What is leprosy
Leprosy also known as Hansen’s disease, is a chronic infectious disease caused by slow-growing bacteria called Mycobacterium leprae, which has a preference for the skin and peripheral nerves 1. Leprosy is curable and treatment in the early stages can prevent disability. Mycobacterium leprae is an acid-fast, rod-shaped bacillus. Mycobacterium leprae bacteria grow very slowly causing slowly progressive granulomatous disease and it may take up to 20 years to develop signs of the infection. Leprosy primarily affects the skin, mucous membranes (lining of the nose or nasal mucosa), peripheral nervous system (nerve function), eyes and testes. The form leprosy disease takes depends on the person’s immune response to the infection. With early diagnosis and treatment, leprosy can be cured and usually prevent disability that can result from the disease. People with leprosy can continue to work and lead an active life during and after treatment. Once treatment is started, the person is no longer contagious. However, it is very important to finish the entire course of treatment as directed by the doctor.
Leprosy is one of the oldest known diseases of mankind and was once feared as a highly contagious and devastating disease, but now scientists know it doesn’t spread easily and treatment is very effective once recognized. Leprosy is curable but if left untreated, the nerve damage can result in crippling of hands and feet, paralysis, and blindness. Still, a lot of stigma and prejudice remains about leprosy, and those suffering from it are isolated and discriminated against in many places where leprosy is seen. Continued commitment to fighting the stigma through education and improving access to treatment will lead to a world free of this completely treatable disease.
The Mycobacterium leprae bacteria attack the nerves, which can become swollen under the skin. This can cause the affected areas to lose the ability to sense touch and pain, which can lead to injuries, like cuts and burns. Usually, the affected skin changes color and either becomes:
- lighter or darker, often dry or flaky, with loss of feeling, or
- reddish due to inflammation of the skin.
If left untreated, the nerve damage can result in paralysis of hands and feet. In very advanced cases, the person may have multiple injuries due to lack of sensation, and eventually the body may reabsorb the affected digits over time, resulting in the apparent loss of toes and fingers. Corneal ulcers and blindness can also occur if facial nerves are affected. Other signs of advanced Hansen’s disease may include loss of eyebrows and saddle-nose deformity resulting from damage to the nasal septum.
Although the global prevalence of leprosy has decreased significantly over the past 20 years 2, it still remains an endemic problem in some tropical and subtropical countries 3. In 2008, a new species, Mycobacterium lepromatosis, was described causing a diffuse form of lepromatous leprosy in Mexico.
Each year, about 150 to 250 people in the United States and 216,108 around the world 4 get leprosy.
Leprosy presents most often during two different periods of life, between the ages of 10 and 14 and in those aged 35-44 years old. It is rarely seen in infants. In nearly all cases, leprosy is due to prolonged contact with another person with the disease. It has rarely been associated with handling infected armadillos in Southern states of the USA.
Leprosy bacteria have been found in armadillos in Brazil, and to a lesser extent, in the southern United States of America. People who hunt, kill, or process or eat armadillo meat are at a higher risk for infection with Mycobacterium leprae 5.
Antibiotics used first-line to eliminate organisms include dapsone, rifampicin and clofazimine. Antibiotics used during the treatment will kill the bacteria that cause leprosy. But while the treatment can cure the disease and prevent it from getting worse, it does not reverse nerve damage or physical disfiguration that may have occurred before the diagnosis. Thus, it is very important that the disease be diagnosed as early as possible, before any permanent nerve damage occurs.
Key facts
- Leprosy is a chronic disease caused by a bacillus, Mycobacterium leprae.
- Prolonged, close contact with someone with untreated leprosy over many months is needed to catch the disease.
- Mycobacterium leprae multiplies slowly and the incubation period of the disease, on average, is 5 years. In some cases, symptoms may occur within 1 year but can also take as long as 20 years to occur.
- The disease mainly affects the skin, the peripheral nerves, mucosa of the upper respiratory tract, and also the eyes.
- Leprosy is curable with multidrug therapy (MDT).
- Leprosy is transmitted via droplets, from the nose and mouth, during close and frequent contacts with untreated cases.
- Untreated, leprosy can cause progressive and permanent damage to the skin, nerves, limbs, and eyes.
- There were 216,108 new leprosy cases registered globally in 2016, according to official figures from 145 countries from the 6 World Health Organization (WHO) Regions.
- Based on 173,358 cases at the end of 2016, prevalence rate corresponds to 0.29/10,000.
Is leprosy contagious?
Yes. Scientists currently think it may happen when a person with leprosy (Hansen’s disease) coughs or sneezes, and a healthy person breathes in the droplets containing the Mycobacterium leprae bacteria. Prolonged, close contact with someone with untreated leprosy over many months is needed to catch the disease.
You cannot get leprosy from a casual contact with a person who has leprosy like:
- Shaking hands or hugging
- Sitting next to each other on the bus
- Sitting together at a meal
Leprosy is also not passed on from a mother to her unborn baby during pregnancy and it is also not spread through sexual contact.
Due to the slow-growing nature of the Mycobacterium leprae bacteria and the long time it takes to develop signs of the disease, it is often very difficult to find the source of infection.
In the southern United States, some armadillos are naturally infected with the bacteria that cause Hansen’s disease in people and it may be possible that they can spread it to people. However, the risk is very low and most people who come into contact with armadillos are unlikely to get leprosy.
For general health reasons, avoid contact with armadillos whenever possible. If you had a contact with an armadillo and are worried about getting Hansen’s disease, talk to your healthcare provider. Your doctor will follow up with you over time and perform periodic skin examinations to see if you develop the disease. In the unlikely event that you have Hansen’s disease, your doctor can help you get treatment.
Is there a cure for leprosy?
Yes. Leprosy is curable with multidrug therapy (MDT).
Who is at risk of leprosy?
Leprosy can affect people of all races all around the world. In the U.S., Hansen’s disease is rare. However, leprosy is most common in warm, wet areas in the tropics and subtropics. Worldwide prevalence is reported to be around 5.5 million, with 80% of these cases found in 5 countries: India, Indonesia, Myanmar, Brazil and Nigeria.
Overall, the risk of getting Hansen’s disease for any adult around the world is very low. That’s because more than 95% of all people have natural immunity to the disease.
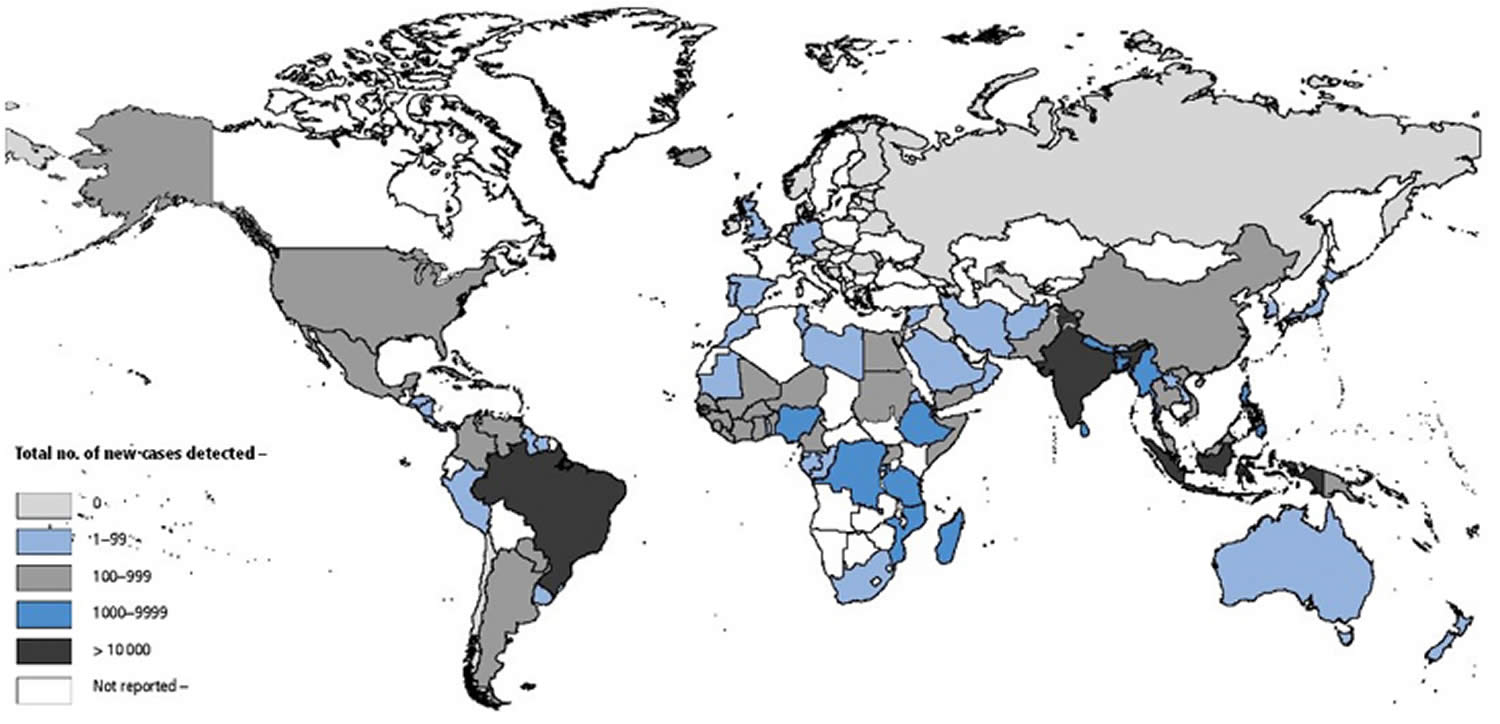
You may be at risk for leprosy if you live in a country where leprosy is widespread. Countries that reported more than 1,000 new cases of leprosy disease to WHO between 2011 and 2015 are:
- Africa: Democratic Republic of Congo, Ethiopia, Madagascar, Mozambique, Nigeria, United Republic of Tanzania
- Asia: Bangladesh, India, Indonesia, Myanmar, Nepal, , Philippines, Sri Lanka
- Americas: Brazil
The distribution of new leprosy cases by country among 136 countries that reported to WHO in 2015. India reported 127 326 new cases, accounting for 60% of the global new leprosy cases; Brazil, reported 26 395 new cases, representing 13% of the global new cases; and Indonesia reported 17,202 new cases, 8% of the global case load. No other countries reported >10,000 new cases. Eleven countries reported between 1000 and 10 000 cases: from Africa, the Democratic Republic of Congo, Ethiopia, Madagascar, Mozambique, Nigeria and United Republic of Tanzania; from Southeast Asia, Bangladesh, Myanmar, Nepal and Sri Lanka; and from Western Pacific, the Philippines. Collectively, these countries reported 19,069 new cases, 14% of all new cases globally. The remaining 10,286 new cases (5%) were reported by 92 countries. Thirty countries reported zero new cases. Ninety-two countries did not report, several of which are known to have cases of leprosy.
You may also be at risk if you are in prolonged close contact with people who have untreated Hansen’s disease. If they have not been treated, you could get the Mycobacterium leprae bacteria that cause Hansen’s disease. However, as soon as patients start treatment, they are no longer able to spread the disease.
Figure 1. Geographical Distribution of New Cases of Leprosy Disease Reported to WHO in 2015
[Source 6]Types of leprosy
There are several forms of leprosy that range from the mildest indeterminate form to the most severe lepromatous type. More severe forms arise because of less effective immune response to the infection. Most of those infected mount an appropriate immune response and never develop signs of leprosy.
The polymorphic nature of Hansen disease has inspired the development of various classification systems. The most comprehensive of these is the Ridley-Jopling system, which characterizes leprosy along a granulomatous continuum from tuberculoid to lepromatous leprosy (see Table 1) 7.
Depending on clinical features, leprosy is classified as:
- Indeterminate leprosy
- Tuberculoid leprosy
- Borderline tuberculoid leprosy
- Mid-borderline leprosy
- Borderline lepromatous leprosy
- Lepromatous leprosy
Patients with indeterminate leprosy, a very early form of leprosy, may either be cured or progress to one of the other forms of leprosy depending on their immune status. Within each type of leprosy, a patient may remain in that stage, improve to a less debilitating form or worsen to a more debilitating form depending on their immune state. Lepromatous leprosy is the only form that never reverts to a less severe form.
Table 1. Classification of leprosy
| CLASSIFICATION OF LEPROSY | ||||||
| Clinical findings | Lepromatous leprosy | Borderline lepromatous leprosy | Mid-borderline leprosy | Borderline tuberculoid leprosy | Tuberculoid leprosy | Indeterminate leprosy |
| Type of lesions | Macules, papules, nodules, diffuse infiltration | Macules, papules, plaques, infiltration | Plaques and domeshaped, punched-out lesions | Infiltrated plaques | Infiltrated plaques, often hypopigmented | Macules, often hypopigmented |
| Number | Numerous | Many | Many | Single, usually with satellite lesions, or more than 5 lesions | One or few (up to 5) lesions | One or few |
| Distribution | Symmetric | Tendency to symmetry | Evident asymmetry | Asymmetric | Localized, asymmetric | Variable |
| Definition | Vague, difficult to distinguish normal versus affected skin | Less well- defined borders | Less well-defined borders | Well-defined, sharp borders | Well-defined, sharp borders | Not always defined |
| Sensation | Not affected | Diminished | Diminished | Absent | Absent | Impaired |
| Bacilli in skin lesions | Many (globi) | Many | Many | Few (1+), if any, detected | None detected | Usually none detected |
Tuberculoid leprosy
- Can be either one large red patch with well-defined raised borders or a large hypopigmented asymmetrical spot
- Lesions become dry and hairless
- Loss of sensation may occur at site of some lesions
- Tender, thickened nerves with subsequent loss of function are common
- Spontaneous resolution may occur in a few years or it may progress to borderline or rarely lepromatous types
Borderline tuberculoid leprosy
- Similar to tuberculoid type except that lesions are smaller and more numerous
- Disease may stay in this stage or convert back to tuberculoid form, or progress
Mid-borderline leprosy
- Numerous, red, irregularly shaped plaques
- Sensory loss is moderate
- Disease may stay in this stage, improve or worsen
Borderline lepromatous leprosy
- Numerous lesions of all kinds, plaques, macules, papules and nodules. Lesions looking like inverted saucers are common
- Hair growth and sensation are usually not impaired over the lesions
Lepromatous leprosy
- Early nerve involvement may go unnoticed
- Numerous lesions of all kinds, plaques, macules, papules and nodules
- Early symptoms include nasal stuffiness, discharge and bleeding, and swelling of the legs and ankles
Left untreated, the following problems may occur in lepromatous leprosy:
- Skin thickens over forehead (leonine facies), eyebrows and eyelashes are lost, nose becomes misshapen or collapses, ear lobes thicken, upper incisor teeth fall out
- Eye involvement causing photophobia (light sensitivity), glaucoma and blindness
- Skin on legs thickens and forms ulcers when nodules break down
- Testicles shrivel causing sterility and enlarged breasts (males)
- Internal organ infection causing enlarged liver and lymph nodes
- Voice becomes hoarse due to involvement of the larynx
- Slow scarring of peripheral nerves resulting in nerve thickening and sensory loss. Fingers and toes become deformed due to painless repeated trauma.
How is leprosy spread?
It is not known exactly how leprosy (Hansen’s disease) spreads between people. Scientists currently think it may happen when a person with leprosy (Hansen’s disease) coughs or sneezes, and a healthy person breathes in the droplets containing the Mycobacterium leprae bacteria. Prolonged, close contact with someone with untreated leprosy over many months is needed to catch the disease.
You cannot get leprosy from a casual contact with a person who has leprosy like:
- Shaking hands or hugging
- Sitting next to each other on the bus
- Sitting together at a meal
Leprosy is also not passed on from a mother to her unborn baby during pregnancy and it is also not spread through sexual contact.
Due to the slow-growing nature of the Mycobacterium leprae bacteria and the long time it takes to develop signs of the disease, it is often very difficult to find the source of infection.
In the southern United States, some armadillos are naturally infected with the bacteria that cause Hansen’s disease in people and it may be possible that they can spread it to people. However, the risk is very low and most people who come into contact with armadillos are unlikely to get leprosy.
For general health reasons, avoid contact with armadillos whenever possible. If you had a contact with an armadillo and are worried about getting Hansen’s disease, talk to your healthcare provider. Your doctor will follow up with you over time and perform periodic skin examinations to see if you develop the disease. In the unlikely event that you have Hansen’s disease, your doctor can help you get treatment.
What does leprosy look like?
The range of cutaneous manifestations in leprosy is vast, and can be initially misdiagnosed as other skin diseases 9, especially in non-endemic areas.
Figure 2. Leprosy
Figure 3. Lepromatous leprosy
Figure 4. Leprosy
Figure 5. Leprosy histoid type
Leprosy symptoms
Once infected with the mycobacteria, the average incubation period is two to three years, but it can range from 6 months to 40 years or longer. In 90% of patients the first sign of the disease is a feeling of numbness, which may precede skin lesions by a number of years. Temperature is the first sensation lost, followed by light touch, pain and then deep pressure. Sensory loss usually begins in the extremities (toes and fingertips).
Symptoms mainly affect the skin, nerves, and mucous membranes (the soft, moist areas just inside the body’s openings). The first skin lesion is usually the indeterminate type, which causes one or a few hypopigmented (pale) spots before evolving into the borderline, tuberculoid or lepromatous types.
Leprosy disease can cause skin symptoms such as:
- Discolored patches of skin, usually flat, that may be numb and look faded (lighter than the skin around)
- Growths (nodules) on the skin
- Thick, stiff or dry skin
- Painless ulcers on the soles of feet
- Painless swelling or lumps on the face or earlobes
- Loss of eyebrows or eyelashes
Symptoms caused by damage to the nerves are:
- Numbness of affected areas of the skin
- Muscle weakness or paralysis (especially in the hands and feet)
- Enlarged nerves (especially those around the elbow and knee and in the sides of the neck)
- Eye problems that may lead to blindness (when facial nerves are affected)
Symptoms caused by the disease in the mucous membranes are:
- A stuffy nose
- Nosebleeds
Since Hansen’s disease affects the nerves, loss of feeling or sensation can occur. When loss of sensation occurs, injuries such as burns may go unnoticed. Because you may not feel the pain that can warn you of harm to your body, take extra caution to ensure the affected parts of your body are not injured.
If left untreated, the signs of advanced leprosy can include:
- Paralysis and crippling of hands and feet
- Shortening of toes and fingers due to reabsorption
- Chronic non-healing ulcers on the bottoms of the feet
- Blindness
- Loss of eyebrows
- Nose disfigurement
Other complications that may sometimes occur are:
- Painful or tender nerves
- Redness and pain around the affected area
- Burning sensation in the skin.
What causes leprosy
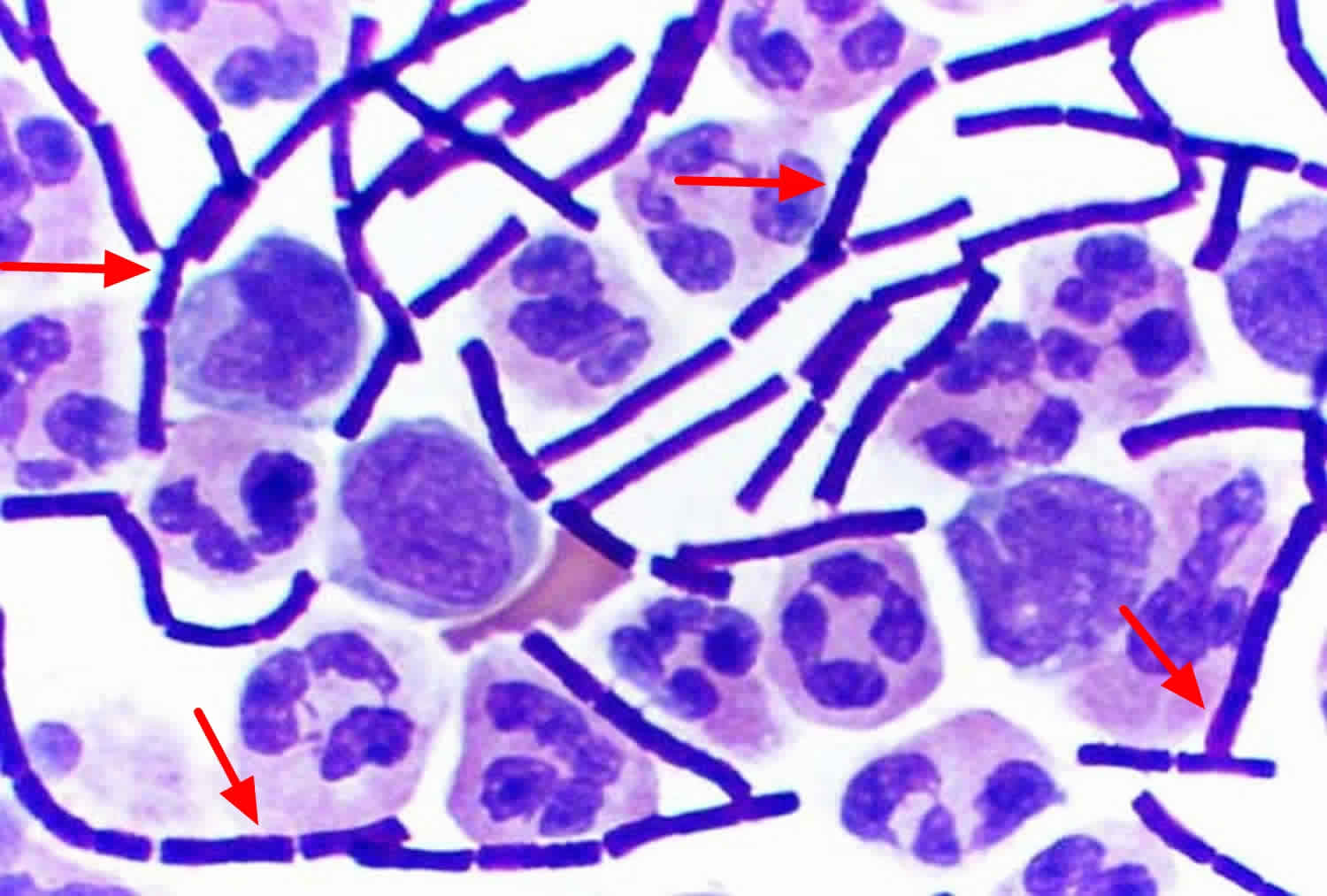
Leprosy (Hansen’s disease) is a chronic infectious disease caused by Mycobacterium leprae bacteria. Mycobacterium leprae bacteria is an acid-fast, rod-shaped bacillus. Mycobacterium leprae bacteria multiply very slowly (dividing approximately once every 13 days) and is an obligate intracellular pathogen that lacks several genes needed for independent survival, thus it has never been grown in bacteriologic media. However, it has been grown in mouse foot pads by injecting ground tissue from lepromatous nodules or nasal scrapings from leprosy patients into the foot pad of the animal. Typically, the granuloma appears at the inoculation site within 6 months. Armadillos can also be experimentally infected and will develop systemic disease, and are now the most common animal used to study Hansen’s disease and its treatment. Mycobacterium leprae bacteria grow very slowly causing slowly progressive granulomatous disease and it may take up to 20 years to develop signs of the infection.
Figure 6. Mycobacterium leprae bacteria
Leprosy diagnosis
Leprosy disease can be recognized by appearance of patches of skin that may look lighter or darker than the normal skin. Sometimes the affected skin areas may be reddish. Loss of feeling in these skin patches is common. You may not feel a light touch or a prick with a needle.
To confirm the diagnosis, your doctor will take a sample of your skin or nerve (through a skin or nerve biopsy) to look for the bacteria under the microscope and may also do tests to rule out other skin diseases. A skin biopsy may show characteristic histopathology, with granulomas (mixed inflammatory cell infiltrate in the deeper layers of the skin, the dermis) and involvement of the nerves. Special staining of the tissue may show acid fast bacilli, the number visible depending on the type of leprosy.
The bacteria may also be found in lepromatous leprosy on smears taken from skin slits made in the ear lobes, but the smears will be negative in the tuberculoid or borderline forms of the disease.
Leprosy treatment
Management of leprosy is aimed at stopping infection and minimizing potential physical deformities. Leprosy disease is treated with a combination of antibiotics depending on the form of the disease. Typically, 2 or 3 antibiotics are used at the same time. These are dapsone with rifampicin, and clofazimine is added for some types of the disease. This is called multidrug therapy (MDT). This strategy helps prevent the development of antibiotic resistance by the bacteria, which may otherwise occur due to length of the treatment.
- Paucibacillary form – 2 antibiotics are used at the same time, daily dapsone and rifampicin once per month
- Multibacillary form – daily clofazimine is added to rifampicin and dapsone.
Varying regimens with multidrug therapy (MDT) are used depending on the type of leprosy and the severity of infection. This may be a combination of two or three antibiotics given over varying lengths of time (up to years). Other antibiotics include minocycline, ofloxacin and clarithromycin.
Oral corticosteroids and thalidomide are helpful in preventing nerve damage by reducing swelling. Long courses are necessary to decrease severity of deformities and disabilities.
In the U.S., people with Hansen’s disease may be treated at special clinics run by the National Hansen’s Disease Program (https://www.hrsa.gov/hansens-disease/index.html). There are several federally supported outpatient clinics throughout the U.S. and Puerto Rico (https://www.hrsa.gov/hansens-disease/ambulatory-clinics.html).
Surgery may sometimes be used to drain abscesses to restore nerve function, reconstruct collapsed nose, or to improve function or appearance of affected areas.
- Treatment usually lasts between one to two years.
- Leprosy can be cured if treatment is completed as prescribed.
Patient education is paramount. Leprosy can be cured but it is essential to take the full course of medication. It is no longer infectious once treatment has begun.
If you are treated for Leprosy disease, it’s important to:
- Tell your doctor if you experience numbness or a loss of feeling in certain parts of the body or in patches on the skin. This may be caused by nerve damage from the infection. If you have numbness and loss of feeling, take extra care to prevent injuries that may occur, like burns and cuts.
- Take the antibiotics until your doctor says your treatment is complete. If you stop earlier, the bacteria may start growing again and you may get sick again.
- Tell your doctor if the affected skin patches become red and painful, nerves become painful or swollen, or you develop a fever as these may be complications of Leprosy disease that may require more intensive treatment with medicines that can reduce inflammation.
If left untreated, the nerve damage can result in paralysis and crippling of hands and feet. In very advanced cases, the person may have multiple injuries due to lack of sensation, and eventually the body may reabsorb the affected digits over time, resulting in the apparent loss of toes and fingers. Corneal ulcers or blindness can also occur if facial nerves are affected, due to loss of sensation of the cornea (outside) of the eye. Other signs of advanced leprosy may include loss of eyebrows and saddle-nose deformity resulting from damage to the nasal septum.
Antibiotics used during the treatment will kill the bacteria that cause leprosy. But while the treatment can cure the disease and prevent it from getting worse, it does not reverse nerve damage or physical disfiguration that may have occurred before the diagnosis. Thus, it is very important that the disease be diagnosed as early as possible, before any permanent nerve damage occurs.
Patients should be instructed how to deal with existing nerve damage for example protecting numb feet from injury. Physical, social and psychological rehabilitation is a necessary for those in whom neglected disease has caused havoc.
Lepra reactions
Lepra reactions occur in 30–50% of patients with leprosy. They may occur before, or more often, after the start of treatment and are induced by medicines, stress and surgical procedures. There are 3 main types of reaction.
Lepra type I (reversal) reaction
Lepra type I (reversal) reaction often affects those with with borderline shifting toward tuberculoid type, as the cell-mediated immune system improves in the first few months of drug treatment or for some other reason such as pregnancy.
Type 1 reactions result in fever, red swollen skin, and tender peripheral nerves. Treatment requires oral corticosteroids and nonsteroidal anti-inflammatories.
Lepra type II reaction
Lepra type II reaction is also called erythema nodosum leprosum. It affects those with with borderline lepromatous or lepromatous leprosy and is a humoral (antibody-antigen) reaction to immune complexes. Repeated episodes tend to occur later in treatment than the type I reaction, usually after several years.
Erythema nodosum leprosum presents as painful red nodules (lumps), which can blister or ulcerate, accompanied by fever, malaise, joint pain, nerve pain, eye disease and involvement of other organs. Treatment may include clofazimine, thalidomide, corticosteroids, colchicine, ciclosporin or tumour necrosis factor antagonists.
Lucio type II phenomenon
Lucio phenomenon is a cutaneous vasculitis in patients with lepromatous leprosy. It is difficult to treat and regimens must include multidrug therapy.
Lucio phenomenon presents as odd-shaped red patches and ulcers on hands, wrists, ankles and feet. It is associated with fever, arthritis, liver and kidney disease.
References- Ramos-e-Silva M, Castro MCR. Mycobacterial Infections In: Bolognia JL, Jorizzo JL, Rapini RP. eds. Dermatology. London: Mosby 2003.
- Moschella SL. An update on the diagnosis and treatment of leprosy. J Am Acad Dermatol. 2004; 51(3):417-26.
- Canizares O, Harman R, Adriaans B. Leprosy. In: Canizares O, Harman R, editors. Clinical tropical dermatology. 2nd ed. Boston: Blackwell Scientific, 1992: 165-200.
- Leprosy. http://www.who.int/en/news-room/fact-sheets/detail/leprosy
- da Silva MB, Portela JM, Li W, Jackson M, Gonzalez-Juarrero M, Hidalgo AS, et al. (2018) Evidence of zoonotic leprosy in Pará, Brazilian Amazon, and risks associated with human contact or consumption of armadillos. PLoS Negl Trop Dis 12(6): e0006532. https://doi.org/10.1371/journal.pntd.0006532
- http://www.who.int/lep/epidemiology/Geographical_distribution_of_new_leprosy_cases_2015.jpg
- Ridley DS, Jopling WH. Classification of leprosy according to immunity. A five-group system. Int J Lepr Other Mycobact Dis. 1966;34(3):255-73.
- Ramos-e-Silva M , Castro MCR. Mycobacterial infections. In: Bolognia JL; Jorizzo JL; Rapini RP. Dermatology. 2nd edition. London: Mosby, 2008; 1109.
- Hartzell JD, Zapor M, Peng S, Straight T. Leprosy: a case series and review. South Med J. 2004; 97(12):1252-6.