What is HGH
HGH is short for human growth hormone. Human growth hormone (HGH) is a 191 amino-acid single chain polypeptide, which is secreted by the somatotrophs in the anterior pituitary gland 1. With the recognition of its multiple and complex effects in the early 1960s, the physiology and regulation of HGH has become a major area of research interest in the field of endocrinology. Human growth hormone (HGH) is described by some as the key to slowing the aging process. Before you sign up, get the facts below.
HGH (human growth hormone) secretion is regulated by several factors including GHRH (growth hormone releasing hormone), somatostatin, ghrelin and IGF-1 (insulin-like growth factor I). Apart from growth hormone releasing hormone (GHRH) primary function of stimulation of growth hormone (GH) secretion, growth hormone releasing hormone (GHRH) plays an essential role in pituitary somatotroph development and proliferation. Somatostatin on the other hand is the main inhibitor of growth hormone secretion. Along with its receptors, somatostatin has been extensively studied over the last decade as a treatment for acromegaly. Several somatostatin receptors (SSTR) have been identified, of which SSTR2 and SSTR5 exhibit greater inhibition on the secretion of growth hormone by the somatotrophs. Somatostatin receptor ligands to SSTR2 and 5, such as octreotide, lanreotide and pasireotide, are approved treatment modalities for acromegaly in some countries.
Growth hormone (GH) is a hormone that is essential for normal growth and development in children. It promotes proper linear bone growth from birth through puberty. In both children and adults, growth hormone helps regulate the rate at which the body both produces energy from food (metabolism) and makes lipids, proteins, and glucose (sugar). It also helps regulate the production of red blood cells and muscle mass.
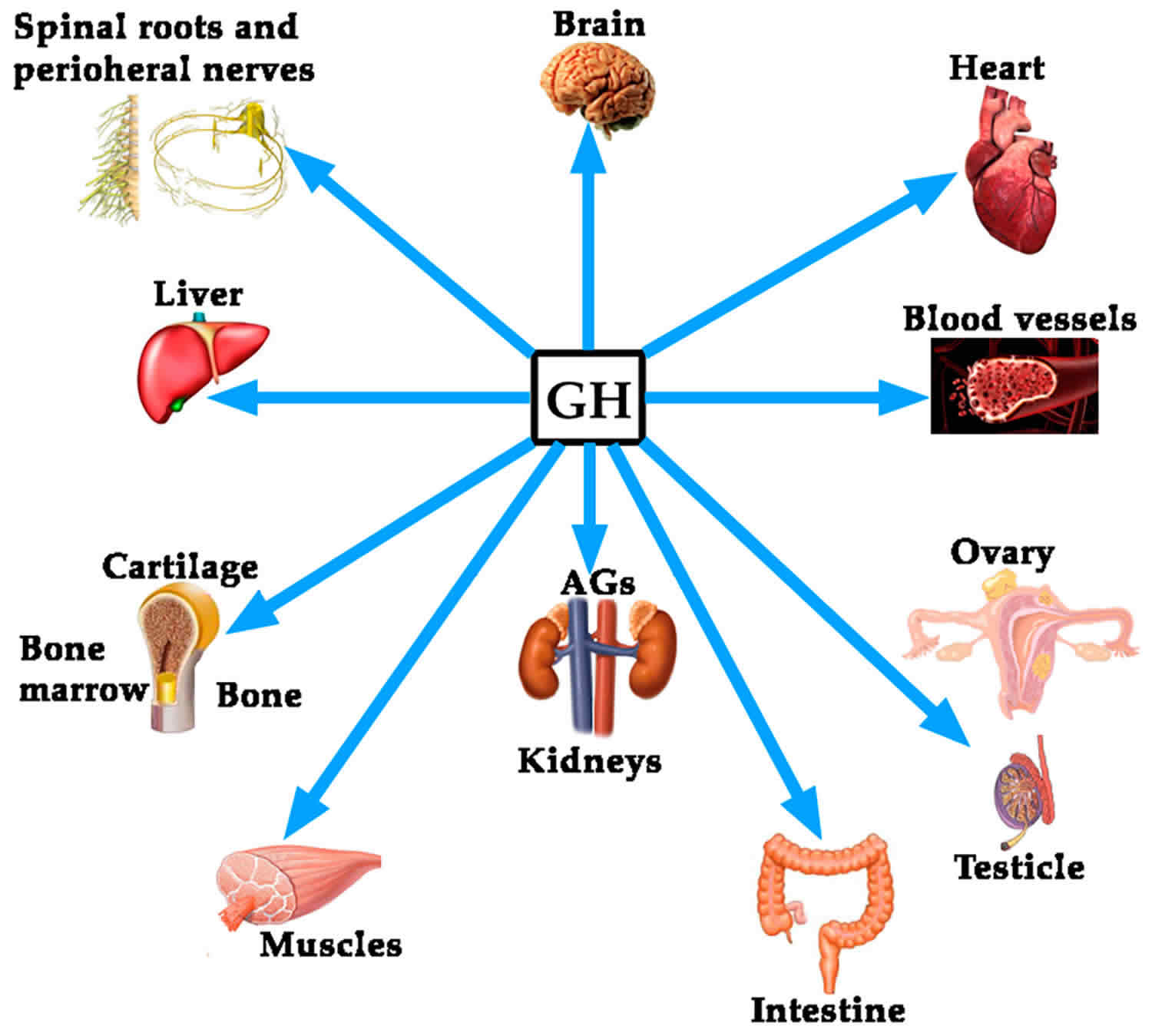
Growth hormone (GH) acts both directly through its own receptors and indirectly through the induced production of Insulin-like Growth Factor I (IGF-I) 1. The “IGF-1 axis” holds a significant place in the field of endocrinology, with numerous research been done on its pharmacokinetics and pharmacodynamics, affecting different organ systems in humans. Its physiological effects have been demonstrated not only in tissue growth, but also in glucose / lipid metabolism, coronary disease, diabetes mellitus and vascular aging. The use of recombinant IGF-1 in IGF-1 deficiency and insulin insensitivity and the use of IGF-1 receptor inhibitors in the promotion of cellular apoptosis, especially in the management of malignancies, are two other main areas of research in prospect.
Growth hormone (GH) is a dynamic hormone, which like most other hormones in the human body, varies in concentration and action under the influence of numerous factors. Growth hormone (GH) is normally released into the bloodstream in pulses throughout the day and night with peaks that occur mostly during the night. Characteristics including age, physical fitness and body composition play a major role in the level and action of growth hormone (GH) in humans and vice versa. It is well recognized for hrowth hormone (GH) vital role in glucose and lipid homeostasis and muscle mass function. These effects are of key significance, especially in the current era with increasing availability and use of recombinant growth hormone (rhGH) in the treatment of adult patients with growth hormone deficiency 2.
Growth hormone deficiency
Children with insufficient growth hormone production grow more slowly and are smaller in size for their age 3. Some children have growth hormone deficiency at birth (congenital), but some may develop a deficiency later due, for example, to a brain injury or tumor. These conditions can affect the pituitary gland, causing a decrease in pituitary function, resulting in a lowered production of pituitary hormones (hypopituitarism). Sometimes, the cause of the deficiency is not known.
In adults, growth hormone plays a role in regulating bone density, muscle mass, and glucose and lipid metabolism. It can also affect heart and kidney function. Deficiencies may have begun in childhood or develop in adulthood. A deficiency can develop, for example, because of damage to the pituitary gland caused by a head injury, brain tumor, or surgery or radiation treatment. This can result in a decrease in pituitary hormones (hypopituitarism). The deficiency in growth hormone can lead to decreased bone density, less muscle mass, and altered lipid levels. However, testing for growth hormone deficiency is not routine in adults who have decreased bone density and/or muscle strength or increased lipids. Growth hormone deficiency is a very rare cause of these disorders.
Growth hormone excess
Excess growth hormone is most often due to a growth hormone-secreting pituitary tumor (usually benign). Frequently, the pituitary tumor causing the excess can be surgically removed and/or treated with drugs or radiation. In most cases, this will cause growth hormone and IGF-1 levels to return to normal or near normal levels.
Too much growth hormone in children can cause their long bones to continue to grow beyond puberty, resulting in the extremely rare condition, gigantism, with heights of 7 or more feet. Those with excess growth hormone may also have thickening of facial features, general weakness, delayed puberty, and headaches.
Excess growth hormone in adults can lead to the rare condition, acromegaly, marked not by bone lengthening but by bone thickening. Although symptoms such as skin thickening, sweating, fatigue, headaches, and joint pain can be subtle at first, increased growth hormone levels can lead to enlarged hands and feet, enlarged facial bones, carpal tunnel syndrome, and abnormally enlarged internal organs. Excess growth hormone can also cause skin tags and intestinal polyps.
If left untreated, both acromegaly and gigantism can lead to complications such as type 2 diabetes, increased risk of cardiovascular disease, high blood pressure, arthritis, and in general, a decreased lifespan.
Regulation of human growth hormone secretion
Growth hormone is a single chain protein with 191 amino-acids and two disulfide bonds. The human growth hormone gene is located on chromosome 17q22 and comprises of five genes. It encodes two distinct growth hormone molecules (22 kDa and 20 kDa) of which 90% in the circulation constitute the 22kDa molecule 4.
Growth hormone is secreted by the somatotroph cells located primarily in the lateral wings of the anterior pituitary. There are many critical processes in pituitary organogenesis, including cell migration, proliferation, differentiation, establishing connections between cells/hypothalamus and development of vasculature including the hypophyseal portal system. Several transcription factors such as Pit-1/Pou1 F1 and PROP1 have been identified to play a vital role in the organogenesis of the anterior pituitary and the development of the somatotrophs. Inactivating mutations or deletions in these transcription factor genes lead to under-development of somatotrophs, lactotrophs and thyrotrophs, ultimately leading to anterior pituitary hypoplasia and pituitary hormone deficiency 5.
The morphological characteristics and number of somatotrophs are remarkably constant throughout life, while secretion changes. Growth hormone secretion occurs in a pulsatile fashion, and in a circadian rhythm with a maximal release in the second half of the night 1.
Two hypothalamic hormones regulate growth hormone secretion, Growth Hormone Releasing Hormone (GHRH) with a stimulatory action at the level of gene transcription, and somatostatin with an inhibitory effect on the growth hormone secretion from the pituitary gland (Figure 1).
Figure 1. Human growth hormone regulation – factors that stimulate and suppress human growth hormone secretion under physiological conditions
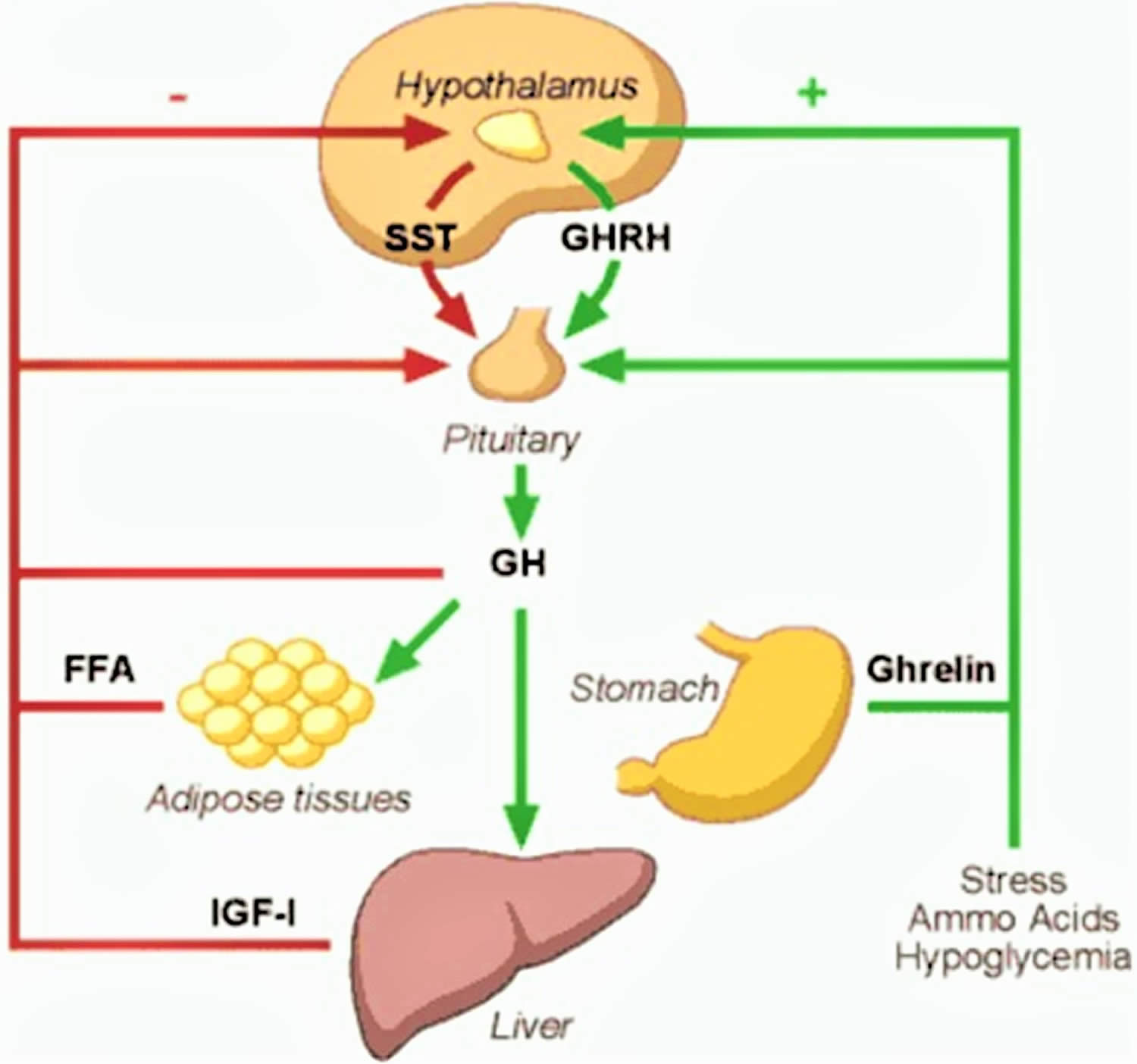 Abbreviations: GH = growth hormone; GHRH = growth hormone releasing hormone, SST = somatostatin; FFA = free fatty acid; IGF-1 =insulin-like growth factor-I
[Source 1 ]
Abbreviations: GH = growth hormone; GHRH = growth hormone releasing hormone, SST = somatostatin; FFA = free fatty acid; IGF-1 =insulin-like growth factor-I
[Source 1 ]What is growth hormone releasing hormone (GHRH)?
Growth hormone releasing hormone (GHRH) is a 44 amino-acid polypeptide produced in the arcuate nucleus of the hypothalamus. These neuronal terminals secrete growth hormone releasing hormone (GHRH) to reach the anterior pituitary somatotrophs via the portal venous system, which leads to growth hormone transcription and secretion. Moreover, animal studies have clearly demonstrated that growth hormone releasing hormone (GHRH) plays a vital role in the proliferation of somatotrophs in the anterior pituitary, where the absence of growth hormone releasing hormone (GHRH) has, in fact, lead to anterior pituitary hypoplasia 6. The secretion of growth hormone releasing hormone (GHRH) is stimulated by several factors including depolarization, α2-adrenergic stimulation, hypophysectomy, thyroidectomy and hypoglycaemia and it is inhibited by somatostatin, insulin-like growth factor-I (IGF-I) and activation of GABAergic neurons.
Growth hormone releasing hormone (GHRH) acts via a seven trans-membrane G protein-coupled stimulatory cell-surface receptor on the somatotrophs. This receptor has been extensively studied over the last decade leading to the identification of several important mutations. Point mutations in the growth hormone releasing hormone (GHRH) receptors, as illustrated by studies done on the lit/lit dwarf mice, showed a profound impact on subsequent somatotroph proliferation leading to anterior pituitary hypoplasia 7. Unlike the mutations in the Pit-1 and PROP-1 genes, which lead to multiple pituitary hormone deficiencies and anterior pituitary hypoplasia, mutations in the growth hormone releasing hormone (GHRH) receptor leads to profound growth hormone deficiency with anterior pituitary hypoplasia. Subsequent to the first growth hormone releasing hormone (GHRH) receptor mutation described by Wajnrajch, et al in 1996, an array of familial growth hormone releasing hormone (GHRH) receptor mutations have been recognized over the last decade. These mutations, in fact, account for almost 10% of the familial isolated growth hormone deficiencies. An affected individual will present with short stature and a hypoplastic anterior pituitary. However, they lack certain typical features of growth hormone deficiency such as midfacial hypoplasia, microphallus and neonatal hypoglycaemia 8.
What is somatostatin?
Somatostatin is a cyclic peptide, encoded by a single gene in humans, which mostly exerts inhibitory effects on endocrine and exocrine secretions. Many cells in the body including specialized cells in the anterior periventricular nucleus and arcuate nucleus produce somatostatin. These neurons secrete somatostatin into the adenohypophyseal portal venous system, via the median eminence, to exert its effect on the anterior pituitary. somatostatin has a short half-life of approximately 2 minutes as it is rapidly inactivated by tissue peptidase in humans. The secretion of somatostatin by the hypothalamic neurons is inhibited by high blood glucose and is induced by serum growth hormone/insulin-like growth factor-I (IGF-I) level, exercise and immobilization 9.
Somatostatin too acts via a seven trans-membrane, G protein coupled receptor and, thus far, five subtypes of the receptor have been identified in humans (somatostatinR1-5). Although all five receptor subtypes are expressed in the human fetal pituitary, adult pituitary only express 4 subtypes (somatostatinR1, somatostatinR2, somatostatinR3, somatostatinR5). Out of these four subtypes, somatotrophs exhibit more sensitivity to somatostatinR2 and somatostatinR5 ligands in inhibiting the secretion of growth hormone. In fact, the inhibition of both receptors seems to exert a synergistic effect on growth hormone inhibition rather than each receptor individually 10.
What is insulin-like growth factor-I (IGF-I)?
Multiple animal and human studies have analyzed the physiological effects of insulin-like growth factor-I (IGF-I) over the last two decades. Initial studies on hypophysectomised animals showed IGF-I to promote growth in all tissues with major rate limitation with hypoglycaemia. These studies also demonstrated the anabolic effects of IGF-I by way of increasing glomerular filtration rate (GFR), improving wound healing and reversal of catabolic effects of nutritional deprivation 11.
Insulin-like growth factor-I (IGF-I) plays a key role in growth, where it acts not only as a determinant of postnatal growth, but also as an intra-uterine growth promoter. Total inactivation of the IGF-I gene in mice produced a perinatal mortality of 80% with the surviving animal showing significant growth retardation compared to controls 12. Human IGF-I deficiency can be either due to growth hormone deficiency, growth hormone receptor inactivation or IGF-I gene mutation. Interestingly, infants with congenital growth hormone deficiency and growth hormone receptor mutations present with only minor growth retardation, whereas the rare patient with IGF-I deficiency, secondary to a homozygous partial deletion of the IGF-I gene, presents with severe pre and postnatal growth failure, mental retardation, sensorineural deafness and microcephaly 13. The differences in the clinical presentation is most likely due to the fact that some degree of IGF-I production is present in patients with growth hormone and growth hormone releasing hormone (GHRH) defects.
More detailed studies on transgenic mice have clearly demonstrated this fact with selective deletion of IGF-I gene expression only in the liver, showing low serum IGF-I concentrations with only 6-8% postnatal growth retardation. In contrast, animals with total IGF-I deletion or only peripherally produced IGF-I deletion showed marked growth retardation 14. Therefore, considering growth, both paracrine/autocrine IGF-1 and liver-derived IGF-I are important in achieving the final adult height.
Both elevated and reduced levels of serum insulin-like growth factor-I (IGF-I) are associated with excess mortality in human adults 15. In addition, it is well recognized in many species including worms, flies, rodents and primates that a reciprocal relationship exists between longevity and activation of the insulin/IGF axis 16. The underlying mechanisms are subjects to continued scrutiny and are likely to be complex. In this regard, it is noteworthy that calorie restriction, associates with increased longevity and reduced insulin/IGF activity in many species 17 since growth hormone levels are increased in calorie restriction and fasting 18. In the context of growth hormone and IGF-I physiology it can be hypothesized that 1) during childhood and adolescence the combined actions of growth hormone and IGF-I in the presence of sufficient nutrition promote longitudinal growth and somatic maturation, 2) continued excess IGF-I activity in adulthood increases the risk for cardiovascular and neoplastic diseases and hence reduces longevity, 3) calorie restriction, which suppresses IGF-I activity and promotes growth hormone secretion, may promote longevity also in human adults 18.
Influence of body composition, physical fitness and age on growth hormone levels
With the introduction of dependable radioimmunological assays it was recognized that circulating growth hormone was blunted in obese subjects 19, and that normal aging was accompanied by a gradual decline in growth hormone levels 20. The latter observation led Rudman et al. 21 to the hypothesis that many of the senescent changes in body composition and organ function were related to or caused by hyposomatotropinemia. The term “somatopause” may be considered a paraphrase for Rudmans hypothesis although it remains uncertain who introduced this persuasive term.
Studies done in the late 90s have uniformly documented that hypopituitary adults with severe growth hormone-deficiency are characterized by increased fat mass and reduced lean body mass 22. It is also known that normal growth hormone levels can be restored in obese subjects following massive weight loss 23, and that growth hormone substitution in growth hormone-deficient adults normalizes body composition 22.
What remains unknown is the cause-effect relationship between hyposomatotropenimia and senescent changes in body composition. Is the propensity for gaining fat and loosing lean body mas initiated or preceded by a primary age-dependent decline in growth hormone secretion and action or vice versa?: accumulation of fat mass secondary to non-growth hormone dependent factors (e.g. life style, dietary habits) results in a feedback inhibition of growth hormone secretion
Moreover, little is known about possible age-associated changes in growth hormone pharmacokinetics and bioactivity.
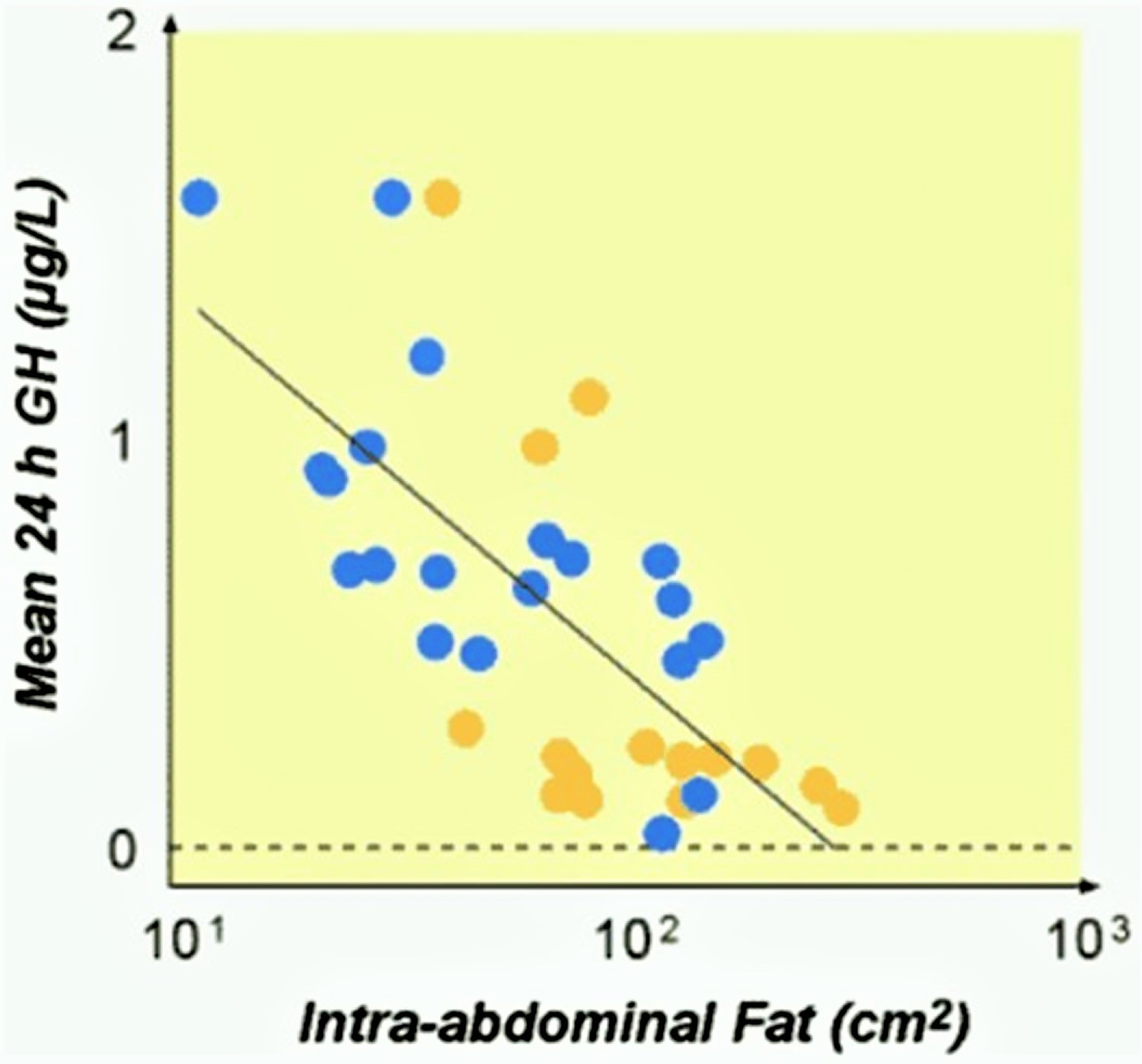
Cross sectional studies done to assess the association between body composition and stimulated growth hormone release in healthy subjects showed that, elderly people (mean age 50 years) had a lower peak growth hormone response to secretagogues (clonidine and arginine), and females had a higher response to arginine when compared to males. Multiple regression analysis, however, revealed that intra-abdominal fat mass was the most important negative predictor of peak growth hormone levels (Figure 2), where as both age, gender and physical fitness were of minor importance. Lean body mass was not significantly associated with growth hormone status in either males or females 24.
Figure 2. Correlation between intra-abdominal fat mass and 24 hour growth hormone secretion
In the same population 24-hour spontaneous growth hormone levels were also analyzed by means of deconvolution analysis of samples obtained every 20-minute. Mean growth hormone levels, growth hormone production rate and growth hormone burst amplitude were higher in young people and in females as compared to older people and males 26. Multiple regression analysis again suggested that intra-abdominal fat mass was the single most important and negative determinant of growth hormone status. Fasting levels of insulin, IGF-I and free fatty acids did not correlate with either estimates of growth hormone status. Surprisingly, lean body mass exhibited a weak inverse correlation with mean 24-hour growth hormone release, but lean body mass was not associated with other attributes of growth hormone status and was not an independent determinant by multiple regression analysis.
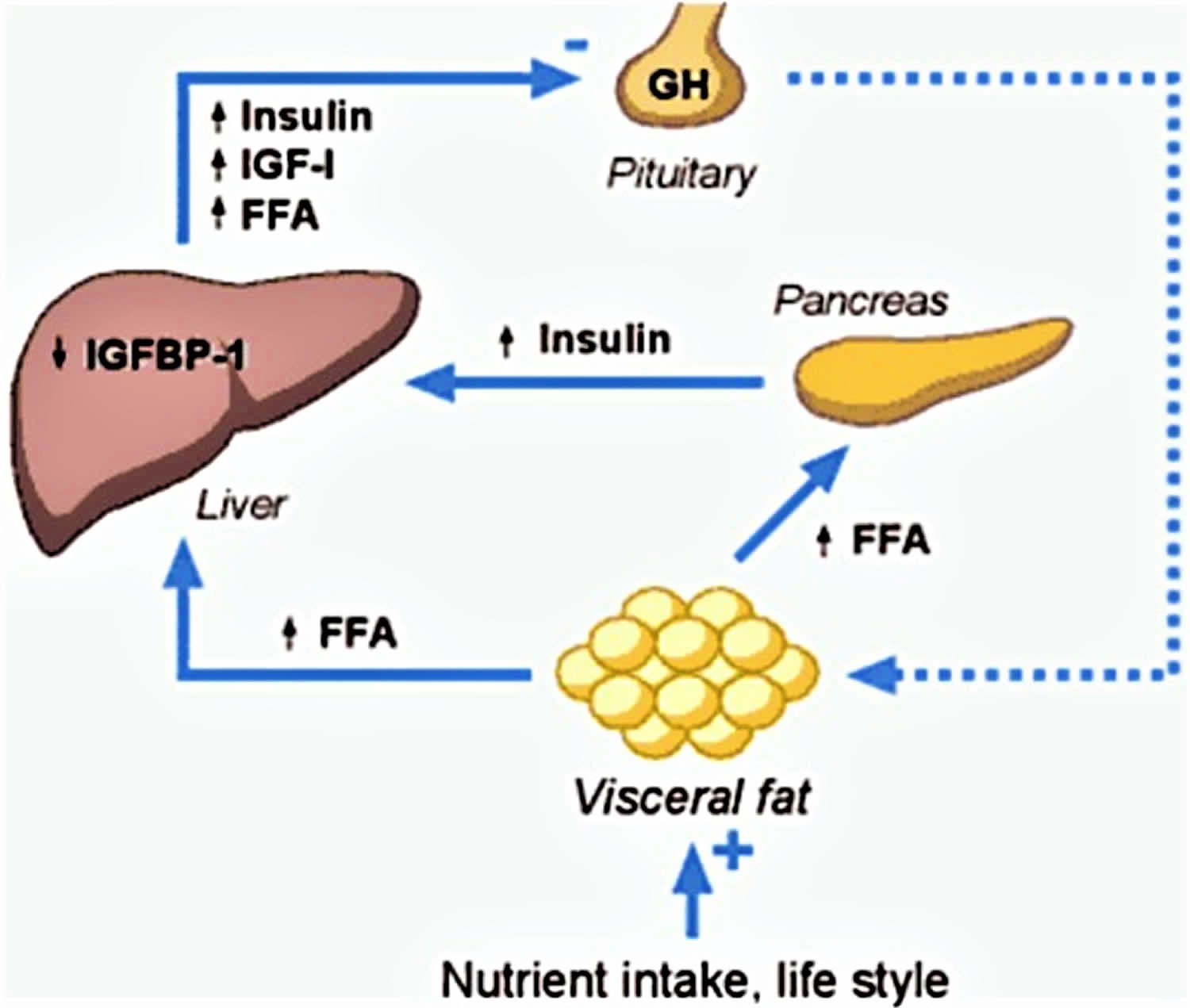
Figure 3. Hypothetical model for the association between growth hormone levels and body composition in adults
Abbreviations: IGF-I = insulin-like growth factor-I; FFA = free fatty acid; IGFBP-1 = insulin-like growth factor-binding protein-1
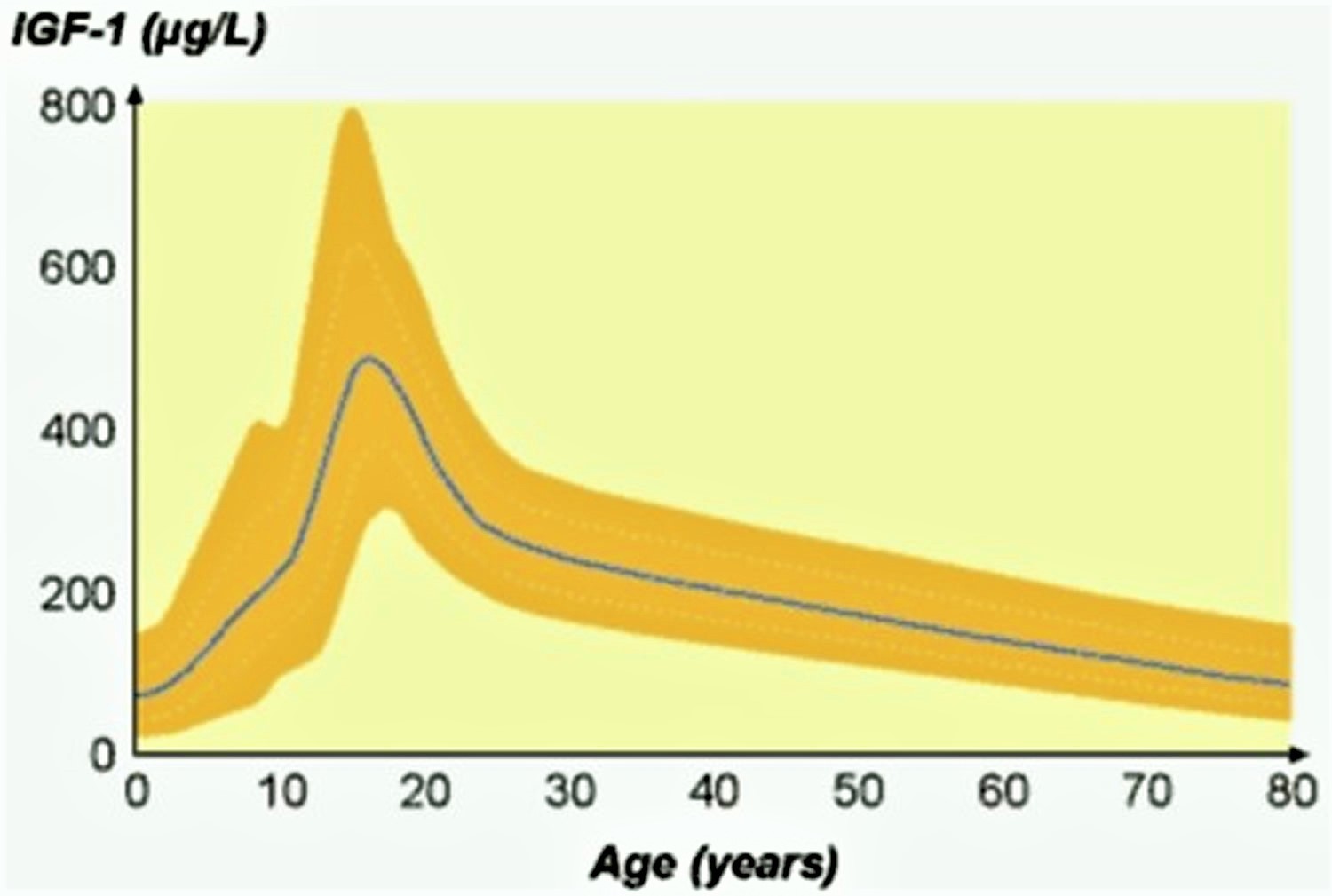
[Source 25 ]A detailed analysis of growth hormone secretion in relation to body composition in elderly subjects has, not been performed. Instead serum IGF-I has been used as a surrogate or proxy for growth hormone status in several studies of elderly men 27. These studies comprise large populations of ambulatory, community-dwelling males aged between 50-90 years. Not unexpectedly serum IGF-I declined with age (Figure 4), but IGF-I failed to show any significant association with body composition or physical performance 27.
Figure 4. Changes in serum insulin-like growth factor-I (IGF-I) with increasing age
[Source 25 ]Other regulators of growth hormone secretion
Various synthetically produced growth hormone releasing compounds and natural hormone ghrelin have been shown to increases the production of growth hormone. Ghrelin is a 28 amino-acid peptide that is the natural ligand for the growth hormone secretagogue receptor. In fact, ghrelin and GHRH have a synergistic effect in increasing circulating growth hormone levels 25. Interestingly, exogenous ghrelin stimulates food intake and gastric emptying 28. In everyday life it is known, that stress, hypoglycemia and ingestion of protein (high levels of circulating amino acids) stimulates growth hormone secretion, while high levels of glucose and free fatty acid inhibits secretion (see Figure 1 above).
Influence of age, sex and body composition on growth hormone action
Considering the great interest in the actions of growth hormone in adults surprisingly few studies have addressed possible age-associated differences in the responsiveness or sensitivity to growth hormone. In normal adults the senescent decline in growth hormone levels is paralleled by a decline in serum IGF-I, suggesting a down-regulation of the growth hormone-IGF-I axis. Administration of growth hormone to elderly healthy adults has generally been associated with predictable albeit modest effects on body composition and a high incidence of side-effects 29. Whether this reflects an unfavorable balance between effects and side effects in older people or employment of excessive doses of growth hormone is uncertain, but it is evident that older subjects are not resistant to growth hormone. Studies in growth hormone deficient adults with pituitary disease strongly suggest that the dose requirement declines with age. Short-term dose response studies clearly demonstrate that older patients require a lower growth hormone dose to maintain a given serum IGF-I level 30, and it has been observed that serum IGF-I increases in individual patients on long-term therapy if the growth hormone dosage remains constant 31. It has also recently been reported that hypopituitary patients above 60 years are highly responsive to even a small dose of growth hormone 32. Interestingly, there appears to be a gender difference in growth hormone deficient adults with men being more responsive in terms of IGF-I generation and fat loss during therapy 33.
The pharmacokinetics and short-term metabolic effects of a near physiological intravenous growth hormone bolus (200 g) were compared in a group of young (30 years) and older (50 years) healthy adults 34. The area under the growth hormone curve was significantly lower in older subjects, whereas the elimination half-life was similar in the 2 groups, suggesting both an increased metabolic clearance rate and apparent distribution volume of growth hormone in older subjects. Both metabolic clearance rate and apparent distribution volume showed a strong positive correlation with fat mass, although multiple regression analysis revealed age to be an independent positive predictor. The short-term lipolytic response to the growth hormone bolus was higher in “young” as compared to “older” subjects, respectively. Interestingly, the same study revealed that the growth hormone binding protein correlated strongly and positively with abdominal fat mass 35.
Growth hormone studies in normal adults
Almost forty years ago it was shown that infusion of high dose growth hormone into the brachial artery of healthy adults reduced forearm glucose uptake in both muscle and adipose tissue 36. This was paralleled by a drop in basal metabolic rate and an increase in muscle uptake of free fatty acid, both of which suggested oxidation of free fatty acid by the muscle. This pattern was opposite that of insulin, and co-administration of insulin and growth hormone resulted in only minimal changes in net fluxes of glucose and free fatty acid across the forearm bed. These studies clearly indicated direct insulin antagonistic effects of growth hormone on muscle and adipose tissue.
The introduction of reliable radioimmunoassays for growth hormone revealed the pulsatile and episodic nature of growth hormone release 37 now known to be generated by alternating secretion of growth hormone releasing hormone (GHRH) and somatostatin. A growth hormone pulse is released roughly every second hour with a mean daily secretion of 0.5 mg 38. Apart from a well-known circadian variation in terms of elevated nocturnal growth hormone levels during the early hours of sleep, growth hormone secretion is amplified during fasting and stress, whereas meals suppress growth hormone release 39.
Scientists studied the metabolic effect of a physiological growth hormone bolus in the post absorptive state, and demonstrated stimulation of lipolysis following a lag time of 2-3 hours to be the most consistent effect 40. Plasma glucose, on the other hand exhibited only minimal fluctuations, and serum insulin and C- peptide levels remained completely stable. This was associated with subtle reductions in muscular glucose up-take and oxidation, which could reflect substrate competition between glucose and fatty acids (i.e. the glucose/fatty acid cycle). In line with this, sustained exposure to high growth hormone levels induces both hepatic and peripheral (muscular) resistance to the actions of insulin on glucose metabolism together with increased (or inadequately suppressed) lipid oxidation. Apart from enhanced glucose/fatty acid cycling, it has been shown that growth hormone induced insulin resistance is accompanied by reduced muscle glycogen synthase activity 41 and diminished glucose dependent glucose disposal 42. Bak et al. 41 also demonstrated insulin binding and insulin receptor kinase activity from muscle biopsies to be unaffected by growth hormone.
Luft et al. 43 clearly demonstrated the glycemic control to deteriorate following exposure to a single supra-physiological dose of human growth hormone in hypophysectomised adults with type 1 diabetes mellitus. Somewhat surprisingly, only modest effects of growth hormone on glucose metabolism were recorded in the first metabolic balance studies involving adult hypopituitary patients 44.
Active acromegaly clearly unmasks the diabetogenic properties of growth hormone. In the basal state plasma glucose is elevated despite compensatory hyperinsulinemia. In the basal and insulin-stimulated state (euglycemic glucose clamp) hepatic and peripheral insulin resistance is associated with enhanced lipid oxidation and energy expenditure 45. There is evidence to suggest that this hyper-metabolic state ultimately leads to beta cell exhaustion’ and overt diabetes mellitus 46, but a more recent study have demonstrated that the abnormalities are completely reversed after successful surgery 45. Conversely, it has been shown that only two weeks administration of growth hormone in supraphysiological doses (8 IU/day) induces comparable acromegaloid – and reversible – abnormalities in substrate metabolism and insulin sensitivity 47.
Effects of growth hormone muscle mass and function in adults without growth hormone-deficiency
The ability of acute and more prolonged growth hormone administration to retain nitrogen in normal adults has been known for decades and more recent studies have documented a stimulatory effect on whole body and forearm protein synthesis.
Rudman et al. 48 was the first to suggest the secretion of growth hormone and IGF-1 levels decline during advancing years-of-life. Growth hormone production and secretion, growth hormone binding protein (GHBP), and insulin-like growth factor-1 (IGF-1) levels decline with aging, which is often referred to as the “somatopause” 49. These changes (somatopause) are associated with age-related loss of vitality and vigor, muscle mass (sarcopenia), physical function and activities of daily living, together with the occurrence of frailty, central adiposity, accelerated risks for cardiovascular complications, and deterioration of mental function 49. The hope is that growth hormone supplementation would slow these processes and improve health during aging. However, treatment with growth hormone has adverse effects and could impair survival if it hastens development of certain cancers (e.g. via IGF-1) or insulin resistance which accelerates the metabolic syndrome.
After puberty, growth hormone levels decrease exponentially 50. Production is reported to decline by 14% per decade 51 and may decline by up to 50% every seven years for adult men 52. Elderly men may produce as little as 50 μg/day compared with pubertal boys who produce 1.0–1.5 mg/day 53. In men 60 years-of-age or older, 35% were growth hormone-deficient 54. Similarly, serum IGF-1 levels progressively decline through the 8th and 9th decades of life and 85% of healthy 59–98 year-old men had low serum IGF-1 levels below the 2.5th percentile for younger men 55.
The mechanism underlying the so-called “somatopause” involves other and perhaps more complex mechanisms than the female menopause. In the mean time the following hypothesis have been proposed:
- Changes in life-style and genetic predispositions promote accumulation of body fat with aging.
- The increased fat mass increases free fatty acid (FFA) availability, inducing insulin resistance and hyperinsulinemia.
- High insulin levels sup- press insulin-like growth factor-binding protein-1 (IGFBP-1) resulting in a relative increase in free IGF-I levels.
- Systemic elevations in free fatty acid (FFA), insulin and free IGF- I suppresses pituitary growth hormone release, which further increases fat mass.
- Endogenous growth hormone is cleared more rapidly in subjects with high amount of fat tissue.
Growth hormone treatment has been hypothesized to augment effects of testosterone supplementation in older men. In one study, there was no benefit to growth hormone treatment or positive interaction of the two hormones on lean body mass or muscle performance 56 In a study by Blackman 57, muscle performance did not improve with either HGH or testosterone treatment alone (100 mg biweekly), but 1-repeition maximum (1-RM) strength and aerobic capacity by VO2max increased significantly with the combination. In a third study, 112 (65–90 year-old) community-dwelling men were randomized to placebo, 3 or 5 μg/kg/day of HGH or transdermal testosterone gel (5-or-10 g/d) for 16 weeks 58. Total and appendicular lean body mass were enhanced by addition of HGH. For men who achieved at least 1.5 kg increases in total and 0.8 kg increases in appendicular lean body mass, there were significant increases of ≥30% in 1-RM strength. Aerobic endurance improved substantially during treatment with both hormones. These latter two studies suggest that HGH may indeed enhance the effects of testosterone administration on muscle performance.
Placebo-controlled growth hormone administration in young healthy adults (21-34 years) undergoing a resistance exercise program for 12 weeks showed a growth hormone induced increase in lean body mass, whole body protein balance and whole body protein synthesis, whereas quadriceps muscle protein synthesis rate and muscle strength increased to the same degree in both groups during training 59. In a similar study in older men (67 years) growth hormone also increased lean body mass and whole body protein synthesis, without significantly amplifying the effects of exercise on muscle protein synthesis or muscle strength 60. An increase in lean body mass but unaltered muscle strength following 10 weeks of growth hormone administration plus resistance exercise training was also recorded by Taafe et al. 61. A more recent study of 52 older men (70-85 years) treated with either growth hormone or placebo for 6 months, without concomitant exercise, observed a significant increase (4.4 %) in lean body mass with growth hormone, but no significant effects on muscle strength 62. Thus no significant clinical benefit from administrating growth hormone to non-growth hormone-deficient senescent patients has been documented yet.
Numerous studies have evaluated the effects of growth hormone administration in chronic and acute catabolic illness. It is noteworthy, that HIV-associated body wasting is a licensed indication for growth hormone treatment in the USA. In this patient category growth hormone treatment for 12 weeks has been associated with significant increments in lean body mass and physical fitness 63.
Studies relating growth hormone and IGF-1 status to longevity provide inconsistent evidence as to whether decreased (somatopause) or high levels (e.g. acromegaly) of these hormones are beneficial or detrimental to longevity 49. Laron Syndrome dwarfs with growth hormone gene deletion and low IGF-1 levels have signs of early aging including wrinkled skin, insulin resistance and diabetes, but lack endothelial dysfunction and have long life-spans often reaching 80–90 years 64. Laron Syndrome dwarfs in one Brazilian cohort of 222 subjects had no malignancies compared to 9–24% of family members who had cancer 65. A small subset (n = 22) of Brazilian patients with Laron Syndrome had increased abdominal obesity, elevated LDL”bad” cholesterol and C-reactive protein (CRP) but lacked increases of carotid intima media thickness or abnormalities with stress echo-cardiograms 66. Reductions in malignancy and atherosclerosis may explain prolonged survival in this population. Finally, natural mutations in the IGF-1 receptor producing cellular resistance to IGF-1 have resulted in short stature and extended longevity. These mutations have been over-represented in centenarians 67.
Ecuadorians with growth hormone receptor mutations, IGF-1 deficiency, and cellular protection from oxidative damage have stunted growth, lower incidence of diabetes and cancer but do not have increased longevity 49. These Ecuadorians may actually have shorter life-spans and two thirds die by 65 years-of-age 68. In patients with Hereditary Dwarfism based on a 7.6 kb deletion of the growth hormone gene resulting in isolated growth hormone deficiency live substantially shorter life-spans compared to family siblings 69, as do adults with untreated growth hormone deficiency and hypopituitarism 70.
Several longitudinal studies provide additional glimpses of the potential effects of growth hormone and IGF-1 on aging. In a report from the Netherlands of 2694 adults with growth hormone deficiency who were treated and followed for an average of 6.1 years, there were 95 deaths 70. The standardized mortality rate was no greater in men but was significantly increased in women due to cardiovascular disease. An 8-year longitudinal study of 376 older men (73–94 years-of-age) showed that men in lowest quartile of IGF-1 bioactivity had a 1.8-fold increased mortality versus the highest quartile 71.
Growth hormone and athletic performance
Much public attention has been given to abuse of growth hormone by professional athletes and Olympic performers. Risk for serious adverse health outcomes and potential for unfair performance advantages are concerning. It is possible that recreational and Master Athletes who perform into their 7–9th decades could also abuse growth hormone.
In one study of rhgrowth hormone (2 mg/d) or placebo for eight weeks in adult recreational athletes, growth hormone administration increased lean body mass by increasing extracellular water but did not increase body cell mass, muscle strength, power or aerobic endurance in men 72. In a meta-analysis of almost 4500 studies, there were only 8 randomized controlled studies that reported muscle performance outcomes 73. Although there were demonstrable benefits on body composition and metabolism in growth hormone treated participants compared to no therapy, growth hormone treatment did not increase biceps or quadriceps strength, improve VO2max, bicycling speed, and power output but was associated with greater lactate production and fatigue. In this meta-analysis, treatment was relatively short (≤3 months) and doses may not have reflected those used during doping or the effect of concomitant use of other anabolic hormones (e.g. testosterone or insulin). These studies suggest that treatment with growth hormone alone generally does not improve physical strength or endurance. It is possible that small improvements, for example, in aerobic endurance, that would not be quantifiable in clinical studies could confer an athletic advantage. There is little reason to believe that the effects would be different in older men with marginally lower growth hormone/IGF-1 status than these younger study participants.
Summary
It is difficult to reconcile the largely protective effects of growth hormone/IGF-1 deficiency on longevity in animals with the inconsistent or deleterious effects of low levels or declining growth hormone/IGF-1 during human aging. Further, the beneficial and adverse regulatory effects of IGF-1 and growth hormone on various organ-specific tissues and aspects of metabolism is incompletely understood and must be investigated to understand pathophysiology that affects longevity and co-morbidities in advanced years (Table 1).
Table 1. Effects of growth hormone and IGF-1 deficiency and excess on longevity in humans
| Mechanism | Clinical outcomes | Longevity effects |
| Growth hormone deficiency | ||
| Ecuadorians – GH receptor mutation | ↑ insulin sensitivity, ↓ incidence of diabetes and cancer | No ↑ 2/3 die by 65 years-of-age |
| Laron Syndrome – GH gene deletion | Early aging – wrinkled skin, insulin resistance, osteopenia but normal endothelial function | May be ↑ to 80–90 years |
| Hereditary Dwarfism – 6.7 kb deletion in the GH gene – untreated GHD | Small stature and heart problems | Shortened versus unaffected sibs |
| Laron Syndrome (n = 222) | No malignancies versus 9–24% in family members | Expected to be ↑ |
| Isolated GHRH-receptor mutation; Brazilian dwarfs (untreated) | Obesity, ↑ LDL-C; no insulin resistance or premature CVD | Not shortened |
| IGF-1 deficiency | ||
| Ashkenazi Jewish centenarians | Short stature, over-representation of mutations in the IGF-1 receptor gene (females only) | Prolonged |
| Polymorphic variants of IGF-1 path (IGF-1r, PI3K, IRS-1, FOXO1A) | ↓ IGF-1 and variants over-represented in long-lived persons | Prolonged |
| Growth hormone excess or growth hormone treatment | ||
| Acromegaly | ↑ diabetes, CVD, heart failure, colon cancer; tumors have increased IGF-1 receptors | Shortened |
| Pituitary extract treatment; United Kingdom cohort | ↑ incidence of colon cancer and Hodgkin’s disease | Shortened |
| Pituitary extract treatment; United States cohort | ↑ deaths due to hypoglycemia and adrenal insufficiency | Death rate ↑ 4-fold |
| Treatment – children with GHD (n = 6928,17 years later) | No ↑ cancer (except bone) but CVD outcomes increased; ↑ risk if dose ≥50 mg/kg/day | ↑ mortality |
| Treatment – adults with GHD (n = 2694; 13,000 treatment years) | Rates of cancer not ↑; mortality ↑ in women (CVD events) | Not affected in men |
Abbreviations: GH = growth hormone; GHD = growth hormone deficieny; CVD = cardiovascular disease
[Source 49 ]Key points
- There is no compelling data that empiric treatment of older men with HGH improves muscle strength or performance (walking speed or ability to climb stairs) or quality of life. Thus, it is unlikely to benefit patients with sarcopenia or frailty.
- Despite enthusiasm for treatment of somatopause and projections that many tens of thousands of persons are using growth hormone as an anti-aging therapy, there is little evidence to support its use to extend longevity or restore youthful health.
- A limited number of studies suggest that growth hormone supplementation in older men does increase total lean body mass modestly by about 2 kg with a similar reduction in fat mass. These effects appear gender specific as women are generally more resistant to the effects of growth hormone, with more modest increases in IGF-1 at similar doses and they often do not show improvements in lean body mass or fat mass 74. However, there is little controlled evidence that treating older men with growth hormone alone improves voluntary muscle strength or performance (e.g. walking speed or ability to climb stairs) or importantly quality of life.
- Growth hormone administration frequently causes adverse events including edema, arthralgias, carpel tunnel syndrome and early insulin resistance.
- Consideration of treatment for idiopathic growth hormone deficiency should be based on presence of signs and symptoms consistent with adult onset growth hormone deficiency.
- Treatment should not be initiated without evidence of impaired growth hormone stimulation by provocative testing (e.g. GHRH-arginine stimulation) since patients may have growth hormone deficiency even with normal serum levels of IGF-1.
- Adverse events with HGH are not frequent with appropriate physiologic dosing but there remain increased risks for arthralgias, carpal tunnel syndrome, fluid retention, increases in blood pressure, and insulin resistance along with other unforeseen effects including potential for increased cancer risk from IGF-1 stimulation.
- Healthcare practitioners need to be alert to abuse of HGH by even older recreational athletes or those desiring to experiment with it as an anti-aging antidote.
HGH and Healthy Aging
Healthy aging is a hot topic. Whether you’re concerned about weight gain, sex drive or chronic diseases, the key to healthy aging is a healthy lifestyle. Eating a variety of nutritious foods, practicing portion control and including physical activity in your daily routine can go a long way toward promoting healthy aging.
If an interest in healthy aging leads you to consider anti-aging therapies — such as restrictive diets, supplements or expensive treatments claiming to postpone or even reverse the aging process — be cautious. There’s no quick fix when it comes to healthy aging. Know what you’re buying, and know how to spot suspicious schemes. Often, anti-aging therapies don’t live up to the claims.
Growth hormone fuels childhood growth and helps maintain tissues and organs throughout life. Human growth hormone produced by the pea-sized anterior pituitary gland — located at the base of the brain. Beginning in middle age, however, the pituitary gland slowly reduces the amount of growth hormone it produces.
This natural slowdown has triggered an interest in using synthetic human growth hormone (HGH) as a way to stave off some of the changes linked to aging, such as decreased muscle and bone mass.
If you’re skeptical, good. There’s little evidence to suggest human growth hormone can help otherwise healthy adults regain youth and vitality. In fact, experts recommend against using HGH to treat aging or age-related conditions.
However, recent data suggest treatment with a GHRH agonist (tesamorelin) can restore normal growth hormone pulsatility and amplitude, increases IGF-1 to upper physiologic ranges, and selectively reduces visceral adipose tissue, carotid intima media thickness, C-reactive protein (CRP), and triglycerides, and improves cognitive function in some older persons. recent observations that tesamorelin benefits important age-related processes affecting cardiovascular disease morbidity and mental function without substantive increases in risk for toxicity or insulin resistance for the older men 49. The GHRH analog, tesamorelin, should be further tested in non-HIV populations (both men and women) to evaluate its effects on reducing abdominal visceral adipose tissue in patients with metabolic syndrome along with those at increased risk for major vessel atherosclerosis and as a potential therapy to treat and prevent dementia, especially in abdominally obese persons.
Do some adults need human growth hormone?
Yes. Adults who have true growth hormone deficiency 2 — not the expected decline in growth hormone due to aging — might be prescribed synthetic human growth hormone by their doctors.
Growth hormone deficiency might be caused by a benign tumor on the pituitary gland (pituitary adenoma). It also might be caused by treatment of a pituitary adenoma with surgery or radiotherapy.
For adults who have a growth hormone deficiency, injections of human growth hormone can:
- Increase exercise capacity
- Increase bone density
- Increase muscle mass
- Decrease body fat
Table 2. Long-term benefits and risks of growth hormone replacement therapy in adult patients with growth hormone deficiency
| Patient Data | Benefits | Risks or Drawbacks |
|---|---|---|
| Body composition | Reduction in fat mass Increase in lean mass Increase in muscle strength | Increase in BMI Increased waist circumference Increase of waist-hip index |
| Bone metabolism | Increase in bone mineral density | Effect on the incidence of fractures not clearly shown |
| Health-related quality of life | Improvement in quality of life questionnaires Greater benefit in patients with low quality of life at baseline | No improvement in all dimensions Probable absence of effect in patients with normal quality of life |
| Cardiovascular risk markers | Increase in HDL-cholesterol Reduction of total and LDL-cholesterol Diastolic blood pressure reduction Reduction of CRP Reduction of carotid intima-media thickness | Reduced insulin sensitivity Increase in fasting glucose and insulin Trend to the increase in the prevalence of metabolic syndrome Increase in lipoprotein (a) |
| Cardiovascular disease | Reduction in the incidence rate of myocardial infarction | Trend to increase in cerebrovascular disease |
| Neoplasms | No increase in the rate of recurrence or progression of hypothalamic-pituitary tumors No increase in overall risk of neoplasia in adults with growth hormone deficiency | Tendency to increase risk of second malignancy in childhood cancer survivors treated with HGH in childhood There are subgroups with increased risk of certain neoplasia in adults who were treated with HGH in childhood |
| Mortality | Tendency to decrease the global and cardiovascular mortality of hypopituitarism | Persistence of higher mortality than the general population in some studies |
Abbreviations: BMI = body mass index; HDL = high density lipoprotein (good cholesterol); LDL = low density lipoprotein (bad cholesterol); CRP = C-reactive protein; GHD = deficiency of growth hormone; HGH = human growth hormone.
[Source 2 ]Human growth hormone (HGH) is also approved to treat adults with AIDS or HIV-related muscle wasting.
Studies of healthy adults taking HGH are limited. Although it appears that human growth hormone can increase muscle mass and reduce the amount of body fat in healthy older adults, the increase in muscle doesn’t translate into increased strength. It isn’t clear if HGH (human growth hormone) might provide other benefits to healthy adults.
Human growth hormone might cause a number of side effects for healthy adults, including:
- Carpal tunnel syndrome
- Increased insulin resistance
- Swelling in the arms and legs (edema)
- Joint and muscle pain
- For men, enlargement of breast tissue (gynecomastia)
HGH (human growth hormone) might also contribute to conditions such as type 2 diabetes and heart disease and possibly an increased risk of some cancers.
Some research suggests that side effects of HGH (human growth hormone) treatments might be more likely in older adults than in younger people. Because the studies of healthy adults taking human growth hormone have been short term, it isn’t clear whether the side effects could eventually dissipate or become worse.
When prescribed by a doctor, HGH (human growth hormone) is administered as an injection under the skin. There’s no pill form of human growth hormone available by prescription. Some websites sell a pill form of human growth hormone, claiming that it produces results similar to the injected form of the drug.
However, there’s no proof that these claims are true. These dietary supplements are sometimes called human growth hormone releasers. There’s also no proof that homeopathic remedies claiming to contain human growth hormone work.
If you have specific concerns about aging, ask your doctor about proven ways to improve your health. Remember, healthy lifestyle choices — such as eating a healthy diet and including physical activity in your daily routine — can help you feel your best as you get older.
Human growth hormone injections
Somatropin injection is a man-made version of human growth hormone (HGH). Growth hormone is naturally produced by the pituitary gland and is necessary to stimulate growth in children. Man-made growth hormone may be used in adults or children who have certain conditions that prevent normal growth. These conditions include growth failure caused by growth hormone deficiency (inability to produce enough growth hormone), chronic kidney disease, idiopathic short stature (unexplained shortness) or short stature due to Noonan syndrome, Turner syndrome, Prader-Willi syndrome, short stature at birth with no catch-up growth, and other causes.
Somatropin injection is also used together with a proper diet to treat short bowel syndrome (SBS), which is a condition that prevents the intestine or gut from absorbing food properly. And somatropin is also used in adults to prevent severe weight loss related to AIDS.
Somatropin injection is available only with your doctor’s prescription. Somatropin injection is available as powder for solution.
Before using human growth hormone injections
Important Information
You should not use somatropin if you have cancer, diabetic retinopathy, or if you are being treated for Prader-Willi syndrome and you are overweight or have severe breathing problems. You should not use somatropin if you have a serious illness due to lung failure or complications from recent surgery, injury, or medical trauma.
Before using human growth hormone injection
You should NOT use somatropin if you are allergic to somatropin or benzyl alcohol, or if you have:
- a serious illness due to lung failure, or complications from recent surgery, injury, or medical trauma;
- active cancer;
- eye problems caused by diabetes (diabetic retinopathy); or
- you are being treated for Prader-Willi syndrome and you are overweight or have severe breathing problems (including sleep apnea).
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Brain tumor
- Cancer
- Childhood brain cancer and radiation treatment
- Closed epiphyses (normal bone growth stopped) in children or
- Diabetic retinopathy (eye condition) or
- Prader-Willi syndrome (a genetic disorder), if severely overweight or have severe breathing problems or
- Severe illness after surgery or major medical emergency (e.g., open heart surgery, abdominal surgery, accidental trauma, or respiratory failure)—Should not be used in patients with these conditions.
- Cancer, history of or
- Fluid retention, history of or
- Hypopituitarism (pituitary gland produces low hormone levels) or
- Hypothyroidism (underactive thyroid gland) or
- Otitis media (ear infection) in children, history of or
- Pancreatitis (inflammation or swelling of the pancreas) or
- Scoliosis (abnormally curved spine)—Use with caution. May make these conditions worse.
- Diabetes, or a family history of—Use with caution. May prevent insulin from working properly. .
- Kidney disease—Use with caution. The effects may be increased because of slower removal of the medicine from the body.
- Turner syndrome—May increase risk of having thyroid and hearing problems.
In some cases, human growth hormone injection should not be used in a child. Certain brands of somatropin contain an ingredient that can cause serious side effects or death in very young infants or premature babies. Do not give this medicine to a child without medical advice.
Some brands of somatropin are not expected to harm an unborn baby, including Genotropin, Omnitrope, Saizen, and Serostim.
It is not known whether certain other brands of somatropin will harm an unborn baby, including Humatrope, Norditropin, Nutropin, Zomacton, and Zorbtive.
Tell your doctor if you are pregnant or plan to become pregnant.
It may not be safe to breast-feed a baby while you are using this medicine. Ask your doctor about any risks.
Somatropin may contain an ingredient that can cause serious side effects or death in very young or premature babies. Do not give this medicine to a child without medical advice.
Human growth hormone injection precautions
It is very important that your doctor check you or your child at regular visits for any problems or unwanted effects that may be caused by this medicine.
This medicine may cause a serious allergic reaction that requires immediate medical attention. Tell your doctor right away if you or your child have a rash, itching, swelling of the face, tongue, or throat, trouble with breathing, or chest pain after you get the injection.
This medicine may cause a dislocation in the hip bone, especially in patients with growth hormone deficiency or Turner syndrome. Check with your doctor right away if you or your child has a limp or pain in the hip or knee.
Pancreatitis (an inflamed pancreas) may occur while you are using this medicine. Check with your doctor right away if you or your child are having more than one of these symptoms: bloating, chills, constipation, darkened urine, fast heartbeat, fever, indigestion, loss of appetite, nausea, pains in stomach, side, or abdomen possibly radiating to the back, vomiting, or yellow eyes or skin.
This medicine may affect blood sugar levels. Check with your doctor if you or your child notice a change in the results of your blood or urine sugar tests or if you have any questions.
This medicine may cause an increased pressure in the head. Check with your doctor immediately if headache, nausea, vomiting, blurred vision, or any other change in vision occurs during treatment. Your doctor may want you or your child to have your eyes checked by an ophthalmologist (eye doctor).
This medicine may cause fluid retention (extra water in the body). Tell your doctor if you or your child have burning, numbness, pain, or tingling in all fingers except smallest finger; swelling of the hands and feet; or pain, swelling, or stiffness of the muscles. Your doctor may adjust your dose to reduce these side effects.
This medicine is usually mixed with Bacteriostatic Water for Injection. You should not use Bacteriostatic Water for Injection if you have had an allergic reaction to benzyl alcohol. If this is a concern, ask your doctor about other ways to mix this medicine.
How should I use human growth hormone injection?
Human growth hormone injection is given as a shot under your skin or into a muscle. Somatropin may sometimes be given at home to patients who do not need to be in the hospital. If you are using this medicine at home, your doctor will teach you how to prepare and inject the medicine. Be sure that you understand exactly how the medicine is prepared and injected.
If you are using this medicine to treat short bowel syndrome, carefully follow your doctor’s instructions about any special diet. Take all other medicines or supplements your doctor has prescribed as part of your combination treatment.
This medicine comes with a patient information insert. Read and follow the instructions in the insert carefully. Ask your doctor if you have any questions.
There are many different forms (e.g., vial, cartridge, injection device) available for this medicine. Make sure your doctor, nurse, or pharmacist instructs you on how to prepare and administer this medication. Also, read all instructions carefully to be sure you know how to use your device.
Each time you get your medicine, check to be sure you have received the proper device. Talk to your pharmacist if you have questions about the device that you were given.
You will be shown the body areas where this shot can be given. Use a different body area each time you give yourself a shot. Keep track of where you give each shot to make sure you rotate body areas. This will help prevent skin problems from the injections.
Use a new needle, unopened vial, or syringe each time you inject your medicine.
You might not use all of the medicine in each vial (glass container). Use each vial only one time. Do not save an open vial. If the medicine in the vial has changed color, or if you see particles in it, do not use it.
Use only the brand of this medicine that your doctor prescribed. Different brands may not work the same way.
Human growth hormone injection dosage
The dose of this medicine will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For injection dosage form:
- For treatment of growth hormone deficiency:
- Adults—Nutropin® or Nutropin AQ®:
- Non-weight based: At first, the usual dose is 0.15 to 0.3 milligrams (mg) injected under the skin once a day. Your doctor may adjust your dose if needed.
- Weight-based: Dose is based on body weight and must be determined by your doctor. At first, the usual dose is not more than 0.006 milligram (mg) per kilogram (kg) of body weight injected under the skin once a day. Your doctor may adjust your dose if needed. However, the dose is usually not more than 0.025 to 0.0125 mg per kg of body weight per day.
- Adults—Saizen®: Dose is based on body weight and must be determined by your doctor. At first, the usual dose is not more than 0.005 mg per kg of body weight injected under the skin once a day. Your doctor may adjust your dose if needed.
- Children—Nutropin® or Nutropin AQ®: Dose is based on body weight and must be determined by your doctor. The weekly dose is up to 0.3 to 0.7 mg per kg of body weight injected under the skin and divided into daily doses. Your doctor may adjust your dose if needed.
- Children—Saizen®: Dose is based on body weight and must be determined by your doctor. The usual dose is 0.06 mg per kg of body weight, given three times per week and injected under the skin or into a muscle. Your doctor may adjust your dose if needed.
- Adults—Nutropin® or Nutropin AQ®:
- For treatment of growth failure due to chronic kidney disease:
- Children—Dose is based on body weight and must be determined by your doctor. The weekly dose is up to 0.35 milligram (mg) per kilogram (kg) of body weight injected under the skin and divided into daily doses. Your doctor may adjust your dose if needed.
- For treatment of idiopathic short stature:
- Children—Dose is based on body weight and must be determined by your doctor. The weekly dose is up to 0.3 milligram (mg) per kilogram (kg) of body weight injected under the skin and divided into daily doses. Your doctor may adjust your dose if needed.
- For treatment of short bowel syndrome:
- Adults—Dose is based on body weight and must be determined by your doctor. At first, the usual dose is 0.1 milligram (mg) per kilogram (kg) of body weight injected under the skin once a day for 4 weeks. Your doctor may adjust your dose if needed.
- Children—Use and dose must be determined by your doctor.
- For treatment of short stature with Turner syndrome:
- Children—Dose is based on body weight and must be determined by your doctor. The weekly dose is up to 0.375 milligram (mg) per kilogram (kg) of body weight injected under the skin and divided into equal doses 3 to 7 times per week. Your doctor may adjust your dose if needed.
Human growth hormone injection side effects
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- abnormal or decreased touch sensation
- bleeding after defecation
- bleeding, blistering, burning, coldness, discoloration of the skin, feeling of pressure, hives, infection, inflammation, itching, lumps, numbness, pain, rash,
- redness, scarring, soreness, stinging, swelling, tenderness, tingling, ulceration, or warmth at the injection site
- bloating or swelling of the face, arms, hands, lower legs, or feet
- blood in the urine
- burning, crawling, itching, numbness, prickling, “pins and needles”, or tingling feelings
- changes in skin color
- cold flu-like symptoms
- cold hands and feet
- confusion
- constipation
- cough or hoarseness
- darkened urine
- decreased urination
- diarrhea
- difficult urination
- dizziness
- dry mouth
- fainting or loss of consciousness
- fast heartbeat
- fast or irregular breathing
- feeling unusually cold
- fever or chills
- full or bloated feeling
- general feeling of discomfort or illness
- headache
- increase in heart rate
- itching
- joint pain
- light-colored stools
- lightheadedness
- loss of appetite
- lower back or side pain
- muscle aching or cramping
- muscle pain or stiffness
- nausea
- pain
- pain, redness, or swelling in the arm or leg
- pains in the stomach, side, or abdomen, possibly radiating to the back
- pressure in the stomach
- rapid, shallow breathing
- rapid weight gain
- rectal bleeding
- runny nose
- shivering
- skin rash
- sneezing
- sore mouth or tongue
- sore throat
- stomach bloating, burning, cramping, or pain
- sudden decrease in the amount of urine
- sweating
- swelling of the abdominal or stomach area
- swelling of the eyes or eyelids
- swelling or puffiness of the face
- swollen joints
- thirst
- tightness in the chest and/or wheezing
- tingling of the hands or feet
- trouble with breathing
- trouble with sleeping
- uncomfortable swelling around the anus
- unpleasant breath odor
- unusual tiredness or weakness
- unusual weight gain or loss
- vomiting
- vomiting of blood
- white patches in the mouth, tongue, or throat
- wrinkled skin
- yellow eyes or skin
Less common
- bone or skeletal pain
- burning, numbness, pain, or tingling in all fingers except smallest finger
- chest pain
- depressed mood
- dry skin and hair
- feeling cold
- hair loss
- hoarseness or husky voice
- slowed heartbeat
- swelling of the ankles
Get emergency help immediately if any of the following symptoms of overdose occur:
Symptoms of Overdose
- anxiety
- blurred vision
- changes in vision
- cold sweats
- coma
- cool, pale skin
- decrease in the amount of urine
- depression
- excessive sweating
- extreme weakness
- flushed, dry skin
- frequent urination
- fruit-like breath odor
- increase in hands and feet size
- increased hunger
- increased thirst
- increased urination
- increased volume of pale, diluted urine
- nightmares
- noisy, rattling breathing
- pain in the arms or legs
- seizures
- shakiness
- shortness of breath
- slurred speech
- stop in menstruation
- swelling of the fingers or hands
- troubled breathing at rest
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- body aches or pain
- breast pain
- change in the color, amount, or odor of vaginal discharge
- congestion
- discoloration of the fingernails or toenails
- dryness or soreness of the throat
- excess air or gas in the stomach or intestines
- frequent urge to defecate
- increased sweating
- passing gas
- rash
- sneezing
- straining while passing stool
- stuffy nose
- tender, swollen glands in neck
- trouble with swallowing
- voice changes
Less common
- discouragement
- feeling sad or empty
- irritability
- lack of appetite
- loss of interest or pleasure
- sleeplessness
- tiredness
- trouble concentrating
- unable to sleep
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
References- Gunawardane K, Krarup Hansen T, Sandahl Christiansen J, et al. Normal Physiology of Growth Hormone in Adults. [Updated 2015 Nov 12]. In: De Groot LJ, Chrousos G, Dungan K, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279056
- Díez JJ, Sangiao-Alvarellos S, Cordido F. Treatment with Growth Hormone for Adults with Growth Hormone Deficiency Syndrome: Benefits and Risks. Int J Mol Sci. 2018;19(3):893. Published 2018 Mar 17. doi:10.3390/ijms19030893 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5877754/
- Murray PG, Clayton PE. Disorders of Growth Hormone in Childhood. [Updated 2016 Nov 16]. In: De Groot LJ, Chrousos G, Dungan K, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278971
- Herrington J, Carter-Su C. Signaling pathways activated by the growth hormone receptor. Trends Endocrinol Metab. 2001; 12:252.
- Mortensen AH, MacDonald JW, Ghosh D, Camper SA. Candidate genes for panhypopituitarism identified by gene expression profiling; Physiol Genomics. 2011; 43(19): 1105–1116.
- Murray PG, Higham CE, Clayton PE. The hypothalamo-growth hormone axis: the past 60 years. J Endocrinol. 2015 Jun 3. pii: JOE-15-0120
- Le Tissier PR, Carmignac DF, Lilley S, Sesay AK, et al. Hypothalamic Growth Hormone-Releasing Hormone (GHRH) Deficiency: Targeted Ablation of GHRH Neurons in Mice Using a Viral Ion Channel Transgene. Mol Endocrinol. 2005; 19(5):1251–1262.
- Kyriaki S. Alatzoglou, Mehul T. Dattani. Genetic causes and treatment of isolated growth hormone deficiency—an update. Nature Reviews Endocrinology. 2010; 6: 562-576.
- Patel YC. Somatostatin and its receptor family. Front Neuroendocrinol. 1999;20(3):157–198.
- Ren SG, et al. Functional association of somatostatin receptor subtypes 2 and 5 in inhibiting human growth hormone secretion. J Clin Endocrinol Metab 2003;88(9):4239–4245.
- Behringer RR, Lewin TM, Quaife CJ, et al. Expression of insulin-like growth factor I stimulates normal somatic growth in growth hormone-deficient transgenic mice. Endocrinology. 1990; 127:1033.
- Powell-Braxton L, Hollingshead P, Giltinan D, Pitts-Meek S, Stewart T. Inactivation of the IGF-I gene in mice results in perinatal lethality. Ann N Y Acad Sci. 1993;692:300–301.
- Woods KA, Camacho-Hu ¨bner C, Savage MO, Clark AJL. Intrauterine growth retardation and postnatal growth failure associated with deletion of the insulin-like growth factor I gene. N Engl J Med. 1996;335:1363–1367
- Lupu F, Terwilliger JD, Lee K, et al. Roles of growth hormone and insulin-like growth factor 1 in mouse postnatal growth. Dev Biol. 2001; 229:141.
- Burgers AM1, Biermasz NR,et al. Meta-analysis and dose-response metaregression: circulating insulin-like growth factor I (IGF-I) and mortality. J Clin Endocrinol Metab. 2011 Sep;96(9):2912-20.
- Bartke A1, Sun LY, Longo V. Somatotropic signaling: trade-offs between growth, reproductive development, and longevity. Physiol Rev. 2013 Apr;93(2):571-98
- Fontana L1, Partridge L, Longo VD. Extending healthy life span–from yeast to humans. Science. 2010 Apr 16;328(5976):321-6.
- Møller N1, Jørgensen JO. Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. Endocr Rev. 2009 Apr;30(2):152-77.
- Copinschi G, Wegienka LC, Hane S, Forsham PH. Effect of arginine on serum levels of insulin and growth hormone in obese subjects. Metabolism. 1967; 16: 485-491.
- Rudman D, Kutner MH, Rogers CM, Lubin MF, Fleming GA, Bain R. Impaired growth hormone secretion in the adult polupation. Relation to age and adiposity. J. Clin. Invest. 1981; 67: 1361-1369.
- Rudman D. Occasional hypothesis: growth hormone, body composition and ageing. J. AM Geriatr Soc. 1985; 33: 800-807.
- Jørgensen JOL, Vahl N, Hansen TB, Thuesen L, Hagen C, Christiansen JS. Growth hormone versus placebo treat- ment for one year in growth hormone deficient adults: increase in exercise capacity and normalisation of body composition. Clin. Endocrinol. 1996; 45: 681-688.
- Williams T, Berelowiz M, Joffe SN, Thorner MO, Rivier J, Vale W, Frohman LA. Impaired growth hormone re- sponse to growth hormone-releasing factor in obesity. A pituitary defect reversed with weight reduction. N. Engl. J. Med. 1984; 311: 1403-1407.
- Vahl N, Jørgensen JOL, Jurik AG, Christiansen JS. Abdominal adiposity and physical fitness are major depermi- nants of the age-associated decline in stimulated GH secretion in healthy adults. J. Clin. Endocrinol. Metab. 1996; 81: 2209-2215.
- Hataya Y, Akamizu T, Takaya K, et al. A low dose of ghrelin stimulates growth hormone (GH) release synergistically with GH-releasing hormone in humans. J Clin Endocrinol Metab. 2001; 86:4552.
- Vahl N, Jørgensen JOL, Skjaerbaek C, Veldhuis J, Ørskov H, Christiansen JS. Abdominal adiposity rather than age and sex predicts mass and regularity of GH secretion in healthy adults. Am J. Physiol. 1997; 272: E1108- E1116.
- Kiel DP, Puhl J, Rosen CJ, Berg K, Murphy JB, MacLean DB. Lack of an association between insulin-like growth factor I and body composition, muscle strength, physical performance or self-reported mobility among older persons with functional limitations. J Am Geriatr Soc. 1998; 46: 822-828.
- van der Lely A J, Tschop M, Heiman ML, Ghigo E. Biological, physiological, pathophysiological, and pharmaco- logical aspects of ghrelin. Endocr Rev. 2004;25:426-57
- Rudman D, Feller AG, Nagraj HS. Effects of human growth hormone in men over 60 years old. N Engl J Med. 1990; 323: 1-6.
- Møller J, Jørgensen JOL, Laursen T, Frystyk J, Naeraa R, Ørskov H, Christiansen JS. Growth hormone (GH) dose regimens in GH deficiency: effects on biochemical growth markers and metabolic parameters. Clin Endocrinol. 1993; 39: 403-408.
- Johannsson G, Rosén T, Lindstedt G, Bosaeus I, Bengtsson B-Å. Effects of 2 years of growth hormone treat- ment on body composition and cardiovascular risk factors in adults with growth hormone deficiency. Endocrinol Metab.1996;3(Suppl. A):3-12.
- Toogood AA, Shalet SM. Growth hormone replacement therapy in the elderly with hypothalamic-pituitary dis- ease: a dose-finding study. J Clin Endocrinol Metab. 1999; 84: 131-136.
- Burman P, Johansson AG, Siegbahn A, Vessby B, Karlsson FA. Growth hormone (GH) deficient men are more responsive to GH replacement therapy than women. J Clin Endocrinol Metab. 1997; 82: 550-555.
- Vahl N, Møller N, Lauritzen T, Christiansen JS, Jørgensen JOL. Metabolic effects and pharmacokinetics of a growth hormone pulse in healthy adults: relation to age, sex and body composition. J Clin Endocrinol Metab. 1997; 82: 3612-3618.
- Fisker S, Vahl N, Jørgensen JOL, Christiansen JS, Øskov H. Abdominal fat determines growth hormone binding protein levels in healthy non-obese adults. J Clin Endocrinol Metab. 1997; 82: 123-128.
- Rabinowitz D, Klassen GA , Zierler KL. Effects of human growth hormone on muscle and adipose tissue me- tabolism in the forearm of men. J Clin Invest. 1965; 44: 51-61.
- Glick SM, Roth J, Yalow RS, Berson SA. Immunoassay of human growth hormone in plasma. Nature. 1963; 199: 784-787.
- Hartman ML, Faria ACS, Vance ML, Johnson ML, Thorner MO, Veldhuis JD. Temoral structure of in vivo growth hormone secretory events in humans. Am J of Physiol. 1991; 250: E101-110.
- Gunawardane K, Krarup Hansen T, Sandahl Christiansen J, et al. Normal Physiology of Growth Hormone in Adults. [Updated 2015 Nov 12]. In: De Groot LJ, Chrousos G, Dungan K, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279056 https://www.ncbi.nlm.nih.gov/books/NBK279056/
- Møller N, Jørgensen JOL, Schmitz O, Møller J, Christiansen JS, Alberti KGMM, Ørskov H. Effects of a growth hor- mone pulse on total and forearm substrate fluxes in humans. Am. J Pshysiol. 1990: 258: E86-E91.
- Bak JF, Møller N, Schmitz O. Effects of growth hormone of fuel utilization and muscle glycogen synthase activi- ty in normal humans. Am J of Physiol. 1991; 260: E736-742.
- Ørskov L, Schmitz O, Jørgensen JOL, Arnfred J, Abildgaard N, Christiansen JS. Influence of growth hormone on glucose induced glucose uptake in healthy men as assessed by the hyperglycaemic clamp technique. J Clin En- docrinol Metab. 1989; 68: 276-282.
- Ikkos D, Luft R, Gemzell C-A, Olivecrona H. Effects of human growth hormone in hypophysectomised diabetic subjects. Lancet. 1958; i: 721-722.
- Henneman DH & Henneman PH. Effects of growth hormone on levels of blood and urinary carbohydrate and fat metabolites in man. J Clin Invest. 1960; 39: 1239-1245.
- Møller N, Schmitz O, Jørgensen JOL, Astrup J, Bak JF, Christensen SE et al. Basal and insulin stimulated sub- strate metabolism in patients with active acromegaly before and after adenomectomy. J Endocrinol Metab. 1992; 74: 1012-1019.
- Sönksen PH, Greenwood FS, Ellis JP, Lowy C, Rutherford A, Nabaaro JDN. Changes of carbohydrate tolerance in acromegaly with progress of the disease and in response to treatment. J Clin Endocrinol. 1967; 27: 1418-1430.
- Møller N, Jørgensen JOL, Ovesen P, Schmitz O, Alberti KGMM et al. Impact of 2 weeks growth hormone treat- ment on basal an insulin stimulated substrate metabolism in humans. Clin Endocrinol. 1993; 39: 577-581.
- Rudman D, Kutner MH, Rogers CM, Lubin MF, Fleming A, Bain R. Impaired growth hormone secretion in the adult populaiton. J Clin Invest. 1981; 67: 1361-1369.
- Growth hormone in the aging male. Best Pract Res Clin Endocrinol Metab. 2013;27(4):541-55. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3940699/
- Rudman D, Kutner MH, Rogers CM, et al. Impaired growth hormone secretion in the adult population: relation to age and adiposity. Journal of Clinical Investigation. 1981;67(5):1361–1369
- Iranmanesh A, Lizarralde G, Veldhuis JD. Age and relative adiposity are specific negative determinants of the frequency and amplitude of growth hormone (GH) secretory bursts and the half-life of endogenous GH in healthy men. Journal of Clinical Endocrinology and Metabolism. 1991;73(5):1081–1088.
- Giustina A, Veldhuis JD. Pathophysiology of the neuroregulation of growth hormone secretion in experimental animals and the human. Endocrine Reviews. 1998;19(6):717–797.
- Veldhuis JD, Liem AY, South S, et al. Differential impact of age, sex steroid hormones, and obesity on basal versus pulsatile growth hormone secretion in men as assessed in an ultrasensitive chemiluminescence assay. Journal of Clinical Endocrinology and Metabolism. 1995;80(11):3209–3222.
- Rudman D, Feller AG, Nagraj HS, et al. Effects of human growth hormone in men over 60 years old. New England Journal of Medicine. 1990;323(1):1–6.
- Abbasi AA, Drinka PJ, Mattson DE, et al. Low circulating levels of insulin-like growth factors and testosterone in chronically institutionalized elderly men. Journal of the American Geriatrics Society. 1993;41(9):975–982.
- Giannoulis MG, Sonksen PH, Umpleby M, et al. The effects of growth hormone and/or testosterone in healthy elderly men. Journal of Clinical Endocrinology and Metabolism. 2006;91(2):477–484.
- Blackman MR, Sorkin JD, Munzer T, et al. Growth hormone and sex steroid administration in healthy aged women and men: a randomized controlled trial. Journal of the American Medical Association. 2002;288(18):2282–2292
- Sattler F, Bhasin S, He J, et al. Testosterone threshold levels and lean tissue mass targets needed to enhance skeletal muscle strength and function: the HORMA trial. Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2011;66 (1):122–129
- Yarasheski KE, Campbell JA, Smith K, Rennie MJ, Holloszy JO, Bier DM. Effects of growth hormone and resis- tance exercise on muscle growth in young men. Am J Physiol. 1992; 262: E261-E267.
- Yarasheski KE, Zascwieja JJ, Campell JA, Bier DM. Effects of growth hormone and resistance exercise on mus- cle growth and strength in older men. Am J Physiol. 1995; 268: E268-E276.
- Taafe DR, Pruitt L, Reim J, Hintz RL, Butterfield G, Hoffman AR, Marcus R. Effects of recombinant human growth hormone on the muscle strength response to resistance exercise in elderly men. J Clin Endocrinol Metabt. 1994; 79: 1361-1366.
- Papadakis MA, Grady D, Black D, Tierny MJ, Gooding GAW, Schamblean M, Grunfeld C. Growth hormone re- placement in healthy older men improves body composition but not functional ability. Ann Intern Med. 1996; 124: 708-716.
- Waters D, Danska J, Hardy K, Koster F, Qualls C, Nickell D, Nightingale S, Gesundheit N, Watson D, Schade D. Recombinant human growth hormone, insulin-like growth factor I and combination therapy in AIDS-associated wasting. Ann Intern Med. 1996; 125: 865-872.
- Laron Z. Do deficiencies in growth hormone and insulin-like growth factor-1 (IGF-1) shorten or prolong longevity? Mechanisms of Ageing and Development. 2005;126(2):305–307
- Shevah O, Kornreich L, Galatzer A, et al. The intellectual capacity of patients with Laron syndrome (LS) differs with various molecular defects of the growth hormone receptor gene. Correlation with CNS abnormalities Hormone and Metabolic Research. 2005;37(12):757–760.
- Menezes Oliveira JL, Marques-Santos C, Barreto-Filho JA, et al. Lack of evidence of premature atherosclerosis in untreated severe isolated growth hormone (GH) deficiency due to a GH-releasing hormone receptor mutation. Journal of Clinical Endocrinology and Metabolism. 2006;91(6):2093–2099.
- Suh Y, Atzmon G, Cho MO, et al. Functionally significant IGF-1 receptor mutations in centenarians. Proceedings of the National Academy of Sciences U S A. 2008;105(9):3438–3442
- Guevara-Aguirre J, Balasubramanian P, Guevara-Aguirre M, et al. Growth hormone receptor deficiency is associated with a major reduction in pro-aging signaling, cancer, and diabetes in humans. Science Translational Medicine. 2011;3(70):70ra13
- Besson A, Salemi S, Gallati S, et al. Reduced longevity in untreated patients with isolated growth hormone deficiency. Journal of Clinical Endocrinology and Metabolism. 2003;88(8):3664–3667
- van Bunderen CC, van Nieuwpoort IC, Arwert LI, et al. Does growth hormone replacement therapy reduce mortality in adults with GH deficiency? Data from the Dutch National Registry of GF Treatment in adults. Journal of Clinical Endocrinology and Metabolism. 2011;96(10):3151–3159
- Brugts MP, van den Beld AW, Hofland LJ, et al. Low circulating insulin-like growth factor I bioactivity in elderly men is associated with increased mortality. Journal of Clinical Endocrinology and Metabolism. 2008;93(7):2515–2522.
- Meinhardt U, Nelson AE, Hansen JL, et al. The effects of growth hormone on body composition and physical performance in recreational athletes: a randomized trial. Annals of Internal Medicine. 2010;152(9):568–577
- Liu H, Bravata DM, Olkin I, et al. Systematic review: the effects of growth hormone on athletic performance. Annals of Internal Medicine. 2008;148(10):747–758.
- Liu H, Bravata DM, Olkin I, et al. Systematic review: the safety and efficacy of growth hormone in the healthy elderly. Annals of Internal Medicine. 2007;146(2):104–115.