Penetrating trauma
Penetrating trauma is an injury that occurs when a foreign object pierces the skin and enters a tissue of the body which could damage the underlying tissues or organs, creating an open wound. The severity of the internal injury depends on the organ(s) penetrated and on how vital the organ is. Penetrating injury is usually the result of the abrupt, direct application of a mechanical force to a focal area 1. The most common causes of penetrating trauma are gunshots and stab wounds 2. The penetrating object may remain in the tissues, come back out the way it entered, or pass through the tissues and exit from another area 3. An injury in which an object enters the body or a structure and passes all the way through is called a perforating injury, while penetrating trauma implies that the object does not pass through 4. Perforating trauma is associated with an entrance wound and an often larger exit wound.
Penetrating trauma suggests the object does not pass through. Penetrating trauma can be caused by violence and may result from:
- Fragments of a broken bone
- Gunshots
- Knife wounds
Penetrating trauma often causes damage to internal organs resulting in shock and infection. The severity depends on the body organs involved, the characteristics of the object, and the amount of energy transmitted. Assessment includes x-rays, CT scans, and MRI. Treatment involves surgery to repair damaged structures and remove foreign objects.
Puncture and penetration are similar.
- A puncture is different from a penetration wound in that there is no exit wound in a puncture.
- This type of trauma is seen in a stabbing or a gunshot wound in which a low-velocity pistol bullet was used.
Penetrating trauma can be serious because it can damage internal organs and presents a risk of shock and infection. Penetrating trauma signs and symptoms vary widely depending on the injured parts of the body and the shape and size of the penetrating object and the amount of energy transmitted to the tissues 2.
Diagnosis is established based on history and imaging studies (X-rays, CT/MRI scans). Management usually involves supportive measures (hemostasis, blood transfusion, respiratory support), and surgical repair of damaged structures and/or removal of foreign bodies.
Males constitute the great majority of patients with penetrating trauma injuries across the United States and the world. In some areas of the United States, approximately 90% of patients with penetrating trauma are male. Injuries are the leading cause of death in patients aged 1-44 years 5.
Penetrating trauma causes
As a projectile passes through tissue, it decelerates and transfers kinetic energy to the tissue. Increased velocity causes more damage than mass. The velocity of the projectile is a more important factor than its mass in determining how much damage is done 3. Kinetic energy increases with the square of the velocity.
- Kinetic energy is described by the following equation: Kinetic energy = ½mv 2 OR 1/2 mass X velocity (squared)
The space left by tissue that is destroyed by the penetrating object forms a cavity, and this is called permanent cavitation. In addition to damage to the tissues they contact, medium- and high-velocity projectiles result in a secondary cavitation injury as the object enters the body, it creates a pressure wave forcing tissue out of the way, creating a cavity or “temporary cavitation” 6. The tissues move back into place, eliminating the cavity, but the cavitation has already done considerable damage. The temporary cavity is the radial stretching of tissue around the bullet’s wound track, which momentarily leaves an empty space caused by high pressures surrounding the projectile that accelerate material away from its path 7.
The characteristics of the damaged tissue determine the severity of the injury: the denser the tissue, the greater the amount of energy transmitted to it. Skin, muscles, and intestines absorb energy and so are resistant to the development of temporary cavitation, while organs such as the liver, spleen, kidney, and brain, which have relatively low tensile strength, are likely to split or shatter because of temporary cavitation 8. Flexible elastic soft tissues, such as muscle, intestine, skin, and blood vessels, are good energy absorbers and are resistant to tissue stretch. If enough energy is transferred, the liver may disintegrate 7.
Penetrating head injury
Penetrating head injury also called penetrating brain injury is a wound in which a projectile breaches the cranium but does not exit it 9.
Based on the speed of penetration, penetrating head injury can be classified into two categories:
- High-velocity penetration: Examples include injuries caused by bullets or shell fragments, from direct trauma or shockwave injury to surrounding brain tissue due to a stretch injury.
- Low-velocity penetration: Examples include a knife or other sharp objects, with direct trauma to brain tissue 10.
The morbidity and mortality associated with penetrating head injury remain high. Analysis of the trauma literature has shown that 50% of all trauma deaths are secondary to traumatic brain injury (TBI) and gunshot wounds to the head caused 35% of these. Traumatic brain injury is the fourth leading cause of death in the United States and is the leading cause of death in persons aged 1-44 years, with approximately 2 million traumatic brain injuries occurring each year 11. A National Institutes of Health survey estimates that 1.9 million persons annually experience a skull fracture or intracranial injury 12. Firearms account for the largest proportion of deaths from traumatic brain injury in the United States; each year, close to 20,000 persons have gunshot wounds to the head 13.
Penetrating head injury causes
Penetrating head injuries can be the result of numerous intentional or unintentional events, including missile wounds, stab wounds, and motor vehicle or occupational accidents (nails, screwdrivers). Stab wounds to the cranium are typically caused by a weapon with a small impact area and wielded at low velocity. The most common wound is a knife injury, although bizarre craniocerebral-perforating injuries have been reported that were caused by nails, metal poles, ice picks, keys, pencils, chopsticks, and power drills 14.
In a study of 14 children with intracranial injuries due to spring- or gas-powered BB or pellet guns, 10 of the children required surgery, and 6 were left with permanent neurologic injuries, including epilepsy, cognitive deficits, hydrocephalus, diplopia, visual field cut, and blindness 15. According to the study authors, advances in compressed-gas technology have led to a significant increase in the power and muzzle velocity of such guns, with the ability to penetrate a child’s skull and brain 15.
Siccardi et al 16 prospectively studied a series of 314 patients with craniocerebral missile wounds and found that 73% of the victims died at the scene, 12% died within 3 hours of injury, and 7% died later, yielding a total mortality of 92% in this series. In another study 17, gunshot wounds were responsible for at least 14% of the head injury-related deaths. A study 18 using multiple logistic regressions found that injury from firearms greatly increases the probability of death and that the victim of a gunshot wound to the head is approximately 35 times more likely to die than is a patient with a comparable nonpenetrating brain injury.
Penetrating head injury signs and symptoms
The presentation depends on the mechanism, site of the lesions, and associated injuries.
The consequences of penetrating head injury depend on the following factors:
- Intracranial path and location: High mortality resulting from those that cross the midline, pass through the ventricles, or come to rest in the posterior fossa
- Energy and speed of entry: These factors depend on the properties of the weapon or missile. They result from energy being transferred from an object to the human skull and the underlying brain tissue. There is a high mortality rate associated with high-velocity projectiles. The kinetic energy involved is related to the square of the velocity. Three mechanisms of injuries have been reported.
- Laceration and crushing
- Cavitation
- Shockwaves
- Size and type of the penetrating object: Usually, large missiles or missiles that fragment within the cranial vault cause more fatalities
- Circumstances or events surrounding the injury
- Other associated injuries
Primary injuries occur immediately. Secondary injuries occur following the time of the injury. The final neurologic outcome is influenced by the extent and degree of secondary brain injury. Therefore, the primary goal in the emergency department is to prevent or reduce conditions that can worsen outcomes, such as hypotension, hypoxia, anemia, and hyperpyrexia.
The amount of damage to the brain depends on the kinetic energy imparted to the brain tissue. This, in turn, depends on the following factors:
- Trajectories of both the missile and the bone fragments through the brain
- Changes in intracranial pressure at the time of impact.
Penetrating head injury complications
Patients who survive penetrating craniocerebral injuries are at risk of experiencing multiple complications, including persistent neurologic deficits, infections, epilepsy, CSF leak, cranial nerve deficits, pseudoaneurysms, arteriovenous fistulas, and hydrocephalus.
Intracranial infections
Intracranial infections can complicate as many as 11% of penetrating craniocerebral injuries 19. Therefore, prevention and proper management of infectious complications can lead to improved outcome in these patients. Patients can develop meningitis, epidural abscess, subdural empyemas, or brain abscess.
Posttraumatic meningitis usually is associated with skull fractures or CSF leak.
Cranial epidural abscess is an uncommon infection that most often occurs secondary to osteomyelitis or because of foreign bodies. The purulent collection remains well localized due to the tight adherence of the dura to the overlying calvaria; however, cranial epidural abscess can cause meningitis and subdural empyema associated with significant morbidity and mortality.
The most frequent source of subdural empyema is penetration through adjacent facial infections, such as paranasal sinusitis or mastoiditis.
Brain abscess can occur after a long period of silent infection. Hida et al reported a case of delayed brain abscess following a penetrating gunshot injury, found 38 years after the insult 20. The treatment of epidural abscess, subdural empyema, and brain abscess consists of prompt surgical intervention followed by prolonged antibiotic therapy.
Epilepsy
Posttraumatic epilepsy is linked to psychosocial disability and is probably a contributing factor to premature death after penetrating head injury 21. The incidence of posttraumatic epilepsy varies widely, depending on the type and severity of the injury. In closed head injury, the incidence of posttraumatic epilepsy varies from 2.9 to 17% for moderate and severe head injury. In contrast, the incidence of epilepsy for military craniocerebral missile wounds is twice as high; most series report a 5- to 10-year incidence of seizures of 32-51%. Almost 50% of victims of penetrating head trauma enrolled in military series become epileptic 22.
The exact pathophysiology of posttraumatic epilepsy after closed or penetrating head injury is not known. Many confounding risk factors, such as retained metal fragments, the extent and site of injury, level of consciousness, residual focal deficit, and complications, have been studied to pinpoint the importance of each in efforts to clarify the pathophysiologic mechanisms of posttraumatic epilepsy.
Cerebrospinal fluid leak
Head trauma is the most common cause of CSF leak. Meningitis occurs in approximately 20% of acute (within 1 week) posttraumatic leaks and 57% of delayed posttraumatic leaks. The use of prophylactic antibiotic administration for CSF leak has been demonstrated to lead to serious infections, including drug-resistant meningitis.
Patients with posttraumatic CSF leak are initially treated conservatively with bed rest in a position that results in a decrease or cessation of the fistulous drainage. If the drainage has not ceased within 24-48 hours, a lumbar drain is inserted and drained at a rate of 10 cc of CSF per hour for 5-7 days. A lumbar drain should not be inserted in patients with significant pneumocephalus. During CSF drainage, progressive diminution of the level of consciousness should alert the clinician to the possibility of pneumocephalus. If the CSF leak does not stop with the lumbar drainage, a surgical intervention to repair the fistulous tract may be indicated.
Vascular injuries may result from direct injury of the vessels by the penetrating object, by blast effect at the time of trauma, or by skull fractures or bone fragments producing vascular occlusion. Direct vascular injuries sustained at the time of head injury initially may be clinically silent and may remain so for weeks, months, or years. In addition, delayed posttraumatic pseudoaneurysms can appear weeks to months after the injury.
Cranial nerve deficits
Patients who experience an injury to the temporal area and/or have a fracture of the temporal bone are especially at risk for carotid artery injury, as well as injury to the facial nerve. Hence, in patients who experience penetrating brain injuries, maintaining a high index of suspicion and obtaining follow-up radiologic studies, usually via cerebral angiography, is important.
Pseudoaneurysm
Pseudoaneurysms may result in a perturbation of the normal blood flow and can act as foci of thrombus formation, or they can rupture, causing a subarachnoid or intracerebral hematoma. They usually require surgical or endovascular treatment. The role of anticoagulation in the treatment of pseudoaneurysms remains controversial, but it may be beneficial in minimizing thrombus propagation and embolization.
Pulmonary embolism
Death from an acute pulmonary embolism due to deep vein thrombosis secondary to a self-inflicted gunshot wound to the face has been reported 23.
Arteriovenous fistula
Arterial dissections occur when a laceration through the intima and sometimes the media permits entry of blood and separation of these inner and outer vascular layers, compromising the vessel lumen. They usually present with transient ischemic attacks or symptoms of stroke. Nonsurgical management of arterial dissections with chronic anticoagulation is usually effective.
Probably the best-recognized posttraumatic arteriovenous fistula is the posttraumatic carotid-cavernous sinus fistula. In general, these fistulae are associated with the blast injury rather than the intracranial penetration; they are usually high-flow fistulas; and they are clinically characterized by a clinical syndrome consisting of pulsating exophthalmos, chemosis, and bruit. Carotid-cavernous fistulae can be diagnosed by cerebral angiography and are best treated by endovascular occlusion.
Penetrating head injury diagnosis
Initial physical examination includes primary and secondary trauma survey with the evaluation of other distracting injuries. A complete physical examination should be performed including a neurological examination. This should include documentation of the Glasgow coma scale (GCS). The involvement of cranial nerves should be assessed, and motor/sensory examination should be performed. It is important to realize that neurologic injury may be manifest distant to the site of impact. If unable to fully and formally assess cranial nerves secondary to lack of patient cooperation, it is important to, at least, document any findings relevant to the patient’s neurology.
In the pre-hospital setting, or in non-trauma facilities, stabilize, but, do not remove penetrating objects such as knives. Patients should be transported quickly to a location capable of providing definitive care. Early recognition of high-risk mechanisms, early imaging, and early evaluation at a level 1 trauma center may improve outcomes 24.
In the emergency department, resuscitation and stabilization should be provided. Manage ABCDE’s (Airway, Breathing, Circulation, Disability, and Exposure/Environment) using Advanced Trauma Life Support (ATLS) guidelines. Perform a primary survey to identify any life-threatening injury. Stabilize, focusing on the airway, breathing, and circulation, including external hemorrhage, while establishing and maintaining cervical spine immobilization. Early activation of a trauma team may help to provide prompt recognition of polytrauma. The target is to maintain a systolic blood pressure of at least 90 mm Hg.
Following initial resuscitation and stabilization, an inspection of the superficial wound should be performed. Identify the entrance wound (and exit wounds, if present). Beware that blood-matted hair may cover these wounds. When a patient presents with a gunshot wound to the head, the other parts of the body including neck, chest, and abdomen should be inspected carefully for other gunshot wounds. Beware that injuries to the heart or great vessels in the chest or abdomen may be even more life-threatening.
A subgaleal hematoma can become extensive because blood easily dissects through the loose areolar tissue; such a hematoma can be a cause of hemodynamic compromise. Apply a sterile dressing to both the entrance and exit wounds. Assess whether there is any oozing of cerebrospinal fluid (CSF), blood, or brain parenchyma from the wound. Evaluate for hemotympanum, which may indicate a basilar skull fracture. Examine all orifices for retention of foreign bodies, the missile, teeth, and bone fragments.
Perform neurological examination, including GCS and document well. Evaluating for signs suggesting raised intracranial pressure is critical. The initial signs and symptoms may be nonspecific and include a headache, nausea, vomiting, and papilledema.
Perform a careful examination of the neck, chest, abdomen, pelvis, and extremities. Assume multiple injuries in cases of penetrating trauma. Obtain a detailed history including the “AMPLE” history with an emphasis on events surrounding the injury. Also, determine the weapon type and/or caliber of the weapon.
CT Scan
If the patient is hemodynamically stable, obtain a Computed Tomography (CT) scan of the head to evaluate for the presence of a mass lesion (hematoma) or cerebral edema. It can be obtained when the patient is stabilized and ready to be transported to the radiology department. A CT scan can adequately identify the extent of the intracranial injury and can also determine the relationship between the penetrating object and the intracranial structures. However, a radiolucent object, such as a wooden object, maybe missed by the CT scan. In patients with penetrating head trauma, a large mass or hematoma may be evident. If intracranial pressure (ICP) is increased, aqueductal stenosis is present, and the third but not fourth ventricle is enlarged.
Certain factors are important in critical decision making and have prognostic implications. These may include the following:
- Sites of entry and exit wounds
- Presence of intracranial fragments
- Missile track and its relationship to both blood vessels and air-containing skull-base structures
- Presence of intracranial air
- Trans-ventricular injury
- Basal ganglia and brain stem injury
- Whether the missile track cross the midline
- Presence of multi-lobar injury
- Presence of basal cistern effacement
- Brain parenchymal herniation
- Presence of any associated mass effects
Plain radiograph
Maybe useful as it provides information about the following:
- Shape of the penetrating object
- Skull fractures (if present)
- An intracranial foreign object (if present)
Computed Tomographic Angiography (CTA)
If a vascular injury is suspected, noninvasive investigative computed tomographic angiography (CTA) should be obtained after patient stabilization.
Magnetic Resonance Imaging (MRI) Scan
Additionally, an MRI Scan may be obtained if penetrating objects are suspected to be wooden objects. It should not be performed if intracranial metallic fragments are present. Such a procedure is contraindicated. However, if no bullets or intracranial metallic fragments are present, then an MRI scan of the brain can be performed in a stable patient. This can provide information about the posterior fossa structures and the extent of possible shared injuries.
Penetrating head injury treatment
Patients with penetrating head trauma require both medical and surgical management 25.
Medical management
A low threshold for obtaining surgical consultation should be considered in cases of penetrating head trauma. Beware that many patients with penetrating head trauma will likely require operative intervention.
DO NOT remove any penetrating object from the skull in the emergency department until trauma and neurosurgical evaluation is obtained. Also, the protruding object should be stabilized, and provision should be made to protect it from moving during transportation of the patient, to prevent further injury.
Assess the need for endotracheal intubation:
- Inability to maintain adequate ventilation
- Inability to protect the airway due to depressed level of consciousness
- Neck or pharyngeal injury
Normalize PCO2. Avoid hyperventilation, because it leads to vasoconstriction and a subsequent reduction in the cerebral perfusion pressure (CPP). This may worsen long-term neurological outcome. Beware that hyperventilation is only a temporizing measure for the reduction of elevated intracranial pressure (ICP). Avoid hyperventilation during the first 24 hours after injury when cerebral blood flow (CBF) often is reduced.
Monitor intracranial pressure (ICP) particularly in patients with Glasgow Coma Scale (GCS) less than 8. Consider head elevation to 30 degrees. This can improve venous drainage and may decrease ICP. The target is to maintain intracranial pressure (ICP) less than 20 mmHg to 25 mmHg and cerebral perfusion pressure (CPP) greater than 70 mmHg. Since cerebral blood flow is difficult to measure continuously, the cerebral perfusion pressure (CPP) is measured as a surrogate. Treatment typically is indicated for intracranial pressure (ICP) greater than or equal to 20 mmHg to 25 mmHg, with guideline goals of ICP less than 20 mmHg and cerebral perfusion pressure (CPP) 50 mmHg to 70 mmHg.
- Propofol, a lipophilic rapid-onset hypnotic with a short half-life that can be titrated to control ICP.
- Mannitol administered as intravenous bolus as needed results in decreased ICP; it reduces the viscosity of blood, improving cerebral blood flow; and it might serve as a free-radical scavenger.
- If the ICP cannot be controlled, barbiturate coma or a decompressive craniectomy may be indicated.
Avoid the use of a nasogastric tube if there may be a skull-base fracture. i.e., there is a risk of intracranial tube insertions or risk of significant bleeding during surgical removal of the penetrating object.
Beware that traumatic aneurysms are more susceptible to rupture than are congenital aneurysms.
Surgical management
A major reason for surgical intervention is the presence of a hematoma. Large hematomas should be evacuated promptly. Early decompression with conservative debridement of the brain may be needed.
The following are significant reasons for surgery:
- To remove masses such as epidural, subdural, or intracerebral hematomas;
- To remove necrotic brain and prevent further swelling and ischemia;
- To control an active hemorrhage; and
- To remove necrotic tissue, metal, bone fragments, or other foreign bodies to prevent infections.
In most cases, the removal of a deep-seated bullet may not be required. However, there are certain indications when removal should be considered. These are:
- Penetrating injury through pterion, orbit, or posterior fossa
- Presence of intracranial hematoma
- Presence of pseudoaneurysm at the time of initial exploration
A craniotomy is needed for low-velocity missile wounds in which the object is still protruding from the head. Avoid using the entry or exit wounds when planning scalp incisions. Some critical factors can determine the outcome for those who survive the initial injury; they depend on prompt and early surgical intervention as well as the ability to provide high-level neurocritical care.
Postoperative care
Antibiotics:
- Intravenous co-amoxiclav 1.2g every 8 hours OR intravenous cefuroxime 1.5g, then 750 mg every 8 hours AND intravenous metronidazole 500mg every 8 hours for 7-14 days 26.
Anticonvulsants:
- Prophylactic phenytoin, carbamazepine, valproate, or phenobarbital is usually given in the first week after an injury 27.
Penetrating head injury prognosis
Traumatic brain injury is the leading cause of disability and death in children aged 0-4 years and adolescents aged 15-19 years. Also, it is estimated that 145,000 children and adolescents (ages 0-19 years) are living with lasting cognitive, physical, or behavioral effects of traumatic brain injury 28.
Approximately 70-90% of patients with penetrating traumatic brain injury die before reaching the hospital, and 50% of those who survive to reach the hospital die during resuscitation attempts in the emergency department (ED). Approximately 35,000 civilian deaths are attributed to penetrating brain injury each year, with firearms-related injuries being the leading cause of mortality in this group. Of the 333,169 US military traumatic brain injurys recorded between 2000-2015, 4,904 were classified as penetrating traumatic brain injury 29.
Many studies have attempted to associate various prognostic factors with outcome. The most important prognostic factor currently recognized is the Glasgow Coma Scale (GCS) after cardiopulmonary resuscitation. Traditionally, the higher the GCS after resuscitation, the better the patient outcome. However, concern has developed that because patients who present in coma are thought to have a dismal prognosis, less aggressive management is often used, contributing to poorer outcome.
Studies over the last decade have examined the outcome of patients with a postresuscitation GCS of 3-5 who underwent aggressive medical and surgical management. Grahm et al 30 found that no patient in a study of 100 patients with postresuscitation GCS of 3-5 had a satisfactory outcome (good/moderately disabled). They also found that no patients with a GCS of 6-8 and bihemispheric or multilobar dominant hemisphere injuries had a satisfactory outcome.
In a review of 190 patients, Levy et al 18 found that only 2 patients with a GCS of 3-5 achieved a moderately disabled outcome. Further analysis showed that these patients had reactive pupils at admission and did not have bihemispheric/multilobar dominant hemispheric injuries. They concluded that surgical intervention is not beneficial in most patients with a GCS of 3-5 but may be beneficial for the rare patient with reactive pupils but without ominous findings on CT scan 18. Despite these studies, some controversy remains regarding surgery performed on patients with a GCS less than 9 and especially regarding patients with a GCS less than 5.
Other poor prognostic factors include age, suicide attempt, and through-and-through injuries. Patients who present with high ICP and/or hypotension also tend to have worse outcomes. CT scan findings associated with poor outcome include (1) bihemispheric injury, (2) intraventricular and/or subarachnoid hemorrhage, (3) mass effect and midline shift, (4) evidence of herniation, and/or (5) hematomas greater than 15 mL on CT scan.
Morbidity and mortality rates associated with penetrating brain injury remain unacceptably high. For patients presenting with a GCS of 3-5, mortality rates remain near 90%, and a satisfactory outcome as defined by the GCS only rarely occurs. Patients presenting with a GCS of 6-8 have a more variable outcome that may be related to differences in management and/or the smaller numbers of patients presenting in this category. Patients with a GCS greater than 9 have much lower mortality rates. Approximately one half of these patients make good recoveries, and 90% have satisfactory outcomes.
The results from one study found that insulin deficiency due to diabetes mellitus imparts an increased risk for mortality in patients with moderate-to-severe traumatic brain injury (TBI) compared to patients without diabetes mellitus (14.4% versus 8.2% ) 31.
Penetrating neck injury
Penetrating neck trauma involves a missile (e.g., ballistic injuries) or sharp object penetrating the skin (e.g., stab injuries) and violating the platysma layer of the neck. This includes gunshot wounds, stab or puncture wounds, and impalement injuries 32. Penetrating neck trauma represents approximately 5-10% of all trauma cases that present to the emergency department. Penetrating neck injuries remain challenging, as there are a number of important structures in a small area and injury to any of these structures may not be readily apparent. About 30% of these cases are accompanied by injury outside of the neck zones as well.
The current mortality rate in civilians with penetrating neck injuries ranges from 3-6%. During World War II, the mortality rate was 7%, and, in World War I, it was 11% 33. Higher mortality rates occur with penetrating neck injury to large vessels, such as the carotid or subclavian arteries and veins.
Recent experience in the treatment of casualties from the Iraq War at Walter Reed Army Medical Center reported the common carotid artery as the most frequently injured cervical vessel 34.
The standard of care is immediate surgical exploration for patients who present with signs and symptoms of shock and continuous hemorrhage from the neck wound. The type of incision depends on the neck zone and the structures at risk for injury.
The following specific injuries must be confirmed and treated during neck exploration:
- Carotid artery injuries
- Vertebral artery injuries
- Jugular vein injury
- Laryngotracheal injuries
- Esophageal injuries
- Nerve injuries
- Thoracic duct injuries
- Thyroid injuries
Neck anatomy
In few other regions of the body are so many vital structures (that would be of immediate concern following injury) located in so small a volume. An injury is not considered to have penetrated the neck unless the injury penetrates the platysma muscle layer. Injuries through the platysma and injuries crossing the midline usually cause a greater degree of damage. The sternocleidomastoid muscle delineates the posterior and anterior regions of the neck. The area of the neck posterior to the cervical vertebral body and the scalene muscles is composed mainly of muscle, bone, and nonvital vessels and lymphatics. Most of the vital structures are located in the anterior or lateral regions.
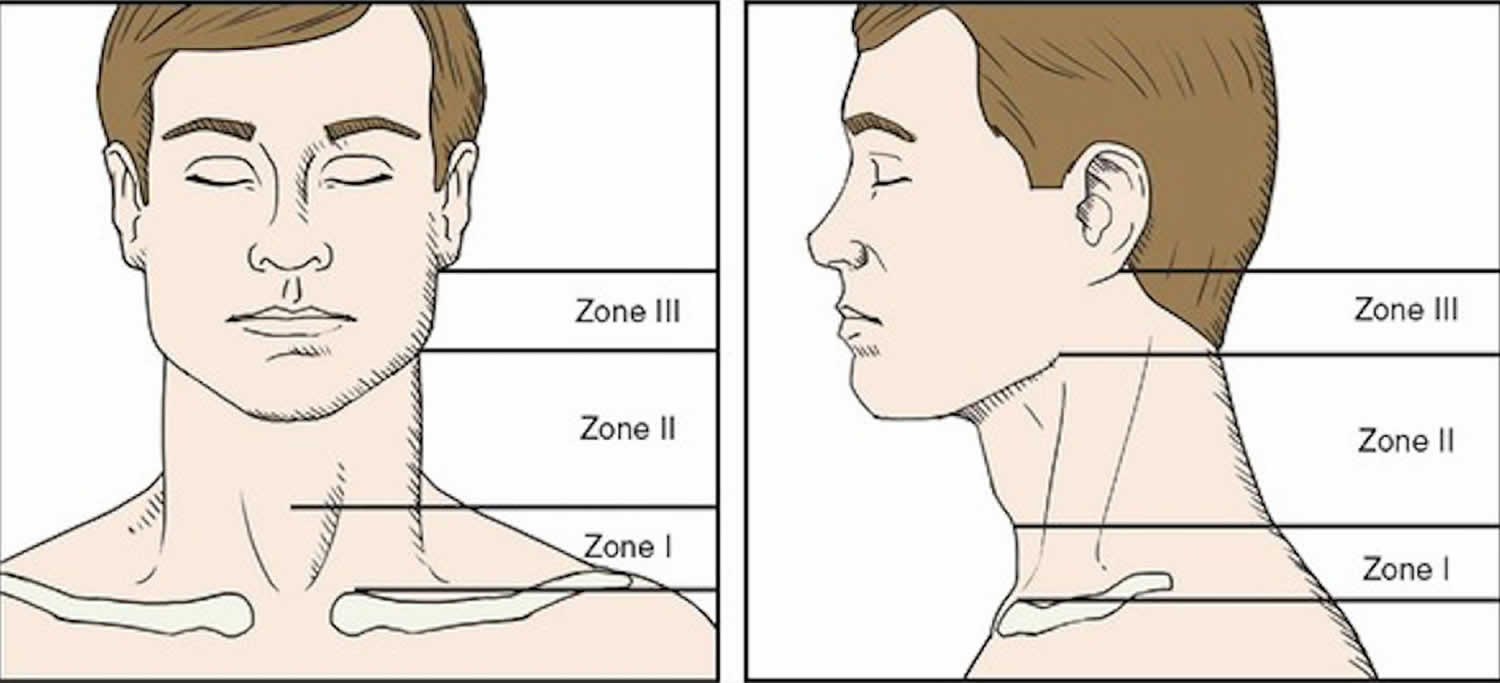
The neck may be divided into 3 zones using anatomic landmarks. Each zone has a group of vital structures that can be injured and may determine the kind of trauma management.
- Zone 1 is the horizontal area between the clavicle/suprasternal notch and the cricoid cartilage encompassing the thoracic outlet structures. The proximal common carotid, vertebral, and subclavian arteries and the trachea, esophagus, thoracic duct, and thymus are located in zone 1.
- Zone 2 is the area between the cricoid cartilage and the angle of the mandible. It contains the internal and external carotid arteries, jugular veins, pharynx, larynx, esophagus, recurrent laryngeal nerve, spinal cord, trachea, thyroid, and parathyroids.
- Zone 3 is the area that lies between the angle of the mandible and the base of the skull. It has the distal extracranial carotid and vertebral arteries and the uppermost segments of the jugular veins.
Tight fascial compartments of neck structures may limit external hemorrhage from vascular injuries, minimizing the chance of exsanguination. However, these tight fascial boundaries may increase the risk of airway compromise because the airway is relatively mobile and compressible by an expanding hematoma.
Figure 1. Zones of the neck in relation to penetrating neck injuries
Penetrating neck injury causes
Penetrating neck injuries, like any trauma, may be classified as intentional or nonintentional. The objects causing these injuries can be divided into stabbing instruments (eg, knives, cutting instruments, puncturing objects, impaling objects) and shooting instruments (eg, missiles, projectiles). Wounding instruments have specific characteristics that affect surgical findings. For example, stab wounds typically have a 10% higher rate of negative exploration than injuries from projectiles.
Two factors in the mechanism of injury in penetrating neck trauma determine the extent of damage to the tissue.
- Weapon characteristics
- The amount of kinetic energy delivered by the wounding agent has to be considered together with its interaction with the involved tissue. Kinetic energy (KE) is described by the following equation: Kinetic energy = ½mv 2 OR 1/2 mass X velocity (squared)
- Low-energy weapons include hand-driven weapons, such as knives or ice picks, which damage with only their sharp point or cutting edge.
- Firearms may be classified as medium-energy (ie, handguns) and high-energy weapons (ie, military assault weapons), with the latter usually defined as having 461 joules or more.
- Projectiles (ie, bullets, missiles) often are differentiated by mass, velocity, shape, and construction because these characteristics affect the extent of tissue disruption.
- Bullet velocity is the most important characteristic considered, with high velocity defined as greater than 2500 ft/s.
- The amount of kinetic energy delivered by the wounding agent has to be considered together with its interaction with the involved tissue. Kinetic energy (KE) is described by the following equation: Kinetic energy = ½mv 2 OR 1/2 mass X velocity (squared)
- Location of injury and tissues or organs involved
- Tissue injury results from either a direct impact by the penetrating projectile or tissue displacement from temporary cavitation.
- Wound sites and, if present, the wounding agent in the neck provide an indication of the likely injury complex.
Penetrating neck injury signs and symptoms
Evidence of significant injury to vital structures of the neck may be indicated by the following clinical manifestations:
- Dysphagia – Tracheal and/or esophageal injury
- Hoarseness – Tracheal and/or esophageal injury (especially recurrent laryngeal nerve)
- Oronasopharyngeal bleeding – Vascular, tracheal, or esophageal injury
- Neurologic deficit – Vascular and/or spinal cord injury
- Hypotension – Nonspecific; may be related to the neck injury or may indicate trauma elsewhere
Proposed hard signs of airway injury include the following:
- Subcutaneous emphysema – Tracheal, esophageal, or pulmonary injury
- Air bubbling through the wound
- Stridor or respiratory distress – Laryngeal and/or esophageal injury
Several so-called hard signs that strongly indicate vascular injury are as follows:
- Hematoma (expanding) – Vascular injury
- Active external hemorrhage from the wound site – Arterial vascular injury
- Bruit/thrill – Arteriovenous fistula
- Pulselessness/pulse deficit
- Distal ischemia (neurologic deficit in this case)
The evaluation of a patient with penetrating neck trauma always should start with advanced trauma life support (ATLS), a paradigm that begins with a directed primary survey emphasizing airway, breathing, and circulation (ABC). After patients are stabilized, they undergo a secondary survey that includes a complete history and a thorough physical examination. These steps, together with the studies discussed in Workup, are used to identify the likely injury complex and to direct further treatment or diagnostic testing.
There is evidence to suggest that the hard signs of airway injury are more reliable and result in less negative operative explorations compared with hard signs of vascular injury. The rate of negative exploration for patients with hard signs of vascular injury varies widely, but it may be estimated at 10%. However, series that report these cases as “nonsignificant” injury or as negative explorations lack clear definition, and it is difficult to draw any useful conclusion from the data.
Penetrating neck injury diagnosis
Imaging studies
- Cervical anteroposterior and lateral radiography is used to evaluate for vertebral bony injury; retained foreign bodies; and foreign body deformity, location, size, and number.
- Four-vessel cerebral angiography is indicated with clinical evidence of significant vascular injury (ie, hard signs) in zone 1 and zone 3, as well as in selectively managed zone 2 injuries. Physical examination findings reliably guide the use of invasive testing for suspected zone 2 vascular injury. In fact, the percentage (about 1%) of missed vascular injuries using physical examination screening criteria is similar to the false-negative rate for angiography. Data from Ferguson and colleagues suggest that, in the absence of hard vascular signs with a zone 3 injury, angiography is not necessary 35. This concept holds true for many types of suspected arterial injury. This represents a dramatic change in evaluation, as angiography was previously mandatory for all penetrating zone 3 injuries.
- Hypotension and exsanguination should prompt operative exploration in most centers. Certain centers that have in-house angiographers may proceed to the angiography suite for injuries in zone 1 and zone 3 despite hypotension or hemorrhage. Angiography remains the criterion standard for defining arterial anatomy and injury complexes, with an accuracy close to 100%.
- Arteriography demonstrates a low yield (< 1%) of findings that alter treatment in asymptomatic patients. Arteriography usually is performed using a digital subtraction angiography (DSA) technique that reduces the amount of contrast required and yields a superior computer-manipulated image for evaluation.
- Helical computed tomographic angiography (CTA) is less invasive and is showing promise in defining vascular neck injury. Possibly, in the future, this technique may replace angiography.
- Two-dimensional Doppler studies are a noninvasive alternative to angiography to evaluate vascular injury in critical areas (principally in zone 2). Its role in zone 3 evaluation is quite limited, given the obvious anatomic limitations of ultrasound in this region. This study typically incorporates a static B mode image of the interrogated vessel in combination with real-time ultrasound and Doppler velocity determination coupled with spectral analysis. This is covered in the umbrella term Duplex. Three-dimensional images for reformation are increasingly available but require costly imaging systems that may not be readily available in the emergency department. Such tests may be best used in stable patients with zone II injuries without any signs of vascular injury to complete the examination of the regional vital structures.
- Esophagography is essential to evaluate for an esophageal perforation. Selecting the oral contrast medium for esophageal injury detection is controversial. One school of thought contends that oral iodinated aqueous contrast media better demonstrates perforations and anastomotic leakage with less risk of complications than barium; the sensitivity of this technique in detecting esophageal injury increases from 70-89% when combined with esophagoscopy. The other school of thought contends that aqueous contrast media is hypertonic and, if extravasated into the mediastinum, induces a local inflammatory reaction. Barium solution is inert in the mediastinum and has been used for decades within the tracheobronchial tree for contrast bronchography prior to the advent of flexible bronchoscopy.
- Computed tomography (CT) scan is a study that can evaluate many structures at a time and that is enhanced with the use of intravenous nonionic contrast media. If available, helical or spiral CT scans permit multiplanar views and 3-dimensional reconstructions. A CT scan is excellent for helping to define and diagnose a laryngeal injury. A CT scan can also be useful to help define a missile tract. A CT scan does not increase the sensitivity of detecting an esophageal injury. If an esophageal injury is suspected, esophagoscopy is the procedure of choice.
- CT angiography (CTA) is gaining acceptance as an adjunctive screening tool. A review by Woo and colleagues 34 reports that the use of CTA is associated with less operative exploration, less negative explorations, and reduced use of invasive studies, such as conventional angiography. Physical examination findings supplemented by CTA should have a prominent role in the selective management of penetrating neck injuries. CTA has replaced angiography as the initial study of choice in the vascular evaluation of a neck injury 36.
- The improved spatial resolution of the multidetector CT scan has improved the diagnostic capability and the accuracy of this modality, further supporting it as the initial study of choice for civilian injury.
- Renewed interest as to the optimal management of wartime penetrating neck injuries has been addressed by Fox and colleagues 37 in the delayed assessment of war casualties at Walter Reed Army Medical Center. A significant number of delayed evaluations found injuries, and retained missile fragments, were a limitation to accurate assessment at the zone of injury with CT examination. They assert that, for the military injury, arteriography remains the criterion standard.
- The advantage of magnetic resonance imaging is not elucidated clearly for penetrating neck injuries; continual evaluation and monitoring of trauma patients who are in potentially critical condition presents a problem during this procedure.
- Even when readily available, time constraints of magnetic resonance angiogram (MRA) limit its use in the acute phase of traumatic evaluation.
- ACR Appropriateness Criteria 38 recommend that in penetrating neck injuries, CT angiography of the neck is the preferred imaging procedure to evaluate the extent of injury. The guidelines also note that catheter-based arteriography is useful for further evaluation and an x-ray barium swallow single contrast may be considered in conjunction with direct visualization techniques if there remains a concern for aerodigestive injury.
Diagnostic procedures
- Direct laryngoscopy – For evaluation of oropharyngeal and tracheal injuries
- Flexible bronchoscopy – For delineation of tracheal and bronchial injuries
- Esophagoscopy – Flexible esophagoscopy can be used to detect an esophageal injury with less risk of procedure-related complications than rigid esophagoscopy (ie, rupture and complications from general anesthesia). Concerns exist regarding the introduction of oropharyngeal flora into the tissue planes of the neck when performing upper endoscopy in the presence of a perforation because visualization of the central lumen is aided by continuous gas insufflation through the endoscope.
Laboratory studies
Hemoglobin concentration is useful to evaluate for the immediate need for transfusion and to document the starting point for future comparison.
A blood specimen for typing is useful should transfusion be required. As patients who have had prior transfusions become alloimmunized, early recognition of antibody formation is essential to provide compatible blood products.
A toxicologic screen is indicated for the patient with an altered sensorium. This is important to help differentiate the altered sensorium of intoxication from a neurologic etiology following penetrating neck trauma with an arterial injury component.
Penetrating neck injury treatment
The definitive management of penetrating neck trauma continues to be under debate and investigation. Among these investigations is the question of whether the mechanism of injury should dictate the specific management approach. For example, the question exists as to whether a different approach should be applied to gunshot injuries compared to stab wounds.
Although the debate between mandatory neck exploration and selective management already may have favored the latter, the debate has not been resolved with finality. Currently, the debate focuses on selective management versus expectant management and whether the paradigm has shifted too far.
Specific to the ongoing management debate is the question of which essential diagnostic modalities are required for optimal evaluation in the selective management approach. The question exists as to which diagnostic modalities ensure that injuries are not missed.
The optimal surgical management of the carotid artery injury is another controversy in need of resolution. The issues involve whether severe neurologic deficits (ie, coma) and demonstrated absence of antegrade flow in the internal carotid artery contraindicate repair. In several studies, the reestablishment of antegrade flow in these cases has been suggested to be hazardous because it may convert an ischemic infarction into a hemorrhagic infarction.
Further controversy exists regarding the optimal management of vascular injuries identified solely on screening CT angiography in the absence of clinical signs of vessel injury. However, most of these discussions arise in the setting of blunt neck injury. The use of these rapidly developing endovascular techniques for the treatment of subclinical injuries in the neck lacks clear guidelines at present.
Prehospital care
- Resuscitative efforts are imperative, with the emphasis on the airway, breathing, and circulation (ABC).
- The airway is cleared of any obstruction and assessed for possible injury.
- A depressed sensorium and demonstrated poor oxygenation and ventilation are indications to establish a more optimal airway (ie, through endotracheal intubation) and possibly start mechanical ventilation.
- Control of bleeding with direct pressure on the wound site is adequate initially. Large-bore intravenous catheters for fluid resuscitation are inserted. Studies suggest that resuscitation targets with regard to blood pressure be lowered to the range of a mean arterial pressure of 50 mm Hg until definitive hemorrhage control is possible. The concern is that aggressive resuscitation may elevate the blood pressure and increase hemorrhage through an uncontrolled injury site.
- Cervical spine precautions are implemented with suspected spinal cord injury, but these are rare.
- Expeditious transport to an adequate emergency care facility is warranted.
Medical therapy
- To secure a definitive airway, translaryngeal endotracheal intubation should be performed in penetrating neck injuries accompanied by respiratory failure or in cases in which urgent exploration is necessary 39.
- If translaryngeal intubation fails, as occurs in extensive facial or mandibular fractures, a cricothyroidotomy (see the videos below) may be required. Expeditious intubation of a tracheotomy produced by the penetrating injury sometimes may be lifesaving.
- Adequate ventilation and oxygenation usually entails invasive mechanical ventilation. Noninvasive ventilation has little role in treating patients with penetrating neck trauma.
- A warmed balanced sodium chloride solution (ie, Ringer lactate) is the initial resuscitation fluid of choice. Colloid resuscitation strategies may include starch products or component products for transfusion of red blood cells or clotting factors as appropriate.
- Evaluate and monitor the neurologic status of the patient with consideration for spinal cord injury, as well as vascular trauma with cerebral circulatory compromise.
- After the primary survey and resuscitation and stabilization of the patient (if possible without an operation), attention is directed to the identification of specific injuries to determine whether surgical treatment is indicated. If no significant injuries requiring surgery are present, observation or expectant management may proceed.
Surgical therapy
The standard of care is immediate surgical exploration for patients who present with signs and symptoms of shock and continuous hemorrhage from the neck wound. Surgical management varies in difficulty depending on the area of neck injury. Surgical exposure of the injury is particularly difficult in zone 1 and zone 3. Vascular control may be problematic in zone 1 (proximal control) and zone 3 (distal control). This consequently leads to the higher mortality rates in patients with vascular injuries in these neck zones.
Preoperative details
Continue resuscitative efforts and establish a complete list of possible injuries, by diagnostic tests if necessary. Other sites of injury include the adjacent thorax and head or other distant body parts in multiple injuries. Preparation for surgery also includes tetanus prophylaxis, antibiotic prophylaxis (gram-positive coverage), and a specimen for blood typing should component therapy be required.
Intraoperative details
A stabilizing measure that has been reported to be useful involves the placement of a Foley catheter through the injury tract and the balloon inflated to tamponade bleeding. Several series have reported the use of this stabilizing measure, followed by angiography and other ancillary testing to guide the use of operative management. Navsaria reported the use of this strategy in South Africa with a high rate of successful nonoperative management with negative angiography and adjunctive tests 40.
Recently, similar damage-control principles have been described for the critical vascular neck wound. Rezende-Neto and colleagues 41 performed a limited neck exploration without definitive repair of a ligated internal jugular vein and closed a wound over two Foley balloons and rapidly moved the patient to the intensive care unit for resuscitation. After 36 hours, the patient was returned to the operating room for successful, definitive treatment.
A study 42 compared outcomes with Foley catheter tamponade with those obtained with traditional use of external pressure. The study concluded that for penetrating neck and maxillofacial injuries in a combat environment, Foley catheter balloon tamponade significantly reduced mortality when compared with direct pressure techniques through its effect on preventing delayed bleeding 42.
The type of incision depends on the neck zone and the structures at risk for injury. An additional consideration is proper exposure to gain adequate proximal and distal control of the involved blood vessels. The standard neck incision, parallel to the medial border of the sternocleidomastoid muscle, can be used for most zone II injuries and can be extended cephalad for zone III injuries, specifically for injuries to the distal carotid or vertebral arteries. Extension of the standard neck incision, transversely to the opposite side, can be performed for bilateral injuries.
A transverse or collar-type incision can be performed for suspected injuries traversing the cervical region, providing exposure to both sides and obviating the need for bilateral neck incisions.
A supraclavicular incision provides good exposure for zone 1 injuries. Removal of the head of the clavicle with an oscillating saw may provide better exposure. In conjunction, an anterolateral thoracotomy incision also may be used for thoracic inlet injuries.
The trapdoor or open-book thoracotomy includes a median sternotomy with an anterolateral extension and a supraclavicular extension for more exposure of zone I injuries.
The specific injuries described below must be confirmed and treated during neck exploration. Note that multiple structures frequently are injured from penetrating neck injury because of the numerous vital structures that are contained in a small area.
Carotid artery injuries are the most common, with an incidence of approximately 9%. They also pose one of the most immediate life-threatening situations. The objective of surgical care is to arrest hemorrhage yet maintain cerebral blood flow and preserve neurologic function. Arteriorrhaphy, vein patch, or segmental repair with autogenous reversed saphenous vein graft can be performed to repair the injury. Arterial repair is shown to have lower morbidity and mortality rates than ligation. The presence of neurologic deficits, coma, and shock, especially preoperatively, are poor prognostic signs but are not absolute contraindications for carotid artery repair. Carotid ligation is advocated in patients who are comatose with no evidence of antegrade flow in the internal carotid artery. Ligation also can be an option when uncontrollable hemorrhage is present and temporary shunt placement is technically difficult.
Vertebral artery injuries have been diagnosed with increasing frequency with liberal use of arteriography, particularly 4-vessel angiography. The treatment of choice in the well-perfused patient is expectant management. Definitive intervention is indicated if a pseudoaneurysm, an arteriovenous fistula, or persistent bleeding is documented. Surgical repair can be performed, but, if the circle of Willis is patent, ligation is always an option. Angiographic embolization has advantages for this difficult-to-access artery, but distal control is still a problem.
Jugular vein injury repair is contingent on the condition of the patient. Repair can be performed by simple lateral closure, resection and reanastomosis, or saphenous vein graft reconstruction, particularly the internal jugular. Repairing at least one side is very important if both internal jugular veins are injured. The external jugular vein can be ligated without any adverse effects.
Laryngotracheal injuries also are common, with a combined incidence of 10% among cases of penetrating neck trauma. Tracheal injuries can be repaired primarily in one layer of sutures. Interposition of adjacent omohyoid or sternocleidomastoid muscles should be performed when esophageal and arterial repair to prevent fistula formation are performed concomitantly. Tracheostomy is indicated when injury is severe, but performing it through the site of surgical repair should be avoided. A soft intralaryngeal stent in extensive disruption of the cartilaginous support of the larynx is recommended.
Esophageal injuries are the third most common in penetrating neck trauma (6%). Signs and symptoms of dysphagia, hematemesis, subcutaneous crepitus, retropharyngeal air, and injuries to adjacent structures are strong indicators of esophageal injury. Early diagnosis lessens the probability of delayed treatment and missed injury, which can be devastating (ie, mediastinitis). The recommended management of esophageal injury is primary repair and adequate drainage. Oral feeding may be initiated after a barium swallow study shows no evidence of a leak. For extensive injuries or in cases of delayed diagnosis with significant infection, the better option is to establish a controlled fistula with catheter drainage or an esophagostomy. Hypopharyngeal wounds sometimes can be treated with just a nasogastric tube for feeding and parenteral antibiotics. Feeding can be through a feeding jejunostomy or parenteral nutrition.
Nerve injuries account for about 1-3% of cases of penetrating neck trauma. Injury to the vagus, recurrent laryngeal nerve, or brachial plexus should be repaired primarily when feasible (ie, a well-perfused patient without active hemorrhage). Spinal cord injury caused by penetrating trauma is managed expectantly. Steroids have not been shown to benefit injury from penetrating neck trauma.
Thoracic duct injuries, albeit difficult to demonstrate, can occur. They should be ligated to prevent chylous fistula and infections in the neck and mediastinum.
Thyroid injuries are uncommon despite the thyroid’s size and location in the neck. Injuries can cause significant bleeding that often is controlled with direct pressure or suture ligation. Extensive injury may require an ipsilateral lobectomy to resolve the bleeding.
Severe parotid injury is rarely seen. Parotid injuries with associated vessel injury requiring parotidectomy have been reported.
Postoperative details
Vascular injuries are managed postoperatively to ensure hemorrhage is stopped and blood supply and drainage to affected organs is adequate. Continually monitor the neurologic status of the patient. Ancillary angiographic and Doppler ultrasound studies can be performed to evaluate suspected complications with the repaired vessels.
Demonstration of good oxygenation and ventilation and the ability to maintain a patent airway are the parameters generally used to remove ventilatory support and extubation. Repairs of laryngotracheal injuries may require flexion of the neck to reduce tension.
A barium swallow study is performed after 5-7 days to evaluate the integrity of an esophageal injury repair. Oral feeding is initiated if no evidence of leak is present. The drains and feeding tubes also are discontinued. Parenteral antibiotics often are administered for the same duration. For those with controlled fistulas, definitive repair is performed after resolution of infection. Uncontrolled fistulae require the placement of additional drains and possible reexploration. Reexploration is performed for uncontrolled sepsis, as well as failure of percutaneous drainage methods.
Postoperative recovery
After the initial postoperative recovery period, the patient should be monitored closely for complications. Breakdown of surgical repairs occasionally may occur. A high level of suspicion is needed for the early detection of postoperative complications or the need for diagnostic tests to confirm or rule out suspected problems. Long-term complications are uncommon. Cervical esophageal stenosis is rare but is treated adequately by bougienage.
Complications
Missed injuries or delayed diagnosis can occur after any injury to the neck, particularly in patients presenting with minimal manifestations.
- Persistent hemorrhage – Usually from a missed arterial or venous injury, particularly in zone 1 and zone 3
- Pseudoaneurysms – A later sequela from a missed vascular injury, which often is not bleeding actively during treatment
- Arterial dissection – Incomplete transmural vessel injury may cause this disruption between the layers of the arterial wall.
- Fistulas – Esophagocutaneous, esophagotracheal, tracheocutaneous, venoarterial
- Infections – Most often occur from missed esophageal or laryngotracheal injuries; severe inflammation, abscess formation, or mediastinitis may result.
- Stenosis or obstruction of luminal structures – May happen due to the inflammatory response and scarring around the injured esophagus, larynx, trachea, or vessels
- Neurologic deficits – May occur due to the direct injury to a peripheral nerve or to ischemic infarct caused by arterial injury
- Anastomotic or repair disruption – About 1% of surgical repairs leak and result in hemorrhage, infection, or fistula formation.
- Luminal stenosis or obstruction – The surgical repair and the inflammation can cause the narrowing of the lumen of the injured esophagus, larynx, trachea, or vessels.
- Infectious complications – Occurring particularly with injuries to the trachea and esophagus, severe inflammatory response in the neck, abscess formation, fistulas, or mediastinitis may result.
- Neurologic complications – Can occur as strokes related to major vascular injuries or directly to peripheral nerves
- Thrombosis of an internal jugular vein – Can occur regardless of the method of venorrhaphy
- Massive air emboli – May result from major venous injuries and is an important cause of bilateral, diffuse stroke identified as hypodense lesions on CT scan of the brain
Penetrating neck injury prognosis
Vascular trauma is present in 25% of penetrating neck injuries, with mortality rates approaching 50% in some studies. Tracheobronchial injuries may have an incidence of less than 10% to as high as 20% and a mortality rate of as high as 20%. The injured cervical esophagus can result in devastating complications and eventual outcomes, such as leakage of saliva, bacteria, refluxed acid, pepsin, and even bile. Undiagnosed, this can produce early suppurative infection and an intense necrotizing inflammatory response in the neck, as well as a more devastating outcome if it descends to the mediastinum. An 11-17% increase in the overall mortality rate has been observed after delays of 12 hours in the diagnosis of esophageal injuries.
Two recent reports demonstrate the importance of the setting in which penetrating neck injuries occur, particularly treatment protocols in combat zones. Sarkar et al 43 presented 2 cases from Western Baghdad and Ramasamy et al 44 performed a retrospective medical record review of British military casualties from Iraq and Afghanistan who sustained penetrating neck injuries to determine the need for prehospital cervical immobilization, given current advanced trauma life support (ATLS) protocols requiring spinal precautions when a significant mechanism of injury may damage the cervical spine.
In the study by Ramasamy et al 44, of 90 patients with a penetrating neck injury, 66 (73%) were from explosions and 24 (27%) were from gunshot wounds. In 20 (22%) patients, cervical spine injuries were present; only 6 (7%) survived to reach the hospital, and 4 of these 6 died within 72 hours of their injuries. Of 56 survivors that reached a surgical facility, only 1 (1.8%) had an unstable cervical spine injury requiring surgical stabilization, and this patient subsequently died due to a concomitant head injury.
The investigators determined a high mortality rate is associated with penetrating ballistic trauma to the neck 44. Furthermore, it appears unlikely that survivors of penetrating ballistic trauma to the neck will have unstable cervical spines; therefore, not only is the risk/benefit ratio of mandatory spinal immobilization unfavorable, but cervical collars may also hide potential life-threatening conditions, in addition to putting medical teams at prolonged personal risk 44.
Penetrating chest trauma
Penetrating chest trauma is associated with higher overall mortality; in some studies, up to 60% depending on the mechanism of injury 45. Gunshot and stabbing account for 10% and 9.5% of penetrating chest injuries in the United States, making these the most common cause of penetrating trauma 46. Incidence varies based on geographic location, predominating in urban areas, those prone to interpersonal violence, and areas of conflict. Depending on the penetrating trauma, immediate operative intervention may be needed, making early diagnosis integral to survival. The penetrating injury should also be taken into consideration; for example, stab versus missile injury to the chest can result in different patterns of injury.
The amount of tissue damage is directly related to the amount of energy exchange between the penetrating object and the body part. The density of the tissue involved and the frontal area of the penetrating object are the important factors determining the rate of energy loss.
The energy exchange produces a permanent cavity inside the tissue. Part of this cavity is a result of the crushing of the tissue as the projectile passes through. The expansion of the tissue particles away from the pathway of the bullet creates a temporary cavity. Because this cavity is temporary, one must realize that it was once present in order to understand the full extent of injury.
Penetrations from blast fragments or from fragmentation weapons can be particularly destructive because of their extremely high velocities. Weapons designed specifically for antipersonnel effects (eg, mines and grenades) can generate fragments with initial velocities of 4500 ft/s, a far greater speed than even most rifle bullets. The tremendous energy imparted to tissue from fragments with such velocity causes extensive disruptive and thermal tissue damage.
Weaponry of the 21st century consists mostly of improvised explosive devices (IEDs). These devices are homemade bombs, and they create a deadly triad of penetrating, blast, and burn wounds. Of the thoracic trauma that is seen in the current Global War on Terror, 40% is penetrating chest trauma.
Penetrating chest trauma causes
Gunshot and stabbing account for 10% and 9.5% of penetrating chest injuries, making these the most common cause of penetrating trauma in the United States46.
The mechanism of injury may be categorized as low-, medium-, or high-velocity, as follows:
- Low-velocity injuries include impalement (eg, knife wounds), which disrupts only the structures penetrated
- Medium-velocity injuries include bullet wounds from most types of handguns and air-powered pellet guns and are characterized by much less primary tissue destruction than wounds caused by high-velocity forces
- High-velocity injuries include bullet wounds caused by rifles and wounds resulting from military weapons
Shotgun injuries, despite being caused by medium-velocity projectiles, are sometimes included within management discussions for high-velocity projectile injuries. This inclusion is reasonable because of the kinetic energy transmitted to the surrounding tissue and subsequent cavitation.
Ballistics may be divided into three major categories, as follows:
- Internal ballistics describes the characteristics of the projectile within the gun barrel
- External ballistics examines the factors that affect the projectile during its path to the target, including wind resistance and gravity
- Terminal ballistics evaluates the projectile as it strikes its target
Gun shot wounds
The degree of injury also depends on the bio mechanics of the penetrating projectile and includes the efficiency with which energy is transferred from the object to the body tissues. Other factors that dictate the severity of injury include the physical characteristics of the weapon, such as its velocity, size of impact face, deformability and the density of the body tissues penetrated. The velocity of the penetrating projectile is the single most important factor that determines the severity of the wound.
The amount of tissue damage is directly related to the amount of energy exchange between the penetrating object and the body part. The density of the tissue involved and the frontal area of the penetrating object are the important factors determining the rate of energy loss.
The mechanism of injury may be categorized as low, medium, or high velocity. Knives usually produce limited injury because they are classified as low-velocity projectiles. Medium-velocity injuries include bullet wound from most types of handguns and air-powered pellet guns, and are characterized by much less primary tissue destruction than wound caused by high-velocity forces. High-velocity injuries include bullet wound caused by rifles and wounds from military weapons.
Bullets causes injuries of similar severity to knife wounds and tissue damage in the path of penetrating bullet. However, bullets also produce injury in structures adjacent to the bullet path. They produce tissue cavitation and by producing shock waves, extend the area of tissue damage. This cavity collapses because of the resultant vacuum effect, then reforms and collapses several times with diminishing amplitude until all motion ceases. These missiles results in exit wounds that are substantially larger than their corresponding entrance wounds 47.
Dense organs, such as bone and liver, absorb more energy resulting in more injury. Lungs, which have a much lower density, absorb less energy and fortunately suffer less of an injury 48. This explains the low frequency of operative intervention in penetrating chest trauma.
The cardinal rule of management is to leave the impaling object in situ while the patients rapidly transported to an operating theater, because it can have a tamponade-like effect on damaged vascular structures. The object should be removed only in controlled surgical environment.
As always in trauma, initial management begins with establishing airway, breathing, and circulation (ABC). Indications for emergency endotracheal intubation include apnea, profound shock and inadequate ventilation. Chest radiography is not indicated in patients with clinical signs of a tension pneumothorax and immediate chest decompression is accomplished with either a large-bore needle at the second intercostal space or, more definitively, with a tube thoracostomy.
Volume replenishment is the cornerstone of treating hemorrhagic shock, but can also cause significant compromise of other organs systems, such as acute respiratory distress syndrome (ARDS) or a tremendous increase in lung water (soggy lungs) and cardiac compromise 49.
A large chest wall defect can result in a sucking chest wound or large open pneumothorax. This occurs when the injury consists of a large chest wall defect in addition to a sizable visceral pleural injury. A tension pneumothorax usually does not occur because there is a large chest wall defect which allow egress of air. Hypoxia and respiratory acidosis caused by hypoventilation and often asphyxiation can result if this condition is not treated. A patient’s inability to ventilate can be temporarily corrected by covering the wound with a plastic sheet that is taped shut with the exception of a small area of a few inches left unsealed to act as a one-way valve to permit the egress of air from the hemithorax during the phase of exhalation. Immediate placement of a chest tube to prevent tension pneumothorax is required and to facilitate more normal pulmonary ventilation 50.
In hospital, management of a large open chest defects requires operative debridement with removal of devitalized tissue and foreign bodies, such as shotgun wadding materials and bone fragments and closure of the wound. Sometimes, this can be accomplished by mobilizing the surrounding tissues. However, large soft tissue defects may require rotational or free musculocutaneous flaps. The pectoralis muscle, latissimus dorsi or rectus abdominis flaps can be used. The use of synthetic materials such as Marlex, Gore-Tex or methylmethacrylate may be appropriate for elective chest wall reconstruction, but their usage is not recommended after the trauma, due to the risk of infection from contaminationed injury 51.
Stab wounds
Stab wounds of the chest can be made by the different sharp objects such as knifes, daggers, pieces of glass or other metals. The shape of this wounds is not typical, due to the skin elasticity which usually shrink the entrance to the wound.
The severity of stabbing depends on the point of entry to the chest (wound below the nipples in front and the inferior scapular angle at back should be considered as thoraco-abdominal wounds) which organ has been injured (chest wall vessels, lung, heart, great thoracic vessels, visceral pleura, oesophagus, diaphragm), shape and sharpness of penetrating object and finally is penetrating object still in the chest wound or has been taken out. In most cases, stabbing object penetrate through the chest wall hurting intercostal blood vessels and with its tip visceral pleura, contributing developing of pneumothorax or hematopneumothorax 52.
Clinical manifestation of stabbing wound is pain at the point of stabbing, irritation cough and short breath. After taking out the stabbing object from the wound, profuse bleeding is usually present and sometimes wheezing from the suction wound. Blood clot and transected tissue from the chest wall can cover the stabbing wound converting open pneumothorax to tension pneumothorax.
Bleeding from the wound is usually from the intercostal blood vessels, since they are part of systemic circulation, comparing to blood vessels from lungs which are the part of pulmonary circulation with lower pressure.
Penetrating chest trauma signs and symptoms
Admission history and physical examination are usually brief and are oriented to the injury. Evaluations of vital signs, consciousness, airway competency, vascular integrity, and pump (cardiac) function are rapidly performed before devoting attention to the point of injury. If the patient is stable and no significant injury is found that requires immediate surgery, a full diagnostic evaluation can be performed (see Workup).
Any entry wound below the nipples (front) and the inferior scapular angles (dorsum) should be considered an entry point for a course that may have carried the missile into the abdominal cavity.
Missiles from gunshot wounds (GSWs) can penetrate all body regions regardless of the point of entry. Any patient with a gunshot entry wound for which a corresponding exit wound cannot be identified should be considered to have a retained projectile, which could embolize to the central or distal vasculature.
A patient with combined intrathoracic and intra-abdominal wounds has a markedly greater chance of dying.
Open pneumothorax
Open pneumothorax can be recognized by drifting the air through the wound, synchronously with breathing and may be visibly bubbling. During inspiration, when a negative intra-thoracic pressure is generated, air is entrained into the chest cavity not through the trachea but through the hole in the chest wall. This is because the chest wall defect is much shorter than trachea, and hence provides less resistance to flow. Once the size of the hole is more than 0.75 times the size of the trachea, air preferentially enters through the thoracic cavity 53.
This results in hypoxia and respiratory acidosis caused by hypoventilation and often asphyxiation can result if left untreated. The open pneumothorax can become tension if a flap has been created that allows air into the pleural cavity, but not out.
Clinically, breathing is rapid, shallow and labored. There is reduced expansion of the hemithorax, accompanied by reduced breath sounds and an increased percussion note 54.
The definitive management of the open pneumothorax is to place an occlusive dressing over the wound, converting the open pneumothorax into the closed and immediately placing the intercostal chest tube. Rarely, if a chest tube is not available and the patient is far from a definitive care facility, a bandage may be applied over the wound and taped on three sides. This acts as a flap-valve to allow air to escape from the pleural cavity during expiration, but not to enter during inspiration 55.
Tension pneumothorax
Tension pneumothorax develops when a disruption involves visceral, parietal pleura or the tracheobronchial tree. Tension pneumothorax can occur as traumatic, spontaneus or iatrogenic etiology. The disruption occurs when a one-way valve forms, allowing air inflow into the pleural space and prohibiting air outflow. The volume of this nonabsorbable intrapleural air increases with each inspiration. As a result, pressure rises within the affected hemithorax, causes the mediastinum shift toward the contralateral side and compresses the other lung and right atrium of the heart (superior and inferior vena cava) compromised returing the venous blood to the heart-reducing pre load to the heart. Hypoxia leads to increased pulmonary vascular resistance via vasoconstriction. If untreated, the hypoxemia, metabolic acidosis and decreased cardiac output lead to cardiac arrest and death 56.
Physical examination in patient with a tension pneumothorax usually reveals severe respiratory distress, distended neck veins, a hyper-expanded chest, a deviated trachea and absent breath sounds on the affected side.
The immediate release of a tension pneumothorax is best accomplished by placing a needle into the pleural space to allow pressure in the pleura to equilibrate with the outside air. A large-bore, sterile hypodermic needle is introduced into the second intercostal space in midclavicular line. This relieves the compression of the underlying lung as well as the distortion of vital mediastinal structures. Release of the pressure decreases compression on the superior and inferior vena cavae and allows better venous return to the heart and immediate equilibration between the pleural space and the ambient air.
Tension pneumothorax may develop insidiously, especially in patients with positive pressure ventilation.
Penetrating pulmonary injuries are managed with tube thoracostomy alone in most patients (approximately 75%) 57. Of those who require operative intervention, 24% have been shown to require repair of pulmonary hilar or major parenchymal injuries 58. Pulmonary resections in this setting have been shown to carry a mortality rate of 30-60% 59. Death typically ensues from exsanguinating hemorrhage or massive air embolism 60. Air embolism occurs in the setting of a fistulous connection between a bronchus and a pulmonary vein. With spontaneous respiration, the pressure differential favors a gradient from the vein to the bronchus resulting in hemoptysis in 22% of these patients. With positive pressure ventilation or with Valsalva-type respiration, the gradient is reversed 61 and results in systemic air embolism 62.
Penetrating chest trauma complications
Retained pulmonary parenchymal foreign bodies
The decision to remove a retained foreign body depends on its size, its location, and any specific problems associated with it. Objects larger than 1.5 cm in diameter, centrally located missiles, irregularly shaped objects, and missiles associated with evidence of contamination may be prophylactically removed. Typically, such removal is best performed 2-3 weeks following the acute injury.
Chest-wall hernia
A chest-wall hernia is usually a complication of thoracotomy. A patient with a chest-wall hernia presents with pain and an obvious defect, but occasionally a lung may be entrapped and become necrotic. Management includes resection of nonviable tissue and closure with tissue flaps or artificial material
Posttraumatic lung cyst
Pseudocyst of the lung is a rare development and usually manifests as a well-circumscribed, rounded, central air cavity identified on chest radiographs or CT scans. Most do not require specific treatment and resolve spontaneously within a few weeks. Patients with secondary infection present with a lung abscess and should be treated with standard therapy, including antibiotics and drainage.
Pulmonary hematoma
Hematomas form in 4-11% of patients with pulmonary contusions and are observed more frequently in patients with blunt trauma. Symptoms of fever and hemoptysis usually abate in 1 week, though chest radiographs usually demonstrate resolution within 4 weeks. Hematomas are associated with an increased prevalence of abscess formation.
Systemic air embolism
Systemic air embolism is usually described following central penetrating lung injury and is a special risk following primary blast injuries to the lungs. Air can enter the left side of the heart through bronchial and pulmonary venous fistulae and embolize to the coronary and systemic circulations. A precipitating factor is often the institution of PPV with resulting air being forced into the low-pressure pulmonary venules. Embolism can also occur with any thoracic great-vessel injury.
Manifestations include seizures, arrhythmias, and cardiac arrest. Resuscitation requires thoracotomy, clamping of the pulmonary hilum, and aspiration of air from the left ventricle and ascending aorta. Experience with hyperbaric oxygen therapy has generally been good but is usually reserved for those centers with access to larger chambers (ie, to support associated medical personnel).
Bronchial stricture
Missed tracheobronchial laceration may result in significant strictures. Patients present with variable degrees of dyspnea. Evaluation with bronchoscopy and CT is followed by treatment with open operative repair or stenting.
Tracheoesophageal fistula
Delayed tracheoesophageal fistula is rare, generally manifesting approximately 10 days following injury, possibly from delayed necrosis following a blast injury. Usually, the airway at or just above the carina is involved. The timing of surgery or intervention is unclear and depends on the degree of ventilatory leak and the overall condition of the patient.
Persistent air leak and bronchopleural fistula
Traumatic air leaks that last longer than 7 days are unlikely to resolve spontaneously, and judicious manipulation of the chest tube to increase or decrease the suction may be appropriate in order to facilitate healing. Bronchopleural fistulae imply a direct communication between the major airways and the pleural space and usually require some form of intervention for closure.
Empyema
Empyema occurs in 2-6% of patients with penetrating chest trauma. Traumatic empyema differs from nontraumatic forms because it is more often loculated and requires operative debridement. Initial treatment is tube drainage. Thoracoscopy, particularly if performed within 7-10 days, is effective for draining the infection.
Ventilator-associated pneumonia
Ventilator-associated pneumonia occurs in 9-44% of ventilated patients. It increases the mortality in patients who do not have ARDS from 26% to 48% and in patients with ARDS from 28% to 67%. Management consists of ventilator support and appropriate systemic antibiotic therapy.
Missile embolization
Embolization to the pulmonary arteries is usually treated with surgical removal or interventional techniques. A chest radiograph taken immediately preceding incision or intraoperative fluoroscopy is mandatory in order to detect more distal embolization that may occur during positioning. Asymptomatic patients with small distal fragments may be treated expectantly. Occasionally, missile emboli may migrate through a patent foramen ovale or from central parenchymal or vascular injuries to gain access to the left side of the heart and then to the systemic circulation.
Cardiovascular fistulae
Most cardiovascular arterial-to-venous fistulae occur following stab wounds. Virtually all manifest as a machinery murmur after approximately 1 week. Innominate artery-to-vein fistulae are the most common. Patients with coronary artery fistulae, usually to the right ventricle, present with ischemia, cardiomyopathy, pulmonary hypertension, or bacterial endocarditis. Aortocardiac, aortopulmonary, and aortoesophageal fistula are quite rare because the probability of survival from the acute injury is slim.
In the past, penetrating chest trauma patients with cardiovascular fistulae typically required open repair, but in current practice, many such patients can be treated with interventional techniques.
Thoracic duct injury and chylothorax
Injuries to the thoracic great vessels may be complicated by concomitant thoracic duct injury, which, if unrecognized, may produce devastating morbidity due to severe nutritional depletion. Initial management of a delayed chylothorax is always aggressive but nonoperative. Hyperalimentation with total enteral foodstuff restriction (ie, parenteral hyperalimentation) may result in a significant number of spontaneously sealing thoracic duct injuries.
Failure to spontaneously seal after 5-7 days indicates the need for surgical intervention, which should be individualized because the optimal approach is controversial. The number of proponents for direct suture control is equal to the number of those preferring a right thoracotomy to ligate the vessel as it traverses the diaphragm. Experienced personnel can approach the duct thoracoscopically or with video assistance, thus minimizing additional discomfort to the patient.
Penetrating chest trauma diagnosis
Since the trajectory of penetrating injury can vary, a thorough evaluation is key. The primary survey identifies immediately life-threatening injuries. These injuries should be addressed at the time of identification.
Any organ within the chest is potentially susceptible to penetrating trauma, and each should be considered in the evaluation of a patient with thoracic injury 63. These organs include the following:
- Chest wall
- Lung and pleura
- Tracheobronchial system, including the esophagus, diaphragm, thoracic blood vessels, and thoracic duct
- Heart and mediastinal structures
Following a routine method of TRAUMA PROTOCOL evaluation reduces missed injuries. Injuries to the heart and lungs are usually serious, and early diagnosis is vital since they have the highest mortality if missed. Injuries to other thoracic structures also need to be considered; the ribs, clavicle, trachea, bronchi, esophagus, and large vessels including the aorta and veins need to be evaluated in the secondary and tertiary survey.
Potential injuries that should be ruled out include:
- Large hemothorax
- Large pneumothorax
- Pericardial effusion with or without tamponade
- Hemoperitoneum (depending on trajectory)
Once the initial exam is complete and adjunct imaging is complete, a secondary survey may reveal:
- Rib fractures
- Small hemothorax
- Small pneumothorax
- Pulmonary contusion
- Chest wall contusion
There are physical exam findings that increase suspicion of chest trauma. Open wounds should be considered as possible points of entry and or exit. When discussing missile injury, it is imperative to refrain from documenting entry vs exit points since this is a forensic notation and incorrect documentation can have legal ramifications.
Diagnostics
While chest radiography prevails, it does have limitations. Since chest radiography is achieved in the supine position, small and medium-sized pneumothoraces and hemothoraces may be missed 64.
The extended-Focused Assessment with Sonography in Trauma (eFAST) may be done with the primary survey, especially in an unstable patient. Extended-Focused Assessment with Sonography in Trauma (eFAST) allows for quick identification of chest areas with air and/or blood and helps focus definitive management.
The 4 views of the traditional Focused Assessment with Sonography in Trauma (FAST) exam include the cardiac (subxiphoid) window, right upper quadrant (RUQ, or Morrison’s pouch), left upper quadrant (LUQ) and suprapubic (bladder) window. Presence of a black collection outside of an organ, viscera, or pericardia suggests a positive FAST exam.
The eFAST includes pulmonary views and also evaluates for pneumothorax and hemothorax, in addition to the traditional 4 views. eFAST should be started in the area where there is the highest suspicion for injury. If the thorax is of concern, then this is where the eFAST should begin. This includes anterior chest wall evaluation between ribs for pneumothorax and looking for the continuation of the spinal stripe caudal to the diaphragm in the RUQ and LUQ windows to evaluate for hemothorax. The spinal stripe can be present in cases of pleural effusion. Similar to a positive FAST exam, any presence of fluid in the trauma patient is assumed to be blood.
Computed tomography (CT) is more sensitive and specific. However, this requires the patient to be stable for transport.
Other adjuncts include endoscopy, bronchoscopy, and electrocardiography to complete evaluation when warranted.
Penetrating chest trauma treatment
Once the ABCs (airway, breathing, circulation) have been addressed, injury-specific interventions should be undertaken.
Indications for emergency endotracheal intubation include the following:
- Apnea
- Profound shock
- Inadequate ventilation
Immediate, life-threatening injuries require prompt intervention, such as emergency tube thoracostomy for large pneumothoraces, and initial management of hemothorax. For cases of hemothorax, adequate drainage is imperative to prevent retained hemothorax. Retained hemothorax can lead to empyema requiring video-assisted thoracoscopic surgery.
There has been an incremental increase in the utilization of cardiothoracic surgeons for operative intervention in thoracic trauma; although relatively little data are available, this does appear to have resulted in improved patient outcomes 65.
The majority of thoracic trauma can be managed non-operatively. However, 15% of patients require operative management and surgery should not be delayed when appropriate. Operative exploration of thoracic injuries should be considered if tube thoracostomy drainage exceeds 1000 to 1500 mL immediately, or there is an output of about 200 mL per hour for 2 to 4 hours or ongoing resuscitation (blood transfusion, persistent hypotension) with no other discernable cause 66.
In cases where cardiac arrest is imminent, emergency department thoracotomy (EDT) may be indicated for resuscitation. The best survival results are seen in patients who undergo EDT thoracotomy for thoracic stab injuries who arrive with signs of life. Per the Western Trauma Association Critical Decisions in Trauma: Resuscitative thoracotomy success of EDT for patients arriving in shock with penetrating cardiac injury approximates 35% and 15% for all penetrating wounds 67.
Medical management
Damage control appears to be the current mantra in the advanced care of penetrating chest trauma 68. Damage control requires modification of the ABCs of trauma, in that resuscitative and diagnostic techniques are used simultaneously in the immediate time after the unstable patient’s presentation. Quickly and solely controlling hemorrhage and contamination to expedite reestablishing a survivable physiology is the essence of thoracic damage control. Additionally, aggressive correction of the acidosis, coagulopathy, and hypothermia occurs in the intensive care unit (ICU) 69.
Volume replenishment is the cornerstone of treating hemorrhagic shock but can also cause significant compromise of other organ systems. Continuous infusions of even blood or normotonic fluids cause significant peripheral tissue edema, frank acute respiratory distress syndrome (ARDS), or a tremendous increase in lung water (“soggy lungs”) and cardiac compromise. Newer approaches, described in both military and civilian literature, are emphasizing the use of hypertonic solutions in an effort to minimize these complications.
Alternatively, several groups have championed the concept of “scoop and run” in the treatment of injuries in the field 70. With the development of modern (civilian) emergency medical services 71, field care of injured patients has improved. Rapid assessment to identify life-threatening injuries along with key interventions (ie, management of the airway and control of hemorrhage) and avoidance of massive volume increases before rapid transport to the closest appropriate facility is the current standard of care. This is in contrast to the concept of “stay and play,” during which trained personnel make major triage and treatment decisions in the field.
If the patient has persistently low systemic pressure, a source of ongoing blood loss or some other mechanisms to explain the hypotension (eg, cardiac tamponade or tension pneumothorax) should be preferentially sought. Additionally, some data suggest that continued volume resuscitation before surgical control of bleeding may worsen both the bleeding process and final outcome.
Fluid collections in either hemithorax should be treated with percutaneous thoracostomy tubes.
A review by Kamarova et al 72 found strong evidence for antibiotic prophylaxis in patients with chest wounds requiring tube thoracostomy. A systematic review and meta-analysis by Ayoub et al 73 found that in patients with penetrating and blunt chest injuries that necessitated the insertion of a chest drain, prophylactic antibiotic administration was associated with a reduced risk for posttraumatic empyema and pneumonia.
Surgical indications
Thoracotomy
Thoracotomy may be indicated for acute or chronic conditions. Acute indications include the following:
- Cardiac tamponade
- Acute hemodynamic deterioration/cardiac arrest in the trauma center
- Penetrating truncal trauma (resuscitative thoracotomy)
- Vascular injury at the thoracic outlet
- Loss of chest wall substance (traumatic thoracotomy)
- Massive air leak
- Endoscopic or radiographic evidence of significant tracheal or bronchial injury
- Endoscopic or radiographic evidence of esophageal injury
- Radiographic evidence of great vessel injury
- Mediastinal passage of a penetrating object
- Significant missile embolism to the heart or pulmonary artery
- Transcardiac placement of an inferior vena caval shunt for hepatic vascular wounds
Patients who arrive in cardiac arrest or who arrest shortly after arrival may be candidates for emergency resuscitative thoracotomy 74. A right chest tube must be placed simultaneously. The use of emergency resuscitative thoracotomy has been reported to result in survival rates of 9-57% for patients with penetrating cardiac injuries and survival rates of 0-66% for patients with noncardiac thoracic injuries, but overall survival rates are approximately 8% 75.
The Eastern Association for the Surgery of Trauma developed an evidence-based practice management guideline for the use of emergency department (ED) thoracotomy (EDT) in patients who present pulseless with signs of life after penetrating thoracic injury 76.
The proportion of patients with penetrating chest trauma who can be treated without operation has been reported to be in the range of 29-94% 75.
Chronic indications for thoracotomy include the following:
- Nonevacuated clotted hemothorax
- Chronic traumatic diaphragmatic hernia
- Traumatic cardiac septal or valvular lesion
- Chronic traumatic thoracic aortic pseudoaneurysm
- Nonclosing thoracic duct fistula
- Chronic (or neglected) posttraumatic empyema
- Infected intrapulmonary hematoma (eg, traumatic lung abscess)
- Missed tracheal or bronchial injury
- Tracheoesophageal fistula
- Innominate artery/tracheal fistula
- Traumatic arterial/venous fistula
Another indication for acute thoracotomy is often based on chest tube output. Immediate evacuation of 1500 mL of blood is a sufficient indication; however, the trend in output is more important. If bleeding persists with a steady trend of more than 250 mL/hr, thoracotomy is probably indicated.
Thoracoscopy
The role of video-assisted thoracoscopic surgery (VATS) in the management of penetrating chest trauma has been expanding rapidly 77. Initially promoted for the management of retained hemothoraces and the diagnosis of diaphragmatic injury, VATS is being used by trauma and thoracic surgeons for treatment of chest-wall bleeding, diagnosis of transmediastinal injuries, pericardial window, and persistent pneumothoraces 78. The major contraindication for VATS is hemodynamic instability.
Admission
Asymptomatic patients with penetrating thoracic injuries and a normal imaging on presentation should be observed for development of a delayed pneumothorax or hemothorax 79. A repeat examination and imaging should be performed in a delayed fashion. There is no good evidence indicating how long that delayed evaluation should be, however, by convention, at least 6 hours is most appropriate. If the reevaluation is unremarkable, the patient can be discharged from the emergency department, with instructions for strict return if the patient develops increasing shortness of breath, painful swallowing or chest pain.
Minor injuries may simply require close monitoring and pain control. Care should be taken in the young and the elderly. Patients with 3 or more rib fractures, a flail segment, and any number of rib fractures with pulmonary contusions, hemopneumothorax, hypoxia, or pre-existing pulmonary disease should be monitored at an advanced level of care 80.
Pain control
Pain control greatly affects mortality and morbidity in patients with chest trauma 81. Pain leads to splinting which worsens or prevents healing. In many cases, the inability to cough leads to collection of secretions eventually leading to a pneumonia. Early analgesia should be considered to decrease splinting. In the acute setting, IV push doses of short-acting narcotics should be used 82.
Other pain control options include interpleural nerve blocks, transdermal patches, intravenous patient control analgesia (PCA) and epidural analgesia.
Nonnarcotic transdermal patches are safe pain management options for many patients. They should be considered for patients with persistent chest wall pain despite lack of confirmed rib fractures, for patients being discharged or as an adjunct treatment for those who are admitted.
Antibiotics
Prophylactic antibiotics administration for tube thoracostomy for blunt thoracic trauma does not reduce the incidence of empyema or pneumonia when placed with sterile technique.
They should be considered in cases of grossly contaminated wounds, or in cases where the sterile technique was interrupted 83.
All patients with penetrating injury should have up-to-date tetanus vaccination.
Surgical treatment of specific injuries
Chest-wall injury
The chest serves the important functions of respiration and of protection of the vital intrathoracic and upper abdominal organs from externally applied force and is composed of the rigid structure of the rib cage, clavicles, sternum, scapulae, and heavy overlying musculature. Most wounds to these structures can be managed nonoperatively or by means of simple techniques such as tube thoracostomy. The treatment of a stable patient with a normal initial chest radiograph remains controversial.
Ammons et al 84 further defined the role of outpatient observation of selected patients with nonpenetrating thoracic gunshot wounds (GSWs) and stab wounds. In their study, observation for 6 hours with subsequent repeat chest radiography revealed a 7% rate of delayed pneumothorax, and hospitalization was avoided in 86% of patients treated according to this protocol 85.
Closure of a large open chest-wall defect can be a formidable task. When techniques involving closure with autogenous tissue of myocutaneous flaps based on the trapezius, rectus abdominis, pectoral, or latissimus dorsi muscles fail, prosthetic material (eg, polypropylene mesh, expanded polytetrafluoroethylene, or cyanoacrylate) may be used.
Rarely, chest-wall hemorrhage from the muscular, intercostal, and internal mammary arteries can result in exsanguination and may require operative control.
First- and second-rib fractures are often accompanied by serious associated injuries, particularly if multiple rib fractures are evident. Treatment of any associated injuries must be expeditious.
Severe thoracic injury that causes paradoxic motion of segments of the chest wall has been termed flail chest, which may be categorized by size or location. In adults, pulmonary contusion accompanies flail chest injuries in approximately half the patients.
Primary treatment of chest-wall injuries involves a combination of pain control, aggressive pulmonary and physical therapy, selective use of intubation and ventilation, and close observation for respiratory decompensation. Sufficient evidence supports the notion that the pathophysiologic findings associated with severe chest-wall trauma are related to the underlying injuries, chiefly pulmonary contusion and parenchymal injuries, and have little to do with the movement of the chest wall.
Indications for operative fixation of the chest wall or sternum include the following:
- Need for thoracotomy for other reasons
- Large flail segments in patients with borderline premorbid pulmonary status
- Severe instability and pain and failure to wean from the ventilator after an adequate trial
- Secondary infections
Lung injuries
Injuries related to the pleural space can generally be divided into two main categories, pneumothorax and hemothorax. Most patients with such injuries can be cared for with a simple tube thoracostomy. A massive hemothorax is defined as more than 1500 mL of blood in the pleural space. Usually, 200-300 mL of blood must collect in the pleural space before a hemothorax can be detected on a chest radiograph.
Although tube thoracostomy is often a lifesaving procedure and is relatively straightforward, it should not be taken too lightly. A review of almost 600 tube thoracostomies revealed a complication rate of 21% 86.
Pulmonary parenchymal lacerations result in bleeding and air leaks, and the vast majority of these lacerations can be treated with tube thoracostomy. These lacerations extend from the surface of the lung toward the hilum or the trajectory of the penetrating object. They can range from minor lacerations to lobar bisection. Of penetrating injuries that require thoracostomy, 80-90% can be managed with simple measures (eg, stapling, tractotomy, and oversewing).
Fewer than 3% of all patients who require thoracotomy require a pneumonectomy, and this procedure is reserved for patients with severe hilar vascular injuries 87. Postoperatively, aggressive diuresis and selective lung ventilation may reduce the prevalence of pulmonary edema and stump dehiscence.
Tracheobronchial injuries
As many as 75-80% of penetrating injuries involve the cervical trachea, whereas 75-80% of blunt injuries occur within 2.5 cm of the carina. These injuries always occur with other injuries, especially to the great vessels; without early recognition and prompt intervention, they frequently are fatal.
Respiratory distress, subcutaneous emphysema, pneumothorax, hemoptysis, and mediastinal emphysema are the most common manifestations. Occasionally, complete or near-complete transection results in the “fallen lung” sign on chest radiographs. If possible, bronchoscopy should be performed on any patient in whom tracheobronchial injury is suggested.
Patients with small injuries without appreciable leaks who do not require positive-pressure ventilation (PPV) can be treated nonoperatively; however, most patients require urgent repair. The principles of operative repair include debridement with a tension-free end-to-end anastomosis while preserving the blood supply. The preferred suture technique is debatable but usually requires a monofilament suture with knots tied on the outside.
In cases where primary surgical repair is not possible (eg, because of coexisting comorbid conditions, multiple associated trauma injuries, patient instability, or lack of local expertise), endobronchial techniques may be considered 88.
Delay or lack of recognition is common, and subsequent complications of stenosis and obstruction are the rule in missed tracheobronchial injuries.
Esophageal injuries
The exact prevalence of injury to the esophagus due to external trauma is unknown but is lower than 1% among injured patients admitted to hospitals. The majority of esophageal injuries are due to penetrating trauma from a variety of instruments (ie, iatrogenic trauma).
Recognizing injury to the esophagus following trauma is difficult because of the rarity of injuries to this organ, the paucity of clinical signs in the initial 24 hours, and the frequent presence of multiple other injuries. Delayed treatment results in the rapid development of sepsis and an associated high risk of death; therefore, any possibility of injury must prompt aggressive investigation, including radiography, endoscopy, and thoracoscopy (when warranted). The combined use of these techniques has a sensitivity of almost 100%.
Operative management is dictated by the following:
- Site of primary injury
- Presence and severity of associated injuries
- Condition of the patient
- Degree of local suppuration
- Condition of the esophageal tissues
- Delay since injury
Primary repair with adequate tissue buttressing and drainage is the preferred method. Exclusion-diversion procedures have been advocated when primary repair is thought to be contraindicated. Esophageal replacement, when required, is, at best, a poor substitute for the original organ.
Complications after esophageal repair include the following:
- Esophageal leaks and fistulae
- Wound infections
- Mediastinitis
- Empyema
- Sepsis
- Pneumonia
Long-term complications, such as esophageal stricture, are also possible.
Diaphragmatic injury
The diaphragm is frequently injured in penetrating thoracoabdominal trauma. Such injury occurs in 15% of stab wounds and in 46% of gunshot wounds (GSWs). Only 15% of the injuries are longer than 2 cm; therefore, herniation of abdominal contents is rarely immediate. Blunt injuries tend to result in larger lacerations.
No distinctive signs and symptoms are associated with penetrating diaphragmatic injuries. A high index of suspicion is usually required for diagnosis.
Penetrating diaphragmatic injuries are frequently difficult to diagnose without laparoscopy or laparotomy. Diagnostic peritoneal lavage (DPL) appears to be the best-studied procedure, though no consensus has been reached regarding the best red blood cell (RBC) count to use. Laparoscopy and thoracoscopy can be useful in both diagnosing and treating penetrating diaphragmatic injuries.
In general, acute injuries are approached via laparoscopy or laparotomy because of associated injuries, and chronic injuries are approached via thoracoscopy because of dense adhesions that arise between the abdominal contents and the lung. Most injuries require repair with heavy nonabsorbable sutures; some large tears may require mesh closure. Lateral tears may require resuspension from the chest wall.
As many as 13% of injuries are missed in emergency settings, and the patient may present years later when visceral herniation occurs (85% within 3 years), manifesting as decreased cardiopulmonary reserve, obstruction, or frank sepsis. Bowel strangulation and gangrene are associated with a high mortality.
Practice guidelines for the management of traumatic diaphragmatic injuries were published by Eastern Association for the Surgery of Trauma in 2018 89.
Thoracic great-vessel injury
The great vessels of the chest include the aorta, its major branches at the arch (eg, innominate, carotid, and subclavian), and the major pulmonary arteries. The primary venous conduits include the superior and inferior vena cavae and their main tributaries, as well as the pulmonary veins. Damage to vascular structures depends on the specific location and degree of vessel disruption; arterial injuries are more rapidly fatal. The prevalence of great-vessel injuries ranges from 0.3% to 10%.
More than 90% of thoracic great-vessel injuries are caused by penetrating trauma (eg, from gunshot wounds (GSWs), shrapnel woulds, stab wounds, or therapeutic misadventures). Historically, thoracic injuries are associated with a high morbidity; however, Pate et al reported a 71% survival rate in patients who reach the hospital alive after penetrating chest trauma. The trauma surgeon must resuscitate, diagnose, and treat the patient within minutes following admission to the trauma emergency unit.
A patient’s hemodynamic stability dictates the next phase of managing a penetrating great-vessel injury. Patients who are stable after initial resuscitation are best served by a further diagnostic workup. Helical computed tomography (CT), CT angiography (CTA), and transesophageal echocardiography (TEE) offer several advantages over other diagnostic studies.
Helical CT is a noninvasive, sensitive test for assessing mediastinal hematomas and evaluating aortic wall and intraluminal abnormalities. The development of multidetector CT (MDCT) has allowed significantly shorter acquisition times (< 2 minutes for a whole-body CT scan), the ability to retrospectively reconstruct thinner sections, and improvements in three-dimensional (3D) reconstructions.
CTA has developed into a primary method of determining vascular injuries, obviating the much more invasive and operator-dependent conventional angiographic techniques, long held to be the criterion standard for assessment of vascular trauma.
The role of TEE is evolving. Whereas its usefulness for characterizing and confirming traumatic aortic dissections has long been established, it is only comparatively recently that it has come to be used directly in trauma evaluation. The previous lack of experienced operators in the ED setting is being addressed, and continued exposure of the technique will undoubtedly increase its use in the evaluation of trauma patients.
If required, conventional angiography or digital subtraction angiography (DSA) is performed with a surgeon in attendance. The role of intravascular ultrasonography in the evaluation of the trauma patient remains to be determined.
Patients who remain in extremis or show continued rapid hemodynamic deterioration are best served by an emergency thoracotomy for rapid descending aortic cross-clamping and manual control of bleeding. Patients who are successfully resuscitated but remain hemodynamically unstable or who demonstrate continued massive blood loss are unable to undergo a further diagnostic workup and are immediately taken to the operating room.
Proper choice of an incision in order to gain adequate exposure for control and repair of the injury is of prime importance. A median sternotomy with supraclavicular extensions for access to the subclavian vessels is the most useful incision. A posterolateral thoracotomy is the incision of choice for access to the descending thoracic aorta. The trapdoor, or book, incision is of purely historical significance.
Operative repair of thoracic aortic injuries is virtually always possible by means of lateral aortorrhaphy with extremely short cross-clamp times. Rarely, if ever, is an interposition graft required. Adjunctive measures of cardiopulmonary bypass, temporary bypass shunts, or active aortic shunts (eg, a centrifugal pump) are usually not described for use in patients with penetrating trauma but are almost exclusively used for blunt injury. Paraplegia has only rarely been reported after successful repair of penetrating thoracic aortic injury, even after prolonged aortic cross-clamping following emergency thoracotomy.
Because of the proximity of other organs to the thoracic great vessels, an additional diagnostic workup that includes bronchoscopy, esophagoscopy, and echocardiography may be necessary. The timing of these interventions continues to be debated.
Patients with great-vessel injuries have a higher prevalence of associated venous, esophageal, and bronchial plexus injuries than patients without great-vessel injuries do. Trauma patients with severe concomitant injuries who are unlikely to tolerate operative repair may be treated more frequently with endovascular stenting in the future. Mitchell’s series of stent-graft repair of thoracic aortic lesions included seven posttraumatic cases.
The Society for Vascular Surgery (SVS) published data 90 regarding the use of endovascular grafts in the treatment of acute aortic transections; 97% were due to a motor vehicle accident. Sixty symptomatic patients were treated with an aortic endograft, with a mean operating time of 125 minutes and an all-cause mortality of 9.1% at 30 days.
Nonoperative treatment predominantly applies to patients with blunt aortic injuries who are unlikely to benefit from immediate repair (eg, those with minor intimal defects or small pseudoaneurysms). The long-term natural history of these minor vascular injuries remains uncertain; therefore, careful follow-up monitoring, including serial imaging studies, is a critical component of nonoperative treatment.
Cardiac injuries
Traumatic cardiac penetration is highly lethal, with case fatality rates of 70-80%. The degree of anatomic injury and occurrence of cardiac standstill, both related to the mechanism of injury, determine survival probability. Patients who reach the hospital before cardiac arrest occurs usually survive. Those patients surviving penetrating injury to the heart without coronary or valvular injury can be expected to regain normal cardiac function on long-term follow up 91.
Ventricular injuries are more common than atrial injuries, and the right side is involved more often than the left side. In 1997, Brown and Grover 92 noted the following distribution of penetrating cardiac injuries:
- Right ventricle – 43%
- Left ventricle – 34%
- Right atrium – 16%
- Left atrium – 7%
The Beck triad (ie, high venous pressure, low arterial pressure, and muffled heart sounds) is documented in only 10-30% of patients who have proven tamponade 93.
Pericardiocentesis can be both diagnostic and therapeutic, though some centers report a false-negative rate of 80% and a false-positive rate of 33%. This procedure is reserved for patients with significant hemodynamic compromise without another likely etiology.
Echocardiography is a rapid, noninvasive, and accurate test for pericardial fluid. It has a sensitivity of at least 95% and is incorporated into the focused assessment with sonography for trauma (FAST) protocol.
Once again, the management algorithm is based on the patient’s hemodynamic status, with patients who are in extremis or who are profoundly unstable benefiting from emergency thoracotomy with ongoing aggressive resuscitation. In patients with gunshot wounds (GSWs) from high-caliber missiles, the absence of an organized cardiac rhythm portends a grave prognosis. For patients with stab wounds or GSWs from low-caliber missiles who are apparently lifeless upon arrival, resuscitative thoracotomy is justified.
Stable patients with cardiac wounds may be diagnosed by using a subxiphoid pericardial window 94. Bleeding must be rapidly controlled using finger occlusion, sutures, or staples. Inflow occlusion and cardiopulmonary bypass are rarely necessary. Distal coronary injuries are usually ligated, whereas proximal injuries may require bypass grafts. Intracardiac shunts or valvular injuries in patients who survive are usually minor and do not require emergency repair. Foreign bodies in the left cardiac chambers must be removed.
Postoperative deterioration may be due to bleeding or postischemic cardiac myocardial dysfunction. Residual and delayed sequelae include postpericardiotomy syndrome, intracardiac shunts, valvular dysfunction, ventricular aneurysms, and pseudoaneurysms. Wall et al 95, in a classic 1997 paper, described in detail the management of 60 complex cardiac injuries.
Penetrating chest trauma prognosis
The outcomes of treating patients with penetrating chest trauma are directly related to the extent of their injuries and the timeliness with which treatment is initiated. Patients arriving in a stable condition may expect full recovery, but those presenting with lesser levels of stability have diminishing probabilities of survival. No attempt should be made to resuscitate, let alone definitively treat, patients presenting with no vital signs or with obviously nonsurvivable injuries (eg, massive cardiac destruction).
Guidelines for initiation of emergency department (ED) thoracotomy were published in 2014 by the American College of Surgeons (ACS), the American College of Emergency Physicians (ACEP), the National Association of EMS Physicians (NAEMSP), and the American Academy of Pediatrics (AAP) 96; the Eastern Association for the Surgery of Trauma (EAST) published its own guideline in 2015 76.
In a 2010 report from a single center that included 158 patients who underwent thoracotomy within 24 hours after penetrating chest trauma, those patients who died had a significantly lower systolic blood pressure (42 ± 36 mm Hg) than those who survived (83 ± 27 mm Hg) 97.
Penetrating abdominal trauma
Penetrating abdominal trauma typically involves the violation of the abdominal cavity most commonly by a gunshot wound or stab wound 98. The most common organs injured are the small bowel (50%), large bowel (40%), liver (30%), and intra-abdominal vascular (25%) 99. When the injury is close range, there is more kinetic energy than those injuries sustained from a distance. Even though most gunshot wounds typically have a linear projection, the high-energy wounds are associated with unpredictable injuries. There may also be secondary missile injuries from bone or bullet fragments. Stab wounds that penetrate the abdominal wall are difficult to assess. Occult injuries can be missed, resulting in delayed complications that can add to the morbidity 100.
Penetrating abdominal trauma is due to stabbings, ballistic injuries, and industrial accidents. These injuries may be life-threatening because abdominal organs bleed profusely. If the pancreas is injured, further injury occurs from autodigestion. Injuries of the liver often present in shock because the liver tissue has a large blood supply. The intestines are at risk of perforation with concomitant fecal matter complicating penetration.
Approximately 40% of homicides and 16% of suicides by firearm involved injuries to the torso 101.
- Traumatic injury is the third leading cause of death and number one in persons aged 1 to 44 years.
- Penetrating abdominal trauma affects 35% of those patients admitted to urban trauma centers and up to 12% of those admitted in suburban or rural centers.
Penetrating abdominal trauma may cause hypovolemic shock and peritonitis. Penetration may diminish bowel sounds due to bleeding, infection, and irritation, and injuries to arteries may cause bruits. Percussion reveals hyperresonance or dullness suggesting blood. The abdomen may be distended or tender indicating surgery is needed.
The standard management of penetrating abdominal trauma is a laparotomy. A greater understanding of mechanisms of injury and improved imaging has resulted in conservative operative strategies in some cases.
Penetrating abdominal trauma causes
Gunshot wounds, considered high-velocity projectiles, are the most common cause (64%) of penetrating abdominal trauma, followed by stab wounds (31%) and shotgun wounds (5%).
Penetrating abdominal trauma may result from urban violence. Domestic violence crosses all socioeconomic barriers and is an important consideration in the evaluation of injuries sustained at home and those reportedly involving the patient’s family or significant other.
From a global perspective, penetrating abdominal trauma in most settings results principally from military actions and wars.
Penetrating abdominal trauma may be iatrogenically introduced. Documented complications of diagnostic peritoneal lavage include injuries to the underlying bowel, bladder, or major vessels such as the aorta or vena cava. Fortunately, the incidence of such complications is relatively small.
A gunshot wound (GSW) is caused by a missile propelled by combustion of powder. These wounds involve high-energy transfer and, consequently, can involve an unpredictable pattern of injuries. Secondary missiles, such as bullet and bone fragments, can inflict additional damage. Military and hunting firearms have higher missile velocity than handguns, resulting in even higher energy transfer.
In penetrating abdominal trauma due to gunshot wounds, the most commonly injured organs are as follows 102:
- Small bowel (50%)
- Colon (40%)
- Liver (30%)
- Abdominal vascular structures (25%)
The severity of shotgun wounds depends on the distance of the victim from the weapon. The mass of a shot pellet is minimal, and thus its velocity decreases rapidly after the shell leaves the barrel of the gun. When the distance is less than 3 yard, the injury is considered high velocity; if the distance exceeds 7 yard, most of the buckshot penetrates only the subcutaneous tissue.
Stab wounds are caused by penetration of the abdominal wall by a sharp object. This type of wound generally has a more predictable pattern of organ injury. However, occult injuries can be overlooked, resulting in devastating complications.
In penetrating abdominal trauma due to stab wounds, the most commonly injured organs are as follows 102:
- Liver (40%)
- Small bowel (30%)
- Diaphragm (20%)
- Colon (15%)
The mechanism that underlies the penetrating trauma (eg, gunshot wound, stab wound, impalement) relates to the mode of injury (eg, accidental or intentional injury, homicide, suicide). Homicide or intentional injury is the predominant mode of abdominal injury in this patient population. Accidental injury is most common in pediatric home firearm injuries but is uncommon by comparison to the overall levels of homicide and intentional injury. Suicide via penetrating abdominal trauma is uncommon.
Injuries from possible abuse
Pediatric, pregnant, or geriatric patients whose injury occurs in the home may be victims of child abuse, domestic violence, or elder abuse, respectively. Failure to inquire about possible abuse or neglect in such cases is an error of omission and one for which the physician may be held legally accountable.
Mandatory reporting may be required for each of these types of abuse, although specific reporting requirements vary by patient population and locale. For example, statewide databases include external cause of injury codes (E-codes) for the coding and tracking of these injury mechanisms.
Pregnancy
The evaluation of penetrating trauma in the pregnant patient needs to be a coordinated, multidisciplinary effort. Trauma in pregnancy is currently a leading cause of nonobstetric maternal death, and maternal death is the most common cause of fetal death. However, while maternal death rate following penetrating abdominal trauma is 10%, fetal death rate nears 80%.
Anterior abdominal penetrating injury commonly results in injury to the uterus and fetus in the last half of pregnancy. Gunshot wounds have a higher mortality for both mother and fetus 103.
As pregnancy advances into the second trimester, the gravid uterus moves into the abdominal cavity and out of the protected position in the bony pelvis wherein a pregnancy-specific pattern of injury develops. Superiorly displaced visceral organs are less likely to be injured overall, but they are at greater risk when penetrating trauma involves the upper abdomen. Penetrating trauma to the upper abdomen is worrisome for maternal bowel injury, and many authorities strongly believe that upper abdominal injuries should be operatively managed.
Conversely, the uterus and fetus are at significantly increased risk for direct injury as they grow toward the diaphragm. This likely results from the protective effect of the large, muscular uterus on visceral organs. Because trauma over the uterus has a higher risk of fetal injury, an individualized approach has been advocated and may be better suited for lower abdominal injuries.
Gunshot wounds produce transient shock waves and cavitations in displacement of kinetic energy to body tissue, causing more severe injury than a low-velocity knife injury. Stab wounds to the abdomen are less common than gunshot wounds in the pregnant patient, and they have a lower mortality for both mother and fetus.
Fetal mortality generally results from either premature delivery or direct fetal injury by the foreign body. As in blunt trauma, the biophysical status of the fetus should be evaluated by ultrasonography early in the resuscitation after maternal injuries have been stabilized.
The standard of care is to prioritize the emergent treatment of the gravid patient above that of her fetus. However, a definitive role exists for perimortem cesarean section.
Usual criteria for perimortem cesarean section include a fetus of more than 26 weeks’ gestational age (fundal height >26 cm above the pubic symphysis or halfway between the xiphoid and the umbilicus) and a dead or moribund mother. In one review of predictors of fetal survival following such a procedure, more than 70% of surviving fetuses were delivered within 5 minutes of maternal death.
Perimortem cesarean section is a heroic attempt at fetal preservation; the viable fetus that is greater than 26 weeks and has heart tones has a 40-70% chance of survival. More than a 20-minute delay between maternal death and fetal delivery usually results in fetal demise. Care must be taken when interpreting this data, as many of the patients included in the studies of perimortem cesarean sections had experienced blunt trauma 104.
Well-planned preparation is essential to ensure fetal survival should a postmortem cesarean section be indicated. Ideally, an obstetrician should perform the procedure; however, a trauma surgeon or the ED physician also may deliver the fetus in this circumstance, especially when no obstetric support is emergently available.
Every woman who sustains penetrating abdominal (or other) trauma should be questioned specifically about domestic violence. The incidence of domestic violence increases during pregnancy and is clustered during the third trimester.
Geriatric patients
Geriatric patients respond to trauma and shock differently than their younger counterparts, owing to the presence of comorbid conditions, decreased physiologic reserve, elasticity of the vascular system, and concomitant medication use. The decreased physiologic reserve reduces the ability to respond to injury or tolerate aggressive resuscitation, while polypharmacy can alter the hemodynamic response to shock and complicate the patient’s clinical picture. Therefore, the unique characteristics of the geriatric patient often result in under-evaluation of risk and resuscitation status because the absence of tachycardia and hypotension is often misleading. Serum lactate measurements are a better reflection of shock and the response to resuscitative efforts than traditional vital signs in elderly patients.
Trauma in the elderly population should always prompt a search for underlying causes if the precipitating cause is not readily apparent (eg, assault).
Elder mistreatment should always be considered when evaluating trauma to older persons that occurred at their residence. A home safety evaluation as part of a social service inquiry into the appropriateness of home support systems should be conducted.
Pediatric patients
Penetrating injuries account for 10-20% of all pediatric trauma admissions at most centers. Gunshot wounds are responsible for the overwhelming majority of penetrating traumatic injuries and have a significantly higher mortality rate than do blunt mechanisms.
Management approaches have been derived largely from the adult experience. A paucity of literature is dedicated to pediatric penetrating abdominal trauma. However, application of adult strategies to similar life-threatening injuries in the pediatric population has been generally found appropriate 105.
Adult trauma facilities usually have the capability to triage, treat, and stabilize pediatric trauma patients. Transfer guidelines should be established delineating what types of injury complexes are appropriate for the surrounding pediatric facilities.
Consider child abuse during the evaluation of all pediatric trauma patients with suspicious injuries or circumstances. Social workers well versed in investigating child abuse are invaluable in this situation.
Penetrating abdominal trauma signs and symptoms
Signs and symptoms of penetrating abdominal trauma depends on various factors, including the type of penetrating weapon or object, the range from which the injury occurred, which organs may be injured, and the location and number of wounds.
Close-range injuries transfer more kinetic energy than those sustained at a distance, although range is often difficult to ascertain when assessing gunshot wounds. A gunshot wound is caused by a missile propelled by combustion of powder. These wounds involve high-energy transfer and, consequently, can involve an unpredictable pattern of injuries. Secondary missiles, such as bullet and bone fragments, can inflict additional damage. Stab wounds are caused by penetration of the abdominal wall by a sharp object. This type of wound generally has a more predictable pattern of organ injury. However, occult injuries can be overlooked, resulting in devastating complications.
Penetrating abdominal trauma complications
Penetrating abdominal trauma complications include:
- Open wounds
- Sepsis
- Fistulas
- Wound dehiscence
- Colostomy/ileostomy
- Short bowel syndrome
Penetrating abdominal trauma diagnosis
Medical history
The history provides clues to the most likely injury patterns and potential management priorities. Emergency medical services (EMS) personnel are often essential in providing a history, especially in a critically ill patient or one with altered mental status.
A common acronym describing important information to gather when taking the history is AMPLE, as follows:
- Allergies
- Medications
- Prior illnesses and operations
- Last meal
- Events and environment surrounding injury
The anatomic location of injury and type of weapon (ie, gun, knife) direct the diagnostic process. Information such as the number of gunshots heard or the number of times the patient was stabbed, and the patient’s position at the time of injury help describe the trajectory and path of the injuring object.
Close-range injuries transfer more kinetic energy than those sustained at a distance, although range is often difficult to ascertain when assessing gunshot wounds.
Blood loss at the scene should be quantified as accurately as possible from EMS personnel. However, research has shown that this assessment is very difficult and rarely reliable. The character of the bleeding (eg, arterial pumping, venous flow) may assist in determining whether major vascular injury has occurred 106.
The initial level of consciousness or, for moribund patients, the presence of any signs of life at the scene (ie, pupillary response, respiratory efforts, heart rate or tones) is vital to determine the prognosis and to guide resuscitative efforts. Particularly important is the patient’s response to therapy en route to the ED. Evidence of hypotension in the field should raise suspicion for intra-abdominal injury.
Physical examination
Assessment of the patient begins at the scene of the incident by EMS personnel. Upon arrival at the emergency department (ED), communication of the incident history and the patient’s vital signs to the emergency or trauma team is of paramount importance.
The initial physical examination begins with visual assessment of the patient during transport into the ED, with particular focus on the ABCs. Rapid determinations regarding respiratory effort, perfusion, external hemorrhage, and consciousness level are usually easily made. Confounding injuries or medical problems, such as tension pneumothorax or acute myocardial infarction, need be excluded.
Initial vital signs assist in determining injury severity and need for operative intervention. Hypotension, narrow pulse pressure, tachycardia, high or low respiratory rate, or signs of inadequate end organ perfusion in the setting of penetrating abdominal trauma provide evidence of significant intra-abdominal injury, especially vascular trauma, and warrant immediate surgical exploration.
Examination of the abdomen in a patient who is awake may indicate peritoneal signs, such as pain and guarding and rebound tenderness. Hemodynamically stable patients with penetrating abdominal trauma and peritonitis can be assumed to have a hollow visceral perforation and may have significant intra-abdominal hemorrhage. Thus, peritonitis on physical examination is a trigger for emergent intervention regardless of vital signs.
Peritoneal signs develop when the peritoneal envelope and the posterior aspect of the anterior abdominal wall are both inflamed. The peritoneal or retroperitoneal blood and organ contents inflame deeper nerve endings (visceral afferent pain fibers) and result in poorly defined pain. Irritation of the parietal peritoneum leads to somatic pain, which tends to be more localized; however, the diffuse nature of intra-abdominal spillage often leads to diffuse findings.
Referred pain may provide a clue to organ damage. For example, left shoulder pain may result from a damaged spleen with subphrenic blood.
Abdominal distention in an unresponsive patient may indicate active internal bleeding. In hypotensive patients, this may be an indication for immediate exploration. Focused Assessment With Sonography for Trauma (FAST) examination can be useful in this situation to detect massive hemoperitoneum.
Rectal examination is performed on all patients with penetrating abdominal trauma, because blood per rectum and, in males, high-riding prostate can indicate bowel injury and genitourinary tract injury, respectively. Notation of blood at the urethral meatus is also a sign of genitourinary tract injury.
Physical examination includes inspection of all body surfaces, with notation of all penetrating wounds. Multiple wounds may represent either entrance or exit wounds and must not be labeled as such, since multiple missiles or foreign objects may be retained within the body.
Wounds located on the anterior abdomen can be explored locally to determine whether they penetrate the peritoneum. On the flank area and back area, exploration is more difficult and less reliable. Therefore, flank and back wounds are not explored and are considered penetrating unless obviously superficial.
When immediate operative intervention is not requisite, further evaluation ensues with laboratory testing and diagnostic and imaging studies. Sometimes before an x-ray is performed a paper clip is taped over entry and exit wounds 107.
Patients without recordable cardiac activity upon presentation should not be further resuscitated.
Primary survey
The primary survey is defined by the mnemonic ABCDE: Airway, Breathing, Circulation, Disability, and Exposure/Environment. Although described sequentially, much of this evaluation may be performed simultaneously and problems identified are managed immediately.
The airway is assessed immediately for patency, protective reflexes, foreign body, secretions, and injury. Breathing is assessed by determining the patient’s respiratory rate and by subjectively quantifying the depth and effort of inspiration.
The circulation assessment begins with an evaluation of the patient’s mental status, skin color, and skin temperature. Patients in significant hemorrhagic shock will progress from anxiety to agitation and finally coma if their blood loss continues unabated. The traditional vital signs of heart rate, blood pressure, and respiratory rate are not sensitive or specific for hemorrhagic shock.
Disability is assessed early to document neurologic deficits before giving sedation or paralytics. The Glasgow Coma Score and the gross motor and sensory status of all 4 extremities should be determined and recorded. The physician should recognize the need for cerebroprotection measures in cases of brain injury. Hypotension and hypoxemia exacerbate secondary brain injury and increase mortality by 50% in patients with traumatic brain injury.
Exposure is particularly important in the patient with a traumatic mechanism of injury, in whom it may disclose additional, potentially life-threatening injuries. Complete exposure and head-to-toe visualization is mandatory in a patient with penetrating abdominal trauma. This includes the buttocks, posterior legs, scalp, posterior part of the neck, and perineum. There is little to be gained by practicing spinal immobilization unless spinal injury is obvious.
Once the primary survey is complete, a complete head-to-toe physical examination is performed as an integral part of the secondary survey, including digital rectal and genital examinations. This detailed examination may need to be delayed until after operative therapy has corrected obvious life-threatening injury.
Secondary survey and injury assessment
External inspection for injuries with respect to anatomic landmarks aids identification of possible intracavitary injury.
Common physical examination recommendations include evaluation for tympany (a bell-like or percussive note upon gently tapping on the abdomen), dullness to percussion, and bowel sounds. Abdominal distention, not clearly due to “bagging” or swallowed air, may be an indicator of an intra-abdominal catastrophe. A vascular injury is often found in combination with hollow or solid viscus penetration or devitalization.
The physical examination is a more reliable indicator for surgical intervention with penetrating abdominal trauma than with blunt trauma. At many trauma centers, repeated abdominal examinations are the preferred approach for managing hemodynamically stable patients with penetrating abdominal stab wounds.
When selective nonoperative management is used, the indications for operative intervention include the development of hemodynamic instability or the development of increasing pain, peritoneal findings (eg, point tenderness, involuntary guarding, rebound tenderness), or diffuse and poorly localized pain that fails to resolve.
Evisceration has historically been a clear indication for operative management. However, some centers replace eviscerated omentum and serially observe or image these patients.
Impaling objects may tamponade otherwise uncontrolled hemorrhage if the object resides within or crosses a major vessel or solid organ such as the portal vein or liver. Therefore, penetrating objects should not be removed except where definitive treatment can be provided.
For patients with abdominal stab wounds, a policy of observation and serial examination with discharge in 10-12 hours of patients with negative findings has been proposed. While studies have shown promising results, this approach has not been fully validated in multiple centers 108.
Blood and urine studies
In case of need for emergent operation, all patients with penetrating abdominal trauma should undergo certain basic laboratory testing, as follows:
- Blood type and crossmatch
- Complete blood count (CBC)
- Electrolyte levels
- Blood urea nitrogen (BUN) and serum creatinine level
- Glucose level
- Prothrombin time (PT)/activated partial thromboplastin time (aPTT)
- Venous or arterial lactate level
- Calcium, magnesium, and phosphate levels
- Arterial blood gas (ABG)
- Urinalysis
- Serum and urine toxicology screen
Patients who arrive in shock should be typed and cross-matched for 4-8 units packed red blood cells. The CBC provides a baseline value for later comparison, even though it may not reveal the extent of active bleeding. The basic chemistry profile reveals any baseline renal insufficiency or electrolyte abnormalities. Coagulation studies (PT with international normalized ratio [INR] and PTT) may indicate development of coagulopathy. The importance of early coagulopathy of trauma has recently been emphasized. Up to 30% of patients present to the ED with established coagulopathy prior to any resuscitation. Moreover, these patients have significantly increased mortality.
The ABG permits calculation of the anion gap (reference range, 8-12 mmol/L) and base deficit (reference range, ±4 mmol/L) as guides to hypoperfusion. It provides important information regarding acid-base balance and, thus, the hemodynamic stability of the patient.
Urine dipstick testing may reveal occult blood indicative of genitourinary tract injuries. Female patients should have urine pregnancy testing.
Ethanol and drug screens are also standard practice in trauma patients. Studies have shown that even brief intervention and counseling in patients at the time of admission for trauma injury has positive outcomes.
Plain radiography
A chest radiograph is obtained on all patients because penetration of the chest cavity cannot be ruled out, even with abdominal stab wounds or even-numbered GSWs (ie, apparent entrance and exit wounds) outside the chest. Chest radiographs can reveal hemothorax or pneumothorax or irregularities of the cardiac silhouette, which can be a sign of cardiac injury or great vessel injury. Air under the diaphragm indicates peritoneal penetration. Chest radiography is relatively specific, although insensitive, for diagnosing diaphragmatic injury.
Abdominal radiographs in 2 views (ie, anterior-posterior [AP], lateral) are also obtained on all patients with GSWs to help determine missile trajectory and to account for retained missiles (ie, bullets, shrapnel, and foreign bodies) in patients with odd-numbered GSWs. If all foreign bodies are not accounted for, consider the possibility that the foreign body is intraluminal or intravascular, and thus is a potential source of emboli distant from the site of entrance.
Ultrasound
Ultrasonography has been widely used in the assessment of patients with blunt trauma, but it has only recently been used in the assessment of patients with penetrating injuries. In these cases, the study is performed using the focused assessment with sonography for trauma (FAST). FAST has gained acceptance in the evaluation of penetrating abdominal trauma because of its speed, noninvasiveness, and reproducibility in diagnosing intraperitoneal injury that requires laparotomy.
FAST uses 4 views of the chest and the abdomen (ie, pericardial, right upper quadrant, left upper quadrant, pelvis) to evaluate for pericardial fluid indicative of cardiac injury and for free peritoneal fluid. Free fluid in the abdomen can be a sign of hemorrhage secondary to liver or splenic laceration or, less commonly, of spillage secondary to hollow viscus injury.
While FAST has been found to be 94-98% specific for abdominal injury in penetrating abdominal trauma, its sensitivity of 46-67% is not good 109. That is, a positive FAST result in the setting of penetrating trauma is usually an indication for laparotomy due to the high positive predictive value for a therapeutic laparotomy. Unfortunately, a negative FAST result cannot rule out the need for laparotomy and cannot be relied on to exclude important intraperitoneal injury; these patients require further testing to rule out occult injury 110.
Sonographic evaluation of penetrating wounds also has been evaluated in the detection of fascial defects resulting from anterior abdominal stab injuries, reducing the need for local wound exploration. In one prospective trial, a positive fascial sonogram result obviated invasive wound exploration because such patients were then taken to the operating room (OR). However, a negative fascial sonogram result did not rule out a penetration of the peritoneum 111.
Computed tomography
CT scanning is used in the evaluation of patients with stab wounds to the flank and the back and in the evaluation of selected patients with abdominal stab wounds and penetrating, nontangential GSWs. Abdominal CT is the most sensitive and specific study in identifying and assessing the injury severity to the liver or spleen 112. The presence of a contrast blush on CT or ongoing hemorrhage is an indication for laparotomy or angiography and embolization 113.
Triple-contrast helical CT has been evaluated as a diagnostic modality in hemodynamically stable patients with penetrating torso trauma. Oral, intravenous, and rectal contrasts are administered, and the images are reviewed for evidence of peritoneal penetration and visceral injuries.
Triple-contrast CT has been found to be 97% accurate in the evaluation of penetrating flank and back wounds. Exploration of these wounds is more difficult, less reliable, and therefore not indicated. [21] One study of CT with IV contrast only found it useful for patients with GSW to the abdomen selected for nonoperative management 114.
Specific signs of peritoneal penetration on CT include the following:
- A wound tract outlined by hemorrhage, air, or bullet or bone fragments that clearly extend into the peritoneal cavity
- The presence of intraperitoneal free air, free fluid, or bullet fragments
- Obvious intraperitoneal organ injury
The diagnosis of significant penetrating injury should not be delayed by routinely obtaining CT scans of the abdomen and pelvis. Instead, patients with an appropriate history, physical examination or vital sign abnormalities, in particular with a positive FAST, should undergo expeditious exploration 115. There is no place for CT scanning in hemodynamically unstable patients with penetrating abdominal injury.
The primary limitation of CT is lack of sensitivity in diagnosing mesenteric, hollow visceral, and diaphragmatic injuries, all of which are common in penetrating trauma. Therefore, unless the wound is clearly superficial on CT scan, admission and serial observation is indicated, even with a negative CT result for injury 116.
No absolute indications exist for CT in anterior penetrating trauma. Some centers use CT as a screening tool to complement physical examination, while others perform serial examination or diagnostic peritoneal lavage (DPL).
In a prospective study of 200 patients, CT was found to be 97% sensitive and 98% specific for peritoneal violation 117. Laparotomy based on CT findings in 38 of these patients was considered therapeutic in 87%, nontherapeutic in 8%, and negative in 5%. These results were comparable to others obtained with the use of clinical examination, diagnostic peritoneal lavage plus local wound exploration, and diagnostic peritoneal lavage alone 118.
Patient selection is extremely important when considering CT as a diagnostic adjunct in patients with penetrating abdominal trauma. The availability and quality of the CT scan and the experience of the examining radiologist are also key considerations.
Diagnostic or therapeutic procedures
In patients with penetrating abdominal trauma, certain procedures that are necessary for treatment may at times provide diagnostic information.
All patients undergoing endotracheal intubation require decompression of the stomach to decrease the risk of aspiration. Blood in the nasogastric tube can indicate upper gastrointestinal injury.
Foley catheterization insertion is required to monitor the fluid resuscitation status of the patient with penetrating abdominal trauma. The presence of blood in the urine is a sign of genitourinary tract injury.
Diagnostic peritoneal lavage
In the hemodynamically stable patient with penetrating abdominal injury, diagnostic peritoneal lavage can be used to identify hollow viscus or diaphragmatic injury. While very sensitive and specific, diagnostic peritoneal lavage requires a fair amount of time to perform, and it has been supplanted in many institutions’ protocols by FAST, CT scan, and/or laparoscopy. The primary disadvantages are invasiveness, inability to evaluate the retroperitoneum, moderate specificity for therapeutic laparotomy, and a significant false-positive rate 119.
diagnostic peritoneal lavage can be performed via either a closed or open method. The bladder and stomach must be decompressed. The closed method involves a small skin puncture with blind insertion of a catheter over a guidewire (ie, Seldinger technique). The open method involves exposure of the peritoneum through a small infraumbilical incision and insertion of catheter under direct vision (ie, mini-laparotomy).
Aspiration of gross blood or food particles is positive for peritoneal penetration and organ injury. If aspiration is negative, 1 liter of warm normal saline or lactated Ringer solution (20 mL/kg for pediatric patients) is infused rapidly and allowed to return by placing the intravenous bag on the floor 119. The fluid is then sent for analysis (eg, cell count, differential, Gram stain, bilirubin, amylase, vegetable matter, fecal matter).
A positive test result varies with the mechanism of injury. A red blood cell (RBC) count of greater than 100,000/mm3 or white blood cell count of 100-500/mm3 count may be considered positive in a stab wound. However, if a diaphragmatic injury is possible, some physicians lower the value of a positive test to an RBC threshold of 5000/mm³. Because of the more serious nature of gunshot wounds, clinicians often use a similarly lower value for a positive test when there is concern a projectile has entered the peritoneal cavity 119.
The lower the threshold for positivity, the more sensitive the test, but the higher the nontherapeutic laparotomy rate (ie, higher rate of false-positive result).
Laparoscopy
Laparoscopy is a reasonably safe, effective procedure for the evaluation and treatment of hemodynamically stable patients with abdominal trauma, and it can reduce the number of nontherapeutic laparotomies performed. In thoracoabdominal stab wounds, laparoscopy aids in the diagnosis of diaphragmatic and other intra-abdominal injuries.
Patients with stab wounds to the anterior abdomen or with uncertain peritoneal penetration are also candidates for diagnostic laparoscopy. Gunshot wounds to the anterior abdomen with questionable penetration may be assessed this way.
Multiple studies have shown a reduction in unnecessary laparotomies in patients with a penetrating mechanism but no identifiable organ injury who underwent diagnostic laparoscopy. In one center with significant experience with diagnostic laparoscopy in penetrating abdominal trauma, laparoscopy was associated with decreased cost and length-of-stay when compared with open laparotomy (n=44) 111.
A retrospective study of 44 laparoscopies in patients with penetrating abdominal trauma found that half of were negative for penetration and resulted in avoidance of laparotomy 120. A prospective study of 99 patients showed that diagnostic laparoscopy was negative in 62% of the patients with penetrating abdominal trauma, reducing the rate of unnecessary laparotomy from 78.9% to 16.9% 121.
The successful incorporation of diagnostic laparoscopy into the management of patients with penetrating abdominal trauma depends on the selection of hemodynamically stable patients, the availability and ease of use of quality laparoscopic equipment, and the experience of the surgeon in using the technique for diagnostic purposes in traumatic injuries.
Penetrating abdominal trauma treatment
The management of abdominal trauma varies according to the following factors:
- Mechanism and location of injury
- Hemodynamic and neurologic status of the patient
- Associated injuries
- Institutional resources
Management of the patient with penetrating abdominal trauma continues to evolve. After many years of obligatory exploration, expectant management of selected patients has become commonplace.
Much of the present controversy involves the determination of which patients or, more specifically, which injury patterns are suitable for expectant management. Several different methods have been used to establish the injuries present and therefore the need for operative intervention in patients with penetrating abdominal trauma. Most trauma centers use an algorithm with multiple diagnostic modalities whose uses are based on the pattern of injuries and the clinical status of the patient.
In general, gunshots to the abdomen are usually associated with hollow viscus injury and usually require exploration. Knife wounds are associated with lower incidence of intra-abdominal injury, and hence, their work-up requires clinical judgment and experience. Many protocols exist for evaluating patients with a stab wound to the abdomen. Blood work is always done but is nonspecific. The use of DPL and FAST can be performed to assess the stable patient with a knife or gunshot wound, but both these modalities have a high rate of false negatives. CT scan is used in patients with wounds of the flank and back and can help assess solid organ injury. The diagnostic test of choice is a triple contrast CT scan in hemodynamically stable patients. Other imaging tests may be done to assess for any associated head or skeletal injury. In most hospitals, penetrating trauma is handled by a trauma team. After the ABCs are completed, most gunshot patients require an exploratory laparotomy. This view is now changing, and stable patients with gunshot wound with no signs of peritonitis who have been evaluated by a triple contrast CT scan may be observed if there is no evidence of intra-abdominal injury.
The indications for surgical intervention include 122:
- patient with hemodynamic instability,
- development of peritoneal findings such as involuntary guarding, point tenderness or rebound tenderness, and
- diffuse abdominal pain that does not resolve.
Patients with a stab wound with clear signs of peritonitis similarly require a laparotomy. Stable patients with stab wounds may be locally explored or undergo a triple contrast CT scan. The principles of surgery include (1) management of bleeding, (2) quick identification of any serious injury, (3) rapid control of contamination, and (4) reconstruction when possible. If there is an associated vascular injury, a consult with a vascular surgeon is highly recommended.
Depending on the injury, these patients often need some rehabilitation to get them back to their original level of function 123.
Penetrating abdominal trauma prognosis
The death rate from penetrating abdominal trauma spans the entire spectrum (0-100%), depending on the extent of injury and time of presentation to the emergency department. Stab wounds to the abdomen usually have a much better prognosis than gunshot wounds 124. In the presence of massive abdominal contamination from a perforated viscus, hemorrhage, multiorgan injury, associated head injury, or coagulopathy, the mortality rates are high. In patients who are promptly resuscitated and explored, the mortality rates remain low. The majority of deaths occur within the first 24 hours of injury. Risk factors that predict mortality include female gender, the presence of shock on arrival, delay in treatment and associated head injury 99.
Injury patterns differ depending on the weapon. Low-velocity stab wounds are generally less destructive and have a lower degree of morbidity and mortality than gunshot wounds and shotgun blasts. Gunshot wounds and other projectiles have a higher degree of energy and produce fragmentation and cavitation, resulting in greater morbidity 125.
Patients with violation of anterior abdominal wall fascia without peritoneal injury have a 0% mortality rate and minimal morbidity rate, while those with multiorgan injury complexes presenting with hypotension, base deficit less than -15 mEq/L HCO3, core temperature less than 35° C, and development of coagulopathy have a dramatically increased mortality rate mandating “damage control” resuscitation 126.
An average mortality rate for all patients with penetrating abdominal trauma is approximately 5% in most level 1 trauma centers, but this population is necessarily biased, given the higher acuity seen at such centers, thus skewing the data.
Survival from penetrating abdominal trauma has not measurably changed in the past decade, largely because of death within 24 hours resulting from irreversible hemorrhagic shock and exsanguination. More than 80% of deaths occur within 24 hours of admission, 66.7% at the initial operation associated with abdominal vascular injury. In contrast, survival from penetrating abdominal injury without vascular injury remains high 127.
Temporal distribution of deaths in penetrating trauma is significantly different from that in blunt trauma. The majority of deaths from penetrating trauma occur between 1 and 6 hours from admission. In contrast, the highest number of deaths from blunt trauma occurs beyond 72 hours postadmission and the lowest number occurs during the first hour 127.
Consequently, deaths caused by penetrating trauma are significantly more likely to occur in the emergency department or the operating room than deaths caused by blunt trauma, which predominantly occur in the ICU. Hypoperfusion and its sequelae are the usual cause of death within the first 72 hours, whereas ICU deaths 2 or more weeks later are usually from complications related to sepsis, the systemic inflammatory response syndrome (SIRS), or multiple organ dysfunction syndrome 127.
General factors that predict increased mortality from penetrating abdominal trauma include the following:
- Female sex
- Long interval between injury and operation
- Presence of shock on admission
- Coexisting cranial injury
Patients who present to the ED in the early postoperative period with abdominal pain or signs of infection should be strongly considered for CT scan and surgical consultation.
The death rate (mortality rates of more than 50%) is markedly influenced by prehospital hypotension, massive hemorrhage, arrest in the field or on presentation, acidosis with an initial pH less than 7, lactate level greater than 20 mmol/L, or base deficit more negative than -15 mEq HCO3 127.
In a series by Nicholas and colleagues 125 of 250 patients with penetrating abdominal trauma and positive laparotomies, the overall survival was 86.8%. Mortality was found to be associated with the number of organs injured, vascular injury, and the need for damage-control surgery, emergency department thoracotomy, or operating room thoracotomy.
While damage-control surgery has been used with some success in the management of patients with extensive abdominal trauma, it is associated with significant morbidity, including sepsis, intra-abdominal abscess, and gastrointestinal fistula, according to Nicholas et al 125.
References- Kuhajda I, Zarogoulidis K, Kougioumtzi I, et al. Penetrating trauma. J Thorac Dis. 2014;6(Suppl 4):S461-S465. doi:10.3978/j.issn.2072-1439.2014.08.51 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4203982
- Pollak AN, Gupton CL (2002). Emergency Care and Transportation of the Sick and Injured. Boston: Jones and Bartlett. p. 562. ISBN 0-7637-2046-1
- Stewart MG (2005). “Principles of ballistics and penetrating trauma”. In Stewart MG (ed.). Head, Face, and Neck Trauma: Comprehensive Management. Thieme. pp. 188–94. ISBN 3-13-140331-4
- Blank-Reid C (September 2006). “A historical review of penetrating abdominal trauma”. Crit Care Nurs Clin North Am. 18 (3): 387–401. doi:10.1016/j.ccell.2006.05.007
- Notice to Readers: National Emergency Medical Services Week — May 18–24, 2008 https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5719a7.htm
- DiGiacomo JC, Reilley JF (2002). “Mechanisms of Injury/Penetrating trauma”. In Peitzman AB, Rhodes M, Schwab W, Yearly DM, Fabian T (eds.). The Trauma Manual. Hagerstown, MD: Lippincott Williams & Wilkins. ISBN 0-7817-2641-7
- Maiden, Nicholas (2009). “Ballistics reviews: mechanisms of bullet wound trauma”. Forensic Science, Medicine, and Pathology. 5 (3). pp. 204–9. doi:10.1007/s12024-009-9096-6
- Rhee PM, Moore EE, Joseph B, Tang A, Pandit V, Vercruysse G. Gunshot wounds: A review of ballistics, bullets, weapons, and myths. J Trauma Acute Care Surg. 2016;80(6):853-867. doi:10.1097/TA.0000000000001037
- Penetrating Head (Brain) Injuries. https://emedicine.medscape.com/article/247664-overview
- Das JM, Chandra S, Prabhakar RB. Penetrating brain injury with a bike key: a case report. Ulus Travma Acil Cerrahi Derg. 2015 Dec;21(6):524-6.
- Alao T, Waseem M. Penetrating Head Trauma. [Updated 2020 Jul 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459254
- Bizhan A, Mossop C, Aarabi JA. Surgical management of civilian gunshot wounds to the head. Handb Clin Neurol. 2015. 127:181-93.
- Romero Pareja R, Castro Delgado R, Turégano Fuentes F, Jhon Thissard-Vasallo I, Sanz Rosa D, Arcos González P. Prehospital triage for mass casualty incidents using the META method for early surgical assessment: retrospective validation of a hospital trauma registry. Eur J Trauma Emerg Surg. 2020 Apr;46(2):425-433.
- Paiva WS, de Andrade AF, Amorim RL, Figueiredo EG, Teixeira MJ. Brainstem injury by penetrating head trauma with a knife. Br J Neurosurg. 2012 Oct. 26(5):779-81.
- Kumar R, Kumar R, Mallory GW, Jacob JT, Daniels DJ, Wetjen NM, et al. Penetrating head injuries in children due to BB and pellet guns: a poorly recognized public health risk. J Neurosurg Pediatr. 2015 Oct 23. 1-7.
- Siccardi D, Cavaliere R, Pau A, Lubinu F, Turtas S, Viale GL. Penetrating craniocerebral missile injuries in civilians: a retrospective analysis of 314 cases. Surg Neurol. 1991 Jun. 35(6):455-60.
- Murano T, Mohr AM, Lavery RF, et al. Civilian craniocerebral gunshot wounds: an update in predicting outcomes. Am Surg. 2005 Dec. 71(12):1009-14.
- Levy ML, Masri LS, Lavine S, Apuzzo ML. Outcome prediction after penetrating craniocerebral injury in a civilian population: aggressive surgical management in patients with admission Glasgow Coma Scale scores of 3, 4, or 5. Neurosurgery. 1994 Jul. 35(1):77-84; discussion 84-5.
- Kaufman HH, Timberlake G, Voelker J, Pait TG. Medical complications of head injury. Med Clin North Am. 1993 Jan. 77(1):43-60.
- Hida K, Tsuda E, Sato H, Rai M, Imai T. [Brain abscess discovered 38 years after head injury (author’s transl)]. No Shinkei Geka. 1978 Aug. 6(8):811-3.
- Kazemi H, Hashemi-Fesharaki S, Razaghi S, et al. Intractable epilepsy and craniocerebral trauma: analysis of 163 patients with blunt and penetrating head injuries sustained in war. Injury. 2012 Dec. 43(12):2132-5.
- Lange RT, Lippa SM, French LM, Bailie JM, Gartner RL, Driscoll AE, et al. Long-term neurobehavioural symptom reporting following mild, moderate, severe, and penetrating traumatic brain injury in U.S. military service members. Neuropsychol Rehabil. 2019 Apr 19. 1-24.
- Sacks CA, Kamalian S, Masiakos PT, Alba GA, Patalas ED. Case 31-2018: A 37-Year-Old Man with a Self-Inflicted Gunshot Wound. N Engl J Med. 2018 Oct 11. 379 (15):1464-1472.
- Puffenbarger MS, Ahmad FA, Argent M, Gu H, Samson C, Quayle KS, Saito JM. Reduction of Computed Tomography Use for Pediatric Closed Head Injury Evaluation at a Nonpediatric Community Emergency Department. Acad Emerg Med. 2019 Jul;26(7):784-795.
- Maragkos GA, Papavassiliou E, Stippler M, Filippidis AS. Civilian Gunshot Wounds to the Head: Prognostic Factors Affecting Mortality: Meta-Analysis of 1774 Patients. J. Neurotrauma. 2018 Nov 15;35(22):2605-2614.
- Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock. 2011 Jul;4(3):395-402.
- Antiseizure prophylaxis for penetrating brain injury. J Trauma. 2001 Aug;51(2 Suppl):S41-3.
- Allison, K. M., Byom, L. J. & Turkstra, L. S. (2017). Traumatic Brain Injury in Children and Adolescents. In A. Johnson & B. Jacobson (Eds.), Medical Speech-Language Pathology (3rd ed.). Thieme: New York.
- Van Wyck DW, Grant GA, Lasowitz DT. Penetrating Traumatic Brain Injury: A Review of Current Evaluation and Management Concepts. J Neurol Neurophysiol. 2015. 6: 1000336. doi:10.4172/2155-9562.1000336:6:6
- Grahm TW, Williams FC Jr, Harrington T, Spetzler RF. Civilian gunshot wounds to the head: a prospective study. Neurosurgery. 1990 Nov. 27(5):696-700; discussion 700.
- Ley EJ, Srour MK, Clond MA, et al. Diabetic patients with traumatic brain injury: insulin deficiency is associated with increased mortality. J Trauma. 2011 May. 70(5):1141-4.
- Gupta B, Gulati A, Gupta D. A rare presentation of pellet injury in the neck. ISRN Surg. 2011. 2011:306126
- Penetrating Neck Trauma. https://emedicine.medscape.com/article/433306-overview#a7
- Woo K, Magner DP, Wilson MT, Margulies DR. CT angiography in penetrating neck trauma reduces the need for operative neck exploration. Am Surg. 2005 Sep. 71(9):754-8.
- Ferguson E, Dennis JW, Vu JH, Frykberg ER. Redefining the role of arterial imaging in the management of penetrating zone 3 neck injuries. Vascular. 2005 May-Jun. 13(3):158-63.
- Schroeder JW, Baskaran V, Aygun N. Imaging of traumatic arterial injuries in the neck with an emphasis on CTA. Emerg Radiol. 2009 Oct 2. epub ahead of print.
- Fox CJ, Gillespie DL, Weber MA, Cox MW, Hawksworth JS, Cryer CM, et al. Delayed evaluation of combat-related penetrating neck trauma. J Vasc Surg. 2006 Jul. 44(1):86-93.
- Expert Panels on Neurologic and Vascular Imaging, Schroeder JW, Ptak T, et al. ACR Appropriateness Criteria Penetrating Neck Injury. J Am Coll Radiol. 2017 Nov. 14 (11S):S500-S505.
- Kolber MR, Aspler A, Sequeira R. Conservative management of laryngeal perforation in a rural setting: case report and review of the literature on penetrating neck injuries. CJEM. 2011 Mar. 13(2):127-32.
- Navsaria P, Thoma M, Nicol A. Foley catheter balloon tamponade for life-threatening hemorrhage in penetrating neck trauma. World J Surg. 2006 Jul. 30(7):1265-8.
- Rezende-Neto J, Marques AC, Guedes LJ, Teixeira LC. Damage control principles applied to penetrating neck and mandibular injury. J Trauma. 2008 Apr. 64(4):1142-3.
- Weppner J. Improved mortality from penetrating neck and maxillofacial trauma using Foley catheter balloon tamponade in combat. J Trauma Acute Care Surg. 2013 Aug. 75(2):220-4.
- Sarkar D, Demma A, Stulz D, Hsue G. Expect the unexpected: two cases of penetrating head and neck trauma from Operation Iraqi Freedom. Ear Nose Throat J. 2009 Sep. 88(9):E19-21.
- Ramasamy A, Midwinter M, Mahoney P, Clasper J. Learning the lessons from conflict: Pre-hospital cervical spine stabilisation following ballistic neck trauma. Injury. 2009 Jul 16. epub ahead of print.
- Mumtaz U, Zahur Z, Raza MA, Mumtaz M. Ultrasound And Supine Chest Radiograph In Road Traffic Accident Patients: A Reliable And Convenient Way To Diagnose Pleural Effusion. J Ayub Med Coll Abbottabad. 2017 Oct-Dec;29(4):587-590.
- Aghaei Afshar M, Mangeli F, Nakhaei A. Evaluation of Injuries Caused by Penetrating Chest Traumas in Patients Referred to the Emergency Room. Indian J Surg. 2015 Jun;77(3):191-4.
- Inci I, Ozçelik C, Taçyildiz I, et al. Penetrating chest injuries: unusually high incidence of high-velocity gunshot wounds in civilian practice. World J Surg 1998;22:438-42.
- Boyd AD, Glassman LR. Trauma to the lung. Chest Surg Clin N Am 1997;7:263-84.
- Bickell WH, Wall MJ, Jr, Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med 1994;331:1105-9.
- Mandal AK, Sanusi M. Penetrating chest wounds: 24 years experience. World J Surg 2001;25:1145-9.
- Demetriades D, Velmahos GC. Penetrating injuries of the chest: indications for operation. Scand J Surg 2002;91:41-5.
- Asensio JA, Arroyo H, Jr, Veloz W, et al. Penetrating thoracoabdominal injuries: ongoing dilemma-which cavity and when? World J Surg 2002;26:539-43.
- Hughes RK. Thoracic trauma. Ann Thorac Surg 1965;1:778-804.
- Bokhari F, Brakenridge S, Nagy K, et al. Prospective evaluation of the sensitivity of physical examination in chest trauma. J Trauma 2002;53:1135-8.
- Karmy-Jones R, Jurkovich GJ, Shatz DV, et al. Management of traumatic lung injury: a Western Trauma Association Multicenter review. J Trauma 2001;51:1049-53.
- Sharma A, Jindal P.Principles of diagnosis and management of traumatic pneumothorax. J Emerg Trauma Shock 2008;1:34-41.
- Feliciano DV. The diagnostic and therapeutic approach to chest trauma. Semin Thorac Cardiovasc Surg 1992;4:156-62.
- Robison PD, Harman PK, Trinkle JK, et al. Management of penetrating lung injuries in civilian practice. J Thorac Cardiovasc Surg 1988;95:184-90.
- Richardson JD, Miller FB, Carrillo EH, et al. Complex thoracic injuries. Surg Clin North Am 1996;76:725-48.
- Ho AM. Is emergency thoracotomy always the most appropriate immediate intervention for systemic air embolism after lung trauma? Chest 1999;116:234-7.
- Tsakiridis K, Mpakas A, Kesisis G, et al. Lung inflammatory response syndrome after cardiac-operations and treatment of lornoxicam. J Thorac Dis 2014;6Suppl 1:S78-98.
- Boskovic T, Stanic J, Pena-Karan S, et al. Pneumothorax after transthoracic needle biopsy of lung lesions under CT guidance. J Thorac Dis 2014;6Suppl 1:S99-107.
- Berg RJ, Karamanos E, Inaba K, Okoye O, Teixeira PG, Demetriades D. The persistent diagnostic challenge of thoracoabdominal stab wounds. J Trauma Acute Care Surg. 2014 Feb. 76 (2):418-23.
- Ebrahimi A, Yousefifard M, Mohammad Kazemi H, Rasouli HR, Asady H, Moghadas Jafari A, Hosseini M. Diagnostic Accuracy of Chest Ultrasonography versus Chest Radiography for Identification of Pneumothorax: A Systematic Review and Meta-Analysis. Tanaffos. 2014;13(4):29-40.
- Mollberg NM, Tabachnik D, Farjah F, Lin FJ, Vafa A, Abdelhady K, et al. Utilization of cardiothoracic surgeons for operative penetrating thoracic trauma and its impact on clinical outcomes. Ann Thorac Surg. 2013 Aug. 96 (2):445-50.
- Mowery NT, Gunter OL, Collier BR, Diaz JJ, Haut E, Hildreth A, Holevar M, Mayberry J, Streib E. Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma. 2011 Feb;70(2):510-8.
- Burlew CC, Moore EE, Moore FA, Coimbra R, McIntyre RC, Davis JW, Sperry J, Biffl WL. Western Trauma Association critical decisions in trauma: resuscitative thoracotomy. J Trauma Acute Care Surg. 2012 Dec;73(6):1359-63.
- Roberts DJ, Ball CG, Feliciano DV, Moore EE, Ivatury RR, Lucas CE, et al. History of the Innovation of Damage Control for Management of Trauma Patients: 1902-2016. Ann Surg. 2017 May. 265 (5):1034-1044.
- Phelan HA, Patterson SG, Hassan MO, Gonzalez RP, Rodning CB. Thoracic damage-control operation: principles, techniques, and definitive repair. J Am Coll Surg. 2006 Dec. 203 (6):933-41.
- Sanchez GP, Peng EW, Marks R, Sarkar PK. ‘Scoop and run’ strategy for a resuscitative sternotomy following unstable penetrating chest injury. Interact Cardiovasc Thorac Surg. 2010 Mar. 10 (3):467-8.
- Tobey N, Lopez RA, Waseem M. EMS Chest Injury. [Updated 2020 Jul 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539743
- Kamarova M, Kendall R. 13 Prophylactic antibiotics for penetrating injury: a review of practice at a major trauma centre, literature review and recommendations. Emerg Med J. 2017 Dec. 34 (12):A869.
- Ayoub F, Quirke M, Frith D. Use of prophylactic antibiotic in preventing complications for blunt and penetrating chest trauma requiring chest drain insertion: a systematic review and meta-analysis. Trauma Surg Acute Care Open. 2019. 4 (1):e000246
- Boddaert G, Hornez E, De Lesquen H, Avramenko A, Grand B, MacBride T, et al. Resuscitation thoracotomy. J Visc Surg. 2017 Dec. 154 Suppl 1:S35-S41.
- Biffl WL, Moore EE, Harken AH. Emergency department thoracotomy. Mattox KL, Feliciano DV, Moore EE, eds. Trauma. 4th ed. New York: McGraw-Hill; 2000. 245-58.
- [Guideline] Seamon MJ, Haut ER, Van Arendonk K, Barbosa RR, Chiu WC, Dente CJ, et al. An evidence-based approach to patient selection for emergency department thoracotomy: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015 Jul. 79 (1):159-73.
- Swiech A, Boddaert G, Daban JL, Falzone E, Ausset S, Boutonnet M. Penetrating thoracic injuries: a retrospective analysis from a French military trauma centre. J R Army Med Corps. 2019 Jun 6.
- Casós SR, Richardson JD. Role of thoracoscopy in acute management of chest injury. Curr Opin Crit Care. 2006 Dec. 12 (6):584-9.
- Chou YP, Lin HL, Wu TC. Video-assisted thoracoscopic surgery for retained hemothorax in blunt chest trauma. Curr Opin Pulm Med. 2015 Jul;21(4):393-8.
- Kasotakis G, Hasenboehler EA, Streib EW, Patel N, Patel MB, Alarcon L, Bosarge PL, Love J, Haut ER, Como JJ. Operative fixation of rib fractures after blunt trauma: A practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017 Mar;82(3):618-626.
- Battle CE, Hutchings H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: a systematic review and meta-analysis. Injury. 2012 Jan;43(1):8-17.
- Galvagno SM, Smith CE, Varon AJ, Hasenboehler EA, Sultan S, Shaefer G, To KB, Fox AD, Alley DE, Ditillo M, Joseph BA, Robinson BR, Haut ER. Pain management for blunt thoracic trauma: A joint practice management guideline from the Eastern Association for the Surgery of Trauma and Trauma Anesthesiology Society. J Trauma Acute Care Surg. 2016 Nov;81(5):936-951.
- Heydari MB, Hessami MA, Setayeshi K, Sajadifar F. Use of prophylactic antibiotics following tube thoracostomy for blunt chest trauma in the prevention of empyema and pneumonia. J Inj Violence Res. 2014 Jul;6(2):91-2.
- Ammons MA, Moore EE, Rosen P. Role of the observation unit in the management of thoracic trauma. J Emerg Med. 1986. 4 (4):279-82.
- Etoch SW, Bar-Natan MF, Miller FB, Richardson JD. Tube thoracostomy. Factors related to complications. Arch Surg. 1995 May. 130 (5):521-5; discussion 525-6.
- Phillips B, Turco L, Mirzaie M, Fernandez C. Trauma pneumonectomy: A narrative review. Int J Surg. 2017 Oct. 46:71-74.
- Madden BP. Evolutional trends in the management of tracheal and bronchial injuries. J Thorac Dis. 2017 Jan. 9 (1):E67-E70.
- [Guideline] McDonald AA, Robinson BRH, Alarcon L, Bosarge PL, Dorion H, Haut ER, et al. Evaluation and management of traumatic diaphragmatic injuries: A Practice Management Guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2018 Jul. 85 (1):198-207.
- Dake MD, White RA, Diethrich EB, Greenberg RK, Criado FJ, Bavaria JE, et al. Report on endograft management of traumatic thoracic aortic transections at 30 days and 1 year from a multidisciplinary subcommittee of the Society for Vascular Surgery Outcomes Committee. J Vasc Surg. 2011 Apr. 53 (4):1091-6.
- Carr JA, Buterakos R, Bowling WM, Janson L, Kralovich KA, Copeland C, et al. Long-term functional and echocardiographic assessment after penetrating cardiac injury: 5-year follow-up results. J Trauma. 2011 Mar. 70 (3):701-4.
- Brown J, Grover FL. Trauma to the heart. Chest Surg Clin N Am. 1997 May. 7 (2):325-41.
- Reed RL. Lung infections and trauma. Norton JA, Bollinger RR, Chang AE, Lowry SF, Mulvihill SJ, Pass HI, Thompson RW, eds. Surgery: Basic Science and Clinical Evidence. New York: Springer-Verlag; 2001. 1217-30.
- Stranch EW, Zarzaur BL, Savage SA. Thinking outside the box: re-evaluating the approach to penetrating cardiac injuries. Eur J Trauma Emerg Surg. 2017 Oct. 43 (5):617-622.
- Wall MJ Jr, Mattox KL, Chen CD, Baldwin JC. Acute management of complex cardiac injuries. J Trauma. 1997 May. 42 (5):905-12.
- [Guideline] American College of Surgeons Committee on Trauma, American College of Emergency Physicians Pediatric Emergency Medicine Committee, National Association of EMS Physicians, American Academy of Pediatrics Committee on Pediatric Emergency Medicine, Fallat ME. Withholding or termination of resuscitation in pediatric out-of-hospital traumatic cardiopulmonary arrest. Ann Emerg Med. 2014 Apr. 63 (4):504-15.
- Onat S, Ulku R, Avci A, Ates G, Ozcelik C. Urgent thoracotomy for penetrating chest trauma: analysis of 158 patients of a single center. Injury. 2011 Sep. 42 (9):900-4.
- Penetrating Abdominal Trauma. https://emedicine.medscape.com/article/2036859-overview
- Lotfollahzadeh S, Burns B. Penetrating Abdominal Trauma. [Updated 2020 Jun 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459123
- Taghavi S, Askari R. Liver Trauma. [Updated 2020 Jun 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513236
- Nishimura T, Sakata H, Yamada T, Terashima M, Shirai K, Yamada I, Kotani J. Different Patterns in Abdominal Stab Wound in the Self-Inflicted and Assaulted Patients: An Observational Analysis of Single Center Experience. Kobe J Med Sci. 2017 Jul 20;63(1):E17-E21.
- Feliciano DV, Rozcyki GS. The management of penetrating abdominal trauma. Adv Sur. 1995. 28:1-39.
- Eddy VA, Morris JA, Rozycki GS. The Textbook of Penetrating Trauma. Trauma and pregnancy. Lippincott Williams & Wilkins; 1996. 695-701.
- Mattox KL, Goetzl L. Trauma in pregnancy. Crit Care Med. 2005 Oct. 33(10 Suppl):S385-9.
- Cotton BA, Nance ML. Penetrating trauma in children. Semin Pediatr Surg. 2004 May. 13(2):87-97.
- Tall G, Wise D, Grove P, Wilkinson C. The accuracy of external blood loss estimation by ambulance and hospital personnel. Emerg Med (Fremantle). 2003 Aug. 15(4):318-21.
- Sarici İS, Kalayci MU. Is computed tomography tractography reliable in patients with anterior abdominal stab wounds? Am J Emerg Med. 2018 Aug;36(8):1405-1409.
- Alzamel HA, Cohn SM. When is it safe to discharge asymptomatic patients with abdominal stab wounds?. J Trauma. 2005 Mar. 58(3):523-5.
- Boulanger BR, Kearney PA, Tsuei B, Ochoa JB. The routine use of sonography in penetrating torso injury is beneficial. J Trauma. 2001 Aug. 51(2):320-5.
- Udobi KF, Rodriguez A, Chiu WC, Scalea TM. Role of ultrasonography in penetrating abdominal trauma: a prospective clinical study. J Trauma. 2001 Mar. 50(3):475-9.
- Isenhour JL, Marx J. Advances in abdominal trauma. Emerg Med Clin North Am. 2007 Aug. 25(3):713-33, ix.
- Varin DS, Ringburg AN, van Lieshout EM, Patka P, Schipper IB. Accuracy of conventional imaging of penetrating torso injuries in the trauma resuscitation room. Eur J Emerg Med. 2009 Dec. 16(6):305-11.
- Haan JM, Biffl W, Knudson MM, et al. Splenic embolization revisited: a multicenter review. J Trauma. 2004 Mar. 56(3):542-7.
- Velmahos GC, Constantinou C, Tillou A, Brown CV, Salim A, Demetriades D. Abdominal computed tomographic scan for patients with gunshot wounds to the abdomen selected for nonoperative management. J Trauma. 2005 Nov. 59(5):1155-60; discussion 1160-1.
- Neal MD, Peitzman AB, Forsythe RM, et al. Over reliance on computed tomography imaging in patients with severe abdominal injury: is the delay worth the risk?. J Trauma. 2011 Feb. 70(2):278-84.
- Sivit CJ, Eichelberger MR. CT diagnosis of pancreatic injury in children: significance of fluid separating the splenic vein and the pancreas. AJR Am J Roentgenol. 1995 Oct. 165(4):921-4.
- Shanmuganathan K, Mirvis SE, Chiu WC, Killeen KL, Scalea TM. Triple-contrast helical CT in penetrating torso trauma: a prospective study to determine peritoneal violation and the need for laparotomy. AJR Am J Roentgenol. 2001 Dec. 177(6):1247-56.
- Kelemen JJ 3rd, Martin RR, Obney JA, Jenkins D, Kissinger DP. Evaluation of diagnostic peritoneal lavage in stable patients with gunshot wounds to the abdomen. Arch Surg. 1997 Aug. 132(8):909-13.
- Hedges JR, Roberts JR. Clinical Procedures in Emergency Medicine. Peritoneal procedures. 3rd ed. Philadelphia, Pa: WB Saunders; 1997.
- Simon RJ, Rabin J, Kuhls D. Impact of increased use of laparoscopy on negative laparotomy rates after penetrating trauma. J Trauma. 2002 Aug. 53(2):297-302; discussion 302.
- Taner AS, Topgul K, Kucukel F, Demir A, Sari S. Diagnostic laparoscopy decreases the rate of unnecessary laparotomies and reduces hospital costs in trauma patients. J Laparoendosc Adv Surg Tech A. 2001 Aug. 11(4):207-11.
- Givergis R, Munnangi S, Fayaz M Fomani K, Boutin A, Zapata LC, Angus LG. Evaluation of massive transfusion protocol practices by type of trauma at a level I trauma center. Chin. J. Traumatol. 2018 Oct;21(5):261-266.
- Malkomes P, Störmann P, El Youzouri H, Wutzler S, Marzi I, Vogl T, Bechstein WO, Habbe N. Characteristics and management of penetrating abdominal injuries in a German level I trauma center. Eur J Trauma Emerg Surg. 2019 Apr;45(2):315-321.
- Guillen B, Cassaro S. Traumatic Open Abdomen. [Updated 2019 Apr 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470292
- Nicholas JM, Rix EP, Easley KA, et al. Changing patterns in the management of penetrating abdominal trauma: the more things change, the more they stay the same. J Trauma. 2003 Dec. 55(6):1095-108; discussion 1108-10.
- Moore EE, Feliciano DV, Mattox KL. Trauma. 5th. Injury Severity Scoring. USA: McGraw-Hill; 2004. 88.
- Demetriades D, Murray J, Charalambides K, Alo K, Velmahos G, Rhee P, et al. Trauma fatalities: time and location of hospital deaths. J Am Coll Surg. 2004 Jan. 198(1):20-6.