Mydriasis
Mydriasis is an excessive dilation of the pupil due to disease, trauma or drugs. Normally, the pupil dilates in the dark and constricts in the light. A mydriatic pupil will remain excessively large, even in a bright environment. Sometimes colloquially referred to as a “blown pupil.”
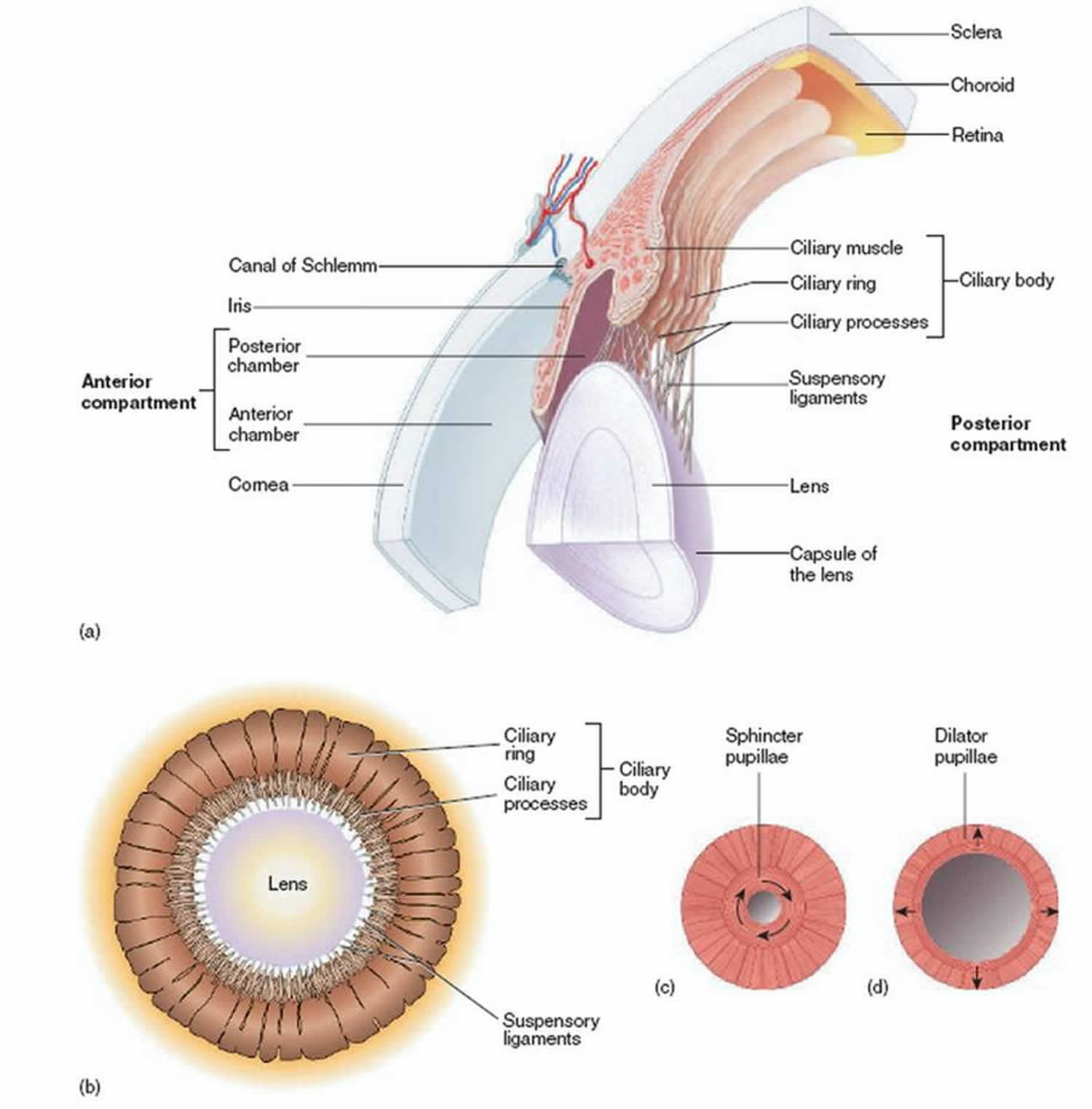
There are two types of muscle that control the size of the iris: circular muscle and radial muscle (Figures 1 and 2). The circular muscle is innervated by the parasympathetic nervous system, the radial muscle by the sympathetic nervous system. Sympathetic stimulation of α1 adrenergic receptors causes the contraction of the radial muscle, and subsequent dilation of the pupil. Conversely, parasympathetic stimulation cause contraction of the circular muscle and constriction of the iris known as miosis.
The mechanism of mydriasis depends on the agent being used. It usually involves either a disruption of the parasympathetic nerve supply to the eye (which causes contraction of the pupil), or over activity of the sympathetic nervous system.
Figure 1. Ciliary muscles
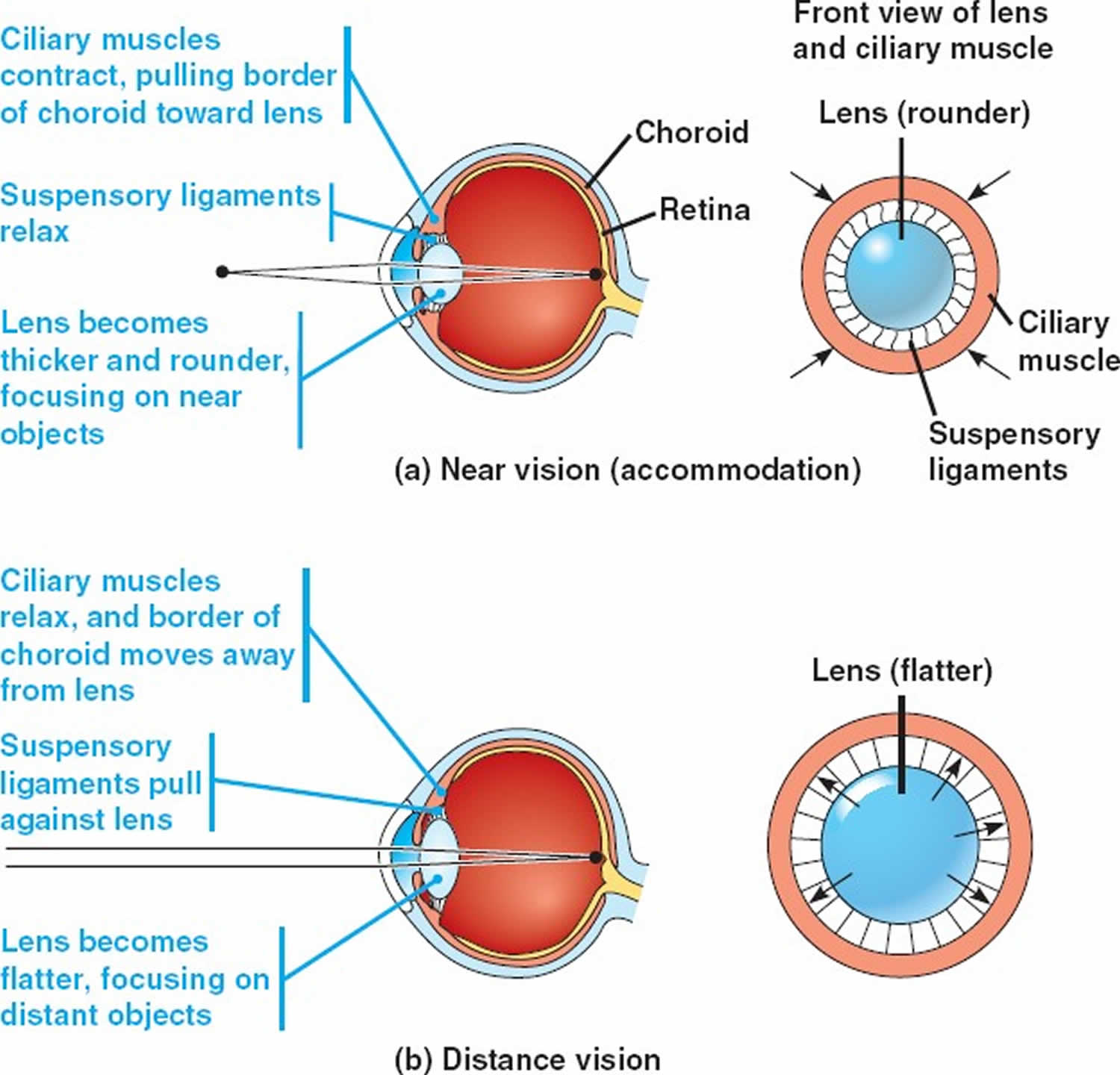
Figure 2. Ciliary muscles function
Mydriasis causes
Mydriasis is caused by either injury to the sphincter muscle in the iris or the parasympathetic nerves innervating the iris 1. Three important causes of mydriasis include an intracranial space-occupying lesion compressing cranial nerve III, pharmacologic mydriasis and traumatic mydriasis.
Common causes of mydriasis:
- Adregenic agents
- Amphetamines
- Antihistamines
- Antipsychotic agents
- Apraclonidine
- Atropine
- Chlorpheniramine
- Chlorpromazine
- Cinnarizine
- Cocaine
- Cyclopentolate
- Diphenhydramine
- Dipivefrin
- Disopyramide
- Dopram injection
- Doxapram hydrochloride
- Hallucinogens
- Hexamethonium
- Hydroxyzine
- Lachesine
- Levomepromazine
- Lysergic acid diethylamide (LSD)
- Mdma
- Mescaline
- Naphazoline
- Noradrenaline
- Opiate
- Oxcarbazepine
- Perazine
- Phenelzine
- Phenylephrine
- Pipothiazine
- Pizotifen
- Prochlorperazine
- Psychedelic mushrooms
- Sibutramine
- Systemic anticholinergics
- Tetrahydrozoline
- Tricyclic antidepressants
- Tropicamide
Mydriatic agent
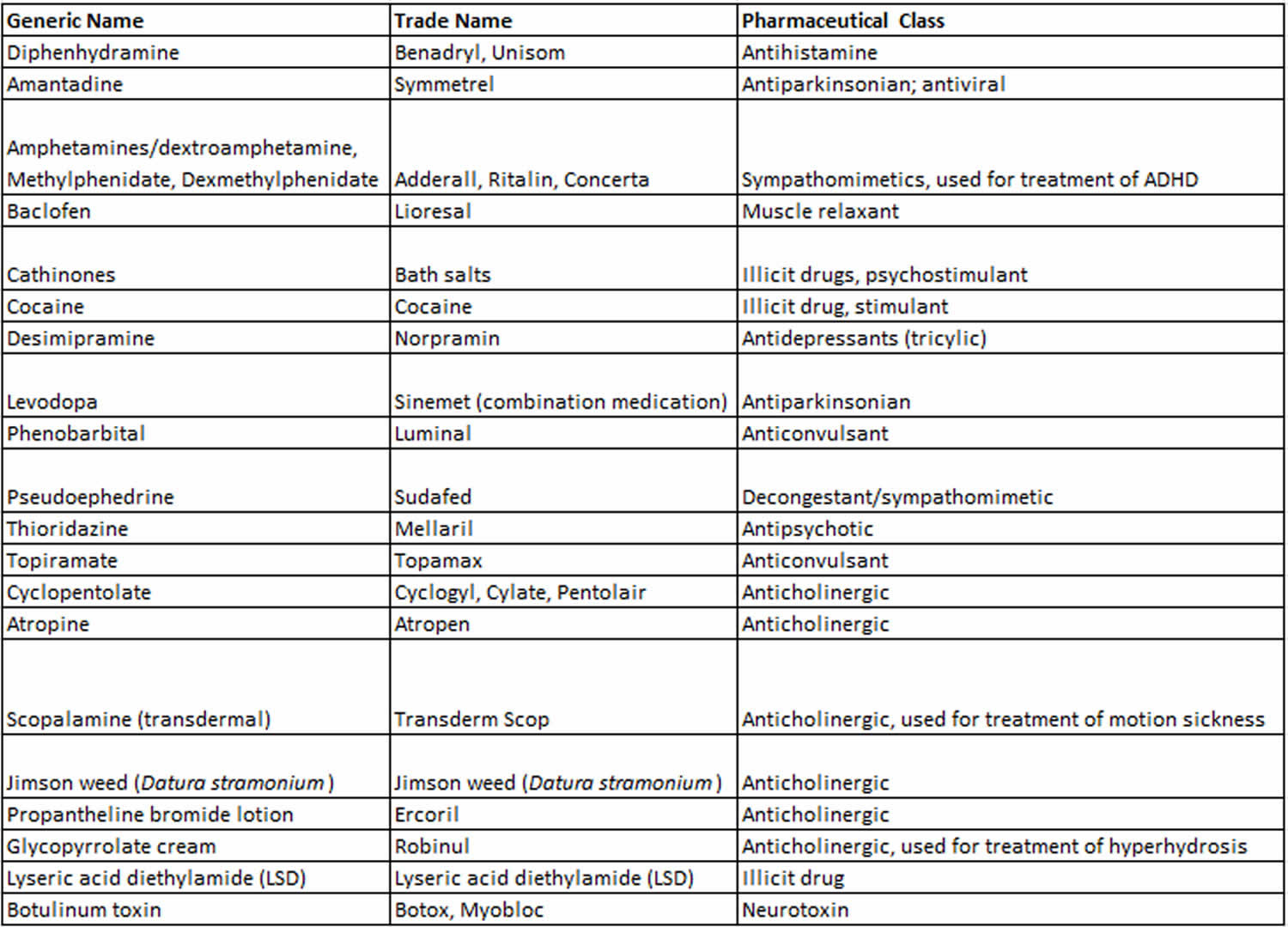
Agents that affect the central nervous system such as atropine, scopolamine, amphetamine, marijuana, lysergic acid diethylaminde (LSD), and glutethimide can cause bilateral mydriasis. This effect is usually accompanied by other signs of central nervous system involvement, such as depression, agitation, and altered level of consciousness. In contrast, the unilateral dilated pupil is usually due to local or topical exposure to an assortment of dilating agents (e.g., mydriatic drops). Anticholinergic mydriasis, also known as pharmacologic blockade and “atropinic” mydriasis, refers to the absolute or partial paralysis of pupillary constriction unilaterally or bilaterally due to topical advertent or inadvertent exposure to an anticholinergic agent. Topical exposure to environmental toxins such as Jimson weed (Datura stramonium) or bella donna alkaloids can also produce mydriasis. Several household or garden plants found in North America contain high concentrations of alkaloids including atropine, scopolamine, hyoscine, and hyoscyamine. The route of exposure to these plant-based mydriatics can include aerosolization of particles from the plant, or direct finger-to-eye contact (e.g., a farmer working in a dusty field, a gardener, or a child picking flowers). Accidental application of nasal drops or sprays with adrenergic properties may also cause a sustained dilation of the pupil (with relatively preserved light reaction). This is also the mechanism of mydriasis caused by indirect acting sympathomimetic drugs like cocaine and amphetamines. Cocaine blocks norepinephrine reuptake at the junction and amphetamines stimulate release of norepinephrine at the junction leading to iris dilator muscle contraction. Adrenergic mydriasis can be distinguished from anticholinergic mydriasis or a cranial nerve III lesion by the presence of blanched conjunctiva, lack of ptosis and motility deficit, and residual light reaction. Local injection of botulinum toxin to treat various neurologic conditions or accidental systemic exposure can also cause toxic pupil. In almost 50% of cases of systemic botulism, bilateral dilated pupils are seen. The mechanism is presynaptic inhibition of acetylcholine release from the short ciliary nerves innervating the iris sphincter muscles.
Anticholinergic mydriasis occurs via blockade of parasympathetic muscarinic acetylcholine receptors on the iris sphincter muscle. Adrenergic mydriasis occurs by overstimulation of the α1-receptors of the iris dilator muscle leading to sustained contraction. Local botulinum toxin overexposure or systemic poisoning leading to mydriasis occurs via presynaptic inhibition of acetylcholine release from the short ciliary nerves innervating the iris sphincter muscles.
The primary risk factor is exposure to mydriatic agents. Common examples of accidental exposure include finger-to-eye contact after handling an anticholinergic agent (e.g., healthcare workers, travelers with motion sickness) and ill-fitting nebulizer treatment masks.
Primary prevention is best accomplished by avoidance of exposure to causative agents. Healthcare workers can reduce their risk of this condition by employing proper hand hygiene practices.
Table 1. Agents that may cause mydriasis therapeutically or in overdoses
[Source 2 ]Mydriatic agent signs and symptoms
Mydriatic agent signs
Patients with bilateral pupil involvement from anticholinergic toxicity may present with altered mental status, dry skin, fever, flushing, myoclonus, seizures, and urinary retention.
Mydriatic agent symptoms
The patient may complain of photophobia and/or blurred vision, but it is not unusual for a patient to be asymptomatic. In the setting of systemic anticholinergic poisoning, the patient may have multiple systemic complaints such as heart palpitations, shortness of breath, constipation, urinary retention, tremulousness, memory difficulty, and visual hallucinations.
Mydriatic agent diagnosis
The diagnosis is made based on the history and physical exam. Often the diagnosis can be made based on a detailed history (e.g., use of topical mydriatics, nasal inhalers, scopolamine patch for motion sickness) supported by physical exam. Special attention should be paid to the patient’s recent exposure history to possible mydriatic agents.
Physical examination
Characteristically, the pharmacologically blocked pupil will have the following qualities: poor or no response to light and poor or no response to near. There should not be ptosis or ocular motility restriction (as in third nerve palsy). There will be poor or no response to pharmacologic (pilocarpine 1%) testing because of the pharmacologic block. The condition may be unilateral or bilateral.
Pharmacologic testing of the dilated pupil with varying concentrations of pilocarpine eye drops can be useful in diagnosis. The following protocol may be used:
- Instill 1 drop 1/10% or 1/16% pilocarpine in each eye. Observe for 45 minutes. If parasympathetic denervation/tonic pupil (e.g., Adie’s pupil) present, the involved eye with the dilated pupil will constrict. The mechanism is hypersensitivity of the cholinergic receptors of the iris sphincter muscle.
- If no constriction following dilute pilocarpine administration, instill 1 drop 1% pilocarpine in each eye. If compressive lesion of cranial nerve III present, constriction of the dilated pupil will occur because there is no dysfunction of the muscarinic receptors of the iris sphincter muscle. If constriction occurs, then consideration for evaluation for third nerve palsy (e.g., exclusion of posterior communicating artery aneurysm should be pursued via high resolution cranial computed tomography angiography (CTA) and magnetic resonance imaging (MRI)/ magnetic resonance angiography (MRA) imaging).
- If following concentrated topical 1% pilocarpine drop administration, no constriction occurs and there is no reaction to light or near, the diagnosis of pharmacologic pupil can be made. Note: One exception is botulinum toxin poisoning. The presynaptic inhibition of acetylcholine release by the neurotoxin results in a toxic dilated pupil that does constrict following 1% pilocarpine administration.
Mydriatic agent treatment
Once the diagnosis of anticholinergic or adrenergic mydriasis is made, the patient can be reassured that the pupil will return to normal size and vision (accommodation) as the effects of the precipitating agent diminish. Steps should be made to prevent repeat exposure to the precipitating agent.
Medical follow up
The patient should be seen in routine follow-up after discontinuation of the precipitating agent (exact timing will depend on the half-life of the agent and route of administration), to ensure return to baseline. Persistent pupil dilation after a sufficient wash-out period should prompt re-evaluation for other causes of pupil dilation.
Mydriatic agent prognosis
Prognosis is excellent for pharmacologic dilation of the pupil, and the condition should completely resolve with removal of the precipitating agent. Resolution of dilation depends on the different agents’ half life.
Traumatic mydriasis
Traumatic mydriasis is pupillary dilation due to blunt eye trauma. Direct blunt trauma to the globe may result in traumatic mydriasis or, less commonly, miosis. Traumatic mydriasis is often associated with iris sphincter tears or small tears in the ciliary muscles that can permanently alter the shape of the pupil. Symptoms include eye pain, blurry vision and photophobia. Pupil is poorly reactive to light in both direct and consensual light exposure. Contusion of the muscle results in a transient mydriasis, while tears to the muscle fibers can cause permanent injury. The mainstay of prehospital management involves protection of the eye from further injury during transport. Emergency department evaluation involves ruling out other causes of mydriasis and facilitating ophthalmologic evaluation. Surgical repair is a potential option for patients with severe and persistent symptoms 3. Cycloplegia is essential to prevent formation of posterior synechiae.
References- Kawasaki A: Disorders of pupillary function, accommodation, and lacrimation. In Miller NR, Walsh FB, Hoyt WF (Eds.), Walsh and Hoyt’s clinical neuro-ophthalmology. Lippincott Williams & Wilkins: Philadelphia, pp. 739–805, 2005.
- Pharmacologic dilation of pupil. https://eyewiki.org/Pharmacologic_dilation_of_pupil
- Angmo, D., Agarwal, T., & Khokhar, S. (2013). Single Pass, Single Suture Technique for Repair of Traumatic Mydriasis. European Journal of Ophthalmology, 23(4), 590–592. https://doi.org/10.5301/ejo.5000237