Incarcerated uterus
Incarcerated uterus also known as trapped pregnant uterus, refers to the entrapment of the uterus in the pelvic cavity behind the sacral promontory 1. Incarcerated uterus is uncommon and is said to occur in 1 in 3,000 pregnancies 2. Uncomplicated incarcerated uterus may be seen in as many as 9% of the pregnancies. Early diagnosis and treatment are critical to optimize pregnancy outcomes. Management becomes more difficult as pregnancy progresses due to increased maternal and fetal risks. In view of the lack of specific signs or symptoms, additional physical and imaging examinations are critical to early diagnosis of incarcerated uterus. Appropriate treatment measures that are tailored to the different gestation weeks may improve pregnancy outcomes.
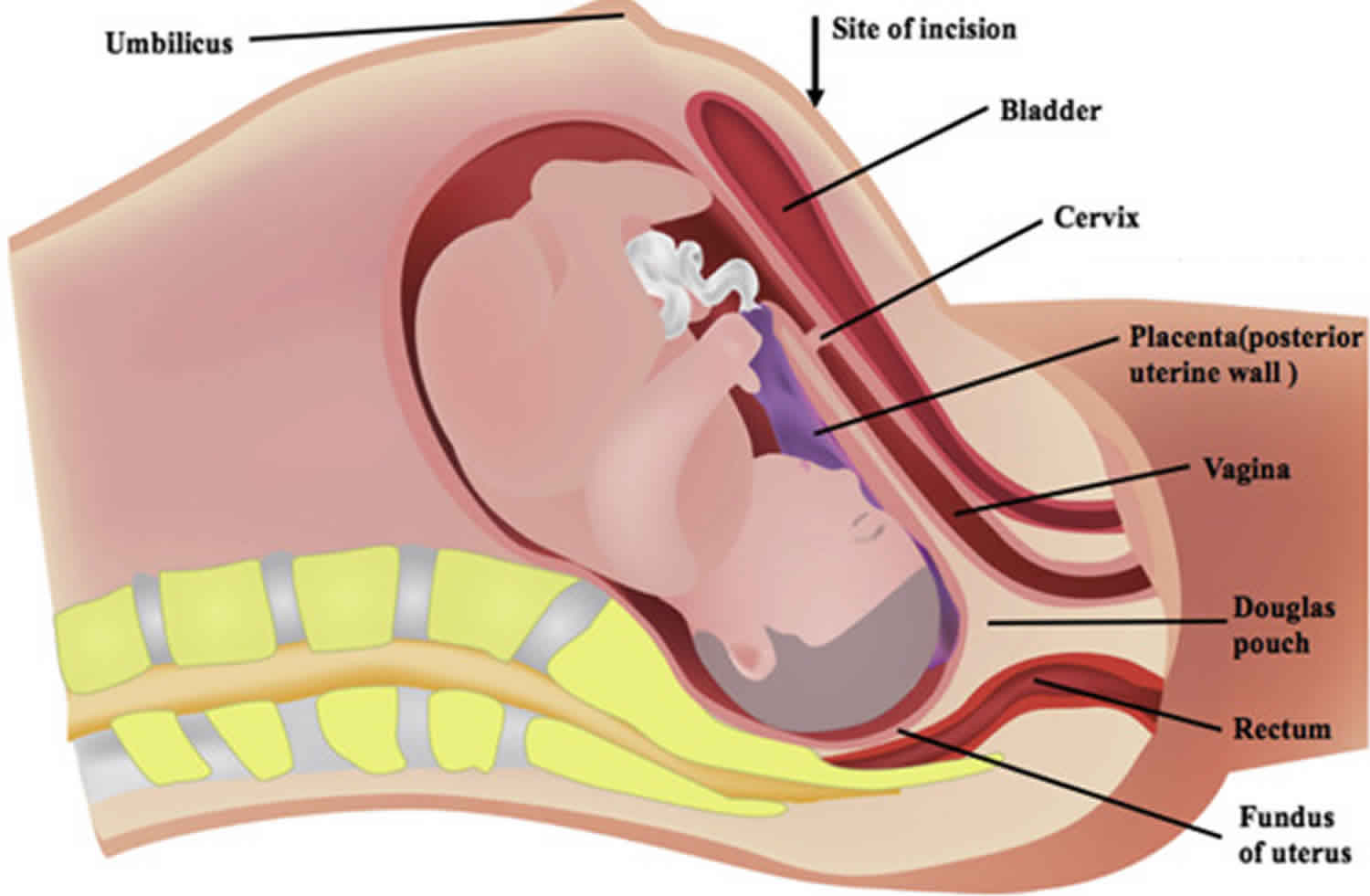
Early pregnancy management is nonsurgical and includes knee to chest maneuvers or manual reduction through the vagina or rectum. Colonoscopic reduction has been described. When less invasive options fail, surgical reduction may be required. If the pregnancy has progressed to term, cesarean delivery is recommended. Obstetric complications include preterm labor, premature rupture of membranes, labor dystocia, spontaneous abortion, and intrauterine fetal demise. At the time of cesarean delivery, failure to recognize uterine incarceration may result in inadvertent injury to the vagina, cervix, or bladder. Non-obstetric complications include venous stasis secondary to compression, hypertension, edema, and increased risk of venous thromboembolism and pulmonary embolus. Urinary obstruction is a frequent finding and may require urologic consult and intervention.
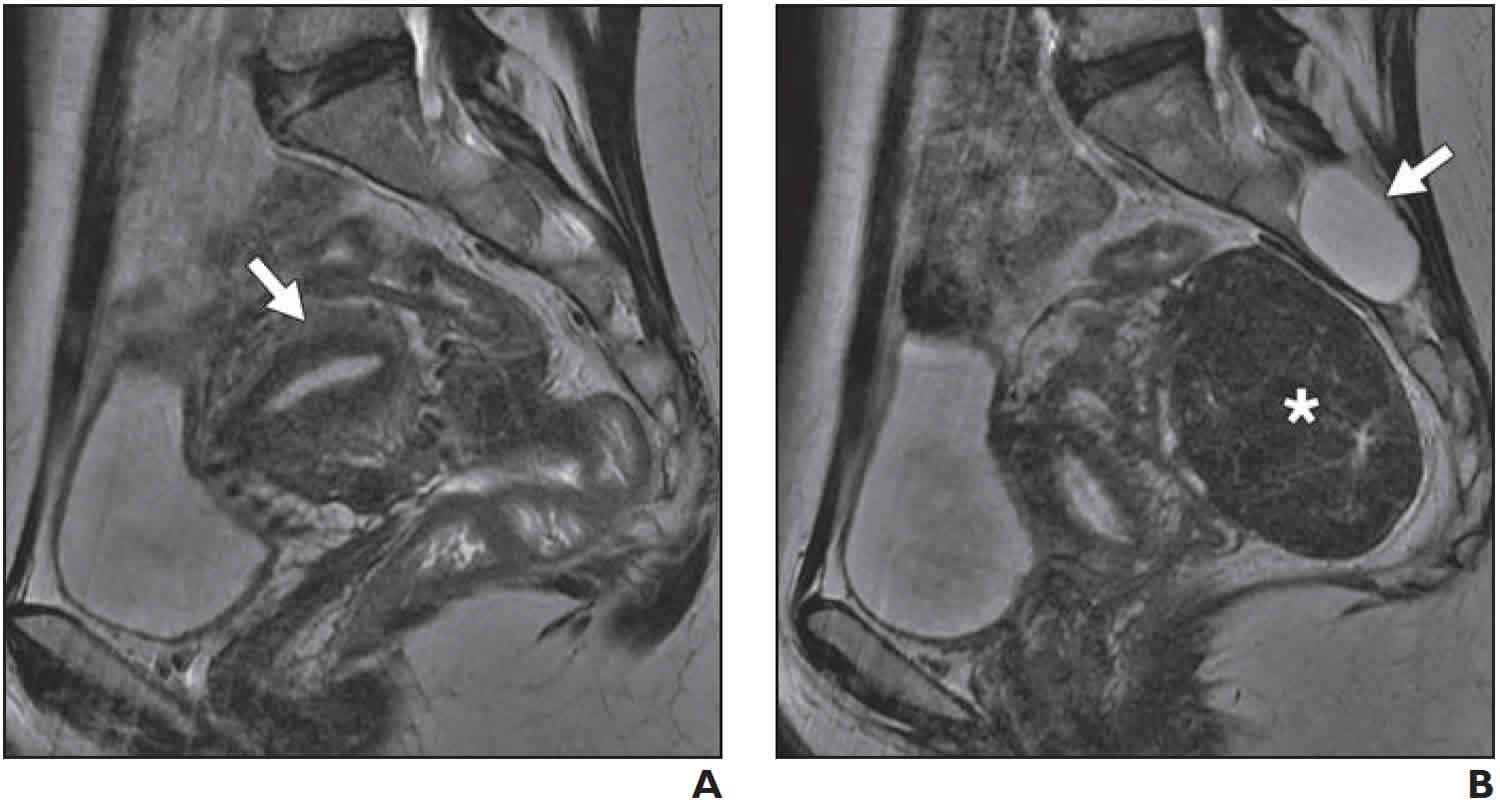
Figure 1. Uterine incarceration MRI
Footnote: 45-year-old woman with history of pelvic pain and previous uterine incarceration. (A) Sagittal T2-weighted fast spin-echo MR image shows retropositioned uterus (arrow). (B) Sagittal T2-weighted fast spin-echo MR image shows large posterior fibroid (asterisk). Patient underwent prophylactic myomectomy to decrease chance of recurrent uterine incarceration in future pregnancies. Incidental finding of Tarlov cyst (arrow) is noted.
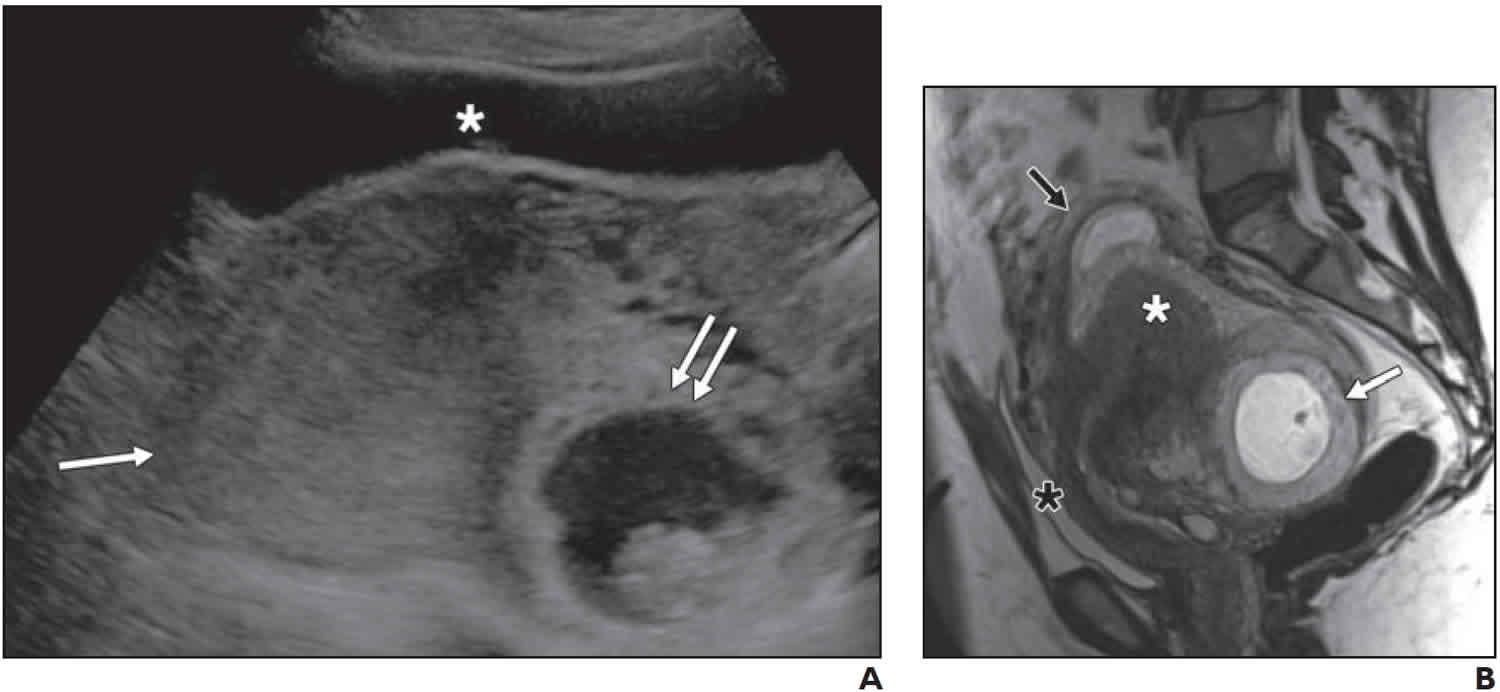
[Source 3 ]Figure 2. Incarcerated uterus ultrasound
Footnote: 40-year-old woman at 10 weeks’ gestational age who presented with pelvic pain. (A) Longitudinal gray-scale transabdominal ultrasound image shows anteriorly located compressed and elongated bladder (asterisk), retropositioned uterus (single arrow), and gestational sac (double arrows) located deep in pelvis. Cervix could not be identified. Because of concern for possible ectopic pregnancy or incarcerated uterus, MRI was performed. (B) Sagittal T2-weighted HASTE MR image shows retropositioned uterus (black arrow), anterior and superior displacement of bladder (black asterisk), and interstitial ectopic pregnancy (white arrow) located in deep pelvis, which was cause of incarcerated uterus diagnosed at surgery. Incidental finding of focal adenomyosis (white asterisk) is noted.
[Source 3 ]Incarcerated uterus causes
Incarcerated uterus or gravid uterine incarceration has no clearly identifiable causes, but is strongly correlated to malposition of the nonpregnant uterus, which is typically retroversion 1. In most cases, the gravid uterus transforms from a pelvic organ to an abdominal organ and the retroverted uterus corrects itself as the fundus rising out of the pelvis between 12 and 14 weeks of gestation and spontaneously falling forward to its normal anatomical position. On rare occasions, the uterus remains in a retroverted position and is trapped in the pelvic cavity. Multiple factors have been identified to prevent the uterus from entering the abdominal cavity, including tumor, uterine malformation, pelvic adhesions secondary to abdominal surgery, inflammation in the pelvis, and endometriosis. Among the 136 patients reviewed, 3 patients had uterine anomalies [didelphic uterus 2 4 and bicornuate uterus 1 5]; 1 had abdominal surgery and presented with serious pelvic adhesion 6; 1 had a deep sacral concavity 7; and 1 had a history of cystitis 8. Two patients reported no special history 9 and the risk information was not available for 2 patients 10. Uterine prolapse, deep sacral concavity, and uterine fibroids are also identified as significant risk factors for a gravid uterus to develop incarceration 11. It is noteworthy that there were 10 cases of recurrent incarceration 1. It appears that pregnant women who had experienced incarceration, especially those with known risk factors discussed above are likely to develop recurrent incarceration during the subsequent gestation.
Eight patients became pregnant through assisted reproductive treatment (ART) 12 and carried significant risk factors for incarceration. There is no definitive report that associates incarceration in pregnant women with assisted reproductive treatment (ART), but common risk factors associated with incarceration, such as endometriosis or pelvic inflammatory diseases, have also been identified for infertility. Gravid uterine incarceration should therefore be considered if a pregnant woman through assisted reproductive treatment (ART) develops abdominal pain and vaginal bleeding. Since woman with assisted reproductive treatment (ART) often receive more extensive monitoring during their pregnancies, gravid uterine incarceration may be diagnosed early and a timely manner, leading to fewer complications. In fact, 7 patients in sporadic case reports who successfully delivered infants because of prompt diagnosis through pelvic examination and abdominal imaging. Patient with a history of lymphatic tuberculosis that could result in pelvic adhesion and bilateral tubal blockage, both of which could contribute to the development of uterine incarceration.
Incarcerated uterus symptoms
Among the 162 reviewed cases, gravid uterine incarceration is mostly diagnosed in the second trimester 1. The symptoms of gravid uterine incarceration vary, but include urinary manifestations (53.70%, urinary retention, frequent urination, dysuria, urgency and paradoxical incontinence), abdominal pain (35.80%), constipation (6.79%), vaginal bleeding (6.17%), pelvic pain (6.79%), back pain (4.94%), tenesmus (1.85%), perineal pain (0.62%), and large painful mass prolapsed outside the anus (0.62%). Fourteen patients (8.64%) are asymptomatic, but also have delivered viable infants in the end, indicating that asymptomatic patients may better outcomes of pregnancy compared to those with severely symptomatic. Clinical complications usually occur after twelve weeks of gestation and are mostly related to the pressure from anatomical structures adjacent to the entrapped uterus, including lower abdominal and pelvic pain, dysuria, urinary frequency, urinary retention, overflow incontinence, rectal pressure, and worsening constipation 13. Among these, urinary retention is the most common symptom that occurs because of elongation of the urethra by displacement of the cervix, loss of the urethrovesical angle, and mechanical compression of the bladder neck. If an incarcerated uterus is not diagnosed and treated promptly, we speculate that bladder rupture, renal failure, spontaneous abortion, intra-uterine growth retardation, prematurity and premature rupture of the membranes, or even uterine sacculation or rupture may happen frequently.
Incarcerated uterus complications
Complications of incarcerated uterus, which can be serious and potentially devastating, depend on the time of diagnosis and most can be prevented with early diagnosis 3. The possibility of or concern for uterine incarceration must be conveyed to alert the obstetrician about the altered anatomy and avoid potential complications. The type of complication associated with incarcerated uterus varies with stage of pregnancy (Table 1).
Table 1. Complications of uterine incarceration
| Stage of Pregnancy | Complication |
| First trimester | Acute urinary retention, rectal pressure, tenesmus, miscarriage |
| Second and third trimesters | Fetal death, uterine rupture, bladder rupture, uterine ischemia, intrauterine growth retardation, premature labor and delivery, renal failure, sepsis |
| Delivery | Vaginal, cervical, or bladder injury |
| Postpartum | Venous thrombosis, pulmonary embolism |
| Future pregnancy | Increased risk of recurrent uterine incarceration |
In the first trimester, the most commonly reported complication is acute urinary retention 14. Bladder catheterization relieved acute urinary retention. Symptoms of lower abdominal pain, urinary frequency,
urgency, and a sensation of incomplete emptying are a result of impingement of the bladder trigone by the anteriorly displaced cervix 15. Constipation, rectal pressure, and tenesmus also may first manifest in the first trimester as the uterine body becomes wedged in the hollow of the sacrum and presses against the rectum 16. Miscarriage associated with incarcerated uterus has also been reported in the late first trimester 15. Patient presented with uncontrollable abdominal pain and underwent surgical myomectomy for pain relief but subsequently had a spontaneous abortion 1 day after myomectomy.
In the second and third trimesters, intrauterine fetal death, uterine ischemia, intrauterine growth retardation, premature labor and delivery, renal failure, and sepsis have been reported 17. In a small series of
nine patients, Gibbons and Paley 16 reported a fetal mortality rate of 33%. In a recent series of eight patients with incarcerated uterus, one pregnancy was complicated by chorioamnionitis, which led to premature delivery and neonatal mortality 17. Uterine rupture and bladder rupture during the second and third trimesters are usually reported as a result of attempted manual repositioning of the incarcerated uterus 18.
During delivery, which usually requires cesarean delivery, inadvertent vaginal, cervical, or bladder injury can occur because of the anterosuperior positioning of these organs with an incarcerated uterus 19. A cesarean delivery performed using a traditional horizontal incision can lead to iatrogenic vaginal injury, bladder injury, and even accidental cervical hysterectomy if there is an iatrogenic cervical transection 20. Investigators have suggested that a vertical skin incision should be performed for cesarean delivery instead to expand the field of view and reach the most cranial uterine pole to avoid accidental transection of the bladder, cervix, or vagina 20.
In the postpartum period, patients are at risk for pulmonary embolism, which is related to venous thrombosis in the pelvic veins secondary to chronic compression by the incarcerated uterus 21.
Patients with a history of uterine incarceration are at risk for recurrence with subsequent pregnancies. MRI can help to identify the cause of uterine incarceration or predisposing risk factors. For example, in a patient with a history of uterine incarceration, MRI (Figure 1) showed a large posterior fundal fibroid that predisposes her to recurrent uterine incarceration with future pregnancies 22. Recurrent uterine incarceration may be prevented by early surveillance and early manipulation of the retropositioned gravid uterus. Repositioning of a retroverted uterus is most likely to be successful in early pregnancy 23.
Incarcerated uterus diagnosis
Diagnosis of uterine incarceration remains difficult because its symptoms are often non-specific and absent in early pregnancy 10. It is worth noting that in case reports, all diagnoses were made by clinical suspicion alone before 1969, but after 1974, especially after 2000, an increasing number of cases benefited from pelvic examination combined with imaging methods based on suspected symptoms. This could be explained by advances in imaging technology in recent years, which also indicated that ultrasound scanning or MRI facilitated early recognition and appropriate treatment of uterine incarceration.
In general, the features of pelvic examination can be described as follows. The cervix is anteriorly transfixed behind the pubic symphysis, making it difficult to expose. Additionally, sacculation of the posterior wall of the vagina and posterior fornix bulge may be observed, and the fundus is palpable within the curvature of the sacrum and could not be moved. Ultrasound examination could confirm incarceration. Abdominal sonography shows an advantage over transvaginal sonography in exhibiting the position of the cervix and its internal ostium and in determining the relationships between vagina, uterus and bladder, when the cervix is elongated and wedged behind the symphysis 11. MRI is superior to ultrasound in the detailed scanning of gravid uterus incarceration 24. It is suggested that every pregnant woman with an incarceration of the uterus should have MRI 25. However, if the diagnosis is not suspected, the imaging findings can be misinterpreted as an intraperitoneal pregnancy, placenta previa or incorrect fetal presentation 26. For some women, bloody vaginal discharge occurred at 15 weeks and 2 days of gestation, and urinary retention followed in the 16th week gestation.
Incarcerated uterus treatment
No single treatment can be deemed more successful than the others for gravid uterus incarceration. Most obstetricians tend to replace the uterus in its natural position as soon as possible after diagnosis 11. According to the gestational age, various management options may be considered. When incarceration of the retroverted gravid uterus is diagnosed in the late early trimester or early second trimester, obstetricians should fully evaluate the possibility of turning the uterus to a normal position. A passive reduction from a repeated knee-chest position after emptying the bladder can be recommended before 14 weeks of gestation. Between 14 and 20 weeks, the patient can also attempt a knee-chest position. If this method is unsuccessful, manual manipulation can be attempted. It is recommended to do this maneuver before 20 weeks of gestation, for more complications such as preterm labor may be caused by manual manipulation later than 20th week of gestation 27. All maneuvers should only be performed after the bladder and bowel have been emptied, to reduce the risk of rupture of the bladder, bowel or uterus 28. Additionally, pessary may be helpful after repositioning 29. Colonoscopic insufflation of the rectosigmoid at a gestational age of 13–15 weeks helped the reposition of the incarcerated uterus, which was reported by Seubert et al. 30. It has been reported that the epidural anesthesia is an effective way to manage reduction of an incarcerated uterus 31. In a literature review, six cases ended in a normal pregnancy after reposition under anesthesia 32. Anesthesia may increase the chance of a successful reduction because the uterus was easily released under anesthesia. If all interventions fail, laparoscopy or laparotomy is usually performed 33. Operative procedures are not appropriate for patients with uterine incarceration, which is diagnosed before 20 weeks of gestation, because they can result in abortion or preterm delivery; furthermore, following such procedures, close follow-up is needed during the remainder of pregnancy. In the third trimester, uterine contractions usually fail to dilate the cervix because of incarceration. As a result, the risk of uterine rupture should be considered 34. Caesarean section should be planned if reduction cannot be performed during the remainder of pregnancy 35.
In 162 reviewed cases, cases of incarceration recognized in the first or second trimester of pregnancy account for 67.28% (109/162). Treatment of reposition was successfully attempted in 83 cases. After reposition, 68 patients successfully delivered infants 1, including 36 term deliveries 36, and information for other cases was not available. Treatment methods vary in invasiveness, and because incarceration was quite rare, no study has yet been performed to determine the supremacy of any single treatment modality.
References- Han C, Wang C, Han L, et al. Incarceration of the gravid uterus: a case report and literature review. BMC Pregnancy Childbirth. 2019;19(1):408. Published 2019 Nov 8. doi:10.1186/s12884-019-2549-3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6839127
- Hamod H, Chamberlain PF, Moore NR, Mackenzie IZ. Conservative treatment of an incarcerated gravid uterus. BJOG. 2002;109:1074–1075.
- The Incarcerated Uterus: A Review of MRI and Ultrasound Imaging Appearances. AJR:201, July 2013 DOI:10.2214/AJR.12.9473 https://www.ajronline.org/doi/pdf/10.2214/AJR.12.9473
- Sutter R, Frauenfelder T, Marincek B, Zimmermann R. Recurrent posterior sacculation of the pregnant uterus and placenta increta. Clin Radiol. 2006;61:527–530.
- Minassian VA, Dunn M. Recurrent sacculation of the pregnant uterus. A case report. J Reprod Med. 2000;45:1003–1006.
- Jacobsson B, Wide-Swensson D. Recurrent incarceration of the retroverted gravid uterus-a case report. Acta Obstet Gynecol Scand. 1999;78:737.
- Hooker AB, Bolte AC, Exalto N, Van Geijn HP. Recurrent incarceration of the gravid uterus. J Matern Fetal Neonatal Med. 2009;22:462–464.
- Silva PD, Berberich W. Retroverted impacted gravid uterus with acute urinary retention: report of two cases and a review of the literature. Obstet Gynecol. 1986;68:121–123.
- van Beekhuizen HJ, Bodewes HW, Tepe EM, Oosterbaan HP, Kruitwagen R, Nijland R. Role of magnetic resonance imaging in the diagnosis of incarceration of the gravid uterus. Obstet Gynecol. 2003;102:1134–1137.
- Dierickx I, Van Holsbeke C, Mesens T, Gevers A, Meylaerts L, Voets W, et al. Colonoscopy-assisted reposition of the incarcerated uterus in mid-pregnancy: a report of four cases and a literature review. Eur J Obstet Gynecol Reprod Biol. 2011;158:153–158.
- Dierickx I, Mesens T, Van Holsbeke C, Meylaerts L, Voets W, Gyselaers W. Recurrent incarceration and/or sacculation of the gravid uterus: a review. J Matern Fetal Neonatal Med. 2010;23:776–780.
- Matsushita H, Watanabe K, Wakatsuki A. Management of a second trimester miscarriage in a woman with an incarcerated retroverted uterus. J Obstet Gynaecol. 2014;34:272–273.
- Newell SD, Crofts JF, Grant SR. The incarcerated gravid uterus: complications and lessons learned. Obstet Gynecol. 2014;123:423–427.
- Chauleur C, Vulliez L, Seffert P. Acute urine retention in early pregnancy resulting from fibroid incarceration: proposition for management. Fertil Steril 2008; 90:1198.e7–e10
- Dierickx I, Van Holsbeke C, Mesens T, et al. Colonoscopy-assisted reposition of the incarcerated uterus in mid-pregnancy: a report of four cases and a literature review. Eur J Obstet Gynecol Reprod Biol 2011; 158:153–158
- Gibbons JM Jr, Paley WB. The incarcerated gravid uterus. Obstet Gynecol 1969; 33:842–845
- Fernandes DD, Sadow CA, Economy KE, Benson CB. Sonographic and magnetic resonance imaging findings in uterine incarceration. J Ultrasound Med 2012; 31:645–650
- Patterson E, Herd AM. Incarceration of the uterus in pregnancy. Am J Emerg Med 1997; 15:49–51
- van der Tuuk K, Krenning RA, Krenning G, Monincx WM. Recurrent incarceration of the retroverted gravid uterus at term: two times transvaginal caesarean section—a case report. J Med Case Rep 2009; 3:103
- Gottschalk EM, Siedentopf JP, Schoenborn I, Gartenschlaeger S, Dudenhausen JW, Henrich W. Prenatal sonographic and MRI findings in a pregnancy complicated by uterine sacculation: case report and review of the literature. Ultrasound Obstet Gynecol 2008; 32:582–586
- Singh MN, Payappagoudar J, Lo J, Prashar S. Incarcerated retroverted uterus in the third trimester complicated by postpartum pulmonary embolism. Obstet Gynecol 2007; 109:498–501
- Jacobsson B, Wide-Swensson D. Recurrent incarceration of the retroverted gravid uterus: a case report. Acta Obstet Gynecol Scand 1999; 78:737
- Grossenburg NJ, Delaney AA, Berg TG. Treatment of a late second-trimester incarcerated uterus using ultrasound-guided manual reduction. Obstet Gynecol 2011; 118:436–439
- Gardner CS, Jaffe TA, Hertzberg BS, Javan R, Ho LM. The incarcerated uterus: a review of MRI and ultrasound imaging appearances. AJR Am J Roentgenol. 2013;201:223–229.
- Dierickx I, Meylaerts LJ, Van Holsbeke CD, et al. Incarceration of the gravid uterus: diagnosis and preoperative evaluation by magnetic resonance imaging. Eur J Obstet Gynecol Reprod Biol. 2014;179:191–197.
- Fernandes DD, Sadow CA, Economy KE, Benson CB. Sonographic and magnetic resonance imaging findings in uterine incarceration. J Ultrasound Med. 2012;31:645–650.
- Jacobsson B, Wide-Swensson D. Incarceration of the retroverted gravid uterus: a review. Acta Obstet Gynecol Scand. 1999;78:665–668.
- Patterson E, Herd AM. Incarceration of the uterus in pregnancy. Am J Emerg Med. 1997;15:49–51.
- Dierickx I, Delens F, Backaert T, Pauwels W, Gyselaers W. Case report: incarceration of the gravid uterus: a radiologic and obstetric challenge. J Radiol Case Rep. 2014;8:28–36.
- Seubert DE, Puder KS, Goldmeier P, Gonik B. Colonoscopic release of the incarcerated gravid uterus. Obstet Gynecol. 1999;94:792–794.
- Algra LJ, Fogel ST, Norris MC. Anesthesia for reduction of uterine incarceration: report of two cases. Int J Obstet Anesth. 1999;8:142–143.
- Policiano C, Araújo C, Santo S, Centeno M, Pinto L. Incarcerated gravid uterus: early manual reduction vs. late spontaneous resolution. Eur J Obstet Gynecol Reprod Biol. 2014;180:201–202.
- Inaba F, Kawatu T, Masaoka K, Fukasawa I, Watanabe H, Inaba N. Incarceration of the retroverted gravid uterus: the key to successful treatment. Arch Gynecol Obstet. 2005;273:55–57.
- Wang L, Wang J, Huang L. Incarceration of the retroverted uterus in the early second trimester performed by hysterotomy delivery. Arch Gynecol Obstet. 2012;286:267–269.
- Gerscovich EO, Maslen L. The retroverted incarcerated uterus in pregnancy: imagers beware. J Ultrasound Med. 2009;28:1425–1427.
- Pabuçcu EG, Kiseli M, Yarci Gursoy A, Bostanci A, Caglar GS, Dincer CS. Successful vaginal delivery at term following ventro-fixation procedure for uterine incarceration. J Obstet Gynaecol. 2016;36(7):869–872.