Mucopurulent discharge
Mucopurulent discharge is the emission or secretion of fluid containing mucus and pus (muco pretaining to ‘mucus’ and purulent pertaining to ‘pus’) from the eye, nose, cervix, vagina, or other part of the body due to infection and inflammation.
Mucopurulent cervical discharge
Mucopurulent cervical discharge or mucopurulent endocervical discharge can be caused by the following:
- Noninfectious cervicitis (inflammation of the uterine cervix)
- Local trauma – eg, cervical irritation caused by tampons, a cervical cap, the string from an intrauterine contraceptive device, a pessary, or a diaphragm
- Radiation
- Chemical irritation – eg, vaginal douches, latex exposure, or contraceptive creams
- Systemic inflammation – eg, Behçet syndrome
- Malignancy
- Infectious cervicitis
- The infectious causes of cervicitis, all of which are sexually transmitted infections (STIs) or sexually transmitted diseases (STDs), are significantly more common than the noninfectious causes. Infectious cervicitis may be caused by Chlamydia trachomatis, Neisseria gonorrhoeae, or herpes simplex virus (HSV). In most cases of cervicitis, however, lab tests fail to isolate an organism; this is particularly true in women with low risk factors 1. Trichomonas vaginalis, which, technically, causes vaginal infections, is commonly included in the discussion of cervicitis.
- Vaginal discharge possible causes:
- Smells fishy = bacterial vaginosis
- Thick and white, like cottage cheese = thrush (candidiasis)
- Green, yellow or frothy = trichomoniasis
- With pelvic pain or bleeding = chlamydia or gonorrhoea
- With blisters or sores = genital herpes
Because the female genital tract is contiguous from the vulva to the fallopian tubes, there is some overlap between vulvovaginitis and cervicitis; both conditions are commonly categorized as lower genital tract infections. Infections involving the endometrium and fallopian tubes are commonly categorized as upper genital tract infections.
The most common causes of cervicitis are infectious, with sexual transmission of organisms such as with Chlamydia trachomatis and Neisseria gonorrhoeae being the primary means by which it is spread 1. Other etiologic organisms include Trichomonas vaginalis and herpes simplex virus (HSV), especially primary type 2 HSV 1.
Noninfectious causes of cervicitis include local trauma, radiation, chemical irritation, systemic inflammation, and malignancy. Limited data exist to suggest frequent douching, as well as Mycoplasma genitalium infection and bacterial vaginosis, as potential causes 1.
Risk factors for cervicitis include the following:
- Multiple sex partners
- Young age
- Single marital status
- Urban residence
- Low socioeconomic status
- Alcohol or drug use
Although the role of Mycoplasma genitalium in pelvic inflammatory disease (PID) is unclear, a study of 2378 British female students reported that this organism does not appear to be a significant etiologic agent for PID in this population (the incidence of PID was 3.9% over 12 mo in women with Mycoplasma genitalium infection vs 1.7% in noninfected women) 2.
In a later study, however—a Swedish report on 5519 women at an outpatient gynecologic service—it was noted that Mycoplasma genitalium was a strong independent risk factor for PID and cervicitis, although there was a lower frequency of both conditions relative to women with Chlamydia trachomatis infection 3. Further investigation is needed to determine the role of Mycoplasma genitalium in PID, infertility, and cervicitis 4.
A study by Dehon et al 5 found a high prevalence of Mycoplasma genitalium (7.4%) among the HIV-infected women and also found that chronic Mycoplasma genitalium infection was associated with increased secretion of proinflammatory cytokines and marked inflammatory cervical infiltrates in the cervix with enrichment of HIV target cells. The study concluded that not only was Mycoplasma genitalium implicated as an etiologic agent of cervicitis in HIV-infected women but that it also provided a potential mechanism for enhanced HIV transmission to an uninfected partner 5.
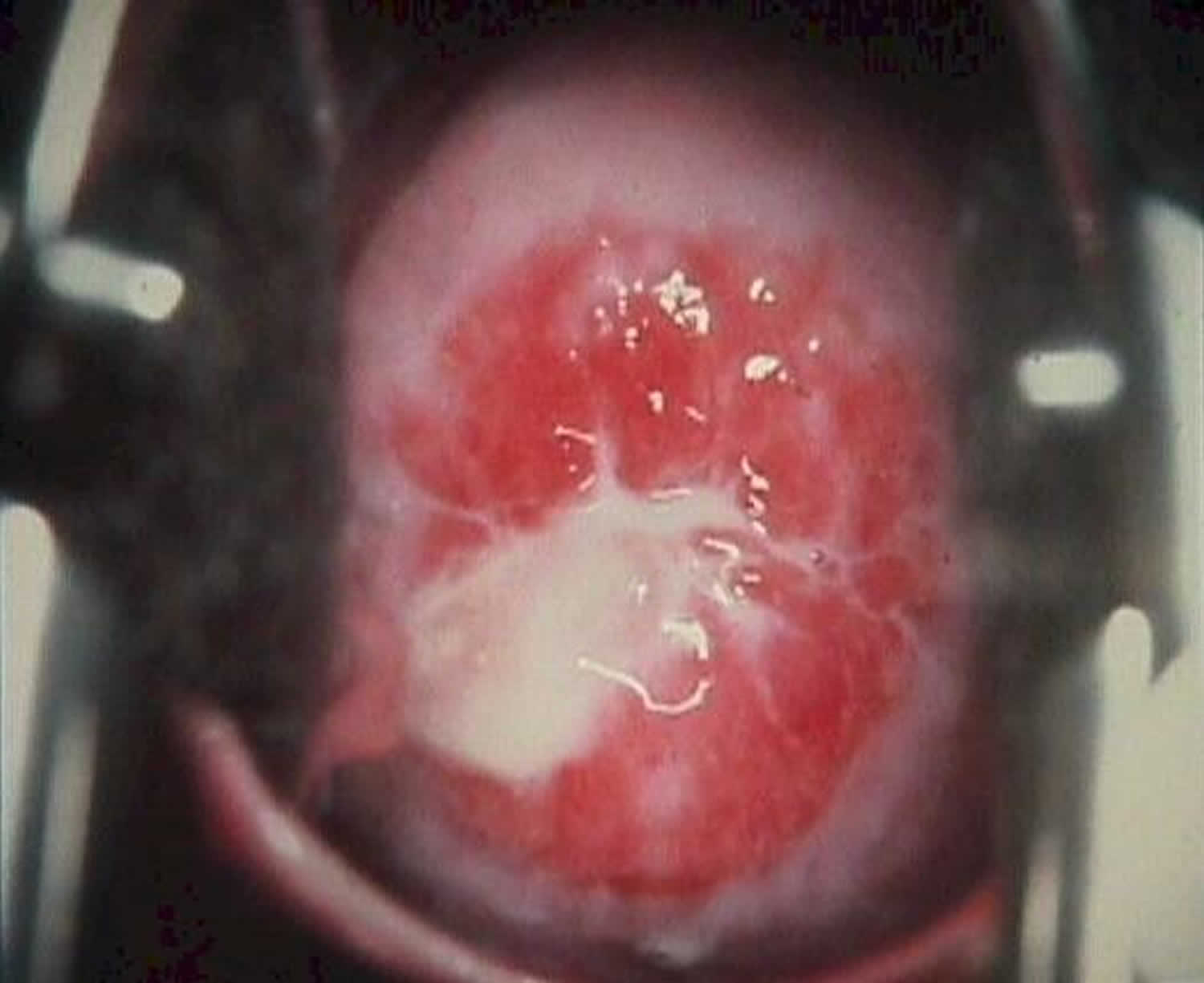
Figure 1. Mucopurulent cervical discharge
See a doctor or go to a sexual health clinic if:
- your discharge changes color, smell or texture
- you produce more discharge than usual
- you feel itchy or sore
- you bleed between periods or after sex
- you get pain when peeing
- you get pain in the area between your tummy and thighs (pelvic pain)
Mucopurulent nasal discharge
Mucopurulent nasal discharge is seen with bacterial infections.
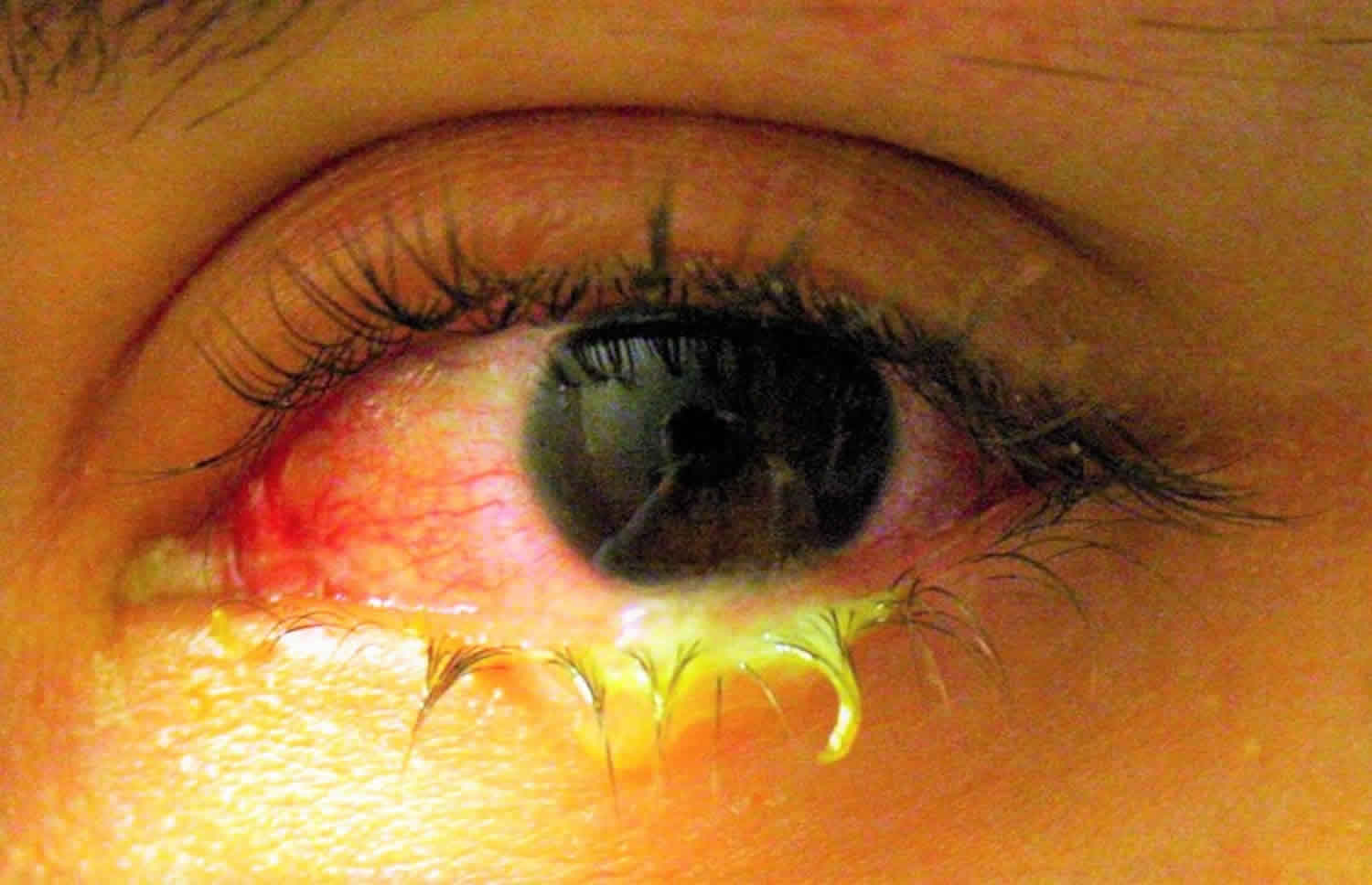
Mucopurulent eye discharge
Mucopurulent eye discharge is seen with bacterial infections. Bacterial conjunctivitis is one of the most commonly encountered eye problems. Conjunctivitis that produces sticky pus is contagious.
Acute bacterial conjunctivitis is primary due to Staphylococcus aureus, Streptococcus pneumoniae, and Haemophilus influenzae. Other pathogens responsible for acute disease are Pseudomonas aeruginosa, Moraxella lacunata, Streptococcus viridans, and Proteus mirabilis. These organisms may be spread from hand to eye contact or through adjacent mucosal tissues colonization such as nasal or sinus mucosa.
Hyperacute conjunctivitis is primarily due to Neisseria gonorrhoeae, which is a sexually transmitted disease (STD). Neisseria meningitidis is also in the differential and is important to consider as it can lead to potentially fatal meningeal or systemic infection.
Chronic conjuctivitis is primarily due to Chlamydia trachomatis. However, chronically ill, debilitated, or hospital patients can become colonized with other virulent bacteria responsible for chronic conjunctivitis. Staphylococcus aureus and Moraxella lacunata may also cause chronic conjunctivitis in patients with associated blepharitis.
Risk factors for bacterial conjunctivitis:
- Since these bacteria are usually spread from other infected individuals, poor hygenic habits may increase the risk of infection
- Poor contact lens hygiene
- Contaminated cosmetics
- Crowded living or social conditions such elementary schools, military barracks etc
- Ocular diseases including dry eye, blepharitis, and anatomic abnormalities of the ocular surface and lids
- Recent ocular surgery, exposed sutures or ocular foreign bodies
- Chronic use of topical medications
- Immune compromise
- Neonates are at particularly high risk for conjunctivitis (neonatal conjunctivitis).
See a doctor if:
- your baby has red eyes – get an urgent appointment if your baby is less than 28 days old with red eyes
- you wear contact lenses and have conjunctivitis symptoms as well as spots on your eyelids – you might be allergic to the lenses
- pain in your eyes
- sensitivity to light
- changes in your vision, like wavy lines or flashing
- intense redness in 1 eye or both eyes
- Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2015: Diseases Characterized by Urethritis and Cervicitis. MMWR Recomm Rep 2015;64(3). June 15, 2015. 51-53.
- Oakeshott P, Aghaizu A, Hay P, Reid F, Kerry S, Atherton H. Is Mycoplasma genitalium in women the “New Chlamydia?” A community-based prospective cohort study. Clin Infect Dis. 2010 Nov 15. 51(10):1160-6.
- Bjartling C, Osser S, Persson K. Mycoplasma genitalium in cervicitis and pelvic inflammatory disease among women at a gynecologic outpatient service. Am J Obstet Gynecol. 2012 Jun. 206(6):476.e1-8.
- McGowin CL, Anderson-Smits C. Mycoplasma genitalium: an emerging cause of sexually transmitted disease in women. PLoS Pathog. 2011 May. 7(5):e1001324
- Dehon PM, Hagensee ME, Sutton KJ, Oddo HE, Nelson N, McGowin CL. Histological Evidence of Chronic Mycoplasma genitalium-Induced Cervicitis in HIV-Infected Women: A Retrospective Cohort Study. J Infect Dis. 2016 Jun 1. 213 (11):1828-35.