Level of consciousness
Level of consciousness (LOC) is a measurement of a person’s arousability and responsiveness to stimuli from the environment 1. A mildly depressed level of consciousness or alertness may be classed as lethargy; someone in this state can be aroused with little difficulty 1. People who are obtunded have a more depressed level of consciousness and cannot be fully aroused 2. Those who are not able to be aroused from a sleep-like state are said to be stuporous 2. Coma is the inability to make any purposeful response 2. Scales such as the Glasgow coma scale have been designed to measure the level of consciousness.
Consciousness is a general awareness of oneself and the surrounding environment. Consciousness is a dynamic state and can, therefore, be changed 3. The normal state of consciousness comprises either the state of wakefulness, awareness, or alertness in which most human beings function while not asleep or one of the recognized stages of normal sleep from which the person can be readily awakened 4.
An altered level of consciousness can result from a variety of factors, including alterations in the chemical environment of the brain (e.g. exposure to poisons or intoxicants), insufficient oxygen or blood flow in the brain, and excessive pressure within the skull. Prolonged unconsciousness is understood to be a sign of a medical emergency 5. A deficit in the level of consciousness suggests that both of the cerebral hemispheres or the reticular activating system have been injured 6. A decreased level of consciousness correlates to increased morbidity (sickness) and mortality (death) 7. Thus it is a valuable measure of a patient’s medical and neurological status. In fact, some sources consider level of consciousness to be one of the vital signs 8.
The exact neuronal connections that modulate alertness, wakefulness, and normal sleep and drowsiness are not well defined 4. A distinct group of neurons, the reticular formation, is located in the periventricular areas of the midbrain, pons, and medulla. In addition to modulating various interconnecting pathways within the brainstem, this group of neurons relates to the levels of alertness and wakefulness. It is postulated that a diffuse group of neuronal connections emanates from this reticular formation, projecting up the midbrain into the thalamic structures and then on to the cortex. This system is referred to as the ascending reticular activating system. The ascending reticular activating system receives input from all sensory systems, and efferent connections are extensive. It is thought that this system is responsible for modulating alertness and sleep. As such, any interruption of this system could result in alteration in the level of consciousness (or in abnormalities in the sleep cycle).
The mechanisms producing dysfunction of the ascending reticular activating system arc varied and strongly dependent on the cause of the illness. In some instances, there may be more than one factor contributing to deterioration in the level of consciousness. For instance, metabolic and toxic diseases generally produce stupor or coma by affecting neuronal metabolism or altering neuronal transmission. In such situations, dysfunction generally occurs in an orderly rostrocaudal fashion, beginning with cortical dysfunction and sequentially involving the diencephalon, midbrain, pons, and medulla (such a progression is characteristic of the induction and maintenance of general anesthesia). Early on, with involvement of the cortex, seizures or other abnormal movement patterns that are cortically modulated (such as myoclonus) can occur.
It is unusual for a supratentorial mass lesion to result in significant alteration in the level of consciousness unless it is quite large or involves both hemispheres. Instead, progressive stupor or coma with such a lesion can be attributed to a separate physiologic process at the brainstem level or to the secondary effects on the brainstem of shifts and herniations. An example of the former would be the association of a posttraumatic supratentorial subdural hematoma with axonal stretch and tearing at the brainstem level. The latter is best exemplified by a brief description of transtentorial herniation and its consequences. When a supratentorial mass lesion becomes large enough to displace the medial aspect of the temporal lobe over the tentorial edge, the patient may acquire an ipsilateral partial third nerve palsy characterized by pupillary dilation and ptosis, and possibly a homonymous hemianopsia from occipital ischemia due to compression of the ipsilateral posterior cerebral artery at the tentorial edge. As the brainstem is twisted and contorted within the tentorial hiatus, small areas of hemorrhage or ischemia may develop within it, resulting in alterations in level of consciousness.
Mass lesions within the brainstem produce coma by virtue of direct effects on the reticular formation. Cerebellar lesions can cause coma by secondary brainstem compression.
At all times when evaluating the patient with an alteration in level of consciousness, the clinician must keep foremost in his or her mind the most common causes of coma. Leading the list are the various metabolic and toxic disturbances of the brain such as acid–base disequilibrium, disorders of oxygen or glucose metabolism, uremic and hepatic encephalopathy, drug overdose, and poison ingestion. Epilepsy and various postconvulsive states can present as altered consciousness. Cerebrovascular disorders such as ischemic or embolic stroke, intracerebral or subarachnoid hemorrhage are also common causes of stupor or coma. Infection (meningitis, cerebral abscess, or encephalitis) can be the culprit. Intracranial sequelae of head injury frequently result in alteration in consciousness, as can brain tumors, either primary or metastatic. On occasion, two or more etiologies may be operating; for instance, the alcoholic who presents in grade 2 coma with both an elevated blood alcohol level and a subdural hematoma.
Consequently, the history is important in the diagnosis of the causes of altered levels of consciousness. Knowledge of the temporal course and sequence of symptom evolution, or the presence of associated disease states, is most helpful.
It is helpful to have a standard scale by which one can measure levels of consciousness. This proves advantageous for several reasons: Communication among health care personnel about the neurologic condition of a patient is improved; guidelines for diagnostic and therapeutic intervention in certain situations can be linked to the level of consciousness; and in some situations a rough estimate of prognosis can be made based partly on the scale score. In order for such a scale to be useful it must be simple to learn, understand, and implement. Scoring must be reproducible among observers. The Grady Coma Scale (Table 1) has proved functional in this regard. It has been used for more than 10 years at Grady Memorial Hospital in Atlanta, Georgia, to gauge the level of consciousness of patients in the neurosurgical intensive care unit and elsewhere. The grade I patient is only slightly confused. The grade II patient requires a light pain stimulus (such as a sharp pin tapped lightly over the chest wall) for appropriate arousal, or may be combative or belligerent. The grade III patient is comatose but will ward off deeply painful stimuli such as sternal pressure or nipple twist with an appropriate response. The grade IV patient reacts inappropriately with either decorticate or decerebrate posturing to such deeply painful stimuli, and the grade V patient remains flaccid when similarly stimulated.
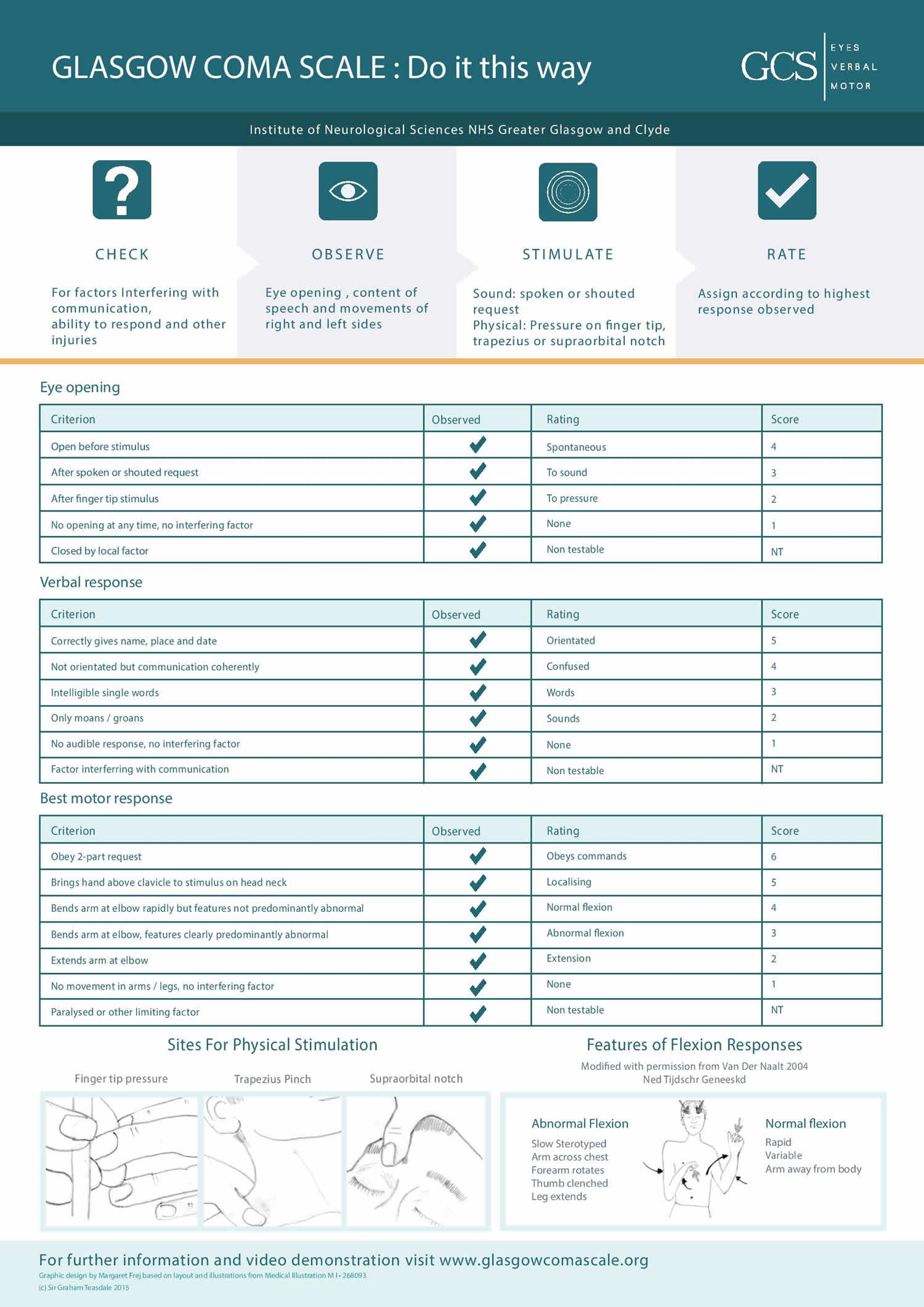
Many other coma scales have been developed. Most are tailored to specific subsets of patients and are designed not only to reflect level of consciousness but also to include additional data so that more reliable comparisons can be made for research purposes or more reliable prognostic determinations can be made. An example of such a scale is the Glasgow Coma Scale (Table 3). The Glasgow Coma Scale or GCS is a neurological scale that aims to give a reliable, objective way of recording the general level of consciousness in patients with traumatic brain injury (TBI) and to to help gauge the severity of an acute brain injury 9. The Glasgow Coma Scale (GCS) is divided into 3 categories, eye opening (E), motor response (M), and verbal response (V). The Glasgow Coma Scale score is determined by the sum of the score in each of the 3 categories, with a maximum score of 15 and a minimum score of 3, as follows:
- Glasgow Coma Scale score = eye opening (E) + motor response (M) + verbal response (V)
Based on motor responsiveness, verbal performance, and eye opening to appropriate stimuli, the Glascow Coma Scale was designed and should be used to assess the depth and duration coma and impaired consciousness. Glasgow Coma Scale helps to gauge the impact of a wide variety of conditions such as acute brain damage due to traumatic and/or vascular injuries or infections, metabolic disorders (e.g., hepatic or renal failure, hypoglycemia, diabetic ketosis), etc. Education is necessary to the proper application of the Glasgow Coma Scale 10. The predictive value of the GCS, even when applied early, is limited 11. Despite these and other limitations 12, health care practitioners continue to use Glasgow Coma Scale widely.
Glasgow Coma Scale was initially used to assess level of consciousness after head injury, and the Glasgow Coma Scale is now used by first aid, emergency medical services, and doctors as being applicable to all acute medical and trauma patients. In hospitals it is also used in monitoring chronic patients in the intensive care. The Glasgow Coma Scale was published in 1974 by Graham Teasdale and Bryan J. Jennett, professors of neurosurgery at the University of Glasgow’s Institute of Neurological Sciences at the city’s Southern General Hospital 13.
The AVPU scale (an acronym from “alert, verbal, pain, unresponsive”) is another means of measuring level of consciousness: people are assessed to determine whether they are alert, responsive to verbal stimuli, responsive to painful stimuli, or unresponsive 14. AVPU is a straightforward scale that is useful to rapidly grade a patient’s gross level of consciousness, responsiveness, or mental status. The AVPU scale is used during pre-hospital care, emergency rooms, general hospital wards, and ICU settings 15.
The basis of the AVPU scale is on the following criterion 14:
- Alert: The patient is aware of the examiner and can respond to the environment around them on their own. The patient can also follow commands, open their eyes spontaneously and track objects.
- Verbally Responsive: The patient’s eyes do not open spontaneously. The patient’s eyes open only in response to a verbal stimulus directed toward them. The patient is able to directly react to that verbal stimulus in a meaningful way.
- Painfully Responsive: The patient’s eyes do not open spontaneously. The patient will only respond to the application of painful stimuli by an examiner. The patient may move, moan, or cry out directly in response to the painful stimuli.
- Unresponsive: The patient does not respond spontaneously. The patient does not respond to verbal or painful stimuli.
The AVPU scale is a quick and simple way of detecting altered mental status in a patient. No formal training is necessary to use this score. It can be utilized during first aid and in the pre-hospital setting as any score lower than an “A” is considered abnormal until proven otherwise. This should prompt the examiner to conduct additional assessments or begin more definitive care. Emergency medical services crews may begin with AVPU, to be followed by a GCS assessment if the AVPU score is below “A.” AVPU is less detailed than the Glasgow Coma Scale, but it is performed at a much faster rate. AVPU was initially used in the primary survey of trauma patients, as a decreased mental status could indicate inadequate circulation of oxygenated blood to the brain 16.
Similarly to GCS, where a score of 8 or lower prompts health care providers to consider the need for airway protection, the AVPU scale also addresses airway management and aspiration risks. Patients scoring “P” or “U” may have decreased or absent gag reflexes and thus are unable to maintain a patent airway. This status should prompt the healthcare provider to consider initiating a means of airway protection to avoid airway compromise or aspiration.
The AVPU scale correlates to distinct GSC ranges, as outlined below 17.
- Glasgow Coma Scale Score 15 ~ Alert
- Glasgow Coma Scale 12-13 ~ Verbally Responsive
- Glasgow Coma Scale 5-6 ~ Physically Responsive
- Glasgow Coma Scale 3 ~ Unresponsive
Other scales for assessing mental status exist and may be superior to AVPU in specific settings.
The Glasgow Coma Scale (GCS) and the Richmond Sedation and Agitation Scale (RASS) are two scales used for assessing mental status. One study showed that in admitted patients, both GCS and RASS were significantly more accurate predictors of mortality then AVPU. Further, the routine tracking of GCS and/or RASS on the wards may improve the accuracy of detecting patients with deteriorating clinical status 17.
The ACDU Scale (alertness, confusion, drowsiness, and unresponsiveness) is another 4-point scale similar to AVPU. One study showed that ACDU (alertness, confusion, drowsiness, and unresponsiveness) might be superior for the simple ward assessment of seriously ill patients compared to AVPU. Additionally, median GCS scores associated with ACDU (alertness, confusion, drowsiness, and unresponsiveness) were 15, 13, 10 and 6. The median values of ACDU were more evenly distributed than AVPU when researchers compared both scales to GCS. This even distribution may indicate that ACDU (alertness, confusion, drowsiness, and unresponsiveness) is superior at identifying early deteriorations in the conscious level when they occur in critically ill ward patients compared to AVPU 18.
The Simplified Motor Score (SMS) categorizes and scores patients in the following three categories: obeys commands, localizes pain, and withdraws to pain or worse. It is used to evaluate patients in the pre-hospital and acute care setting for possible traumatic brain injury. One study has shown it to have the best interrater reliability for assessing the altered loss of consciousness (LOC) of traumatic and non-traumatic cause among AVPU, GCS, and ACDU 19.
Table 1. Grady Coma Scale
| Responds appropriately to: | ||||
|---|---|---|---|---|
| Grade | State of awareness | Calling name | Light pain | Deep pain |
| I | Confused, drowsy, lethargic, indifferent and/or uncooperative; does not lapse into sleep when left undisturbed | Yes | Yes | Yes |
| II | Stuporous; may be disoriented to time, place, and person; will lapse into sleep when not disturbed; or belligerent and uncooperative | No | Yes | Yes |
| III | Deep stupor; requires strong pain to evoke movement | No | No | Yes |
| IV | Exhibits decorticate or decerebrate posturing to a deep pain stimulus | No | No | No |
| V | Does not respond to any stimuli; flaccid | No | No | No |
The level of consciousness determines to a certain extent the level of functional disturbance within the neuraxis. A patient who qualifies as a grade 1 or 2 has cortical or diencephalic dysfunction. The grade 3 patient has physiologic dysfunction above the midbrain. Grade 4 coma indicates dysfunction above the levels of the cerebral peduncles or pons, and with grade 5 coma the medulla may be all that is working. Observation of the pattern of respiration may further support the examiner’s impression of dysfunctional level (Table 2). Cheyne-Stokes respiration means trouble at or above the diencephalon; central neurogenic hyperventilation (which is rare) points to difficulty at the upper midbrain; apneustic respiration suggests functional pontine deficit; and an ataxic breathing pattern suggests dorso-medial medullary dysfunction. Observation of the rate, pattern, and depth of respiration over at least several minutes is necessary to document such alterations. Like respiratory patterns, the size and reactivity of the pupils can be used to substantiate further the level of dysfunction within the neuraxis (see Table 4 below). Small reactive pupils suggest diencephalic localization, frequently on a metabolic basis. Large pupils that dilate and contract automatically (hippus) but do not react to direct light stimulus suggest a tectal lesion. Midposition fixed pupils localize to the midbrain. Bilateral pinpoint pupils are indicative of pontine trouble.
Table 2. Some abnormal respiratory patterns found in comatose patients
| Pattern | Description | Site of dysfunction |
|---|---|---|
| Cheyne–Stokes | Periodic breathing in which phases of hyperpnea alternate with apnea; the phases alternate every 30 to 45 seconds | Cerebral hemispheres; diencephalons |
| Central neurogenic hyperventilation | Deep, rapid respirations at a rate of 24 or more/min | Midbrain; diencephalons |
| Apneustic | A prolonged inspiratory “cramp”; a prolonged gasp | Pontine tegmentum |
| Ataxic | Random sequences of shallow and deep respiration without pattern | Medulla |
Table 3. Glasgow Coma Scale
| Eye Opening Response (E) |
| Spontaneous–eyes open with blinking at baseline = 4 points |
| Opens eyes to verbal stimuli, command, speech = 3 points |
| Opens eyes to pain only (not applied to face) = 2 points |
| No eye opening = 1 point |
| Best Motor Response (M) |
| Obeys verbal commands for movement = 6 points |
| Purposeful movement to painful stimuli = 5 points |
| Withdraws in response to painful stimuli = 4 points |
| Flexion in response to painful stimuli (decorticate posturing) = 3 points |
| Extension response in response to painful stimuli (decerebrate posturing) = 2 points |
| No response = 1 point |
| Best Verbal Response (V) |
| Oriented conversation = 5 points |
| Confused conversation, but able to answer questions = 4 points |
| Inappropriate words = 3 points |
| Incomprehensible speech or sounds = 2 points |
| No response = 1 point |
Total Glasgow Coma Scale score = 15
- Total Glasgow Coma Scale score 15 is Normal
- Total Glasgow Coma Scale score 3-14 is Abnormal
Altered level of consciousness
The abnormal state of consciousness is more difficult to define and characterize, as evidenced by the many terms applied to altered states of consciousness by various observers 4.
Among such terms are:
- clouding of consciousness,
- confusional state,
- delirium,
- lethargy,
- obtundation,
- stupor,
- dementia,
- hypersomnia,
- vegetative state,
- akinetic mutism,
- locked-in syndrome,
- coma,
- brain death.
Many of these terms mean different things to different people, and may prove inaccurate when transmitting and recording information regarding the state of consciousness of a patient 4. Nevertheless, it is appropriate to define several of the terms as closely as possible.
- Awake: Alert, responds immediately and fully to commands may or may not be fully oriented
- Clouding of consciousness is a very mild form of altered mental status in which the patient has inattention and reduced wakefulness.
- Confusional state is a more profound deficit that includes disorientation, bewilderment, and difficulty following commands.
- Delirious includes disorientation, restlessness, hallucinations, sometimes delusions.
- Somnolent or sleepy. A somnolent person shows excessive drowsiness and responds to stimuli only with incoherent mumbles or disorganized movements 20
- Lethargy consists of severe drowsiness in which the patient can be aroused by moderate stimuli e.g. voice, and then responds, but may not be oriented in time, place or person and then drift back to sleep.
- Obtundation is a state similar to lethargy in which the patient has a lessened interest in the environment, slowed responses to stimulation, and tends to sleep more than normal with drowsiness in between sleep states. Patients can be aroused by stimuli (not pain), i.e. shaking, and will then respond to questions or commands. Remains aroused as long as stimulation is applied, if not will fall asleep, questions are answered with minimal response. During the arousal, patient responds but may be confused
- Stupor is a condition of deep sleep or unresponsiveness. Stupor means that only vigorous and repeated stimuli will arouse the individual, and when left undisturbed, the patient will immediately lapse back to the unresponsive state.
- Coma is a state of unarousable unresponsiveness. There is no motor response to the external environment or to any stimuli, even deep pain or suctioning. There is no arousal to any stimulus. Reflexes may be present, abnormal movement (posturing) to pain may be present.
Level of consciousness evaluation
The technique of evaluation of the patient with an altered level of consciousness can be divided into three phases 4:
- The first is to determine the level of consciousness itself.
- Second is evaluation of the patient, searching carefully for hints as to the cause of the confusion or coma.
- Third is the presence or absence of focality of the disorder, both in terms of the level of dysfunction within the rostrocaudal neuraxis and specific involvement of cortical or brainstem structures.
After the physician makes sure that no immediate life-threatening emergency such as airway obstruction or shock is present, the examination begins with observation of the patient:
- What is the position of the patient?
- Does the patient have one or more extremities positioned in an unusual manner, which might suggest paralysis or spasticity?
- Are the eyes opened or closed?
- Does the person acknowledge your presence, or is he or she oblivious to it?
If the patient is alert, acknowledges the presence of the examiner, seems well oriented to time and place and not confused on general questioning, then the level of consciousness would be considered normal. Thus one can have a normal level of consciousness yet be of subnormal intellectual capability, have a focal neurologic deficit such as an aphasia or hemiparesis, or exhibit abnormal thought content such as a schizophrenic patient might.
As the patient’s name is called in a normal tone of voice or if, during an attempt at a simple conversation, it is noted that the person is confused, drowsy, or indifferent, an abnormal level of consciousness exists. Individuals who respond with recognition when their name is called and do not lapse into sleep when left undisturbed, can be said to be in a grade 1 coma. If the alteration in level of consciousness is more severe, so that the person lapses into sleep when not disturbed and is arousable only when a pin is tapped gently over the chest wall, the grade of coma is 2. This category also includes the patient who is organically disoriented, belligerent, and uncooperative (as can be seen in various states of intoxication), or in the young adult with moderately severe head injury.
If such efforts as calling the patient’s name in a normal tone of voice or pricking the skin over the chest wall lightly with a pin result in no response, the examiner must choose a deeper pain stimulus. My preference is a pinch or slight twist of the nipple. Other options include sternal pressure, which may be applied with the fisted knuckle, or squeezing the nailbed. The slight periareolar bruising from repetitive nipple twisting is much less problematic to the eventually recovered patient than the chronically painful subperiosteal or subungual hemorrhage from the latter options. Under no circumstances should one apply such a painful stimulus as irrigation of the ears with ice water until the status of the intracranial pressure is known. The patient’s response to the deep pain stimulus is then noted. A patient who winces and/or attempts to ward off the deep pain stimulus appropriately can be said to be in a grade 3 coma.
The deep pain stimulus may, however, result in abnormal postural reflexes, either unilateral or bilateral. The two most common are decorticate and decerebrate posturing. In both states, the lower extremity exhibits extension at the knee and internal rotation and plantar flexion at the ankle. In decorticate posturing, the upper extremity is held adducted at the shoulder and flexed at the elbow, wrist, and metacarpal-phalangeal joints. In the decerebrate state, the upper extremity is adducted at the shoulder and rigidly extended and internally rotated at the elbow. In either case, the patient exhibiting such posturing to a deep pain stimulus is rated a grade 4 coma. The patient who maintains a state of flaccid unresponsiveness despite deep pain stimulation is a grade 5 coma.
Once the level of consciousness is determined, a careful check for hints as to the cause of the alteration in level of consciousness should be undertaken. In most instances the history (which can be obtained from the patient or those who accompany him, or from available medical records) is more valuable than is the examination. History is not always available, however, and in all instances a careful examination is merited.
- Vital signs may obviously suggest infection, hypertension, shock, or increased intracranial pressure with bradycardia.
- Is there evidence of trauma to the head or elsewhere?
- Inspect the scalp thoroughly for abrasions or contusions, and if blood is seen, explain it even if it means shaving part of the scalp to do so.
- Is there periorbital or retroauricular ecchymosis, or is there blood behind the tympanic membrane to suggest basilar skull fracture?
- Is there papilledema or intraocular hemorrhage?
- Is the conjunctiva icteric, the liver enlarged, or does the patient have asterixis?
- Are the lips or nailbeds discolored or pale so as to suggest anemia or pulmonary dysfunction?
- Is the neck stiff—a warning of meningitis or subarachnoid hemorrhage.
- Is there anything to suggest intoxication with drugs or poisons, such as an unusual odor to the breath or body or pinpoint pupils?
The next step is to try to localize the problem that is resulting in alteration of consciousness, first by trying to localize the dysfunction to a level within the rostrocaudal neuraxis and second by searching for focal clues such as specific cranial nerve deficits, abnormal reflexes, or motor asymmetry.
Table 4. Possible pupillary patterns in comatose patients
| Pattern | Site of dysfunction |
|---|---|
| Small, reactive | Diencephalon |
| Large “fixed,” with hippus | Midbrain tectum |
| Midposition, “fixed” | Midbrain |
| Pinpoint, not reactive | Pons |
| One dilated | Suggests transtentorial herniation |
Examination of the so-called brainstem reflexes is of utmost importance in evaluation of the patient in grade 3, 4, or 5 coma (Table 5). All rely on integrity of centers within the pons or dorsal midbrain. As emphasized earlier, the cold-water caloric test should not be done until the status of the patient’s intracranial pressure is known. Irrigation of the eardrum with ice water causes such pain that the patient’s Valsalva response may be enough to initiate herniation in the already tenuous situation of markedly increased intracranial pressure. Suggested methods for testing these reflexes are outlined in Table 5.
Further examination may be productive in revealing findings such as a unilateral dilated pupil, a focal cranial nerve deficit, an asymmetry of movement suggesting a hemiparesis, abnormal movements suggesting seizure activity, a reflex asymmetry, or a focal sensory abnormality that will help further localize the area of trouble within the central nervous system. The specific techniques for such examination are covered elsewhere.
Table 5. Brainstem Reflexes
| Reflex | Technique | Localization |
|---|---|---|
| Pupillary light reaction | Shine light on pupil and observe constriction | Midbrain and pontine tegmentum |
| Corneal response | Open lid if necessary; lightly stroke cornea with cotton wisp; observe for blink | Pons |
| Oculocephalic response (doll’s eyes) | Hold lids open with one hand while turning head side to side with the other hand; observe rotation of eyes side to side | Pons—vestibular |
| Oculovestibular; cold-water calorics | With head at 30 degrees, irrigate external auditory canal and tympanic membrane slowly with up to 120 ml ice water; observe for conjugate rotation of the eyes toward the side irrigated | Pons—vestibular |
- Kandel ER; Jessell, Thomas M.; Schwartz, James H. (2000). Principles of neural science. New York: McGraw-Hill. p. 901. ISBN 0-8385-7701-6
- Porth C (2007). Essentials of Pahtophysiology: Concepts of Altered Health States. Hagerstown, MD: Lippincott Williams & Wilkins. p. 835. ISBN 978-0-7817-7087-3.
- Hickey IV (1997) The Clinical Practice of Neurological Nursing. 4th edn. JB Lippincott, New York
- Tindall SC. Level of Consciousness. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 57. Available from: https://www.ncbi.nlm.nih.gov/books/NBK380
- Pollak AN, Gupton CL (2002). Emergency Care and Transportation of the Sick and Injured. Boston: Jones and Bartlett. p. 140. ISBN 0-7637-1666-9.
- Porth C (2007). Essentials of Pahtophysiology: Concepts of Altered Health States. Hagerstown, MD: Lippincott Williams & Wilkins. p. 838. ISBN 978-0-7817-7087-3
- Scheld WM, Whitley RJ, Marra CM (2004). Infections of the Central Nervous System. Hagerstown, MD: Lippincott Williams & Wilkins. p. 530. ISBN 0-7817-4327-3
- Pollak AN, Gupton CL (2002). Emergency Care and Transportation of the Sick and Injured. Boston: Jones and Bartlett. p. 140. ISBN 0-7637-1666-9
- Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975 Mar 1. 1(7905):480-4.
- Rowley G, Fielding K. Reliability and accuracy of the Glasgow Coma Scale with experienced and inexperienced users. Lancet 1991; 337:535-538
- Waxman K, Sundine MJ, Young RF. Is early prediction of outcome in severe head injury possible? Arch Surg 1991; 126:1237-1242
- Eisenberg HM. Outcome after head injury: Part I: general Considerations, in Becker DP, Povlishock JR (eds): Central Nervous System Trauma Status Report, 1985. Washington, DC: U.S. Government Printing Office, 1988:271-280
- Teasdale G, Jennett B. Assessment of coma and impaired conciousness: a practical scale. Lancet. 1974; 2:81-84.
- Romanelli D, Farrell MW. AVPU (Alert, Voice, Pain, Unresponsive) [Updated 2019 Feb 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538431
- Hoffmann F, Schmalhofer M, Lehner M, Zimatschek S, Grote V, Reiter K. Comparison of the AVPU Scale and the Pediatric GCS in Prehospital Setting. Prehosp Emerg Care. 2016 Jul-Aug;20(4):493-8.
- Planas JH, Waseem M. Trauma Primary Survey. [Updated 2019 Feb 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430800
- Zadravecz FJ, Tien L, Robertson-Dick BJ, Yuen TC, Twu NM, Churpek MM, Edelson DP. Comparison of mental-status scales for predicting mortality on the general wards. J Hosp Med. 2015 Oct;10(10):658-63.
- McNarry AF, Goldhill DR. Simple bedside assessment of level of consciousness: comparison of two simple assessment scales with the Glasgow Coma scale. Anaesthesia. 2004 Jan;59(1):34-7.
- Gill M, Martens K, Lynch EL, Salih A, Green SM. Interrater reliability of 3 simplified neurologic scales applied to adults presenting to the emergency department with altered levels of consciousness. Ann Emerg Med. 2007 Apr;49(4):403-7, 407.e1.
- Kruse MJ (1986). Nursing the Neurological and Neurotrauma Patient. Totowa, N.J: Rowman & Allanheld. pp. 57–58. ISBN 0-8476-7451-7