Medullary cystic kidney disease
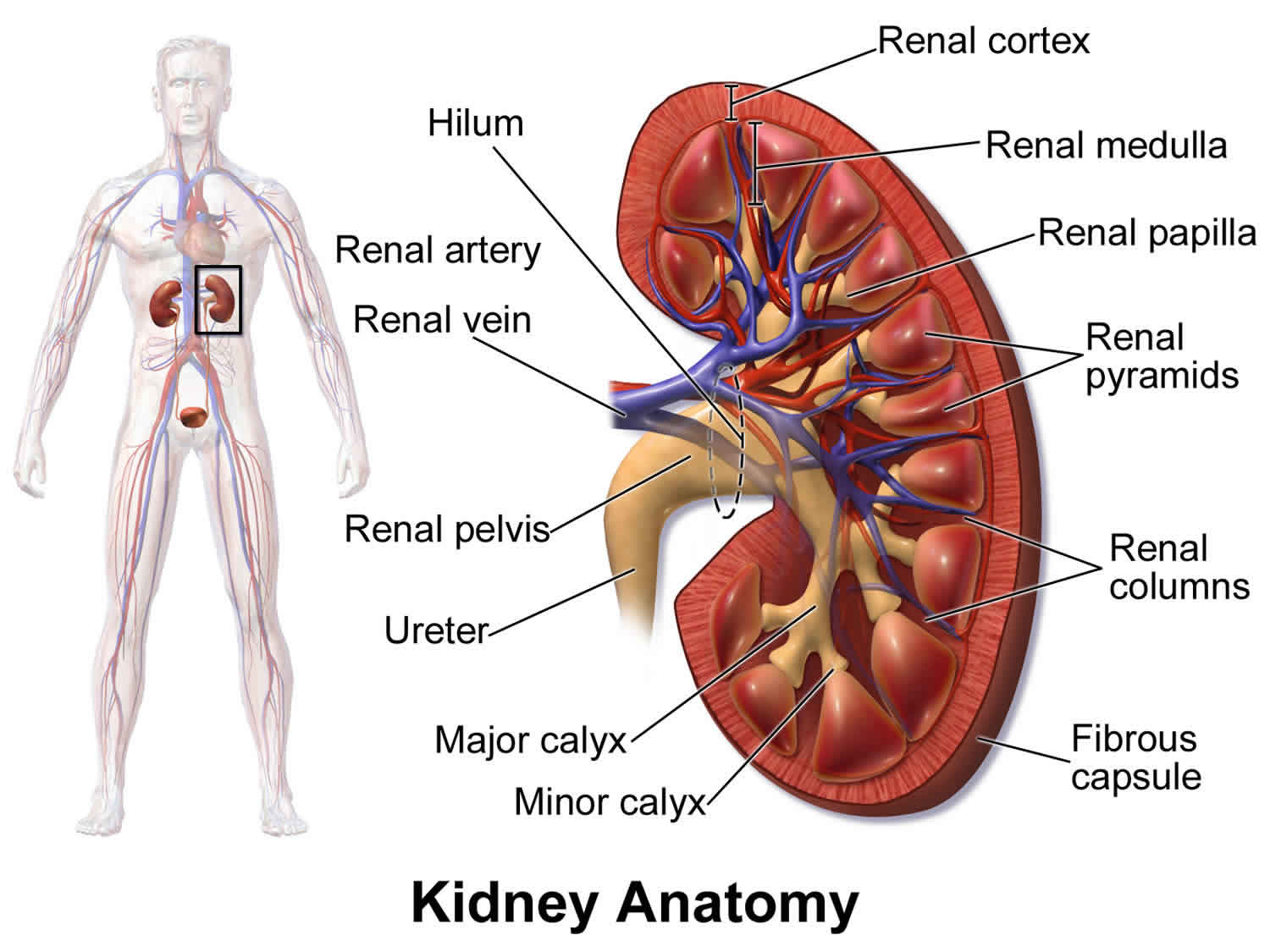
Medullary cystic kidney disease also called autosomal dominant tubulointerstitial kidney disease, is very rare group of diseases that affect the tubules of the kidney 1. Medullary cystic kidney disease is characterized by cysts in the inner portions of the kidney, is inherited in an autosomal dominant pattern, and commonly results in kidney failure at a very young age. If you have this disease, you will need to see a pediatric nephrologist. Adult nephrologists do not commonly see this disease. You may even require genetic testing. You should see a genetic specialist to see if the proper diagnosis has been made.
Medullary cystic kidney disease have the following characteristics:
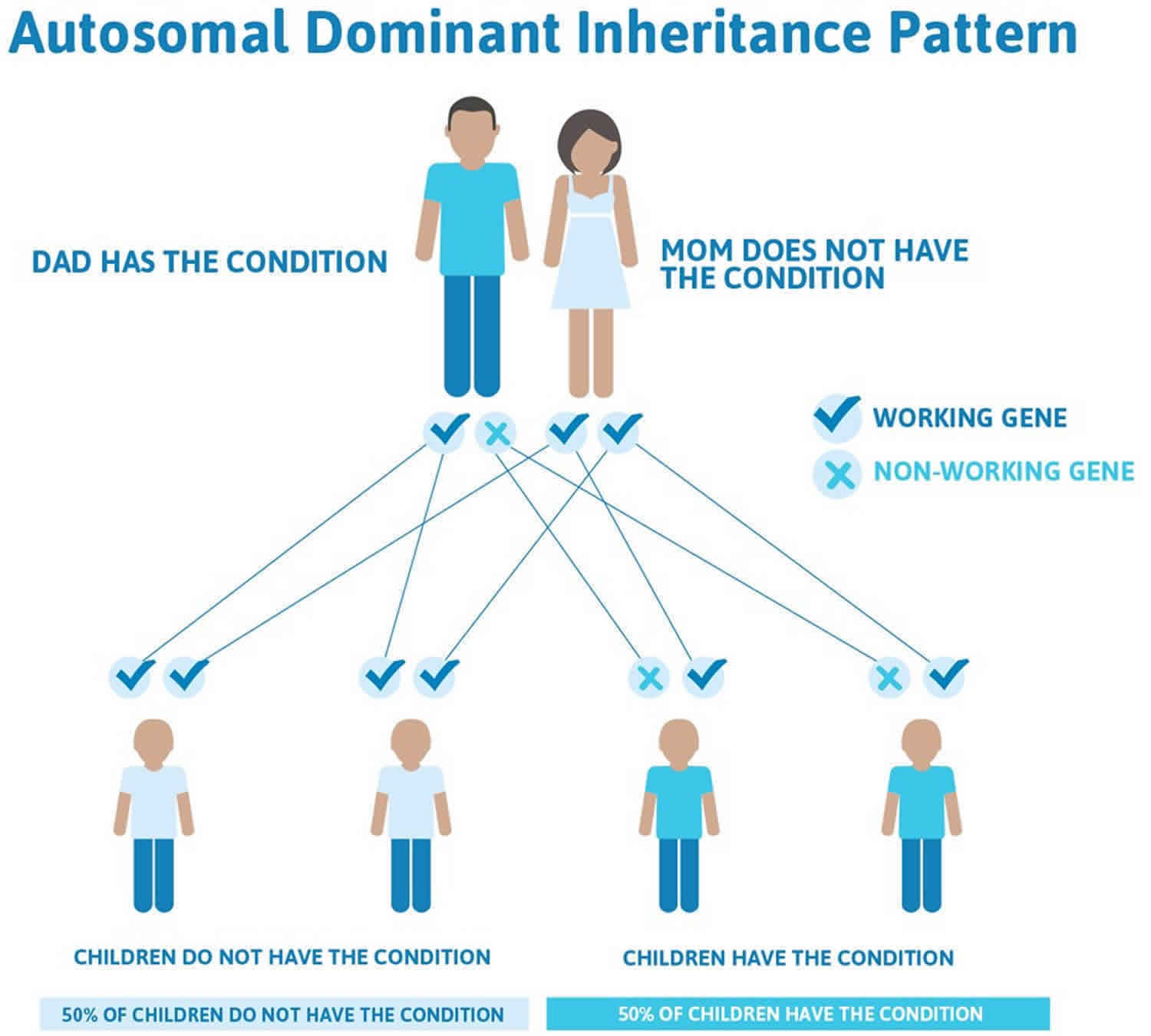
- Medullary cystic kidney disease (autosomal dominant tubulointerstitial kidney disease) are inherited in an autosomal dominant manner; this means that a parent has a 50% chance of passing the disease on to their children. Often many family members are affected.
- Chronic kidney disease develops. This initially is noticed as an elevated blood creatinine level. There are no symptoms from an elevated creatinine until it is very high, so often the elevated creatinine is found out on blood testing at a doctor’s office or in the hospital. Often, doctors are uncertain why the creatinine is elevated. As chronic kidney disease progresses, and the creatinine rises more, patients develop symptoms of fatigue, anemia, and feel cold all the time. Decreased appetite and fluid retention develop as the patient nears the need for dialysis.
- Dialysis or kidney transplant is required sometime between the 4th and 7th decade of life.
- Several types of the disease are associated with elevated uric acid concentrations in blood and gout, which sometimes starts in the teenage years. In ADTKD-UMOD and ADTKD- REN, some – but not all – family members are affected by gout.
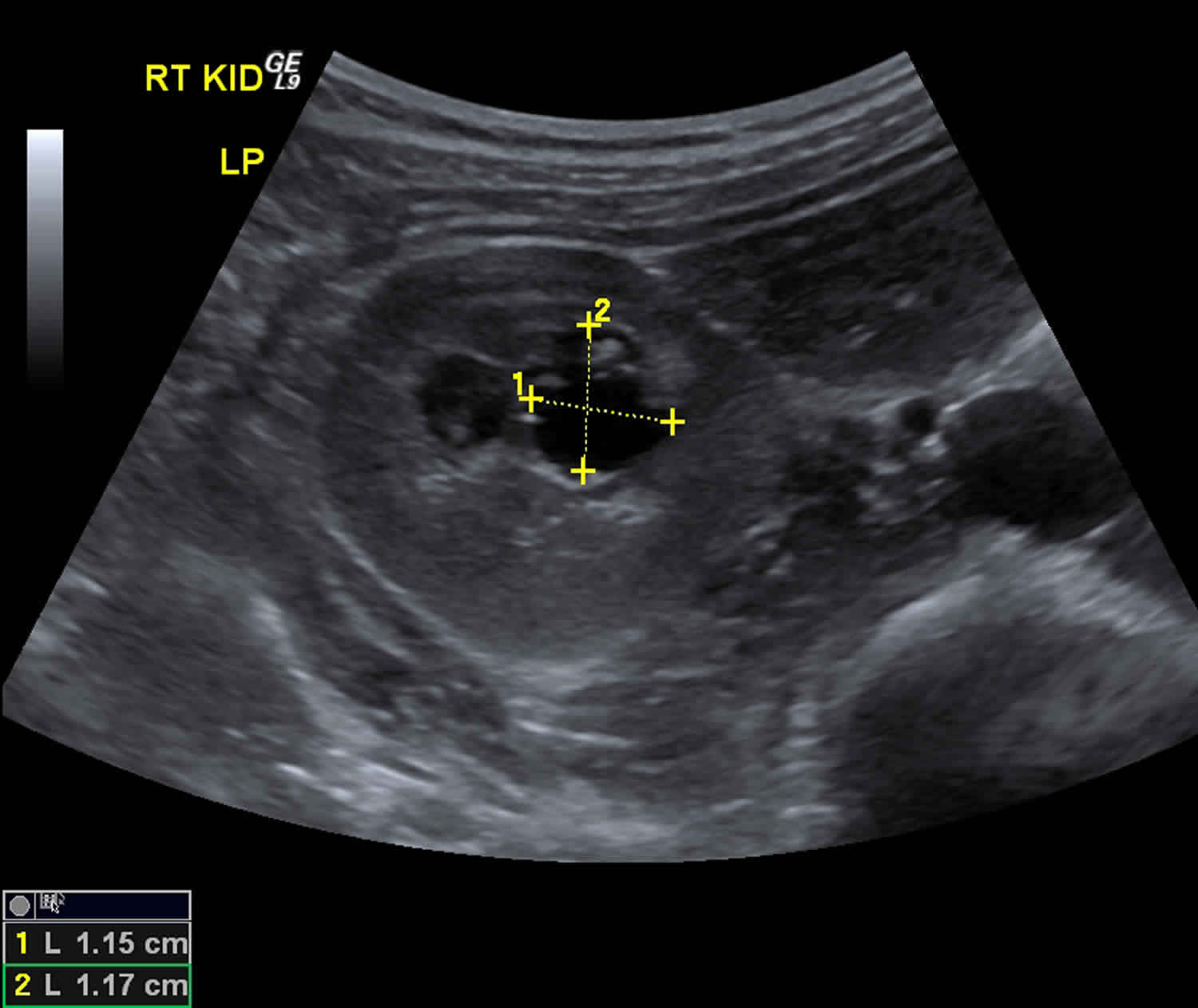
Signs and symptoms of all forms of medullary cystic kidney disease include slowly worsening kidney disease (often becoming apparent by the teenage years) that ultimately results in end-stage kidney disease at some time between the ages of 20 and 70, depending on the genetic cause and severity. Urine exams of people with medullary cystic kidney disease show a bland urinary sediment (little blood or little or no protein). Kidney ultrasound examination is generally normal early in the disease course, but some people with medullary cystic kidney disease have cysts in the center of the kidneys (medullary cysts) that may be seen on an ultrasound 1.
There are 3 known subtypes of medullary cystic kidney disease, which are classified based on their genetic causes and presence of additional features 2:
- UMOD-related autosomal dominant tubulointerstitial kidney disease (ADTKD-UMOD) also known as uromodulin kidney disease (formerly known as UMOD-associated kidney disease, familial juvenile hyperuricemic nephropathy type 1, medullary cystic kidney disease type 2, and uromodulin storage disease) 3. Uromodulin kidney disease (ADTKD-UMOD) is the most common form of this condition. It is caused by a mutation in the UMOD gene producing a protein called uromodulin. This protein is only made in the kidney. The age of onset varies but kidney problems are usually noted in adolescence,and may progress to end-stage renal disease (ESRD) between the fourth and seventh decades of life. High levels of uric acid in the blood (hyperuricemia) and gout (a form of arthritis), sometimes occur as early as the teenage years.
- REN-related autosomal dominant tubulointerstitial kidney disease (ADTKD-REN) previously known as “familial juvenile hyperuricemic nephropathy type 2” 4. ADTKD-REN is caused by mutations in the REN gene producing a protein called renin. Kidney disease is usually present in childhood. Many people with this subtype also have anemia in childhood (even before kidney disease begins), low or low-normal blood pressure, mildly high levels of potassium in the blood (hyperkalemia), hyperuricemia and gout.
- MUC1-related autosomal dominant tubulointerstitial kidney disease (ADTKD-MUC1) or Mucin-1 kidney disease or previously known as “medullary cystic kidney disease type 1”. ADTKD-MUC1 (MUC1 kidney disease) is due to mutations in the gene producing the protein mucin-1 5. It is characterized by slowly progressive chronic kidney disease that leads to end-stage renal disease (ESRD) occurring at any age between 20 and 70 years. They do not have any symptoms when they are young, but as they get older, their kidney function declines, and affected individuals usually require dialysis or a kidney transplant between the 3rd and seventh decades of life. There are no other systemic features in addition to chronic kidney disease, although some develop gout in adulthood.
- In some cases, the genetic cause of medullary cystic kidney disease in a family is not known. Autosomal dominant tubulotubulointerstitial kidney disease of unknown genetic cause is the term used to describe families with this disease in whom the cause is not known. These individuals usually have chronic kidney disease but do not have gout. Researchers are now trying to find the cause of this disease.
Inheritance of medullary cystic kidney disease is autosomal dominant, as the name implies. Most people with medullary cystic kidney disease have a family history of “kidney disease” (if not a family history of medullary cystic kidney disease specifically) or some of the other symptoms. The diagnosis of medullary cystic kidney disease may be suspected based on family history, symptoms, and laboratory tests, and it can be confirmed by genetic testing.
Treatment for kidney disease in people with medullary cystic kidney disease generally follows standard guidelines for chronic kidney disease and may involve kidney transplantation, which cures the disease 4. The disease does not recur in the transplanted kidney. Other treatments depend on the symptoms in each person. For example, gout may be treated with allopurinol. High meat and seafood intake could worsen gout 3. Treatment of anemia depends on whether it is causing symptoms. Those with ADTKD-REN are advised to avoid a low-sodium diet and non-steroidal anti-inflammatory drugs 4.
Figure 1. Medullary cystic kidney disease ultrasound
Medullary cystic kidney disease causes
All types of medullary cystic kidney disease follow autosomal dominant inheritance. Dominant genetic disorders occur when only a single copy of an abnormal gene is necessary to cause a particular disease. We all have two copies of each gene. Individuals with medullary cystic kidney disease have one normal copy and one abnormal copy. The parent has a 50/50 chance of passing the abnormal gene on to their child. Thus, children of an affected individual have a 50/50 chance of having the disease. The risk is the same for males and females. There are usually a number of family members affected, with at least a parent and child almost always affected.
ADTKD-UMOD is caused by a mistake (mutation) in a gene that encodes the protein called uromodulin. The abnormal protein builds up in kidney cells and causes slow progression of kidney disease. The reason why affected individuals develop gout is unclear, but likely related to improper function of kidney cells and/or abnormally low amounts of the uromodulin in sites where it is needed.
ADTKD-REN is caused by a mutation in a gene that encodes the protein called renin. The abnormal protein either builds up in kidney cells or is not produced in substantial amounts when needed, and this causes slow progression of kidney disease. Because affected individuals have low amounts of normal renin, patients may have mildly low blood pressure and mildly high potassium levels.
ADTKD-MUC1 is caused by a mutation in the gene that encodes mucoprotein-1. Mucoprotein-1 is a protein that is made in many of the cells of the body and provides a protective lining to the stomach, lungs, kidney tubules, and many other areas of the body. For some reason, the mutation only leads to problems in the kidney, and every other organ/tissue is completely normal.
Autosomal dominant tubulointerstitial kidney disease of unknown cause is caused by a mutation in a gene, but the gene that causes the disease is not yet known.
Figure 2. Medullary cystic kidney disease autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Medullary cystic kidney disease symptoms
All individuals with medullary cystic kidney disease show slow loss of kidney function that may be present as early as childhood. Patients may first be diagnosed with this disease when they are found to have an elevated blood creatinine level (measure of kidney function) on a routine blood test at their doctor’s office. For many individuals, there may be no other symptoms. Doctors will check the urine, and will find that it does not contain blood and little or no protein. A kidney ultrasound is usually normal, and even a kidney biopsy may not point to a cause for this condition. Doctors are often confused because the patient has an elevated creatinine but the urine tests and the kidney ultrasound look normal. Thus, medullary cystic kidney disease is frequently not properly diagnosed. The kidney disease progresses slowly, and patients eventually develop symptoms of kidney failure (nausea, fluid retention) and require dialysis or kidney transplant. The age that kidney transplant or dialysis is required is highly variable, with some individuals requiring it as early as age 17, while other family members may not even require it at age 70. The reason for this variation is unclear.
Individuals with ADTKD-MUC1 only have symptoms of chronic kidney disease progression and do not suffer from other distinctive symptoms, making this form of the disease even more difficult to diagnose.
In addition to chronic kidney disease, patients with ADTKD-UMOD have elevated levels of blood uric acid that can lead to gout. Gout is a form of arthritis (joint inflammation) that commonly affects the big toe, knee, elbow, or other joints. Gout is usually a disease of middle-aged men. Therefore, gout may be misdiagnosed in teenagers with this condition. When gout is diagnosed, doctors frequently are unsure why the gout is present. While many families with ADTKD-UMOD have gout, it is not present in all families.
In addition to high uric acid levels, gout, and chronic kidney disease, Individuals with ADTKD-REN all suffer from anemia early in life, being present as early as one year of age. Anemia usually resolves during adolescence but returns when kidney failure worsens (usually in the 30’s or 40’s). Often, the cause of the anemia is not known when diagnosed. Patients also tend to have low blood pressures and high blood potassium levels. Some, but not all, affected individuals produce more than normal amounts of urine, which can result in bed-wetting in childhood.
Individuals with autosomal dominant tubulointerstitial kidney disease of unknown genetic cause are similar to those with disease due to MUC1 mutations, in that the only symptom is slowly progressive kidney disease.
Medullary cystic kidney disease diagnosis
Several lab tests are very helpful in pointing to this diagnosis. First, a blood test is done to measure the blood creatinine. In this condition, the blood creatinine is usually elevated, beginning in the second decade of life. A blood uric acid level is also tested and is almost always elevated in ADTKD-UMOD and ADTKD-REN (though not elevated early on in ADTKD-MUC1). A urine test (urinalysis) is done. The absence of blood or protein in the urine rules out other possible causes of kidney damage. Thus, most individuals with this condition have high blood creatinine levels, and a normal urinalysis. A kidney ultrasound is also frequently done and usually shows normal kidneys, though some individuals may be found to have cysts in the middle of the kidney. The real key to the diagnosis is that a parent and a child are usually both affected with kidney disease. Kidney biopsy may be performed, but the kidney biopsy cannot specifically diagnose medullary cystic kidney disease: genetic testing is required.
Molecular genetic testing is available for ADKTD-MUC1, ADTKD-UMOD, and ADTKD-REN. Genetic testing for ADTKD-UMOD and ADTKD-REN is available in commercial laboratories. ADTKD-MUC1 testing is available at present free of charge from the Broad Institute, Boston, Massachusetts. In order to arrange for this testing, please contact Anthony Bleyer MD at [email protected]
If no mutations are found, individuals have autosomal dominant tubulointerstitial kidney disease of unknown genetic cause. Further genetic testing can be done at academic medical centers to help diagnose this disease.
Medullary cystic kidney disease treatment
Many affected individuals with ADTKD-UMOD and ADTKD-REN suffer from gout beginning in the teenage years. The gout is easily treated with a medication called allopurinol. Allopurinol is a medicine that is commonly used in the treatment of gout. It has been used for many years and by thousands of patients with gout. Patients occasionally have allergies to the medication, which rarely are severe. This medication easily controls gout in affected individuals. In uromodulin kidney disease, gout, if untreated, will continue and worsen over time. Therefore, early treatment is advisable. Febuxostat is an alternative to allopurinol. Both febuxostsat and allopurinol should be stopped immediately in pregnancy is considered or becoming pregnant is possible. There are other uric acid lowering therapies that can be considered and discussed with the treating physician.
Some doctors believe that allopurinol can slow progression of kidney disease in ADTKD-UMOD, even in patients who do not have gout. It is not clear if allopurinol slows progression of disease. It does not appear to stop progression of the kidney disease entirely.
For ADTKD-MUC1 and ADTKD-REN, there are a group of medications called angiotensin converting enzyme (ACE) inhibitors that have been shown to slow progression of kidney failure in many kidney diseases. It is unclear if they slow progression of disease in uromodulin kidney disease, but it is possible.
For patients with ADTKD-REN who have mildly high blood potassium and mildly low blood pressures, the medication fludrocortisone may be an effective treatment. This treatment was found to improve kidney function in one child with this disease, but did not have an effect on an older patient with advanced kidney disease. It is very important that patients with ADTKD-REN are NOT put on a low sodium diet, as this could worsen kidney function.
Anemia occurring in childhood with ADTKD-REN may be treated with a medication called erythropoietin. This medication is given as a shot once every week or every other week and will correct the anemia. However, the anemia is usually mild and asymptomatic and may not require therapy.
There are no specific treatments for ADTKD-MUC1 or medullary cystic kidney disease of unknown genetic cause.
Individuals with renin mutations should avoid non-steroidal anti-inflammatory agents such as ibuprofen (Advil, Aleve) or naprosyn.
References- Autosomal dominant tubulointerstitial kidney disease (medullary cystic kidney disease). https://www.uptodate.com/contents/autosomal-dominant-tubulointerstitial-kidney-disease-medullary-cystic-kidney-disease
- Autosomal Dominant Tubulo-Interstitial Kidney Disease. https://rarediseases.org/rare-diseases/autosomal-dominant-interstitial-kidney-disease
- Bleyer AJ, Hart PS, Kmoch S. Autosomal Dominant Tubulointerstitial Kidney Disease, UMOD-Related. 2007 Jan 12 [Updated 2016 Jun 30]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1356
- Kmoch S, Živná M, Bleyer AJ. Autosomal Dominant Tubulointerstitial Kidney Disease, REN-Related. 2011 Apr 5 [Updated 2015 Dec 29]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK53700
- Bleyer AJ, Kmoch S. Autosomal Dominant Tubulointerstitial Kidney Disease, MUC1-Related. 2013 Aug 15 [Updated 2016 Jun 30]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK153723