Moon face
Moon face is a medical sign in which the face develops a rounded appearance due to fat deposits on the sides of the face. Moon face is often associated with Cushing’s syndrome or steroid treatment (especially corticosteroids) called iatrogenic Cushing’s syndrome, which has led to it being known as Cushingoid facies.
Cushing syndrome occurs when your body is exposed to high levels of the hormone cortisol for a long time. Cushing syndrome, sometimes called hypercortisolism, may be caused by the use of oral corticosteroid medication. The condition can also occur when your body makes too much cortisol on its own.
Too much cortisol can produce some of the hallmark signs of Cushing syndrome — a fatty hump between your shoulders, a moon face, and pink or purple stretch marks on your skin. Cushing syndrome can also result in high blood pressure, bone loss and, on occasion, type 2 diabetes.
Treatments for Cushing syndrome can return your body’s cortisol production to normal and noticeably improve your symptoms. The earlier treatment begins, the better your chances for recovery.
The signs and symptoms of Cushing syndrome can vary depending on the levels of excess cortisol.
Common signs and symptoms of Cushing syndrome
- Weight gain and fatty tissue deposits, particularly around the midsection and upper back, in the face (moon face), and between the shoulders (buffalo hump)
- Pink or purple stretch marks (striae) on the skin of the abdomen, thighs, breasts and arms
- Thinning, fragile skin that bruises easily
- Slow healing of cuts, insect bites and infections
- Acne
Signs and symptoms women with Cushing syndrome may experience:
- Thicker or more visible body and facial hair (hirsutism)
- Irregular or absent menstrual periods
Signs and symptoms men with Cushing syndrome may experience:
- Decreased libido
- Decreased fertility
- Erectile dysfunction
Other signs and symptoms that may occur with Cushing syndrome:
- Severe fatigue
- Muscle weakness
- Depression, anxiety and irritability
- Loss of emotional control
- Cognitive difficulties
- New or worsened high blood pressure
- Headache
- Increased pigmentation of the skin
- Bone loss, leading to fractures over time
- In children, impaired growth
Figure 1. Cushing syndrome moon face
Footnote: Cushing’s syndrome manifestations on a 10-year old. (a) Moon face, facial erythema, acne. (b) Dorsal cervical fat pad and neck acanthosis nigrican. (c) Axillary acanthosis nigrican. (d) Truncal obesity.
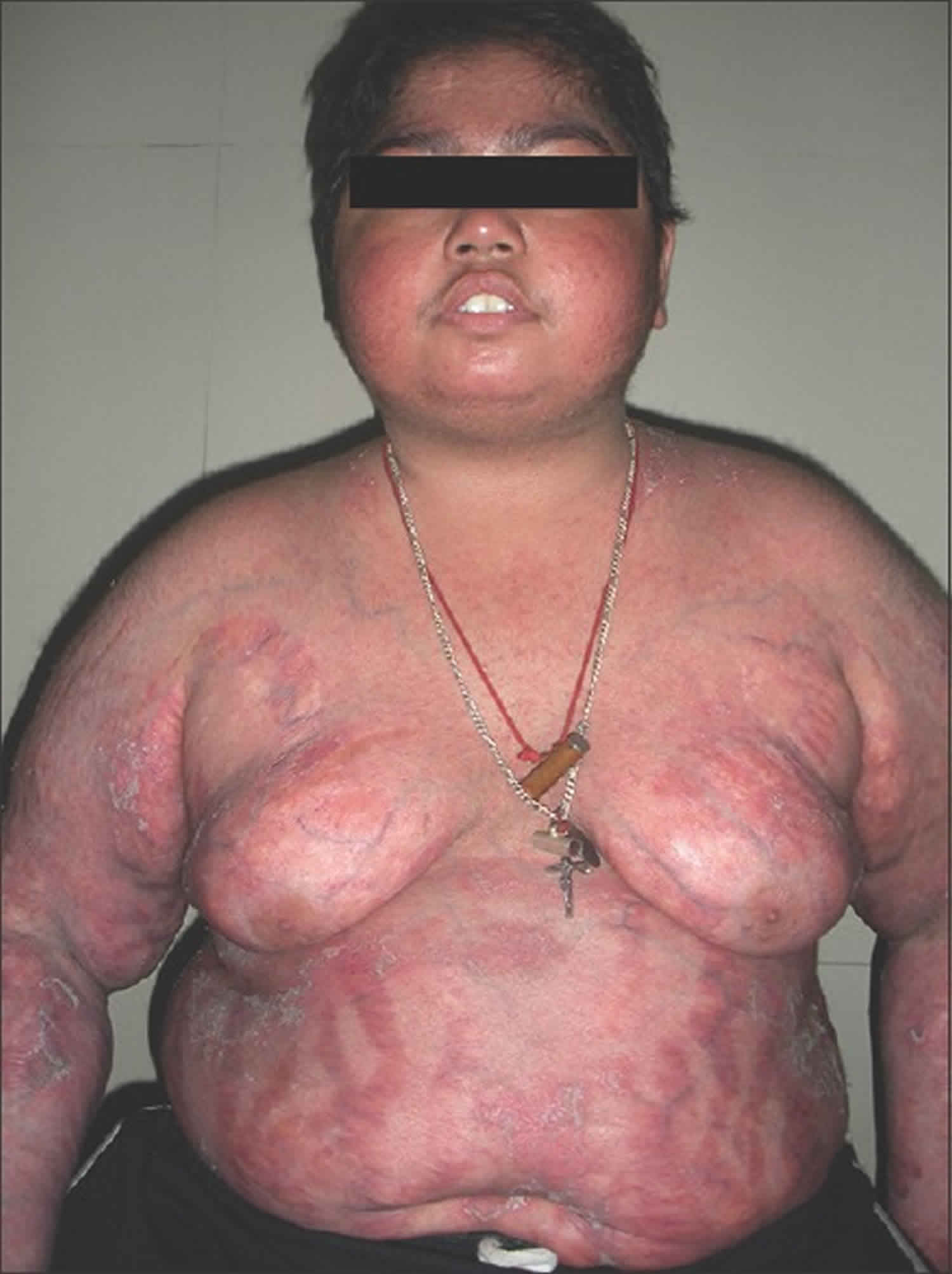
[Source 1 ]Figure 2. Iatrogenic Cushing’s syndrome moon face
Footnote: A 15-year-old young male who developed iatrogenic Cushing’s syndrome after use of topical clobetasol propionate. Broad pink striae were present over the abdomen and thighs along with psoriatic skin lesions. He had bilateral gynecomastia and bilateral small testis (3 ml) and Tanner stage 2 pubic hair. He had significant proximal muscle weakness of lower limbs with preservation of deep tendon reflexes.
[Source 2 ]Cushing syndrome causes
Excess levels of the hormone cortisol are responsible for Cushing syndrome. Cortisol, which is produced in the adrenal glands, plays a variety of roles in your body.
For example, cortisol helps regulate your blood pressure, reduces inflammation, and keeps your heart and blood vessels functioning normally. Cortisol helps your body respond to stress. It also regulates the way you convert (metabolize) proteins, carbohydrates and fats in your diet into usable energy.
However, when the level of cortisol is too high in your body, you may develop Cushing syndrome.
Corticosteroid medications
Cushing syndrome can develop from a cause outside of your body (exogenous Cushing syndrome). One example is taking oral corticosteroid medications in high doses over an extended period of time. These medications, such as prednisone, have the same effect in the body as does cortisol produced by your body.
Oral corticosteroids may be necessary to treat inflammatory diseases, such as rheumatoid arthritis, lupus and asthma. It may also be used to prevent your body from rejecting a transplanted organ. Because the doses required to treat these conditions are often higher than the amount of cortisol your body normally needs each day, side effects from excess cortisol can occur.
It’s also possible to develop Cushing syndrome from injectable corticosteroids — for example, repeated injections for joint pain, bursitis and back pain. Inhaled steroid medicines (taken for asthma) and steroid skin creams (used for skin disorders such as eczema) are generally less likely to cause Cushing syndrome than are oral corticosteroids. But, in some individuals, these medications may cause Cushing syndrome, especially if taken in high doses.
Endogenous Cushing syndrome
Cushing syndrome may also be due to your body’s own overproduction of cortisol (endogenous Cushing syndrome). This may occur from excess production by one or both adrenal glands, or overproduction of the adrenocorticotropic hormone (ACTH), which normally regulates cortisol production.
- A pituitary gland tumor (pituitary adenoma). A noncancerous (benign) tumor of the pituitary gland, located at the base of the brain, produces an excess amount of ACTH, which in turn stimulates the adrenal glands to make more cortisol. When this form of the syndrome develops, it’s called Cushing disease. It occurs much more often in women and is the most common form of endogenous Cushing syndrome.
- An ACTH-secreting tumor. Rarely, a tumor that develops in an organ that normally does not produce ACTH will begin to secrete this hormone in excess, resulting in Cushing syndrome. These tumors, which can be noncancerous (benign) or cancerous (malignant), are usually found in the lungs, pancreas, thyroid or thymus gland.
- A primary adrenal gland disease. In some people, the cause of Cushing syndrome is excess cortisol secretion that doesn’t depend on stimulation from ACTH and is associated with disorders of the adrenal glands. The most common of these disorders is a noncancerous tumor of the adrenal cortex, called an adrenal adenoma.
- Cancerous tumors of the adrenal cortex (adrenocortical carcinomas) are rare, but they can cause Cushing syndrome as well. Occasionally, benign, nodular enlargement of both adrenal glands can result in Cushing syndrome.
- Familial Cushing syndrome. Rarely, people inherit a tendency to develop tumors on one or more of their endocrine glands, affecting cortisol levels and causing Cushing syndrome.
Cushing syndrome diagnosis
Cushing syndrome can be difficult to diagnose, particularly endogenous Cushing syndrome, because other conditions share the same signs and symptoms. Diagnosing Cushing syndrome can be a long and extensive process. You may not have any firm answers about your condition until you’ve had a series of medical appointments.
Your doctor will conduct a physical exam, looking for signs of Cushing syndrome. He or she may suspect Cushing syndrome if you have signs such as rounding of the face (moon face), a pad of fatty tissue between the shoulders and neck (buffalo hump), and thin skin with bruises and stretch marks.
If you’ve been taking a corticosteroid medication for a long time, your doctor may suspect that you’ve developed Cushing syndrome as a result of this medication. If you haven’t been using a corticosteroid medication, these diagnostic tests may help pinpoint the cause:
- Urine and blood tests. These tests measure hormone levels in your urine and blood and show whether your body is producing excessive cortisol. For the urine test, you may be asked to collect your urine over a 24-hour period. Both the urine and blood samples will be sent to a laboratory to be analyzed for cortisol levels. Your doctor might also recommend other specialized tests that involve measuring cortisol levels before and after stimulation or suppression with other hormone medications.
- Saliva test. Cortisol levels normally rise and fall throughout the day. In people without Cushing syndrome, levels of cortisol drop significantly in the evening. By analyzing cortisol levels from a small sample of saliva collected late at night, doctors can see if cortisol levels are too high, suggesting a diagnosis of Cushing syndrome.
Imaging tests. Computerized tomography (CT) scans or magnetic resonance imaging (MRI) scans can provide images of your pituitary and adrenal glands to detect abnormalities, such as tumors. - Petrosal sinus sampling. This test can help determine whether the cause of endogenous Cushing syndrome is rooted in the pituitary or somewhere else. For the test, blood samples are taken from the petrosal sinuses — veins that drain the pituitary gland. A thin tube is inserted into your upper thigh or groin area while you’re sedated and is threaded to the petrosal sinuses. Levels of ACTH are measured from the petrosal sinuses and from a blood sample taken from the forearm. If the ACTH level is higher in the sinus sample, the problem stems from the pituitary. If the ACTH levels are similar between the sinuses and forearm, the root of the problem lies outside of the pituitary gland.
These tests help your doctor diagnose Cushing syndrome, and they may help rule out other medical conditions with similar signs and symptoms. For example, polycystic ovary syndrome — a hormone disorder in women with enlarged ovaries — shares some of the same signs and symptoms as Cushing syndrome, such as excessive hair growth and irregular menstrual periods. Depression, eating disorders and alcoholism also can partially mimic Cushing syndrome.
Cushing syndrome treatment
Treatments for Cushing syndrome are designed to lower the high level of cortisol in your body. The best treatment for you depends on the cause of the syndrome. Options include:
Reducing corticosteroid use
If the cause of Cushing syndrome is long-term use of corticosteroid medications, your doctor may be able to keep your Cushing syndrome signs and symptoms under control by reducing the dosage of the drug over a period of time, while still adequately managing your asthma, arthritis or other condition.
For many of these medical problems, your doctor can prescribe noncorticosteroid drugs, which will allow him or her to reduce the dosage or eliminate the use of corticosteroids altogether. Don’t reduce the dose of corticosteroid drugs or stop taking them on your own. Do so only under your doctor’s supervision.
Abruptly discontinuing these medications could lead to deficient cortisol levels. Slowly tapering off corticosteroid drugs allows your body to resume normal cortisol production.
Surgery
If the cause of Cushing syndrome is a tumor, your doctor may recommend complete surgical removal. Pituitary tumors are typically removed by a neurosurgeon, who may perform the procedure through your nose. If a tumor is present in the adrenal glands, lungs or pancreas, the surgeon can remove it through a standard operation or in some cases by using minimally invasive surgical techniques, with smaller incisions.
After the operation, you’ll need to take cortisol replacement medications to provide your body with the correct amount of cortisol. In most cases, you’ll eventually experience a return of normal adrenal hormone production, and your doctor can taper off the replacement drugs.
However, this process can take up to a year or longer. In some instances, people with Cushing syndrome never experience a resumption of normal adrenal function; they then need lifelong replacement therapy.
Radiation therapy
If the surgeon can’t totally remove a pituitary tumor, he or she will usually prescribe radiation therapy to be used in conjunction with the operation. Additionally, radiation may be used for people who aren’t suitable candidates for surgery.
Radiation can be given in small doses over a six-week period, or with a technique called stereotactic radiosurgery. In the latter procedure, a large, one-time dose of radiation is delivered to the tumor, and the radiation exposure to surrounding tissues is minimized.
Medications
Medications can be used to control cortisol production when surgery and radiation don’t work. Medications may also be used before surgery in people who have become very sick with Cushing syndrome. Doctors may recommend drug therapy before surgery to improve signs and symptoms and minimize surgical risk. Medical therapy may not completely improve all of the symptoms of excess cortisol.
Medications to control excessive production of cortisol at the adrenal gland include ketoconazole, mitotane (Lysodren) and metyrapone (Metopirone).
Mifepristone (Korlym, Mifeprex) is approved for people with Cushing syndrome who have type 2 diabetes or glucose intolerance. Mifepristone does not decrease cortisol production, but it blocks the effect of cortisol on your tissues.
Side effects from these medications may include fatigue, nausea, vomiting, headaches, muscle aches, high blood pressure, low potassium and swelling. Some have more-serious side effects, such as neurological side effects and liver toxicity.
The newest medication for Cushing syndrome is pasireotide (Signifor), and it works by decreasing ACTH production from a pituitary tumor. This medication is given as an injection twice daily. It’s recommended if pituitary surgery is unsuccessful or cannot be done.
Side effects are fairly common and may include diarrhea, nausea, high blood sugar or diabetes, headache, abdominal pain, and fatigue.
In some cases, the tumor or its treatment will cause other hormones produced by the pituitary or adrenal gland to become deficient and your doctor will recommend hormone replacement medications.
If none of these treatment options is appropriate or effective, your doctor may recommend surgical removal of your adrenal glands (bilateral adrenalectomy). This procedure will cure excess production of cortisol, but will require lifelong replacement medications.
Lifestyle and home remedies
The length of your recovery from Cushing syndrome will depend on the severity and cause of your condition. Remember to be patient. You didn’t develop Cushing syndrome overnight, and your symptoms won’t disappear overnight, either. In the meantime, these tips may help you on your journey back to health.
- Increase activities slowly. You may be in such a hurry to get your old self back that you push yourself too hard too fast, but your weakened muscles need a slower approach. Work up to a reasonable level of exercise or activity that feels comfortable without overdoing it. You’ll improve little by little, and your persistence will be rewarded.
- Eat sensibly. Nutritious, wholesome foods provide a good source of fuel for your recovering body and can help you lose the extra pounds that you gained from Cushing syndrome. Make sure you’re getting enough calcium and vitamin D. Taken together, they help your body absorb calcium, which can help strengthen your bones, counteracting the bone density loss that often occurs with Cushing syndrome.
- Monitor your mental health. Depression can be a side effect of Cushing syndrome, but it can also persist or develop after treatment begins. Don’t ignore your depression or wait it out. Seek help promptly from your doctor or a therapist if you’re depressed, overwhelmed or having difficulty coping during your recovery.
- Gently soothe aches and pains. Hot baths, massages and low-impact exercises, such as water aerobics and tai chi, can help alleviate some of the muscle and joint pain that accompanies Cushing syndrome recovery.
- Nguyen, Henry & Tollefson, Megha. (2017). Endocrine disorders and hormonal therapy for adolescent acne. Current opinion in pediatrics. 29. 10.1097/MOP.0000000000000515
- Sahana PK, Sarma N, Sengupta N, Somani PS. A Florid Case of Iatrogenic Cushing’s Syndrome Induced by Topical Steroid with Osteoporosis and Hypogonadism. Indian J Dermatol. 2015;60(4):420. doi:10.4103/0019-5154.160514 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533560