 2009-2014. PloS one, 13(8), e0201726. https://doi.org/10.1371/journal.pone.0201726
- Choi, C. S., Choi, Y. J., Choi, U. Y., Han, J. W., Jeong, D. C., Kim, H. H., Kim, J. H., & Kang, J. H. (2011). Clinical manifestations of CNS infections caused by enterovirus type 71. Korean journal of pediatrics, 54(1), 11–16. https://doi.org/10.3345/kjp.2011.54.1.11