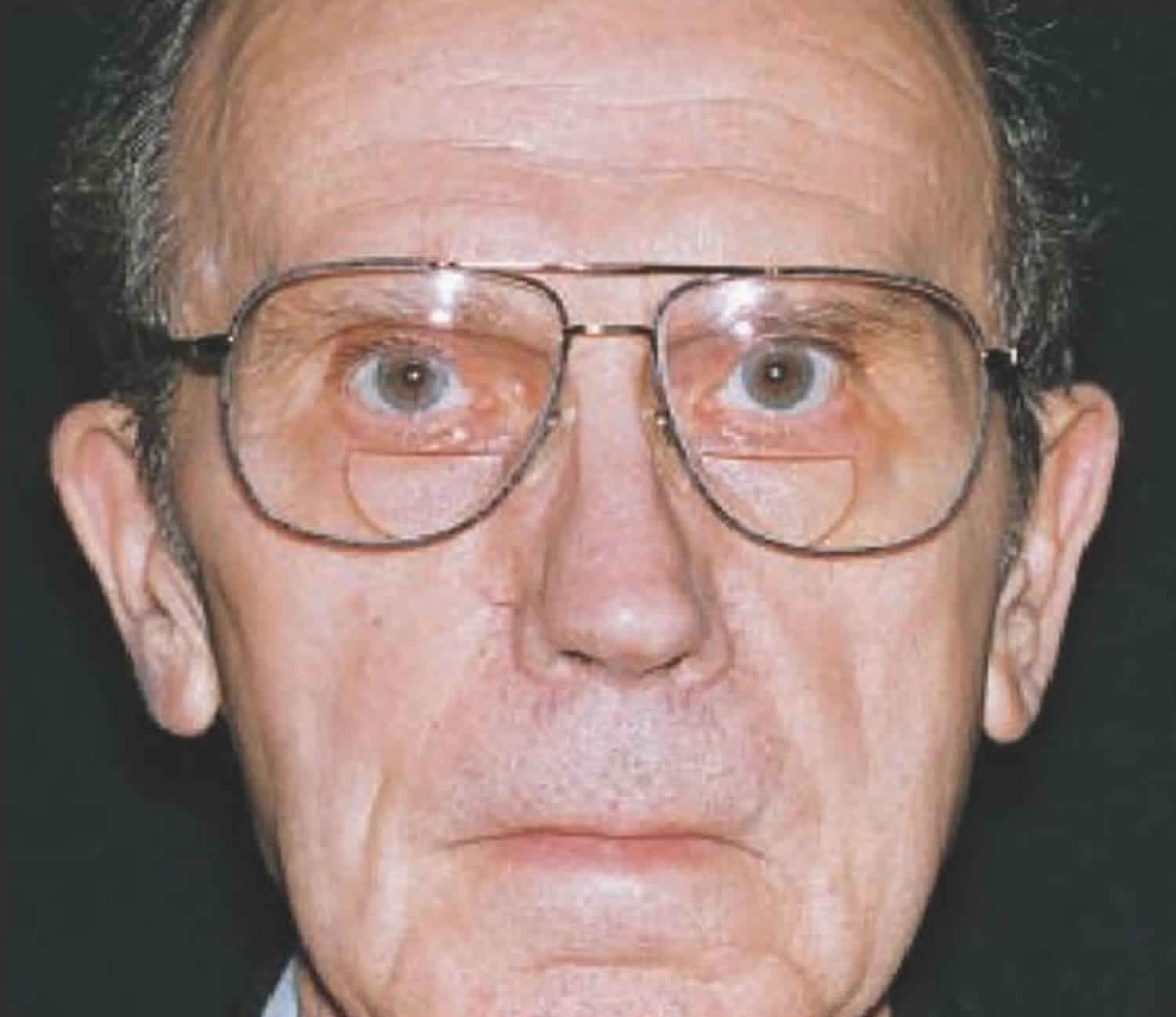
Hypomimia
Hypomimia also known as masked face or facial masking is a clinical term for the Parkinson’s disease symptom more commonly known as an immobile face with reduced blinking, results from the combination of bradykinesia and rigidity. Hypomimia is derived from the Greek word “hypo”, less, and “mimia”, imitation or expression.
When the muscles of your face are stiff or take longer to move, it can be hard to crack a smile, raise your eyebrows or otherwise express your feelings using your face, which is an important part of how people communicate. Combined with Parkinson disease speech changes, such as low voice volume, hypomimia or facial masking can make it hard for others to interpret your mood and intentions. People might assume you’re upset or depressed all the time, which can be frustrating if they constantly ask, “What’s wrong?” when you are feeling fine. On the other hand, if you are experiencing symptoms of depression, talk to your doctor. Mood changes are common in Parkinson’s disease, and treatable.
Hypomimia causes
Dopamine is a chemical messenger (neurotransmitter) that is primarily responsible for controlling movement, emotional responses and the ability to feel pleasure and pain. In people with Parkinson’s disease, the cells that make dopamine are impaired. As Parkinson’s disease progresses, more dopamine-producing brain cells die. Your brain eventually reaches a point where it stops producing dopamine in any significant amount. This causes increasing problems with movement.
Hypomimia symptoms
Hypomimia also known as masked face or facial masking is a clinical term for the Parkinson’s symptom more commonly known as an immobile face with reduced blinking, results from the combination of bradykinesia and rigidity.
Hypomimia treatment
Medications to treat movement symptoms should help with facial masking, as they alleviate rigidity.
Although there are general guidelines that doctors use to choose a treatment regimen, each person with Parkinson’s disease must be individually evaluated to determine which drug or combination of medications is best for them. For some, a “first choice” drug might be one of the levodopa preparations, and for others, an initial prescription may be given for one of the agonists, an MAO inhibitor or an anticholinergic.
The choice of medication treatment depends on many variables including symptoms present, other existing health issues (and the medications being used to treat them) and age. Dosages vary greatly depending on a person’s needs and metabolism.
Since most symptoms of Parkinson’s disease are caused by a lack of dopamine in the brain, many Parkinson’s disease drugs are aimed at either temporarily replenishing dopamine or mimicking the action of dopamine. These types of drugs are called dopaminergic medications. They generally help reduce muscle rigidity, improve speed and coordination of movement and lessen tremor.
Always remember that medication is only part of the overall treatment plan for combatting Parkinson’s disease. Learn more about the available medications, but don’t forget exercise and complementary therapies.
It is also a good idea to ask your doctor for a referral to a speech-language pathologist. He or she can teach you facial exercises that may help with masking, as well as other issues you may be having, including speech and swallowing problems.
Finally, if you are having more frequent cases of people misinterpreting your mood or not believing you when you say how you are doing, try explaining the difficulty with muscle control and expression. This may help people to better understand how you are feeling, and also increase their awareness of Parkinson’s disease.
Healthy eating
While no food or combination of foods has been proved to help in Parkinson’s disease, some foods may help ease some of the symptoms. For example, eating foods high in fiber and drinking an adequate amount of fluids can help prevent constipation that is common in Parkinson’s disease.
A balanced diet also provides nutrients, such as omega-3 fatty acids, that might be beneficial for people with Parkinson’s disease.
Exercise
Exercising may increase your muscle strength, flexibility and balance. Exercise can also improve your well-being and reduce depression or anxiety.
Your doctor may suggest you work with a physical therapist to learn an exercise program that works for you. You may also try exercises such as walking, swimming, gardening, dancing, water aerobics or stretching.
Parkinson’s disease can disturb your sense of balance, making it difficult to walk with a normal gait. Exercise may improve your balance. These suggestions may also help:
- Try not to move too quickly.
- Aim for your heel to strike the floor first when you’re walking.
- If you notice yourself shuffling, stop and check your posture. It’s best to stand up straight.
- Look in front of you, not directly down, while walking.
Alternative medicine
Supportive therapies can help ease some of the symptoms and complications of Parkinson’s disease, such as pain, fatigue and depression. When performed in combination with your treatments, these therapies might improve your quality of life:
- Massage. Massage therapy can reduce muscle tension and promote relaxation. This therapy, however, is rarely covered by health insurance.
- Tai chi. An ancient form of Chinese exercise, tai chi employs slow, flowing motions that may improve flexibility, balance and muscle strength. Tai chi may also prevent falls. Several forms of tai chi are tailored for people of any age or physical condition. A study showed tai chi may improve the balance of people with mild to moderate Parkinson’s disease more than stretching and resistance training.
- Yoga. In yoga, gentle stretching movements and poses may increase your flexibility and balance. You may modify most poses to fit your physical abilities.
- Alexander technique. Alexander technique— which focuses on muscle posture, balance and thinking about how you use muscles — may reduce muscle tension and pain.
- Meditation. In meditation, you quietly reflect and focus your mind on an idea or image. Meditation may reduce stress and pain and improve your sense of well-being.
- Pet therapy. Having a dog or cat may increase your flexibility and movement and improve your emotional health.
Medications
Medications may help you manage problems with walking, movement and tremor. These medications increase or substitute for dopamine.
People with Parkinson’s disease have low brain dopamine concentrations. However, dopamine can’t be given directly, as it can’t enter your brain.
You may have significant improvement of your symptoms after beginning Parkinson’s disease treatment. Over time, however, the benefits of drugs frequently diminish or become less consistent. You can usually still control your symptoms fairly well.
Medications your doctor may prescribe include:
- Carbidopa-levodopa. Levodopa, the most effective Parkinson’s disease medication, is a natural chemical that passes into your brain and is converted to dopamine. Levodopa is combined with carbidopa (Lodosyn), which protects levodopa from early conversion to dopamine outside your brain. This prevents or lessens side effects such as nausea. Side effects may include nausea or lightheadedness (orthostatic hypotension). After years, as your disease progresses, the benefit from levodopa may become less stable, with a tendency to wax and wane (“wearing off”). Also, you may experience involuntary movements (dyskinesia) after taking higher doses of levodopa. Your doctor may lessen your dose or adjust the times of your doses to control these effects.
- Carbidopa-levodopa infusion. Duopa is a brand-name medication made up of carbidopa and levodopa. However, it’s administered through a feeding tube that delivers the medication in a gel form directly to the small intestine. Duopa is for patients with more-advanced Parkinson’s who still respond to carbidopa-levodopa, but who have a lot of fluctuations in their response. Because Duopa is continually infused, blood levels of the two drugs remain constant. Placement of the tube requires a small surgical procedure. Risks associated with having the tube include the tube falling out or infections at the infusion site.
- Dopamine agonists. Unlike levodopa, dopamine agonists don’t change into dopamine. Instead, they mimic dopamine effects in your brain. They aren’t as effective as levodopa in treating your symptoms. However, they last longer and may be used with levodopa to smooth the sometimes off-and-on effect of levodopa. Dopamine agonists include pramipexole (Mirapex), ropinirole (Requip) and rotigotine (Neupro, given as a patch). Apomorphine (Apokyn), is a short-acting injectable dopamine agonist used for quick relief. Some of the side effects of dopamine agonists are similar to the side effects of carbidopa-levodopa. But they can also include hallucinations, sleepiness and compulsive behaviors such as hypersexuality, gambling and eating. If you’re taking these medications and you behave in a way that’s out of character for you, talk to your doctor.
- MAO B inhibitors. These medications include selegiline (Eldepryl, Zelapar), rasagiline (Azilect) and safinamide (Xadago). They help prevent the breakdown of brain dopamine by inhibiting the brain enzyme monoamine oxidase B (MAO B). This enzyme metabolizes brain dopamine. Side effects may include nausea or insomnia. When added to carbidopa-levodopa, these medications increase the risk of hallucinations. These medications are not often used in combination with most antidepressants or certain narcotics due to potentially serious but rare reactions. Check with your doctor before taking any additional medications with an MAO B inhibitor.
- Catechol O-methyltransferase (COMT) inhibitors. Entacapone (Comtan) is the primary medication from this class. This medication mildly prolongs the effect of levodopa therapy by blocking an enzyme that breaks down dopamine. Side effects, including an increased risk of involuntary movements (dyskinesia), mainly result from an enhanced levodopa effect. Other side effects include diarrhea or other enhanced levodopa side effects.
- Tolcapone (Tasmar) is another COMT inhibitor that is rarely prescribed due to a risk of serious liver damage and liver failure.
- Anticholinergics. These medications were used for many years to help control the tremor associated with Parkinson’s disease. Several anticholinergic medications are available, including benztropine (Cogentin) or trihexyphenidyl. However, their modest benefits are often offset by side effects such as impaired memory, confusion, hallucinations, constipation, dry mouth and impaired urination.
- Amantadine. Doctors may prescribe amantadine alone to provide short-term relief of symptoms of mild, early-stage Parkinson’s disease. It may also be given with carbidopa-levodopa therapy during the later stages of Parkinson’s disease to control involuntary movements (dyskinesia) induced by carbidopa-levodopa. Side effects may include a purple mottling of the skin, ankle swelling or hallucinations.
Surgical procedures
Surgical treatment is reserved for Parkinson’s disease patients who have exhausted medical treatment of Parkinson’s disease tremor or who suffer profound motor fluctuations (wearing off and dyskinesias).
Currently, there are two surgical treatments available for people living with Parkinson’s disease — deep brain stimulation (DBS) or surgery performed to insert a tube in the small intestine, which delivers a gel formulation of carbidopa/levodopa (Duopa).
Deep brain stimulation
In deep brain stimulation (DBS), surgeons implant electrodes into a specific part of your brain. The electrodes are connected to a generator implanted in your chest near your collarbone that sends electrical pulses to your brain and may reduce your Parkinson’s disease symptoms.
Your doctor may adjust your settings as necessary to treat your condition. Surgery involves risks, including infections, stroke or brain hemorrhage. Some people experience problems with the deep brain stimulation system or have complications due to stimulation, and your doctor may need to adjust or replace some parts of the system.
Deep brain stimulation is most often offered to people with advanced Parkinson’s disease who have unstable medication (levodopa) responses. deep brain stimulation can stabilize medication fluctuations, reduce or halt involuntary movements (dyskinesia), reduce tremor, reduce rigidity, and improve slowing of movement.
deep brain stimulation is effective in controlling erratic and fluctuating responses to levodopa or for controlling dyskinesia that doesn’t improve with medication adjustments.
However, deep brain stimulation isn’t helpful for problems that don’t respond to levodopa therapy apart from tremor. A tremor may be controlled by deep brain stimulation even if the tremor isn’t very responsive to levodopa.
Although deep brain stimulation may provide sustained benefit for Parkinson’s symptoms, it doesn’t keep Parkinson’s disease from progressing.