What is malnutrition
Malnutrition basically means “poor nutrition” or “bad nutrition” and can refer to undernutrition (not getting enough nutrients) or overnutrition (getting more nutrients than you need). Malnutrition is a serious condition that occurs when a person’s diet doesn’t contain the right amount of nutrients, where there is a disparity between the amount of food and other nutrients that the body needs for proper growth and health and the amount that it receives or takes in (absorbs). This imbalance is most frequently associated with undernutrition, the primary focus of this article, but it may also be due to overnutrition.
The world produces more food than ever before, yet an estimated 200 million people in Africa lack adequate nutrition, in part due to challenges ranging from drought and civil unrest to crop-destroying insects and sanitation problems. A coordinated, interdisciplinary approach among experts in agriculture, nutrition, environment, and public health is needed to help address these complex health and development challenges and to facilitate providing nutritious food to the undernourished.
In United States, groups at risk of malnutrition include those with:
- Chronic disease (consider acute episodes): chronic obstructive pulmonary disease (COPD), cancer, gastrointestinal disease, renal or liver disease and inflammatory conditions such as rheumatoid arthritis, inflammatory bowel disease 1
- Progressive neurological disease: dementia, Parkinson’s disease, motor neurone disease (MND) 1
- Acute illness: where adequate food is not being consumed for more than 5 days (more commonly seen in a hospital than a community setting) 1
- Debility: frailty, immobility, old age, depression, recent discharge from hospital 2
- Social issues: poor support, housebound, difficulty obtaining or preparing food 1
- Rehabilitation: after stroke 1, injury 2, cancer treatment 2
- End of Life/Palliative Care: tailor and adjust advice according to phase of illness 3
Malnutrition can affect anyone; however it is particularly common amongst older people and those who are socially isolated because they can’t get out much or because they have poor physical or mental health. Malnutrition can happen over a long period of time which sometimes makes it difficult to spot. Common signs of malnutrition are:
- unplanned weight loss – which can cause clothes, dentures, belts or jewellery to become loose
- tiredness and lethargy
- alterations in mood
- loss of appetite
- disinterest in food and/or fluids
- loss of muscle strength.
A balanced diet is essential for health and wellbeing. When someone has a poor appetite and is malnourished, calorie dense foods and drinks containing fat and sugar can help to improve energy intake without making portions too big to manage.
Effects of malnutrition include:
- increased risk of illness and infection
- impaired recovery from illness and surgery 2
- slower wound healing 2
- increased risk of falls 4
- poorer clinical outcomes e.g. higher mortality 2
- impaired immune response 2
- impaired psycho-social function 2
- low mood
- reduced energy levels
- reduced muscle strength and frailty 5
- reduced quality of life
- reduced independence and ability to carry out daily activities.
Treatment of undernutrition
- Restoring the nutrients that are missing, making nutrient-rich foods available, and providing supplements for specific deficiencies. In someone who is severely malnourished, this must be done slowly until the body has had time to adjust to the increased intake and then maintained at a higher than normal level until a normal or near normal weight has been achieved.
- Regular monitoring of those patients who have chronic malabsorption disorders or protein- or nutrient-losing conditions. Once the deficiencies have been addressed, putting a treatment plan into place is needed to prevent the malnutrition from recurring.
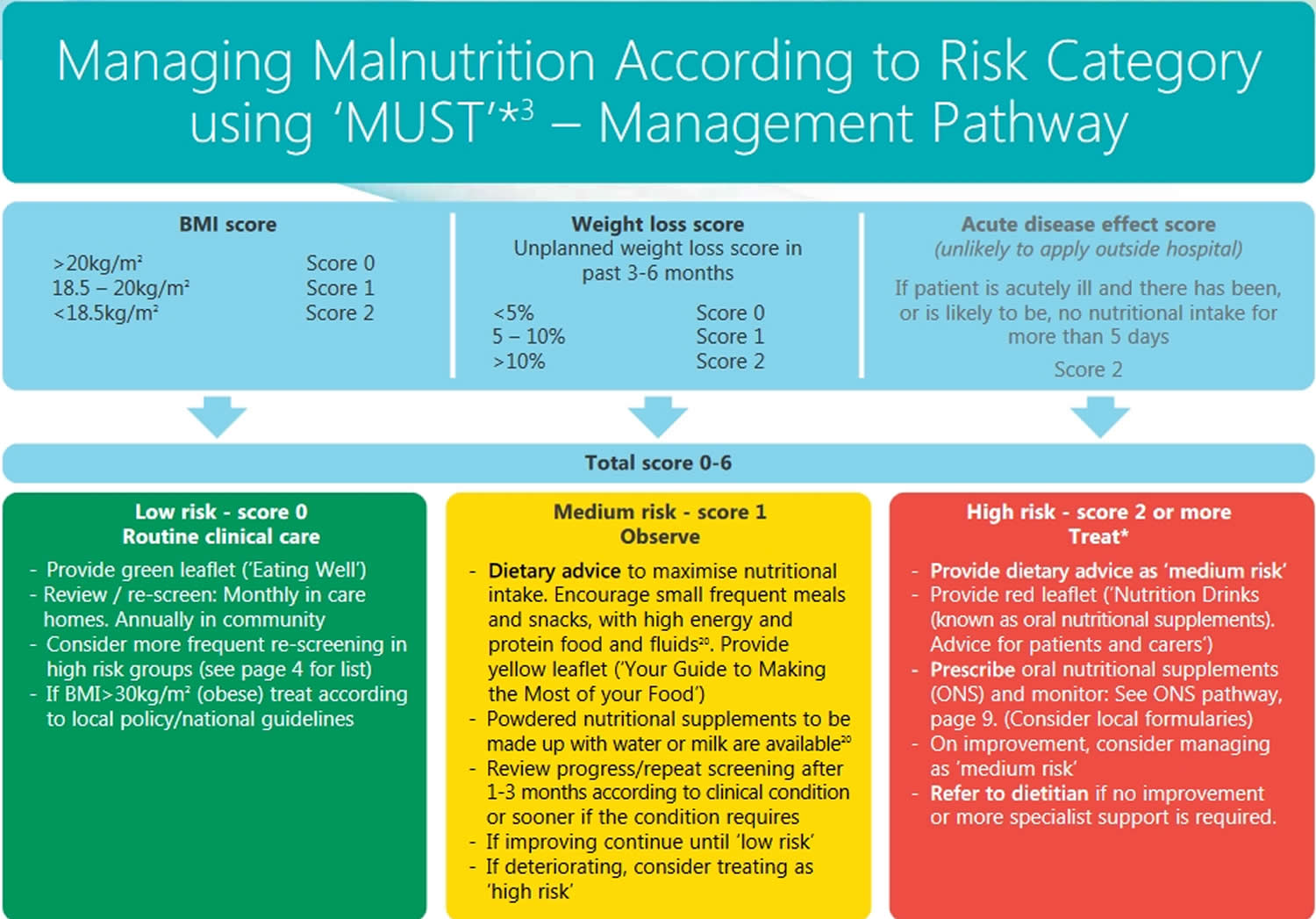
Figure 1. Managing Adult Malnutrition in the Community
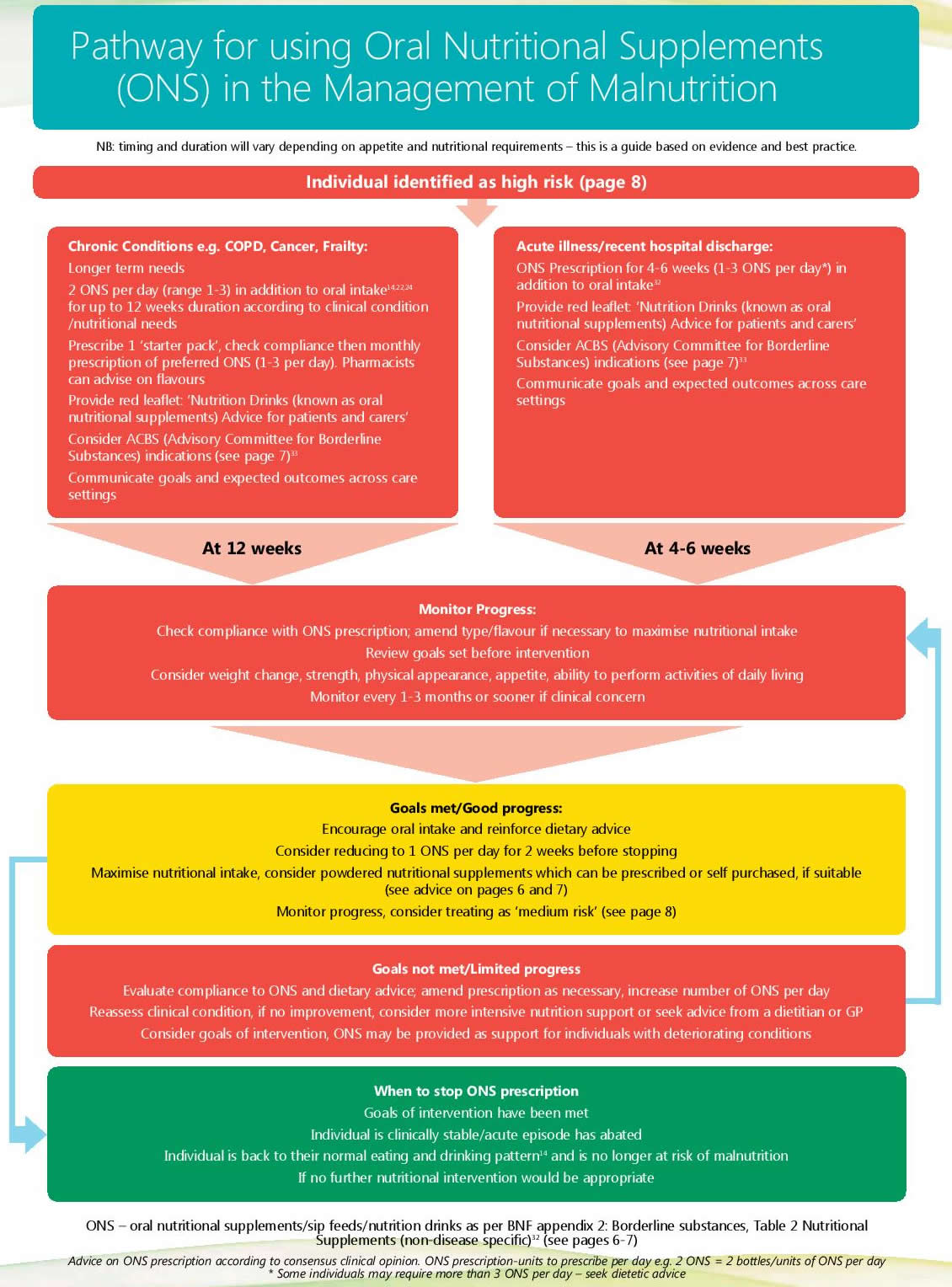
[Source 6]Figure 2. Management of malnutrition (undernutrition) using oral nutritional supplements
[Source 6]Protein is also important for people who are malnourished. If you follow the points listed here, you can make sure you are eating well:
- Eat 2-3 portions of high protein foods every day such as meat, fish, eggs, nuts, beans, pulses, soya, tofu and other meat-free protein foods.
- Eat/drink 2-3 portions of dairy foods every day such as cheese, milk and yoghurt or non-dairy alternatives like soya, almond or coconut milk.
- Eat a serving of starchy food at each meal (e.g. bread, cereals, potatoes, pasta or rice).
- Eat some fruit and vegetables every day (fresh, frozen, tinned, dried or juiced).
- If you enjoy fish, go for oily fish such as mackerel, salmon, herring, trout, pilchards or sardines as these are rich in omega-3 fatty acids. Aim for 2 portions a week (can be tinned or frozen for convenience).
- Have at least 6-8 glasses/mugs of drinks every day, choosing high calorie drinks where possible such as milky drinks (malted drinks, hot chocolate, milky coffee, smoothies and milkshakes) or sugary drinks such as fruit juice, fizzy drinks or squash can provide extra energy. If there are any health concerns which have previously required you to limit fat and sugar in your diet, e.g. diabetes or high cholesterol, you should discuss this with a health professional.
The following simple ideas will help you increase the amount of energy and protein which you eat in a day:
- Eat ‘little and often’ – try a small snack between meals and a dessert after lunch and evening meal.
- Try not to have drinks just before meals to avoid feeling too full to eat.
- Avoid low fat/diet versions of foods and drinks for example skimmed or semi-skimmed milk, low fat yogurt, sugar free drinks etc, or watery soups.
- Choose meals that you enjoy, are easy to prepare and eat, and are high in energy and protein. Items such as tinned fish or beans are easily stored and easy to prepare.
- If you are preparing food for others, remember as we get older, our taste buds change. Older people often prefer much sweeter tastes than they used to.
Add extra energy and protein to foods and fluid by adding high energy and protein ingredients.
Other high energy and protein foods include:
- cheese and crackers
- thick and creamy yogurt
- nuts and seeds
- peanut butter
- Bombay mix
- chips
- chocolate.
You may find that your energy levels change throughout the week and that on some days you feel better than others. Here are some suggestions to make preparing meals easier:
- Make the most of the ‘good days’ by preparing extra meals which you can store in the fridge/freezer as individual portions for ‘bad days’.
- Buy a selection of ready meals for times when you are not up for cooking.
- Make use of meal home delivery services – supermarkets also offer online shopping and home delivery services which may make shopping easier for you.
Swallowing difficulties
If you notice any of the following when eating or drinking you should seek advice from a healthcare professional such as your doctor or practice nurse, who can refer you on to specialist speech and language therapist or a dietitian:
- difficulty swallowing
- choking or coughing
- bringing food back up, sometimes through your nose
- a sensation that food is stuck in your throat or chest
- a change in the sound of your voice whilst/soon after eating i.e. your voice sounds ‘wet’.
Other things to consider:
- Check dentures fit correctly – if not, visit your dentist.
- If you have difficulty using cutlery or with coordination, try ‘finger foods’ such as toast, sandwiches, biscuits, chunks of meat, cheese etc.
- If you suffer from constipation, try gradually increasing your fibre intake by consuming beans, lentils, fruit and vegetables and wholegrain foods whilst also increasing your fluid intake.
- Regular exercise may help increase your appetite and build up your strength- start with something easy for you and increase the intensity gradually.
- If you have vision problems or for people with dementia, try using a colored plate so that the food stands out.
Types of malnutrition
Overnutrition
Chronic overnutrition can lead to obesity and to metabolic syndrome, a set of risk factors characterized by abdominal obesity, a decreased ability to process glucose (insulin resistance), unhealthy lipid levels, and high blood pressure (hypertension). Overweight and obesity is when a person is too heavy for his or her height. Abnormal or excessive fat accumulation can impair health. Overweight and obesity result from an imbalance between energy consumed (too much) and energy expended (too little). Globally, people are consuming foods and drinks that are more energy-dense (high in sugars and fats), and engaging in less physical activity.
People with metabolic syndrome have been shown to be at a greater risk of developing type 2 diabetes and cardiovascular disease. Another uncommon form of overnutrition is vitamin or mineral toxicity. This is usually due to excessive supplementation, for instance, with high doses of fat-soluble vitamins such as vitamin A rather than the ingestion of food. Toxicity symptoms depend on the substance(s) ingested, the severity of the overdose, and whether it is acute or chronic.
Inadequacies in intake of vitamins and minerals, often referred to as micronutrients, can also be grouped together. Micronutrients enable the body to produce enzymes, hormones, and other substances that are essential for proper growth and development.
Micronutrients are dietary components, often referred to as vitamins and minerals, which although only required by the body in small amounts, are vital to development, disease prevention, and wellbeing. Micronutrients are not produced in the body and must be derived from the diet 7.
Deficiencies in micronutrients such as iron, iodine, vitamin A, folate and zinc can have devastating consequences. At least half of children worldwide ages 6 months to 5 years suffer from one or more micronutrient deficiency, and globally more than 2 billion people are affected 8.
International Micronutrient Malnutrition Prevention and Control focuses primarily on helping to eliminate deficiencies in iron, vitamin A, iodine, folate and zinc.
Iodine, vitamin A, and iron are the most important in global public health terms; their deficiency represents a major threat to the health and development of populations worldwide, particularly children and pregnant women in low-income countries.
Iron
- Iron is an essential mineral critical for motor and cognitive development. Children and pregnant women are especially vulnerable to the consequences of iron deficiency 9.
- Low hemoglobin concentration (anemia) affects 43% of children 5 years of age and 38% of pregnant women globally 10
- Anemia during pregnancy increases the risk of maternal and perinatal mortality and low birth weight. Maternal and neonatal deaths are a major cause of mortality, together causing between 2.5 million and 3.4 million deaths worldwide 10
- World Health Organization recommends iron and folic acid supplements for reducing anemia and improving iron status among women of reproductive age 11.
- Flour fortification with iron and folic acid is globally recognized as one of the most effective and low-cost micronutrient interventions 12.
Iodine
- Iodine is one of the most important minerals required by a fetus for brain and cognitive development, though the iodine content in most foods and beverages is low 9.
- 18 million babies are born mentally impaired because of maternal iodine deficiency and 38 million are born at risk of iodine deficiency 13. Globally it is estimated that 2 billion people have insufficient iodine intake 14.
- Fortification of salt with iodine has been one of the most successful nutrition interventions to date–71% of global households have access to iodized salt 15.
- Salt iodization has led to an increase in IQ points and significant decline in the prevalence of iodine deficiency disorders, such as goiters 9.
Vitamin A
- Vitamin A is necessary to support healthy eyesight and immune system functions; children who are deficient face an increased risk of blindness and death from infections such as measles and diarrhea 16.
- Globally, 1 in 3 pre-school aged children and 1 in 6 pregnant women are vitamin A deficient due to inadequate dietary intake 16.
- Vitamin A supplementation of children 6-59 months has been shown to be highly effective in reducing mortality from all causes in countries where vitamin A deficiency is a public health concern 16.
Zinc
- Zinc is a mineral that promotes immunity, resistance to infection, and proper growth and development of the nervous system3, and is integral to healthy pregnancy outcomes 17
- 17.3% of the global population is at risk for zinc deficiency due to dietary inadequacy, though up to 30% of people are at risk in some regions of the world 17.
- Zinc supplementation reduces the incidence of premature birth, decreases childhood diarrhea and respiratory infections, lowers all-cause mortality, and increases growth and weight gain among infants and young children 17.
Folate
- Folate is a vitamin that is essential in the earliest days of fetal growth for healthy development of the brain, spinal cord, and skull 18
- Ensuring sufficient levels of folate in women prior to conception can reduce neural tube defects (a serious birth defect) by up to 50% 18
- Supplementations of women 15-49 years with folic acid, and fortification of foods such as wheat flour with folic acid, are effective interventions for the reduction of birth defects, morbidity, and mortality in newborns 19.
Undernutrition
Undernutrition occurs when one or more vital nutrients are not present or available in the quantity that is needed for the body to develop and function normally. This may be due to insufficient intake, increased loss, increased demand, or a condition or disease that decreases the body’s ability to digest and absorb nutrients from food. While the need for adequate nutrition is a constant, the demands of the body will vary over time.
There are 4 broad sub-forms of undernutrition:
- wasting,
- stunting,
- underweight, and
- deficiencies in vitamins and minerals.
Undernutrition makes children in particular much more vulnerable to disease and death.
Low weight-for-height is known as wasting. It usually indicates recent and severe weight loss, because a person has not had enough food to eat and/or they have had an infectious disease, such as diarrhoea, which has caused them to lose weight. A young child who is moderately or severely wasted has an increased risk of death, but treatment is possible.
Low height-for-age is known as stunting. It is the result of chronic or recurrent undernutrition, usually associated with poor socioeconomic conditions, poor maternal health and nutrition, frequent illness, and/or inappropriate infant and young child feeding and care in early life. Stunting holds children back from reaching their physical and cognitive potential.
Children with low weight-for-age are known as underweight. A child who is underweight may be stunted, wasted, or both.
- During pregnancy, adequate nutritional support is crucial for normal growth and development of the fetus. A deficiency in folic acid during pregnancy can cause birth defects and increase the risk of low birth weight and preterm delivery.
- Children can develop a condition called marasmus, a severe deficiency of calories and protein, as a result of a severe shortage of food. Marasmus is characterized by a thin body and stunted growth. If enough calories are given but the food is lacking in protein, a child may develop kwashiorkor, a condition characterized by fluid accumulation (edema), an enlarged liver, apathy, and delayed development. Deficiencies of specific vitamins can also affect bone and tissue formation. A lack of vitamin D, for instance, can affect bone formation, causing rickets in children. Worldwide, about one-third of all childhood deaths are linked to malnutrition. Food shortages and intestinal parasites are leading causes of malnutrition in the developing world. In the U.S., most cases of malnutrition can be attributed to poor or imbalanced diets.
- Acute conditions such as surgery, severe burns, infections, and trauma can drastically increase short-term nutritional requirements. People who have been malnourished for some time may have weakened immune systems and a poorer prognosis. They frequently take longer to heal from surgical procedures and must spend more days in the hospital. For this reason, many doctors screen and then monitor the nutritional status of their hospitalized patients. Patients having surgery are frequently evaluated both prior to surgery and during their recovery process.
- Chronic diseases may be associated with nutrient loss, increased nutrient demand, and/or malabsorption. Malabsorption may occur with chronic diseases such as celiac disease, cystic fibrosis, pancreatic insufficiency, and pernicious anemia. An increased loss of nutrients may be seen with chronic kidney disease, diarrhea and excessive bleeding. Sometimes, both the conditions and their treatment can cause malnutrition through decreased intake. An example of this are the decreased appetite, difficulty swallowing, and nausea associated both with cancer (and chemotherapy). People who chronically abuse drugs and/or alcohol might not get enough nutrients, lose too many nutrients and/or cannot absorb a sufficient amount of nutrients.
- Elderly people require fewer calories but continue to require adequate nutritional support. They are often less able to absorb nutrients due in part to decreased stomach acid production and are more likely to have one or more chronic ailments that may affect their nutritional status. At the same time, they may have more difficulty preparing meals and may have less access to a variety of nutritious foods. Older people also frequently eat less due to a decreased appetite, decreased sense of smell, and/or mechanical difficulties with chewing or swallowing.
Malnutrition signs and symptoms
General malnutrition often develops slowly, over months or years. As the body’s store of nutrients is depleted, changes begin to happen at the cellular level, affecting biochemical processes and decreasing the body’s ability to fight infections. Over time, a variety of symptoms may begin to emerge, including:
- In children, delayed or slow growth, bloated abdomen, listlessness
- Anemia
- Weight loss, decreased muscle mass, and weakness
- Dry scaly skin
- Fluid accumulation (edema)
- Brittle, thinning hair
- Brittle and malformed (spooned) nails
- Chronic diarrhea
- Slow wound healing
- Bone and joint pain
- Mental changes such as confusion and irritability
- Enlarged thyroid gland (goiter)
Specific nutrient deficiencies may cause characteristic symptoms. For instance, vitamin B12 deficiency can lead to tingling, numbness, and burning in the hands and feet (due to nerve damage); a lack of vitamin A may cause night blindness and increased sensitivity to light; and a lack of vitamin D can cause bone pain, malformation, or osteomalacia. The severity of symptoms depends on the intensity and duration of the deficiency. Some changes, such as to bone and nerves, may be irreversible.
Signs of malnutrition
Common signs of malnutrition include:
- unintentional weight loss – losing 5-10% or more of weight over three to six months is one of the main signs of malnutrition
- a low body weight – people with a body mass index (BMI) under 18.5 are at risk of being malnourished
- lack of interest in eating and drinking
- feeling tired all the time
- feeling weaker
- getting ill often and taking a long time to recover
- in children, not growing at the expected rate or not putting on weight as would normally be expected
Other signs of malnutrition include:
- reduced appetite
- lack of interest in food and drinks
- feeling tired all the time
- feeling weaker
- getting ill often and taking a long time to recover
- wounds taking a long time to heal
- poor concentration
- feeling cold most of the time
- low mood or depression
See your doctor if you have these symptoms. If you notice these problems in someone else, try to encourage them to get help.
Symptoms of malnutrition in adults
The main symptom of malnutrition (undernutrition) is unintended weight loss, although this isn’t always obvious.
Weight loss
Most people who are malnourished will lose weight, but it is possible to be a healthy weight or even overweight and still be malnourished.
Someone could be malnourished if:
- they unintentionally lose 5-10% of their body weight within three to six months
- their body mass index (BMI) is under 18.5 (although a person with a BMI under 20 could also be at risk) – use the BMI calculator to work out your BMI
- clothes, belts and jewellery seem to become looser over time
See your doctor if you’ve unintentionally lost a lot of weight over the last few months.
If you notice a friend or family member has lost lots of weight, talk to them about your concerns and encourage them to get help.
Malnutrition symptoms in children
Symptoms of malnutrition in a child can include:
- not growing at the expected rate or not putting on weight as would normally be expected (faltering growth)
- changes in behavior, such as being unusually irritable, slow or anxious
- low energy levels and tiring more easily than other children
Contact your doctor if you’re concerned about your child’s health or development at any point.
Causes of malnutrition
Malnutrition (undernutrition) is caused by a lack of nutrients in your diet, either due to a poor diet or problems absorbing nutrients from food.
Certain things can increase a person’s risk of becoming malnourished.
Health conditions
Some conditions that can lead to malnutrition include:
- long-term conditions that cause loss of appetite, feeling sick, vomiting and/or changes in bowel habit (such as diarrhea) – these include cancer, liver disease and some lung conditions (such as chronic obstructive pulmonary disease)
- mental health conditions, such as depression or schizophrenia, which may affect your mood and desire to eat
- conditions that disrupt your ability to digest food or absorb nutrients, such as Crohn’s disease or ulcerative colitis
- dementia, which can cause the person to neglect their wellbeing and forget to eat
- an eating disorder, such as anorexia
You can also become malnourished if your body needs an increased amount of energy – for example, if it’s healing after surgery or a serious injury such as a burn, or if you have involuntary movements such as a tremor.
Medicines
Some types of medication may increase your risk of developing malnutrition.
Some medicines have unpleasant side effects – such as loss of appetite, diarrhea or nausea – that could mean you eat less or don’t absorb as many nutrients from your food.
Physical and social factors
The following factors can also contribute to malnutrition:
- teeth that are in a poor condition, or dentures that don’t fit properly, which can make eating difficult or painful
- a physical disability or other impairment that makes it difficult to move around, cook or shop for food
- living alone and being socially isolated
- having limited knowledge about nutrition or cooking
- alcohol or drug dependency
- low income or poverty
Causes of malnutrition in children
In the US, malnutrition in children is commonly caused by long-term health conditions that:
- cause lack of appetite
- disrupt digestion
- increase the body’s demand for energy
Examples of these types of conditions include childhood cancers, congenital heart disease, cystic fibrosis and cerebral palsy.
Some children may become malnourished because of an eating disorder or a behavioral or psychological condition that means they avoid or refuse food.
Malnutrition as a result of a poor diet is rare in the US, but may occur if a child is neglected, living in poverty or being abused.
Nutrient deficiency test
Malnutrition will often be noticeable to the doctor’s trained eye before it causes significant abnormalities in laboratory test results. During physical examinations, a health practitioner will evaluate an individual’s overall appearance: their skin and muscle tone, the amount of body fat they have, their height and weight, and their eating habits. In the case of infants and children, doctors will look for normal development and a normal rate of growth.
If there are signs of malnutrition, a healthcare practitioner may order laboratory screening tests to evaluate a person’s blood and organ function. Additional individual tests may be ordered to look for specific vitamin and mineral deficiencies. If general malnutrition and/or specific deficiencies are diagnosed, then laboratory testing may be used to monitor the response to therapy. A person who has malnutrition because of a chronic disease may need to have his or her nutritional status monitored on a regular basis.
Hospitalized patients are often assessed for nutritional status prior to or at the time of admission. This may include a history, an interview by a dietician, and laboratory tests. If the results of these tests indicate possible nutritional deficits, patients may be provided nutritional support prior to a surgery or procedure and be monitored regularly during recovery.
Laboratory tests may include:
For general screening and monitoring:
- Lipid panel
- CBC (complete blood count)
- CMP (comprehensive metabolic panel)
- Albumin
- Total protein
For nutritional status and deficiencies:
- Iron tests such as serum iron, transferrin and iron-binding capacity, and ferritin
- Vitamins and trace minerals such as B12 and folate, vitamin A, vitamin D, B vitamins, calcium, and magnesium
- Prealbumin: although commonly used as a marker of malnutrition, levels of this protein may be affected by a number of conditions other than malnutrition. Research is continuing in order to better understand the role(s) of prealbumin in the body, especially the reasons for changes observed during illness, and the clinical utility of prealbumin testing.
- Albumin has been used in the past along with or instead of prealbumin to evaluate nutritional status but now is more often used to screen for and help diagnose liver or kidney disease.
- Leptin: suppressed levels may indicate malnutrition in some patients; this test is not widely available.
- Celiac disease blood tests measure the amount of particular antibodies in the blood. The most common tests include anti-tissue transglutaminase (tTG), IgA class, quantitative immunoglobulin A (IgA) test, and deamidated gliadin peptide antibodies (anti-DGP), IgA or IgG.
Non-laboratory tests
Imaging and radiographic scans may be ordered to help evaluate the health of internal organs and the normal growth and development of muscles and bones. These tests may include:
- X-rays
- CT (Computed Tomography)
- MRI (Magnetic Resonance Imaging)
Malnutrition treatment
Treatment for malnutrition (undernutrition) depends on the underlying cause and how malnourished the person is.
They may be given advice to follow at home, or they may be supported at home by a dietitian or other qualified healthcare professional. In severe cases, treatment in hospital may be needed.
Dietary changes and supplements
A dietitian will advise about dietary changes that can help.
They may create a tailored diet plan that ensures the person gets enough nutrients.
They may also suggest:
- having a healthier, more balanced diet
- eating “fortified” foods that contain extra nutrients
- snacking between meals
- having drinks that contain lots of calories
- getting home supermarket deliveries
If these measures aren’t enough, taking extra nutrients in the form of supplements may be advised. These should only be taken on the advice of a healthcare professional.
Feeding tubes
For people who are unable to eat enough to meet their body’s needs – for example because they have swallowing problems – an alternative way of getting nutrients may be needed.
This can include:
- a tube that’s passed down the nose and into the stomach – called a nasogastric tube
- a tube that’s placed directly into the stomach or gut through the skin of the tummy – called a PEG (percutaneous endoscopic gastrostomy) tube
- a solution containing nutrients being fed directly into the blood through a tube in a vein – known as parenteral nutrition
These treatments are usually first started in hospital, but they can be continued at home if the person is well enough.
How swallowing problems (dysphagia) are treated
Most swallowing problems can be managed, although the treatment you receive will depend on the type of dysphagia you have.
Treatment will depend on whether your swallowing problem is in the mouth or throat (oropharyngeal dysphagia), or in the esophagus (esophageal dysphagia).
The cause of dysphagia is also considered when deciding on treatment or management. In some cases, treating the underlying cause, such as mouth cancer or esophageal cancer, can help relieve swallowing problems.
Treatment for dysphagia may be managed by a group of specialists that may include a speech and language therapist, a dietitian and, possibly, a surgeon.
Treatments for oropharyngeal dysphagia
Oropharyngeal dysphagia can be difficult to treat if it’s caused by a condition that affects the nervous system. This is because these problems can’t usually be corrected using medication or surgery.
There are 3 main ways oropharyngeal dysphagia is managed to make eating and drinking as safe as possible:
- swallowing therapy
- dietary changes
- feeding tubes
Swallowing therapy
You may be referred to a speech and language therapist for swallowing therapy. A speech and language therapist is trained to work with people with eating or swallowing difficulties.
Speech and language therapists use a range of techniques that can be tailored for your specific problem, such as teaching you swallowing exercises.
Dietary changes
You may be referred to a dietitian for advice about changes to your diet to make sure you receive a healthy, balanced diet.
A speech and language therapist can give you advice about softer foods and thickened fluids that you may find easier to swallow. They may also try to ensure you’re getting the support you need at meal times.
Feeding tubes
Feeding tubes can be used to provide nutrition while you’re recovering your ability to swallow. They may also be required in severe cases of dysphagia that put you at risk of malnutrition and dehydration.
A feeding tube can also make it easier for you to take the medication you may need for other conditions.
There are 2 types of feeding tubes:
- a nasogastric tube – a tube passed through your nose and down into your stomach
- a percutaneous endoscopic gastrostomy (PEG) tube – a tube is implanted directly into your stomach
Nasogastric tubes are designed for short-term use. The tube will need to be replaced and swapped to the other nostril after about a month.
PEG tubes are designed for long-term use and last several months before they need replacing.
Most people with dysphagia prefer to use a PEG tube because it can be hidden under clothing. However, they carry a greater risk of minor complications, such as skin infection or blocked tube, compared to nasogastric tubes.
Two major complications of PEG tubes are infection and internal bleeding.
You can discuss the pros and cons of both types of feeding tubes with your treatment team.
Treatments for esophageal dysphagia
Esophageal dysphagia is swallowing difficulties due to problems with the oesophagus.
Medication
Depending on the cause, it may be possible to treat esophageal dysphagia with medication. For example, proton pump inhibitors (PPIs) used to treat indigestion may improve symptoms caused by narrowing or scarring of the esophagus.
Botox
Botox can sometimes be used to treat achalasia, a condition where the muscles in the esophagus become too stiff to allow food and liquid to enter the stomach.
Botox can be used to paralyze the tightened muscles that prevent food from reaching the stomach. However, the effects only last for around 6 months.
Surgery
Other cases of esophageal dysphagia can usually be treated with surgery.
Endoscopic dilatation
Endoscopic dilation is widely used to treat dysphagia caused by obstruction. It can also be used to stretch your esophagus if it’s scarred.
Endoscopic dilatation will be carried out during an internal examination of your esophagus using an endoscopy.
An endoscope (a thin tube with a light and a camera at one end) is passed down your throat and into your esophagus and images of the inside of your body are transmitted to a television screen.
Using the image as guidance, a small balloon or a bougie (a thin, flexible medical instrument) is passed through the narrowed part of your esophagus to widen it.
If a balloon is used, it will gradually be inflated to widen your esophagus before being deflated and removed.
You may be given a mild sedative before the procedure to relax you. There’s a small risk that the procedure could cause a tear or perforation to your esophagus.
Inserting a stent
If you have esophageal cancer that can’t be removed, it’s usually recommended that you have a stent inserted instead of endoscopic dilatation. This is because, if you have cancer, there’s a higher risk of perforating your esophagus if it’s stretched.
A stent (usually a metal mesh tube) is inserted into your esophagus during an endoscopy or under X-ray guidance.
The stent then gradually expands to create a passage wide enough to allow food to pass through. To keep the stent open without blockages, you’ll need to follow a particular diet.
Treatments for babies born with dysphagia
If your baby is born with difficulty swallowing (congenital dysphagia), their treatment will depend on the cause.
Cerebral palsy – a speech and language therapist will teach your child how to swallow, how to adjust the type of food they eat and how to use feeding tubes.
Cleft lip and palate – this is usually treated with surgery.
Narrowing of the esophagus – may be treated with a type of surgery called dilatation to widen the esophagus.
Breastfeeding or bottle feeding
Gastro-esophageal reflux disease (GERD) – can be treated using special thickened feeds instead of your usual breast or formula milk. Sometimes medication may also be used.
If you’re having difficulty bottle feeding or breastfeeding your baby:
- see your midwife, health visitor or doctor
- see breastfeeding help and support and bottle feeding advice.
- Elia M and Russell CA. Combating Malnutrition: Recommendations for Action. Report from the advisory group on malnutrition, led by BAPEN. 2009.
- Stratton RJ et al. Disease-related malnutrition: an evidence-based approach to treatment. Oxford: CABI publishing; 2003.
- Shaw C. Nutrition and Palliative Care Chapter 10. In Nutrition and Cancer. Wiley Blackwell 2011
- Meijers et al (2012). Predicting falls in elderly receiving home care: The role of malnutrition and impaired mobility, Journal of Nutrition, Health and Aging 16(7): 654-658
- Gossier S, Guyonnet S and Volkert D. The Role of Nutrition in Frailty: An Overview. The Journal of Frailty & Aging 2016; 5,2
- A Guide to Managing Adult Malnutrition in the Community 2nd Edition: 2017 https://www.malnutritionpathway.co.uk/library/managing_malnutrition.pdf
- Sight & Life: Micronutrients; Macro Impact, the Story of Vitamins and a Hungry World, 2011 https://issuu.com/sight_and_life/docs/micronutriens_macro_impact
- Investing in the future: A united call to action on vitamin and mineral deficiencies. Global Report 2009 p. 1 http://www.unitedcalltoaction.org/
- Investing in the future: A united call to action on vitamin and mineral deficiencies. Global Report 2009 p. 5 http://www.unitedcalltoaction.org/
- Stevens GA, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995—2011: a systematic analysis of population-representative data. The Lancet Global Health, Volume 1, Issue 1, Pages e16 – e25, July 2013. https://www.thelancet.com/pdfs/journals/langlo/PIIS2214-109X(13)70001-9.pdf
- WHO Guideline: Intermittent iron and folic acid supplementation in menstruating women. http://www.who.int/nutrition/publications/micronutrients/guidelines/guideline_iron_folicacid_suppl_women/en/
- Copenhagen Consensus 2012: Solving the World’s Challenges. https://www.copenhagenconsensus.com/guide-giving/gtg-micronutrient-fortification-and-biofortification-challenge
- Investing in the future: A united call to action on vitamin and mineral deficiencies. Global Report 2009 p. 9 http://www.unitedcalltoaction.org/
- Zimmermann MB. Iodine Deficiency. Endocrine Reviews, June 2009, 30(4):376–408
- Zimmermann MB; Andersson M. Assessment of iodine nutrition in populations: past, present, and future. Nutr Rev. 2012 Oct; 70(10):553-70
- UNICEF – Improving Child Nutrition: The Achievable Imperative for Global Progress 2013, pg23 https://www.unicef.org/media/files/nutrition_report_2013.pdf
- Wessells KR, Brown KH. Estimating the Global Prevalence of Zinc Deficiency: Results Based on Zinc Availability in National Food Supplies and the Prevalence of Stunting. PLoS ONE 2013 7(11): e50568
- Investing in the future: A united call to action on vitamin and mineral deficiencies. Global Report 2009 p. 6 http://www.unitedcalltoaction.org/
- Zimmerman, SL. Fifteen Years of Fortifying With Folic Acid. SIGHT AND LIFE; Vol. 25 (3): 2011 https://sightandlife.org/wp-content/uploads/2017/04/sal_25032011.pdf